Abstract
Background: To our knowledge, there has been no prospective study on the results of arthroscopic repair of superior labrum-biceps anchor complex (SLAP) tears with use of modern techniques. The purpose of the present study was to prospectively evaluate the minimum two-year results for patients with type-II SLAP tears that were treated with arthroscopic suture anchor fixation.
Methods: Forty-seven patients with symptomatic type-II SLAP tears were evaluated preoperatively and at least two years postoperatively with use of the American Shoulder and Elbow Surgeons (ASES) and L'Insalata outcomes instruments and physical examination. The study group included thirty-nine male and eight female patients with a mean age of thirty-six years; thirty-four of the forty-seven patients were athletes. Patients with rotator cuff tears requiring repair or concomitant shoulder instability were excluded.
Results: At an average of 2.7 years, the median ASES and L'Insalata scores were 97 and 93, respectively, compared with baseline scores of 62 and 65 (p < 0.05). The median patient-reported satisfaction rating was 9 (of 10); forty-one patients (87%) rated the outcome as good or excellent. The median patient-reported satisfaction rating was significantly higher for patients with a discrete traumatic etiology than for those with an atraumatic etiology (9 compared with 7); however, there was no significant difference between these groups in terms of the ASES or L'Insalata outcome scores. Overall, twenty-five (74%) of the thirty-four athletes were able to return to their preinjury level of competition, whereas eleven (92%) of the twelve athletes who reported a discrete traumatic event were able to return to their previous level of competition. There were five complications, including four cases of refractory postoperative stiffness.
Conclusions: Our findings indicate that favorable outcomes can be anticipated in the majority of patients after arthroscopic SLAP lesion repair. While only three of four patients overall may be capable of returning fully to their previous level of competition, patients with a distinct traumatic etiology have a greater likelihood of a successful return to sports.
Level of Evidence: Therapeutic Level IV. See Instructions to Authors for a complete description of levels of evidence.
Injuries of the superior labrum-biceps anchor complex were initially recognized as a pathologic entity in overhead athletes by Andrews et al. in 19851. Snyder et al. subsequently defined these injuries as “SLAP” lesions and proposed a classification system that divided them into four subtypes on the basis of the amount of damage to or destabilization of the biceps anchor2. Type-II SLAP lesions, characterized by detachment of the superior labrum and biceps anchor, represent the most commonly encountered variant, accounting for at least 50% of superior labral tears secondary to trauma and the majority of SLAP lesions found in overhead athletes2-7. The proposed etiologies for a type-II SLAP tear include a direct compression injury to the superior labrum between the glenoid and the greater tuberosity in association with trauma or repetitive overhead activities and a traction injury produced by an eccentric biceps contraction during an injury or with deceleration of the arm in overhead athletics1,2,7.
The surgical treatment of SLAP lesions has undergone a considerable evolution because of advances in arthroscopic techniques and instrumentation. Early studies demonstrated only short-term improvement after isolated arthroscopic labral débridement of unstable SLAP lesions, with deteriorating outcomes over time3,8,9. The current approach to type-II SLAP lesions favors surgical repair. Multiple fixation methods have been utilized, including transosseous sutures, arthroscopic suture anchors, staples, screws, and bioabsorbable tacks3,10-19. A survey of the literature revealed outcome data based largely on retrospective series consisting of small numbers of patients and involving various surgical techniques and fixation options. In the only prospective case series that we could identify, Paxinos et al. reported on twenty-four patients who had arthroscopic treatment with use of biodegradable tacks, resulting in nearly complete improvement in terms of pain and recovery of function by three months17. The use of tacks has decreased substantially as reports of synovial inflammation and severe joint destruction due to broken or prominent implants have emerged20,21.
At the present time, arthroscopic repair of type-II SLAP lesions at our institution is performed with use of suture anchors and arthroscopic knot-tying techniques. While the reported outcomes of SLAP lesion repair have been favorable in most series, there is some concern with regard to postoperative stiffness and the ability of patients to successfully resume their previous level of athletic activities. Furthermore, we are not aware of any prospective study documenting patient outcomes after arthroscopic SLAP lesion repair with use of arthroscopic suture anchor stabilization. The purpose of the present study was to prospectively evaluate the minimum two-year results for patients with type-II SLAP tears that were treated with arthroscopic suture anchor fixation. By including only patients with this isolated subset of labral injuries, we hope to more accurately guide patient and physician expectations with regard to outcomes and return to activities.
Materials and Methods
The study was approved by the institutional review board to report from the “Prospective Labrum and Instability Registry” (#21101) established by the faculty members of the Sports Medicine and Shoulder Service at our institution. Patients provided informed consent. Patients who were diagnosed preoperatively with an asymptomatic labral tear and presented for an index arthroscopic labral repair that was to be performed by any member of our department were enrolled before surgery after informed consent was obtained. Patients qualified for inclusion in the registry if they subsequently underwent arthroscopic labral repair with use of suture anchor fixation and arthroscopic knot-tying techniques.
Over a one-year period, a total of 237 patients qualified preoperatively for inclusion in the longitudinal, prospective registry. At the time of surgery, 158 patients were excluded because a different postoperative diagnosis was made, no labral fixation was performed, only labral débridement was performed, or they were classified as having another type of SLAP lesion. The remaining seventy-nine patients underwent arthroscopic repair of a type-II SLAP lesion. Ten patients who underwent concomitant rotator cuff repair and eight patients who underwent concomitant Bankart repair for the treatment of anterior instability were excluded. Of the remaining sixty-one patients, forty-seven (77%) were evaluated after a minimum duration of follow-up of two years (mean, 2.69 years; range, 2.01 to 4.06 years) and represent the study cohort. Fourteen patients were unable to be evaluated at the minimum two-year time point for a variety of reasons; specifically, one patient was involved in compensation litigation regarding the injury and was advised by his legal counsel to forgo follow-up, one patient was out of the country and refused follow-up, and twelve patients were unable to be scheduled for a follow-up visit despite repeated attempts to contact them.
The study group included thirty-nine male and eight female patients with a mean age of thirty-six years (range, fourteen to forty-nine years) at the time of surgery. One patient was less than twenty years of age, nine were twenty to thirty years of age, twenty-three were thirty-one to forty years of age, and fourteen were more than forty years of age. The right shoulder was treated in thirty-two patients, and the left shoulder was treated in fifteen; thirty-four patients had involvement of the dominant extremity. Thirty-four patients had participated in athletics prior to the shoulder injury. These patients included three professional athletes, five collegiate-level athletes, and twenty-six recreational athletes. Twenty-eight patients participated in overhead athletics at a recreational level or higher, including baseball (eleven), tennis (seven), softball (five), swimming (five), volleyball (two), and squash (one).
Twenty-five of the forty-seven patients recounted a distinct traumatic injury of the shoulder due to a fall (twelve), an injury sustained during contact sports or weight-lifting (seven), an injury sustained in an automobile or bicycle accident (three), or an injury associated with lifting a heavy object (three). Twenty-two patients reported an insidious onset of shoulder symptoms with no inciting trauma. All twenty-two patients had been involved in athletics, and twenty had been involved in overhead sports.
Before surgery, the patients completed a series of questionnaires and validated outcomes measures, including the American Shoulder and Elbow Surgeons (ASES) and L'Insalata outcomes instruments, which provided the baseline data for comparison with the postoperative findings. At the time of the minimum two-year follow-up evaluation, patients completed the ASES and L'Insalata questionnaires and were asked to characterize the level of satisfaction with use of a visual analog scale from 0 to 10 (with 0 being highly unsatisfied and 10 being completely satisfied). They were also asked to identify any shoulder symptoms and any subsequent shoulder injuries or operations and to rate their ability to return to active participation in athletics at the previous level.
All patients underwent a targeted physical examination of the affected and contralateral shoulders before surgery in order to assess range of motion, strength, pain and tenderness, and stability as well as to identify the presence or absence of specific signs of labral injury, such as the active compression test. Forty-three of the forty-seven patients underwent an identical evaluation at a minimum of two years postoperatively. To limit bias, the preoperative and two-year postoperative physical examinations were performed by content experts (S.F.B. and J.E.V.) not involved in the care of the patients and not by the individual treating surgeons.
Operative Technique
At our institution, arthroscopic shoulder procedures are routinely performed with the patient under regional anesthesia with intravenous sedation. The patient is positioned in the modified beach-chair position with the involved extremity sterilely prepared and placed in an arm holder for positioning. An examination with the patient under anesthesia is carried out first to determine the passive range of motion in all planes and to identify any instability patterns.
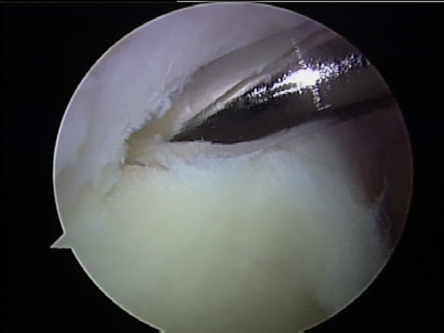
A standard posterior portal is created, and a diagnostic arthroscopic evaluation is carried out. An accessory anterior working portal is established high in the rotator interval region with use of a spinal needle for accurate placement. This portal is placed just anterior to the leading edge of the supraspinatus tendon, adjacent to the biceps tendon, allowing for an optimum angle of approach to the superior labrum for anchor placement and suture passage. An evaluation is then performed to confirm the presence of a type-II SLAP lesion and to characterize its extent in the anterior-posterior plane (Fig. 1-A). Once the diagnosis is confirmed, a 4.5-mm motorized shaver is used to débride the superior aspect of the glenoid at the tear margin to create a bleeding osseous surface for healing, with care being taken to avoid any additional injury to the labral tissue.
Fig. 1-A.
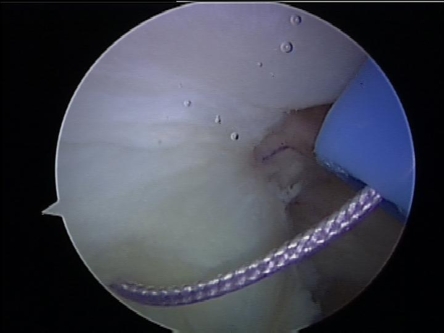
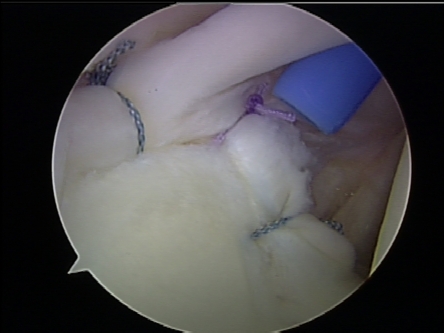
Figs. 1-A through 1-D Arthroscopic images illustrating SLAP repair in a right shoulder. Fig. 1-A Confirmation of a type-II SLAP lesion during diagnostic arthroscopy. Fig. 1-B Preparation of the superior glenoid rim to stimulate a healing response. Fig. 1-C Suture passage with use of the described technique. Fig. 1-D Arthroscopic knot-tying to complete a three-anchor repair.
We routinely perform arthroscopic SLAP lesion repair with use of one or more suture anchors, single-loaded with nonabsorbable suture. In this series, both bioabsorbable and metal anchors were employed; at the present time, we exclusively utilize bioabsorbable suture anchors. Anchor placement can be accomplished through the anterior working portal for all tears that do not have excessive posterior extension (i.e., not beyond the 10 o'clock position in a right shoulder). A guide is used to position the anchor at the articular margin at an angle of 45° to the osseous surface, and a drill is used to perforate the cortical bone before anchor placement (Fig. 1-B). In the case of a tear that extends further posteriorly, anchor placement and suture passage is performed with use of a second posterior portal. This portal is generally placed lateral to the standard posterior portal through the tendinous fibers or the myotendinous junction of the infraspinatus.
After successful anchor placement, sutures are passed in a simple configuration (in most cases) with use of a suture shuttling device or a spinal needle that is placed percutaneously with use of a Neviaser portal approach (Fig. 1-C). Fixation is then secured with use of arthroscopic knot-tying techniques. The type of knot that is utilized is surgeon-dependent, with constructs consisting of either one specialized sliding knot backed up with reversing half-hitches or a standard knot consisting of two half-hitches in the same direction followed by a minimum of four reversing half-hitches (Fig. 1-D). Nonabsorbable sutures are generally utilized, and knots are placed superiorly off of the articular surface with use of the passed suture as the post limb for tying. Anchor placement, suture passage, and knot-tying generally are performed for each point of fixation before moving on to the next point of fixation. In the present series, the number of anchors that were utilized ranged from one to four as determined by the tear configuration and the judgment of the individual surgeon.
Postoperative Management
A published institutional postoperative protocol after arthroscopic SLAP lesion repair22 was uniformly utilized by the surgeons who participated in the present series. Patients were placed in a sling and swathe in the operating room and wore the sling for the first four to six weeks postoperatively. Distal range-of-motion exercises involving the elbow, wrist, and hand were initiated immediately, with passive range of motion of the shoulder beginning during the first two weeks postoperatively. External rotation was limited to neutral for the first four weeks and then was gradually advanced to full; external rotation in abduction was prohibited for the first six weeks. Pain-free, submaximal deltoid isometric and periscapular strengthening exercises were initiated during the first four weeks, with active range of motion of the shoulder and strengthening of the rotator cuff beginning at approximately six weeks postoperatively. Functional exercises, proprioceptive training, plyometrics, and sports-specific rehabilitation were gradually instituted during the second, third, and fourth months.
Patients were allowed to resume athletic activities involving the upper extremities at a minimum of three months postoperatively, provided that they were pain-free and demonstrated a normal range of motion with strength and function approximating those of the contralateral extremity. Overhead throwers resumed athletics after completing a phased throwing program.
Statistical Methods
Registry data were collected and stored with use of an institution-approved, secure data-collection instrument. Continuous data were described with use of means, medians, and standard deviations. A critical p value of 0.05 was used to determine significance. Nonparametric statistical hypothesis tests were used to account for the distribution of continuous data being not normally distributed. The Wilcoxon signed-rank test was used to compare preoperative and postoperative variables, including the ASES and L'Insalata outcome scores and range-of-motion measurements. The Mann-Whitney U test was employed to compare subjective outcome scores and objective range-of-motion measurements between particular groups. A post hoc analysis indicated that the study was sufficiently powered to detect clinically relevant differences in all parameters except external rotation (for which it was powered to detect an 8° to 12° difference).
Source of Funding
Funding for the prospective database and for the present study was provided by an institutional fund; no external funding was utilized. Statistical analysis was supported in part by the Clinical and Translational Science Center Grant (NIH UL1RR024996) at Weill Cornell Medical College.
Results
Operative Findings
All patients had confirmation of a type-II SLAP tear on diagnostic arthroscopy according to defined criteria, including (1) gross visual evidence of a traumatic detachment of the superior labrum from the glenoid and (2) demonstration of instability of the detached portion as evidenced by traction on the biceps anchor with use of a probe and/or an arthroscopic peel-back test.
On the basis of these criteria, care was taken to differentiate between a pathologic detachment and a normal anatomic variant. The extent of the tear in the anterior-posterior plane was quantified in each patient with use of clock-face coordinates. Forty patients had a tear that extended from approximately the 11 o'clock position to the 1 o'clock position. Tears of this size were fixed with either one anchor (nine patients) or more commonly two anchors (thirty-one patients), with one anchor placed just anterior to and one placed directly posterior to the biceps attachment. In seven patients, the tear was noted to extend further anteriorly, posteriorly, or in both directions, requiring three anchors (five patients) or four anchors (two patients) for fixation. Bioabsorbable suture anchors were used in thirty-six of the forty-seven patients. In eleven patients, metal suture anchors were employed.
Subjective Outcomes
Preoperatively and at a minimum of two years postoperatively, all patients completed a series of questionnaires, including two validated measurements of shoulder function (the ASES shoulder index and the L'Insalata shoulder survey) as well as specific questions addressing shoulder symptomatology and the patient's level of satisfaction. These data are summarized in Table I. The median ASES score improved from 62 preoperatively to 97 at more than two years postoperatively (p < 0.05). The median L'Insalata rating improved from 65 preoperatively to 93 at more than two years postoperatively (p < 0.05). Forty-one patients (87%) subjectively rated the outcome as good or excellent, five rated it as fair, and one rated it as poor. Patients were asked to grade their level of satisfaction with the surgical outcome with use of a visual scale from 0 to 10 (with 0 being completely unsatisfied and 10 being completely satisfied); the median satisfaction rating for the entire cohort was 9 at more than two years postoperatively.
TABLE I.
Patient-Reported Subjective Outcomes
| Mean and Standard Deviation | Median | Minimum | Maximum | P Value† | |
|---|---|---|---|---|---|
| ASES score*(points) | <0.05 | ||||
| Preop. | 61.6 ± 17.09 | 62 | 18 | 95 | |
| Postop. | 92.55 ± 10.08 | 97 | 62 | 100 | |
| L'Insalata score (points) | <0.05 | ||||
| Preop. | 61.87 ± 12.95 | 65 | 38 | 88 | |
| Postop. | 90.23 ± 9.51 | 93 | 71 | 100 | |
| Satisfaction rating | 8.3 ± 1.89 | 9 | 2 | 10 | — |
ASES = American Shoulder and Elbow Surgeons.
Wilcoxon signed-rank test.
Objective Assessments
All patients underwent a standardized examination preoperatively. The examination consisted of an assessment of motion (forward elevation, external rotation in both adduction and 90° of abduction, and internal rotation) and tenderness, strength testing, instability testing, and the performance of a number of provocative maneuvers specific to the shoulder, including an active compression test. The active compression test was documented as being positive in forty-five patients (96%) during the preoperative evaluation. The active compression test was negative in forty-six of the forty-seven patients postoperatively. Forty-three patients underwent the same examination at a minimum of two years postoperatively, performed by an independent examiner (S.F.B.) for study purposes. Range-of-motion data, including preoperative and postoperative measurements for the involved extremity, are summarized in Table II. We noted a significant improvement in the mean and median values for forward elevation (p < 0.05) and external rotation at 90° of abduction (p < 0.05) in the involved extremity at the time of the postoperative evaluation.
TABLE II.
Range of Motion
| Mean and Standard Deviation | Median | Minimum | Maximum | P Value* | |
|---|---|---|---|---|---|
| Forward elevation (deg) | <0.05 | ||||
| Preop. | 172.13 ± 9.01 | 170 | 140 | 180 | |
| Postop. | 176.63 ± 4.33 | 180 | 170 | 180 | |
| External rotation (deg) | 0.496 | ||||
| Preop. | 73.62 ± 12.23 | 75 | 30 | 90 | |
| Postop. | 75.35 ± 12.88 | 80 | 45 | 100 | |
| Internal rotation† | 0.566 | ||||
| Preop. | 8.044 ± 3.17 | 7 | 4 | 17 | |
| Postop. | 7.66 ± 2.22 | 7 | 3 | 12 | |
| External rotation at 90° of abduction (deg) | <0.05 | ||||
| Preop. | 82.77 ± 18.05 | 90 | 15 | 110 | |
| Postop. | 96.43 ± 7.91 | 95 | 80 | 120 |
Wilcoxon signed-rank test.
Internal rotation measurements were based on the maximum thoracic level reached with the thumb.
Return to Sports
Preoperatively, thirty-four patients participated in athletics at a recreational level or higher. Twenty-five (74%) of these patients were able to return to their preinjury level of competition. The nine patients who were not able to resume their previous endeavors included one professional athlete, one collegiate athlete, and seven recreational participants. Of the twenty-eight patients who had participated in overhead athletics preoperatively, twenty (71%) were able to return to their preinjury level. This group included seven of eleven patients who played baseball, all five patients who played softball, four of eight tennis or squash players, five of five swimmers, and one of two volleyball players.
Analysis of Factors Potentially Influencing Outcome
While the cumulative subjective and objective outcomes in this patient cohort were encouraging, we sought to identify factors that may have influenced the outcome in either a positive or a negative way. A stratified statistical analysis was performed to evaluate the effect of seven variables on outcome: age (thirty years or younger as compared with more than thirty years), sex, sidedness (left or right), involvement of the dominant or nondominant extremity, tear size, the number of anchors utilized, and the use of metal as compared with bioabsorbable anchors for fixation. With use of the validated outcomes measures (the ASES and L'Insalata surveys), patient-reported satisfaction scores, and objective measurements of postoperative motion as the primary outcome parameters, we could not identify a significant impact of any of these factors on patient outcome with the numbers available.
Traumatic Compared with Atraumatic Etiology
There appeared to be two distinct populations of patients in this cohort: those who had a distinct traumatic injury that was thought to have initiated the symptoms and those who noted an insidious onset of shoulder symptoms. All of the patients in the atraumatic group were involved in athletics and presented with recalcitrant symptoms involving the dominant extremity (twenty) or the nondominant extremity (two) and participated in a vocation that utilized both upper extremities. With the numbers available, no significant differences were detected between these groups with regard to the median ASES score (92 compared with 93) or the median L'Insalata score (90 compared with 89) at more than two years postoperatively. However, the median postoperative patient satisfaction rating was significantly higher for the traumatic group as compared with the atraumatic group (9 compared with 7; p < 0.05). Among the athletes, the percentage of return to competition was 92% (eleven of twelve) in the traumatic group, compared with only 64% (fourteen of twenty-two) in the atraumatic group (p < 0.05).
Concomitant Pathology
While we intentionally excluded patients with coexistent rotator cuff tears that required a formal repair and those with concurrent glenohumeral instability, a number of patients in the present study were noted to have associated pathologic findings. On diagnostic arthroscopy, twenty-four of the forty-seven patients were found to have a partial rotator cuff injury that was treated with débridement only. A subacromial bursectomy was performed in thirty-three patients, and combined bursectomy and acromioplasty was performed in twenty-three patients. Four patients underwent a concomitant distal clavicular excision.
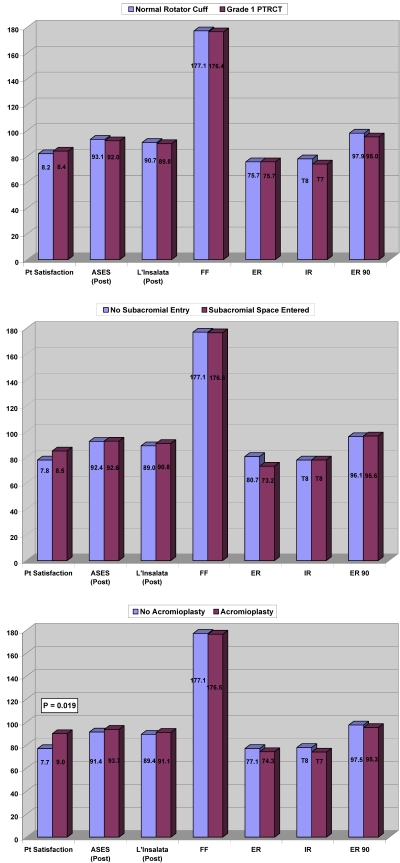
A comparative analysis was performed to identify what influence, if any, the presence of coexistent pathologic findings or the performance of a concurrent procedure had on the outcome parameters. As illustrated in Figure 2, both coexistent partial-thickness injury to the rotator cuff and concurrent subacromial bursectomy did not appear to have an effect (p > 0.05) on the outcome parameters measured. A concomitant acromioplasty had no significant effect on either the ASES score or the L'Insalata score or on range-of-motion measurements (p > 0.05); however, patients who underwent concomitant arthroscopic labral repair and acromioplasty were noted to have significantly higher patient-reported satisfaction values (9.0 compared with 7.7; p = 0.019).
Fig. 2.
Bar graphs illustrating the influence of coexistent pathology and concomitant procedures on outcome parameters. PTRCT = partial-thickness rotator cuff tear, Pt = patient, ASES = American Shoulder and Elbow Surgeons, FF = forward flexion, ER = external rotation, IR = internal rotation, ER 90 = external rotation at 90° of abduction, and post = postoperative.
Complications
There were five complications in the present study, two of which required a repeat surgical procedure. One patient, who initially presented with an atraumatic type-II SLAP tear, underwent arthroscopic repair with use of one anchor and was doing well postoperatively when he sustained a traumatic reinjury of the shoulder. He was diagnosed with a recurrent tear and underwent a repeat arthroscopic SLAP tear repair. He went on to have a successful outcome (ASES score, 98; L'Insalata score, 98; patient-reported satisfaction rating, 10).
Four patients experienced difficulty with severe, refractory postoperative stiffness (Table III). Three of those patients had initially presented with an isolated superior labral tear without a distinct traumatic injury. Those patients were all managed nonoperatively and eventually regained within 15° of the preinjury range of motion. The fourth patient had type-1 diabetes mellitus and had presented with a traumatic type-II SLAP tear. She was also noted to have a low-grade bursal-side injury of the rotator cuff. She underwent débridement of the rotator cuff lesion combined with subacromial decompression and acromioplasty. This patient had development of severe postoperative adhesive capsulitis that did not respond to nonoperative treatment. She then underwent arthroscopic lysis of adhesions and successfully regained full motion.
TABLE III.
Outcomes for Patients with Refractory Postoperative Stiffness
| ASES Score*(points)
|
L'Insalata Score (points)
|
Forward Elevation (deg)
|
External Rotation (deg)
|
Internal Rotation†(deg)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Preop. | Postop. | Preop. | Postop. | Score | Patient Satisfaction | Preop. | Postop. | Preop. | Postop. | Preop. | Postop. |
| 1 | 60 | 92 | 52 | 74 | Good | 7 | 180 | 180 | 60 | 65 | T8 | T12 |
| 2 | 78 | 80 | 71 | 76 | Fair | 2 | 180 | 180 | 70 | 65 | T6 | T10 |
| 3 | 60 | 100 | 52 | 97 | Good | 5 | 180 | 180 | 80 | 45 | T7 | T9 |
| 4 | 35 | 62 | 39 | 73 | Fair | 6 | 160 | 170 | 60 | 50 | T12 | T11 |
| Mean | 58.3 | 83.5 | 53.5 | 80.0 | — | 5.0 | 175 | 177.5 | 67.5 | 56.25 | T8 | T10.5 |
ASES = American Shoulder and Elbow Surgeons.
The values are expressed as the vertebral level that could be reached with the thumb of the patient.
Discussion
A survey of the literature after arthroscopic treatment of type-II SLAP lesions demonstrates an evolution in treatment. In a report on 140 superior labral injuries, Snyder et al. described the transition from treatment of the type-II lesions with débridement (in the first 56% of the patients) to repair with suture anchors in the remaining patients3. Morgan et al. retrospectively reviewed a series of 102 patients who were managed with arthroscopic repair of a type-II SLAP lesion with use of suture anchor fixation. They reported a 97% rate of good or excellent outcomes at one year after surgery4. Kim et al. retrospectively evaluated thirty-four patients who had been managed with arthroscopic suture anchor repair and noted satisfactory outcomes according to the University of California at Los Angeles (UCLA) shoulder score in 94% of the patients13. Recently, Enad et al. reported favorable clinical results (a good or excellent outcome in twenty-four of twenty-seven patients) and a high rate of return to full duty in a series of military patients who had been managed with arthroscopic suture anchor repair of type-II superior labral injuries23.
The current study represents the first\ prospective series, to our knowledge, documenting outcomes after arthroscopic SLAP lesion repair with use of a “modern” technique of arthroscopic suture anchor stabilization. The outcomes presented here are comparable with those of previous studies. At an average of 2.7 years postoperatively, we noted median ASES and L'Insalata scores of 97 and 93, respectively, and 87% of the patients had a good or excellent outcome.
Despite high levels of subjective and objective improvement, overall only 74% of the patients in the present series were able to resume athletics at the preinjury level. This overall proportion, again, is quite consistent with the literature4,5,16-18. For comparison, Ide et al. retrospectively evaluated a cohort of forty athletes who were managed with arthroscopic superior labral repair with use of suture anchor fixation and reported a 75% rate of return to the preinjury level of competition24. There appeared to be two distinct cohorts of patients in the present series: those with a traumatic injury of the shoulder and those in whom a superior labral injury likely developed because of a recurrent overuse mechanism. While the final outcome scores and objective measurements did not differ significantly between the two groups, the patient-reported satisfaction rating was significantly higher for those with a traumatic etiology. We hypothesize that the overuse group had higher demands and that, in those patients, a diminished ability to return to premorbid levels of athletic activity was reflected in a poorer rating of satisfaction. In fact, when patients in the overuse group were asked to substantiate their rating in a follow-up question, three patients specifically stated that they were quite satisfied with the postoperative level of shoulder function for daily activities but were dissatisfied overall because of their failure to return to the preinjury level of athletic competition.
A small number of patients in the present series had complications, the most common being prolonged postoperative stiffness (noted in four patients). The most refractory case occurred in a patient with diabetes, which may have contributed to this complication. In two of the remaining three cases, a delay in the early phases of postoperative rehabilitation was thought to have contributed to the stiffness. While the outcomes for these patients were poorer (mean ASES and L'Insalata scores of 83.5 and 80.0, respectively) when compared with those for the entire cohort, none of the four patients were considered to have had a failure, with two good and two fair outcomes. Residual motion deficits at the time of the latest follow-up were most pronounced in external rotation with the arm at the side and in internal rotation.
The present study had a number of positive attributes, specifically with regard to the study design. The data were collected in a prospective fashion. Patients were managed with a standardized operative approach performed by multiple surgeons at one institution. The rate of clinical follow-up was satisfactory for a patient cohort of this type. We evaluated patients with use of two validated outcomes measurements specific to shoulder disorders, and the patients were examined by an independent examiner at the time of the minimum two-year follow-up evaluation.
We acknowledge that our study does have some limitations. Although it was a prospective study, a power analysis was not performed prospectively, and thus the statistical analysis relied on a post hoc power analysis. While the overall outcomes were favorable, we did not have a control or a comparison group. While some authors have recently advocated alternative approaches such as biceps tenodesis for the treatment of superior labral detachments25,26, specifically those in older patients with concomitant shoulder problems, we are of the consensus that the appropriate treatment for a type-II SLAP lesion in the young athletic population is arthroscopic suture anchor repair with restoration of the anatomy as described. We do not generally perform arthroscopic SLAP lesion repair in patients over the age of fifty years because of an unacceptably high rate of complications and the infrequent occurrence of true superior labral tears in this group of patients.
Another criticism of the present study is the potential variation introduced by including patients managed by multiple surgeons, specifically with regard to diagnostic criteria, operative technique, and postoperative treatment. While this is a valid concern, the surgeons who participated in the present study all employed a similar approach clinically and technically for the treatment of this particular injury. With regard to fixation devices, metal anchors were employed more frequently early in the study, demonstrating a shift from metal to bioabsorbable implants by all of the participating surgeons during this time period.
A final potential criticism of the present study is the inclusion of a subset of patients with coexistent pathology (“low-grade” partial-thickness rotator cuff tears) and/or concurrent procedures (such as bursectomy or acromioplasty), which could add some inconsistency to the outcomes. We believed that this approach could be justified on the basis of a number of points. First, there is an unusually high frequency of associated pathology encountered in the treatment of patients with superior labral injuries3,6,10,19,23,24. Snyder et al. reported a 72% rate of combined lesions in their large series of SLAP lesions, with the most common being impingement syndrome followed by partial-thickness rotator cuff tears3. By study design, we prospectively selected patients for enrollment on the basis of a primary diagnosis of a type-II SLAP tear as indicated clinically and confirmed at the time of surgery. Any associated pathologic finding was deemed to be potentially contributory to this primary diagnosis. We intentionally excluded patients with concomitant problems, such as anterior instability or a large or repairable rotator cuff tear, that could have potentially altered the postoperative rehabilitation protocol or were highly likely to affect the clinical outcome.
In conclusion, arthroscopic treatment of superior labral lesions has evolved. Coexistent pathology is common and should be addressed at the time of arthroscopic repair. On the basis of our findings, favorable clinical outcomes can be anticipated in the majority of patients after arthroscopic SLAP lesion repair. Overall, approximately three of four patients will be able to successfully return to the previous level of athletic ability. However, patients with a distinct traumatic etiology have a higher level of satisfaction with regard to their outcome, which is likely due to their substantially greater likelihood of a successful return to competition. 
Acknowledgments
Note: The authors thank Alana Burns, Kathryn Fong, and Pamela Sanchez, MPH, for their important contributions to this study. They also thank Joseph T. Nguyen, MPH, and Dr. Stephen Lyman for their assistance with statistical analysis. Statistical analysis was supported in part by the Clinical and Translational Science Center Grant (NIH UL1RR024996) at Weill Cornell Medical College.
Disclosure: The authors did not receive any outside funding or grants in support of their research for or preparation of this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which the authors, or a member of their immediate families, are affiliated or associated. Institutional support was supplied only for statistical analysis in part by the Clinical and Translational Science Center Grant (NIH UL1RR024996) at Weill Cornell Medical College.
A video supplement related to the subject of this article has been developed by the American Academy of Orthopaedic Surgeons and JBJS and is available for viewing in the video library of the JBJS website, www.jbjs.org. To obtain a copy of the video, contact the AAOS at 800-626-6726 or go to their website, www.aaos.org.
Investigation performed at the Hospital for Special Surgery, New York, NY
References
- 1.Andrews JR, Carson WG Jr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13:337-41. [DOI] [PubMed] [Google Scholar]
- 2.Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274-9. [DOI] [PubMed] [Google Scholar]
- 3.Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4:243-8. [DOI] [PubMed] [Google Scholar]
- 4.Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy. 1998;14:553-65. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart SS, Morgan C. SLAP lesions in the overhead athlete. Orthop Clin North Am. 2001;32:431-41, viii. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes. The “dead arm” revisited. Clin Sports Med. 2000;19:125-58. [DOI] [PubMed] [Google Scholar]
- 7.O'Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med. 1998;26:610-3. [DOI] [PubMed] [Google Scholar]
- 8.Altchek DW, Warren RF, Wickiewicz TL, Ortiz G. Arthroscopic labral debridement: a three-year follow-up study. Am J Sports Med. 1992;20:702-6. [DOI] [PubMed] [Google Scholar]
- 9.Cordasco FA, Steinmann S, Flatow EL, Bigliani LU. Arthroscopic treatment of glenoid labral tears. Am J Sports Med. 1993;21:425-31. [DOI] [PubMed] [Google Scholar]
- 10.Field LD, Savoie FH. Arthroscopic suture repair of superior labral detachment lesions of the shoulder. Am J Sports Med. 1993;21:783-90. [DOI] [PubMed] [Google Scholar]
- 11.Pagnani MJ, Speer KP, Altchek DW, Warren RF, Dines DM. Arthroscopic fixation of superior labral lesions using a biodegradable implant: a preliminary report. Arthroscopy. 1995;11:194-8. [DOI] [PubMed] [Google Scholar]
- 12.Samani JE, Marston SB, Buss DD. Arthroscopic stabilization of type II SLAP lesions using an absorbable tack. Arthroscopy. 2001;17:19-24. [DOI] [PubMed] [Google Scholar]
- 13.Kim SH, Ha KI, Kim SH, Choi HJ. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84:981-5. [DOI] [PubMed] [Google Scholar]
- 14.O'Brien SJ, Allen AA, Coleman SH, Drakos MC. The trans-rotator cuff approach to SLAP lesions: technical aspects for repair and a clinical follow-up of 31 patients at a minimum of 2 years. Arthroscopy. 2002;18:372-7. [DOI] [PubMed] [Google Scholar]
- 15.Yian E, Wang C, Millett PJ, Warner JJ. Arthroscopic repair of SLAP lesions with a Bioknotless suture anchor. Arthroscopy. 2004;20:547-51. [DOI] [PubMed] [Google Scholar]
- 16.Rhee YG, Lee DH, Lim CT. Unstable isolated SLAP lesion: clinical presentation and outcome of arthroscopic fixation. Arthroscopy. 2005;21:1099. [DOI] [PubMed] [Google Scholar]
- 17.Paxinos A, Walton J, Rutten S, Muller M, Murrell GA. Arthroscopic stabilization of superior labral (SLAP) tears with biodegradable tack: outcomes to 2 years. Arthroscopy. 2006;22:627-34. [DOI] [PubMed] [Google Scholar]
- 18.Cohen DB, Coleman S, Drakos MC, Allen AA, O'Brien SJ, Altchek DW, Warren RF. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy. 2006;22:136-42. [DOI] [PubMed] [Google Scholar]
- 19.Coleman SH, Cohen DB, Drakos MC, Allen AA, Williams RJ, O'Brien SJ, Altchek DW, Warren RF. Arthroscopic repair of type II superior labral anterior posterior lesions with and without acromioplasty: a clinical analysis of 50 patients. Am J Sports Med. 2007;35:749-53. [DOI] [PubMed] [Google Scholar]
- 20.Burkart A, Imhoff AB, Roscher E. Foreign-body reaction to the bioabsorbable Suretac device. Arthroscopy. 2000;16:91-5. [DOI] [PubMed] [Google Scholar]
- 21.Sassmannshausen G, Sukay M, Mair SD. Broken or dislodged poly-L-lactic acid bioabsorbable tacks in patients after SLAP lesion surgery. Arthroscopy. 2006;22:615-9. [DOI] [PubMed] [Google Scholar]
- 22.Levinson M. Superior labrum anterior to posterior (SLAP) repair. In: Cioppa-Mosca J, Cahill JB, Cavanaugh JT, Corradi-Scalise D, Rudnick H, Wolff A; Hospital for Special Surgery, Department of Rehabilitation. Handbook of postsurgical rehabilitation guidelines for the orthopedic clinician. St. Louis: Mosby; 2008. p 416-22.
- 23.Enad JG, Gaines RJ, White SM, Kurtz CA. Arthroscopic superior labrum anterior-posterior repair in military patients. J Shoulder Elbow Surg. 2007;16:300-5. [DOI] [PubMed] [Google Scholar]
- 24.Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33:507-14. [DOI] [PubMed] [Google Scholar]
- 25.Franceschi F, Longo UG, Ruzzini L, Rizzello G, Maffulli N, Denaro V. No advantages in repairing a type II superior labrum anterior and posterior (SLAP) lesion when associated with rotator cuff repair in patients over age 50: a randomized controlled trial. Am J Sports Med. 2008;36:247-53. [DOI] [PubMed] [Google Scholar]
- 26.Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37:929-36. [DOI] [PubMed] [Google Scholar]