Abstract
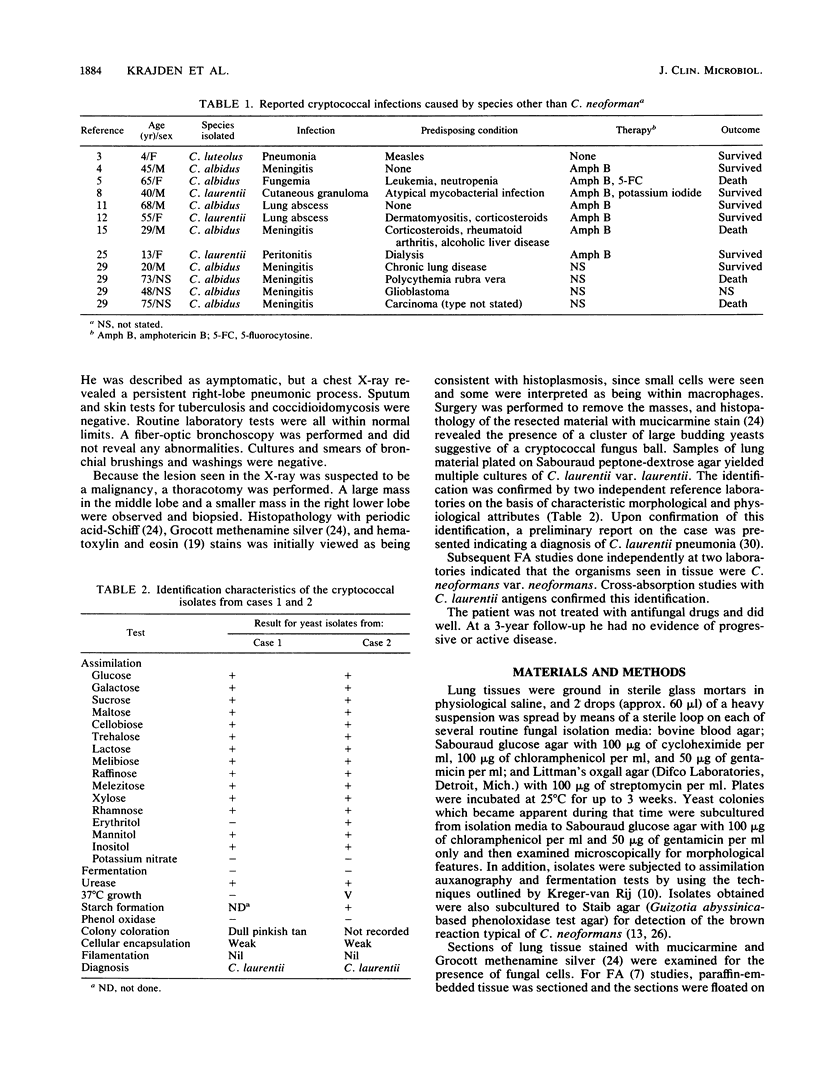
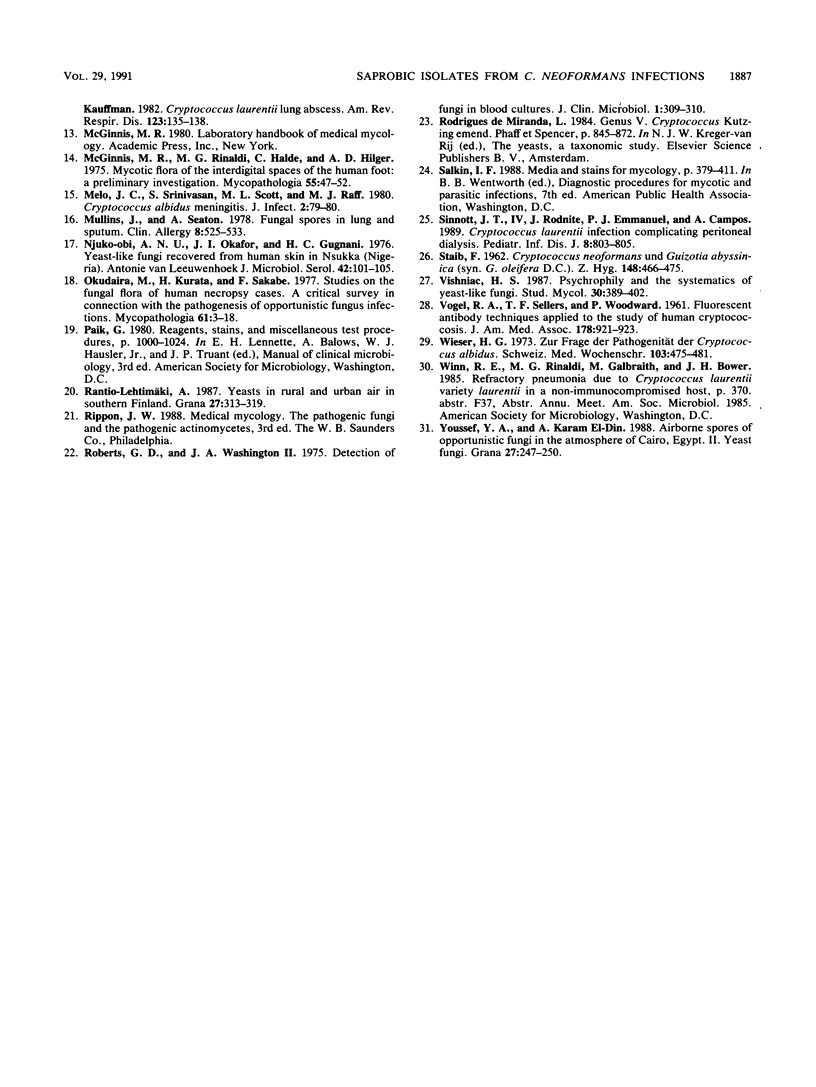
We report two cases in which Cryptococcus laurentii was isolated from surgically resected pulmonary lesions but the cryptococcal cells is tissue reacted positively with a specific fluorescent antibody (FA) conjugate for Cryptococcus neoformans. Both patients had no apparent host defense defects. In both cases, multiple cryptococcal isolates were obtained from tissue, and yeastlike cells consistent with C. neoformans were seen in direct histology. The isolates were identified by assimilation patterns and standard procedures including phenoloxidase reactions. Since C. laurentii was consistently isolated by using stringent procedures, it was considered unlikely that the fungus represented surgical or laboratory contamination. Its presence may be the result of dual infection not detected by FA, but other possible explanations exist. The results show the value of the FA test in diagnostic mycology and call into question previous reports of cryptococci other than C. neoformans as agents of infection.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BINDER L., CSILLAG A., TOTH G. Diffuse infiltration of the lungs associated with Cryptocococcus luteolus. Lancet. 1956 Jun 30;270(6931):1043–1045. doi: 10.1016/s0140-6736(56)90804-2. [DOI] [PubMed] [Google Scholar]
- Bille J., Stockman L., Roberts G. D. Detection of yeasts and filamentous fungi in blood cultures during a 10-year period (1972 to 1981). J Clin Microbiol. 1982 Nov;16(5):968–970. doi: 10.1128/jcm.16.5.968-970.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluck J. L., Myers J. P., Pass L. M. Cryptococcemia due to Cryptococcus albidus. South Med J. 1987 Apr;80(4):511–513. doi: 10.1097/00007611-198704000-00024. [DOI] [PubMed] [Google Scholar]
- Gordon M. A., Lapa E. W. Adherence of digested tissue sections for fungal immunofluorescence. Mycopathologia. 1984 Dec 30;88(2-3):181–184. doi: 10.1007/BF00436451. [DOI] [PubMed] [Google Scholar]
- Gordon M. A. Pulmonary cryptococcosis. A case due to Cryptococcus albidus. Am Rev Respir Dis. 1972 Nov;106(5):786–787. doi: 10.1164/arrd.1972.106.5.786b. [DOI] [PubMed] [Google Scholar]
- Kamalam A., Yesudian P., Thambiah A. S. Cutaneous infection by Cryptococcus laurentii. Br J Dermatol. 1977 Aug;97(2):221–223. doi: 10.1111/j.1365-2133.1977.tb15070.x. [DOI] [PubMed] [Google Scholar]
- Khardori N. Host-parasite interaction in fungal infections. Eur J Clin Microbiol Infect Dis. 1989 Apr;8(4):331–351. doi: 10.1007/BF01963468. [DOI] [PubMed] [Google Scholar]
- Krumholz R. A. Pulmonary cryptococcosis. A case due to Cryptococcus albidus. Am Rev Respir Dis. 1972 Mar;105(3):421–424. doi: 10.1164/arrd.1972.105.3.421. [DOI] [PubMed] [Google Scholar]
- Lynch J. P., 3rd, Schaberg D. R., Kissner D. G., Kauffman C. A. Cryptococcus laurentii lung abscess. Am Rev Respir Dis. 1981 Jan;123(1):135–138. doi: 10.1164/arrd.1981.123.1.135. [DOI] [PubMed] [Google Scholar]
- McGinnis M. R., Rinaldi M. G., Halde C., Hilger A. E. Mycotic flora of the interdigital spaces of the human foot: a preliminary investigation. Mycopathologia. 1975 Feb 28;55(1):47–52. doi: 10.1007/BF00467091. [DOI] [PubMed] [Google Scholar]
- Melo J. C., Srinivasan S., Scott M. L., Raff M. J. Cryptococcus albidus meningitis. J Infect. 1980 Mar;2(1):79–82. doi: 10.1016/s0163-4453(80)91865-4. [DOI] [PubMed] [Google Scholar]
- Mullins J., Seaton A. Fungal spores in lung and sputum. Clin Allergy. 1978 Sep;8(5):525–533. doi: 10.1111/j.1365-2222.1978.tb01506.x. [DOI] [PubMed] [Google Scholar]
- Njoku-Obi A. N., Okafor J. I., Gugnani H. C. Yeast-like fungi recovered from normal human skin in Nsukka (Nigeria). Antonie Van Leeuwenhoek. 1976;42(1-2):101–105. doi: 10.1007/BF00399453. [DOI] [PubMed] [Google Scholar]
- Okudaira M., Kurata H., Sakabe F. Studies on the fungal flora in the lung of human necropsy cases. A critical survey in connection with the pathogenesis of opportunistic fungus infections. Mycopathologia. 1977 Jul 29;61(1):3–18. doi: 10.1007/BF00440753. [DOI] [PubMed] [Google Scholar]
- Roberts G. D., Washington J. A., 2nd Detection of fungi in blood cultures. J Clin Microbiol. 1975 Mar;1(3):309–310. doi: 10.1128/jcm.1.3.309-310.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinnott J. T., 4th, Rodnite J., Emmanuel P. J., Campos A. Cryptococcus laurentii infection complicating peritoneal dialysis. Pediatr Infect Dis J. 1989 Nov;8(11):803–805. doi: 10.1097/00006454-198911000-00017. [DOI] [PubMed] [Google Scholar]
- VOGEL R. A., SELLERS T. F., Jr, WOODWARD P. Fluorescent antibody techniques applied to the study of human cryptococcosis. JAMA. 1961 Dec 2;178:921–923. doi: 10.1001/jama.1961.73040480010008d. [DOI] [PubMed] [Google Scholar]
- Wieser H. G. Zur Frage der Pathogenität des Cryptococcus albidus. Schweiz Med Wochenschr. 1973 Mar 31;103(13):475–481. [PubMed] [Google Scholar]
- da Cunha T., Lusins J. Cryptococcus albidus meningitis. South Med J. 1973 Nov;66(11):1230–passim. doi: 10.1097/00007611-197311000-00006. [DOI] [PubMed] [Google Scholar]



