Abstract
Background
Young patients with anxiety disorders are thought to have a hypersensitive fear system, including alterations of the early sensorimotor processing of threatening information. However, there is equivocal support in auditory blink response studies for an enlarged auditory startle reflex (ASR) in such patients. We sought to investigate the ASR measured over multiple muscles (whole-body) in children and adolescents with anxiety disorders.
Methods
Between August and December 2006, we assessed ASRs (elicited by 8 consecutive tones of 104 dB, interstimulus interval of about 2 min) in 25 patients and 25 matched controls using a case–control design and in 9 nonaffected siblings. We recorded the electromyographic activity of 6 muscles and the sympathetic skin response. We investigated response occurrence (probability %) and response magnitude (area under the curve in μV × ms) of the combined response of 6 muscles and of the single blink response.
Results
In patients (17 girls, mean age 12 years; 13 social phobia, 9 generalized anxiety, 3 other), the combined response probability (p = 0.027) of all muscles, the combined area under the curve of all muscles (p = 0.011) and the sympathetic skin response (p = 0.006) were enlarged compared with matched controls. The response probability (p = 0.48) and area under the curve (p = 0.07) of the blink response were normal in patients compared with controls. The ASR pattern was normal with normal latencies in patients compared with controls. In nonaffected siblings, the sympathetic skin response (p = 0.038), but not the combined response probability of all muscles (p = 0.15), was enlarged compared with controls.
Limitations
Limitations are the sample size and restricted comparison to the psychophysiological ASR paradigm.
Conclusion
The results point toward a hypersensitive central nervous system (fear system), including early sensorimotor processing alterations and autonomic hyperreactivity. The multiple muscle (whole-body) ASR is suggested to be a better tool to detect ASR abnormalities in patients with anxiety disorders than the blink response alone. Abnormalities in ASR serve as a candidate endophenotype of anxiety disorders.
Introduction
A growing body of evidence supports the hypothesis that young patients with anxiety disorders have a highly sensitive fear system.1,2 Abnormalities of fear circuit activation, function of the hypothalamus–pituitary–adrenal axis and autonomic nervous system reactivity have been found.3–17 More specifically, patients with anxiety disorders are thought to experience altered early sensorimotor processing of threatening information.2,18 One of the quickest reactions of the fear system to a suddenly imposed sensory stimulus is the auditory startle reflex (ASR).19–21 The ASR consists of the contraction of several muscles throughout the body and subsequent autonomic changes.21,22 Animal studies showed that this primitive defensive reflex is generated by the caudal brainstem23 and modulated by the amygdala.24 The amygdala is believed to play a key role in emotional processing and pathological anxiety.18,25
There is evidence of an association between anxiety disorders and an enlarged ASR.26–28 However, the results are equivocal, both with regard to posttraumatic stress disorder and other anxiety disorders in adults.29 Findings in children with anxiety disorders range from attenuated to normal ASRs in posttraumatic stress disorder30,31 to normal ASRs in other anxiety disorders.32 It is possible that methodological issues underlie some of the inconsistent findings on the ASR in patients with anxiety disorders. In animals, the ASR is quantified by the electromyographic (EMG) measurement of the whole-body flinch or jump, involving multiple muscles.24,33 In contrast, in human research, the ASR is often electromyographically measured over a single muscle, the orbicularis oculi (blink response).34,35 However, there are indications that the blink response of the ASR is different from the ASR as it occurs in the whole body. First, the auditory blink response and the ASR measured over multiple muscles show different habituation patterns in both adults36–40 and children.41 Second, the auditory blink response and a combined multiple muscles ASR show different abnormalities in several neurologic disorders.42–46 Third, the auditory blink response consists of 2 EMG responses that differ in size and latency.36,47,48 The first is considered to be an eye-protective reflex on its own, whereas the second is part of the ASR.36,49,50 As the 2 responses extensively overlap, it is almost impossible to distinguish them.47,51 Together, these findings support the idea that the blink response does not fully represent the ASR.36 For these reasons, measuring the generalized ASR or the “whole-body ASR” in the form of a multiple-muscle EMG is considered to be more valid and appropriate than the single blink response in quantifying the ASR.36,40,50,52–54
Our aim was to investigate an alternative ASR quantification to that used in blink response studies, the multiple-muscle ASR, in young patients with anxiety disorders. Furthermore, we compared the multiple-muscle ASR, a method routinely used in the neurophysiological literature,39,55 with the blink response, a method routinely used in the psycho-physiologic literature.34 We investigated the following ASR parameters using a case–control design:
the combined response probability (%) of 6 differentially located muscles and the combined EMG area under the curve (μV × ms) of these responses,39
response probability (%) and EMG area under the curve (μV × ms) of the blink response, and34
the sympathetic skin response (the maximal change in μV inside the hand following stimulation, standardized to the intra-individual maximum).56–58
We used the sympathetic skin response to assess the “orienting response,”59 which includes autonomic changes occurring with a latency of longer than 500 ms after an auditory stimulus.21,22 In addition, we studied basic ASR characteristics such as latencies and startle patterns,60 and we assessed the multiple muscle ASR response probability and sympathetic skin response in a small group of siblings of patients with anxiety disorders. We hypothesized that the multiple-muscle ASR and sympathetic skin response would be abnormal in patients compared with controls and that the pattern of the blink response and multiple muscle ASR would be incongruent in patients compared with controls.42–46
Methods
Participants
We approached all patients who were referred to the out-patient clinic of the Child and Adolescent Psychiatry Department of the Academic Medical Center between August and November 2006 and met our inclusion criteria for the study. Inclusion criteria for participation were at least one primary diagnosis of an anxiety disorder and age between 8 and 17 years. One of us (M.J.B.) determined whether the patients had anxiety disorders. Further, the patients were screened for comorbid major depression disorders; comorbid major depression was an exclusion criterion, as the ASR can be reduced in these patients.61 Subsequently, we invited the patients to participate in the study. We excluded patients if they took medication; had a hearing defect; or met criteria for major depressive disorder, neurologic disorder, mental retardation, schizophrenia or other psychotic disorders. We also included a small group of siblings of the patients participating in the study. The siblings did not meet the criteria of a DSM-IV anxiety disorder according to the Anxiety Disorders Interview Schedule (ADIS).62 We invited healthy controls matched for age and sex to participate in the study. We excluded controls if they met criteria for psychopathology, had hearing defects or neurologic disorders. All participants were nonsmokers and we asked them to refrain from caffeinated beverages on the day of testing. The Institutional Board of the Academic Medical Center, Amsterdam, reviewed and approved the study protocol and participant consent forms.
Psychiatric assessment
We used the ADIS62 to formally identify and exclude anxiety disorders in all participants. The ADIS is a semistructured interview based on DSM-IV classification of psychopathology63 and includes both a child and a parent interview (ADIS-C/P). It was translated to Dutch by Siebelink and Treffers, and Dutch norms of the ADIS are available.64
Stimulation
Experimental stimuli consisted of 8 consecutive 104 dB (A) (sound-pressure level), 50 ms, 2000 Hz pure tones with instantaneous rise and fall times.34 Following a digital trigger, we generated the tones using an audio stimulator (Audio ACB 1; Walter Messelektronik) and presented them binaurally through stereo headphones (Vario 4000 S; Optac). The triggers of auditory stimuli were stored in the computer synchronously with the EMG data. We presented the stimuli with varying time intervals (1.5–2.5 min),55,65 which were similar for all participants.
Data collection
We recorded physiologic data, consisting of bipolar left orbicularis oculi, masseter, sternocleidomastoid, deltoid, abductor pollicis brevis, quadriceps EMG and sympathetic skin response measures, using Biosemi’s Active System (www.biosemi.nl). After skin preparation (Nuprep abrasive gel, Weaver and Company), we filled the cutaneous silver-silver chloride flat (11 mm width, 17 mm length, 4.5 mm height) active surface electrodes (equipped with preamplifiers to improve the signal:noise ratio and reduce the movement artifact) with conductive paste (Ten20 conductive, Weaver and Company). We attached the electrodes (excluding those for sympathetic skin response) 2 cm apart using adhesive collars in accordance with recommendations by the Psychophysiology Committee.34 Of the electrodes attached to the orbicularis oculi muscle, we placed one straight below the eye and the other 2 cm toward the ear and slightly higher. We checked the impedance of the electrodes (< 10 kΩ) before recording. We recorded the sympathetic skin response from the palm of the hands with the reference electrode on the dorsum of the hands.57,66 We placed the isolated ground electrode on the temple. The signal was analogue filtered high-pass (first order; −3 dB at 0.16 Hz) and low-pass (5th order antialiasing; −3 dB at 3 500 Hz). We continuously digitized filtered data with a sample frequency of 16 384 Hz per channel using a 24-bit A/D converter.
Procedure
We tested most participants in the afternoon, usually between 4 pm and 6 pm; we tested 3 controls and 1 patient with anxiety disorder in the morning on the weekend. Participants sat on a bed (with backrest) in an upright position; we asked them to sit quietly and relaxed. We gave them the following instructions: “Shortly you are going to hear a series of sounds. Please sit quietly and listen to the sounds as they come. Keep your eyes open during the entire procedure, which will last about 15 minutes.” Subsequently, we placed the headphones and began the stimulation procedure. The preparation took 30 minutes and the experiment lasted 15 minutes.
Data processing
We performed offline data analysis with Brain Vision Analyzer version 1.05 (Brain Products). We digitally filtered orbicularis oculi signals at 100 Hz high-pass 12 dB/oct to minimize DC offsets and slow eye drifts.67–69 The cut-off frequency of the high-pass filtering of the other muscles was 20 Hz.70 Owing to the high sample rate employed (16 384 Hz), the low-pass analogue filter could be chosen at 3 500 Hz. We converted the 14 raw unipolar signals into 7 pairs of bipolar derivations. We segmented all 7 channels into parts of 1 000 ms after the stimulus. We applied baseline correction using the mean of the 0–20 ms time interval. Subsequently, the signals were rectified. We placed markers manually using the Brain Vision Analyzer software and we processed the EMG using MATLAB 7.1 software (MathWorks).
We used several parameters to quantify the magnitude of the ASR. For the multiple-muscle ASR, we used the combined response probability (%) of all muscles and the combined area under the curve (μV × ms) of the responses of all muscles. For the blink response, we used the response probability (%) of the blink response in the single orbicularis oculi muscle and the area under the curve of the blink response (definitions of all ASR parameters are provided in the next paragraphs). We considered the first parameter, the multiple-muscle ASR response probability, to be the primary motor ASR parameter; therefore, we obtained only this parameter and the sympathetic skin response in the siblings. We included the blink response in this study to compare this parameter to the multiple-muscle ASR.
The response probability represents the chance (%) that a certain muscle responds following stimulation.55 We defined the combined response probability of all muscles as the average of the response probabilities (expressed in % chance of a muscle response following stimulation) of the 6 muscles.55 We defined the response probability of the orbicularis oculi response as the chance (%) of the occurrence of an orbicularis oculi response following stimulation. One of us (M.J.B.) visually inspected the EMG activity of all muscles after stimulation with Brain Vision Analyzer to determine which trials could be considered to be valid responses. We scored a response in any of the 6 simultaneously recorded muscles if an increase in EMG activity from baseline occurred.20,21,36 Scoring of these responses was based on the following rules (defined before scoring). We defined a response as a clear increase (duration of increase at least 30 ms, magnitude response at least 30 μV) from baseline. We marked the response onset (20–200 ms following stimulation) at the baseline (at the start of the μV increase). The same investigator scored all responses at the same screen sensitivity (200 μV on the screen, 100 μV below baseline and 100 μV above baseline).
We determined the response probability of the individual muscles by counting the occurrence of these responses, dividing this value by the total number of recorded traces and multiplying the results by 100. We defined latency as the start of the response at the EMG baseline. One of us (M.J.B.) manually marked response onset (latencies) and offset. We marked trials considered as artifacts (e.g., heart beat, loose electrodes) as such and we did not include them in our analysis.
The area under the curve parameters represent the magnitude (expressed in μV × ms) of the scored responses and the quantification of the EMG signal between response onset and offset. Quantification of the EMG burst in area under the curve (rectified integrated signal) is the most direct translation of the raw EMG into measurement units and a commonly used ASR quantification method.34,55 We conformed to the psychophysiology guidelines for human startle eye blink EMG studies.34 In line with Blumenthal and colleagues,34 we did not try to remove the early auditory protective reflex component of the orbicularis oculi area under the curve EMG response.44 Furthermore, we included only the EMG area under the curves of the trials considered to be valid responses in the analysis. For the orbicularis oculi muscle, we included responses with onset latencies between 20 and 100 ms in the analysis.34 For the other muscles, onset latencies were between 20 and 200 ms. We defined the combined area under the curve as the summated log-transformed EMG area under the curve of the 6 muscles.55 We performed a log-transformation to normalize the area under the curve values of the different muscles.
Although we scored responses conforming to the rules we defined, we could not totally rule out investigator bias as it was logistically impossible to keep the investigator completely blind to group membership. Therefore, we also analyzed parameters using fixed time intervals (peak amplitude and area under the curve between 20 and 200 ms following stimulation in all EMG trials). We identified the peak amplitude (μV) of the smoothed (with a 40-Hz low-pass filter34) EMG trials using software between 20 and 200 ms following stimulation, and we averaged these amplitudes per muscle. To obtain the area under the curve of the 20–200 ms time interval, we did not smoothe the EMG trials, but we removed background noise (estimated at 3 times the median of the interval 500–1000 ms following stimulation).67 For both parameters, we obtained the combined response by summing the log-transformed values of all 6 muscles.
Finally, we assessed the autonomic sympathetic skin response (left hand). The sympathetic skin response, comparable to the skin conductance response,71 is an easy test to analyze the sympathetic nervous system function.57,66,72 Any arousal stimulus (i.e., a stimulus that is perceived to be novel, surprising, intense, significant or emotional),73 can be used to activate sympathetic sudomotor nerve fibres and thereby change skin resistance.66 With repetitive auditory stimuli, the sympathetic skin response decreases.57,74 The sympathetic skin response is usually recorded from the palm of the hands, with the reference electrode on the dorsum of the hands.57,66 We defined the baseline as the mean μV 0–900 ms following stimulation (this could be chosen following the stimulus because the onset of the hand sympathetic skin response is 1500 ms following stimulation).75,76 Subsequently, we identified the peak μV during the interval 900–4 000 ms following stimulation by software. We defined the sympathetic skin response as the difference in μV between the baseline and the identified maximum, standardized to the intraindividual maximum (thus giving values ranging from 0% to 100%). It is recommended to standardize the sympathetic skin response intraindividually because it is highly variable.56,77 The intra-individual maximum often was the response following the first stimulus, but not always. We visually inspected the sympathetic skin responses to exclude movement artifacts or artifacts caused by loose electrodes.
Statistical analysis
We performed statistical analyses using SPSS version 15.0 (SPSS Inc.). We performed a power analysis based on a previous study in which ASR latency abnormalities were found.60 With a mean orbicularis oculi latency of 28 and a standard deviation (SD) of 8, a minimum of 20 participants per group is needed for 80% power to detect a clinically relevant change of 25% and a statistical significance of 5%. We used a linear mixed-model analysis (type III tests of fixed effects) to test group differences in parameters over the repeatedly presented stimuli. We performed the analyses under the assumption of compound symmetry for the covariance structure, which is equivalent to the classical approach to repeated-measures analysis of variance (ANOVA). In some parameters, adjustments to the denominator degrees of freedom were needed (e.g., area under the curve of the blink response because only the area under the curves of the responses were included, sympathetic skin response and fixed time interval parameters because of missing values). The response probability parameters revealed a Poisson distribution. We log-transformed area under the curve parameters to reduce skewness of the data and to standardize the area under the curve values of the different muscles (different in size and strength). We then summed them in the combined area under the curve calculation. As the latency distributions were not normally distributed, we performed Wilcoxon and Mann–Whitney tests to assess group differences in latency. We performed a Student t test to assess general characteristics. We considered p ≤ 0.05 to be significant in all tests.
Results
Participants
Of the 28 patients we invited to participate in the study, 3 refused. Nine siblings of the 25 patients enrolled in the study also agreed to participate (8 patients had no siblings aged 8–17 years, 4 siblings refused to participate, 2 patients refused the participation of their siblings and 2 siblings were known to suffer from autism and borderline personality disorder, respectively). We excluded 3 of the 30 individuals we invited to participate in the control group owing to the presence of an anxiety disorder (n = 2) or evidence of a past neurologic disorder (n = 1). As 12 of the remaining 27 controls were boys (44%) and 8 of the 25 patients were boys (32%), we excluded 2 boys (selected on the basis of their age) from the control group to make the control and patient groups optimally similar in terms of number, sex and age. Thus, we included 25 patients with anxiety disorders (17 girls, mean age 12.0 yr, mean height 154.9 cm), 9 siblings (3 girls, mean age 10.5 yr, mean height 147.3 cm) and 25 controls (15 girls, mean age 12.7 yr, mean height 155.9 cm) in the study. Results of our Student t test showed that sex (p = 0.58), age (p = 0.38), height (p = 0.82) and handedness (p = 0.56) did not significantly differ between the groups. Comorbidity among the patients with anxiety disorders was common, with most of the patients having more than one disorder. Other comorbidities included dysthymia (n = 8), attention deficit hyperactivity disorder in remission (n = 1) and suspicion of autism spectrum disorders (n = 1); we referred the patient in whom we suspected an autism spectrum disorder to another clinic for further testing. The primary types of anxiety disorders among the patients are shown in Table 1.
Table 1.
Primary diagnosis among 25 patients with anxiety disorders
| Primary anxiety disorder diagnosis | No. patients |
|---|---|
| Social phobia | 13 |
| Generalized anxiety disorder | 9 |
| Phobia | 2 |
| Panic disorder | 1 |
| Total | 25 |
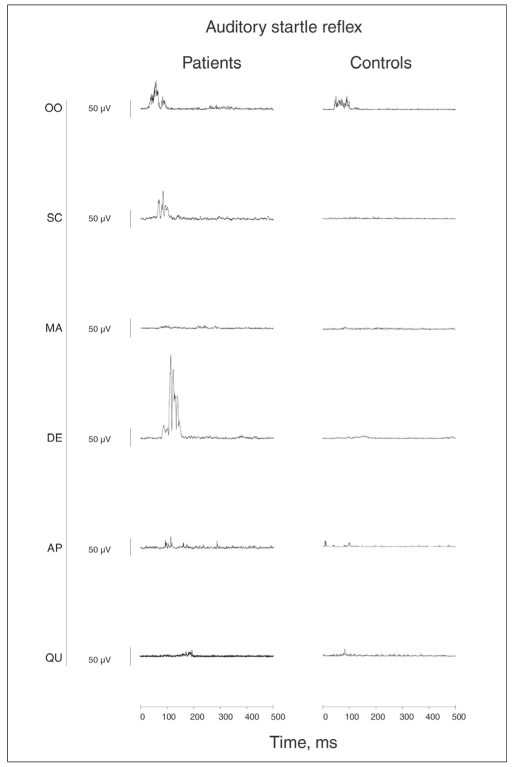
Following auditory stimulation, EMG responses were elicited in the orbicularis oculi, sternocleidomastoid, masseter, deltoid, abductor pollicis brevis and quadriceps muscles (Table 2). Two representative EMGs of a control participant and a patient are shown in Figure 1.
Table 2.
Auditory startle reflex characteristics of individual muscle responses* in patients with anxiety disorder and controls
| Frequency of response, mean (SD) %
|
Area, median (range) μV × ms
|
Latency, median (range) ms
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Muscle | Patients | Controls | p value | Patients | Controls | p value | Patients | Controls | p value |
| Orbicularis oculi | 69.5 (46.1) | 76.5 (42.5) | 0.49 | 783 (52–16 700) | 601 (60–4 760) | 0.07 | 37.9 (21–94) | 39.7 (21–97) | 0.25 |
| Sternocleidomastoid | 34.0 (47.5) | 15.0 (35.7) | 0.021 | 2 565 (301–35 100) | 2 200 (101–23 600) | 0.83 | 58.6 (27–199) | 61.0 (23–181) | 0.88 |
| Masseter | 34.5 (47.6) | 10.5 (30.7) | 0.011 | 1 505 (154–8 390) | 646 (175–16 600) | 0.44 | 47.4 (25–193) | 67.2 (37–126) | 0.09 |
| Deltoid | 15.5 (36.3) | 2.0 (14.0) | 0.025 | 3 390 (535–39 600) | 1 850 (285–23 200) | 0.39 | 66.6 (28–153) | 74.6 (38–150) | 0.54 |
| Abductor pollicis brevis | 19.5 (39.7) | 3.6 (18.8) | 0.016 | 3 670 (159–33 200) | 1 380 (171–6 190) | 0.42 | 72.3 (37–140) | 75.7 (66–123) | 0.86 |
| Quadriceps | 8.5 (27.9) | 1.0 (9.9) | 0.11 | 1 220 (398–2 150) | 921 (251–1 300) | 0.57 | 74.8 (56–114) | 146 (91–170) | 0.08 |
| Combined response | 30.3 (28.2) | 18.2 (14.6) | 0.027 | 7.7 (5.4) | 4.4 (3.4) | 0.011 | ND | ND | ND |
ASR = auditory startle reflex; ND = not done; SD = standard deviation.
The multiple-muscle ASR combined response probability and combined area under the curve were significantly enlarged in patients compared with controls. The blink (orbicularis oculi) response probability and area under the curve were not significantly different in patients compared with controls. The muscle latencies were not significantly different in patients compared with controls.
Fig. 1.
Representative electromygraphs of the auditory startle reflex in a control participant and in a patient. AP = abductor pollicis brevis (hand); DE = deltoid (shoulder); MA = masseter (jaw); OO = orbicularis oculi (eye, blink); QU = quadriceps (leg) muscles; SC = sternocleidomastoid (neck).
Multiple-muscle ASR
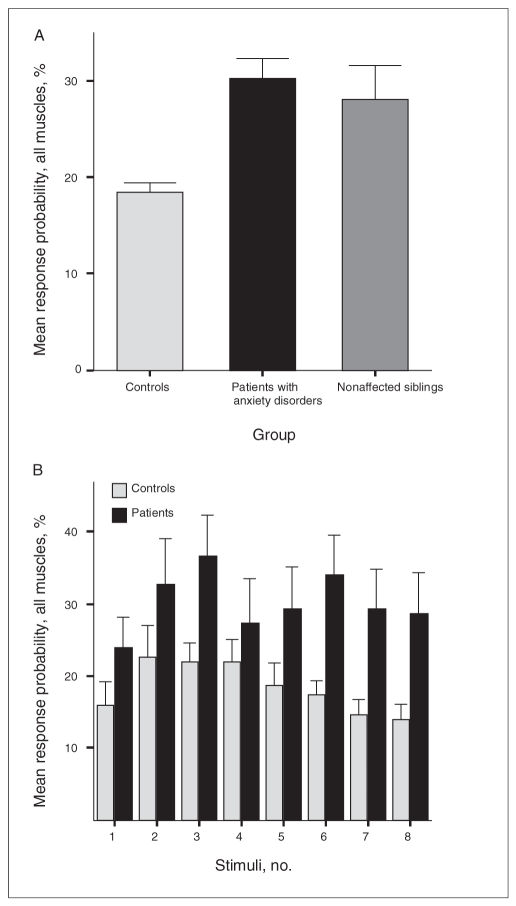
The multiple-muscle response probability was significantly enlarged among patients compared with controls (mean 30.25%, SD 28.2 in the patient group v. mean 18.2%, SD 14.6 in the control group; F1,50 = 5.16, p = 0.027) (Fig. 2 and Table 2). In addition, the response probabilities of all individual muscles other than the orbicularis oculi and quadriceps muscles were significantly enlarged in patients compared with controls (Table 2).
Fig. 2.
Multiple-muscle auditory startle reflex (ASR). (A) The multiple-muscle ASR combined response probability (the mean of the 6 response probabilities) was significantly enlarged in patients compared with controls, but not in siblings compared with controls. (B) The course of the multiple-muscle ASR with the repetitive stimuli is shown for the patients and controls. Bars represent means, error bars represent standard errors of the means.
The combined area under the curve of all muscles was significantly enlarged in patients compared with controls (mean 7.5, SD 5.4 in the patient group v. mean 4.4, SD 3.4 in the control group; F1,50 = 7.05, p = 0.011) (Table 2). In Table 2, the area under the curves of the individual muscles are shown; none was significantly different between groups.
Blink response
The blink response (orbicularis oculi muscle) probability was 69.5% (SD 46.1) among patients and 76.5% (SD 42.5) among controls (Table 2), a difference that was not significant (F1,50 = 0.51, p = 0.47). The blink area under the curve also was not significantly different between the groups after log-transformation (median 783 μV × ms, range 52–16 700 in the patient group v. median 601 μV × ms, range 60–4 760 in the control group; F1,42.8 = 3.47, p = 0.06) (Table 2).
Fixed time interval peak amplitude and area under the curve
The peak amplitude between 20 and 200 ms of all EMG trials was significantly enlarged among patients compared with controls (F1,47.8 = 4.37, p = 0.042). The area under the curve of all EMG trials was not significantly enlarged (F1,42.5 = 2.11, p = 0.15). The peak amplitude of all orbicularis oculi trials (F1,47.8 = 0.28, p = 0.59) and the area under the curve of all or-bicularis oculi trials (F1,47.5 = 0.66, p = 0.79) were not significantly different between groups.
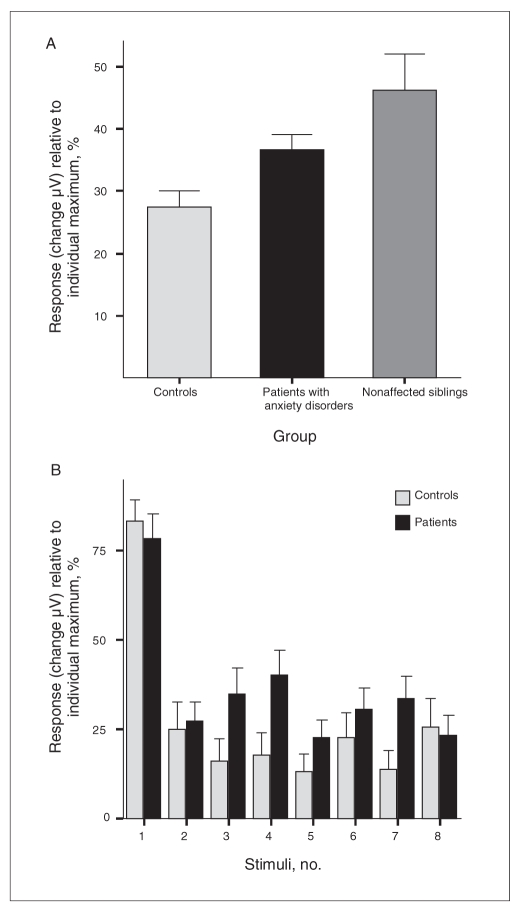
Sympathetic skin response
The sympathetic skin response was significantly enlarged in patients compared with controls (mean 36.8%, SD 34.2 in the patient group v. mean 27.4%, SD 36.6 in the control group; F1,47.7 = 8.20, p = 0.006) (Fig. 3).
Fig. 3.
Sympathetic skin response. (A) The sympathetic skin response (maximal change in μV standardized to the intra-individual maximum) is significantly enlarged in patients and siblings compared with controls. (B) The course of sympathetic skin response with the repetitive stimuli is shown for the patients and controls. Bars represent means, error bars represent standard errors of the means.
ASR pattern
The ASR of both patients and controls showed a similar recruitment pattern. The response probability decreased with increasing distance of the muscle to the startle generator, the caudal brainstem. Furthermore, the pattern of onset latencies of the different muscles of the ASR was normal in patients compared with controls (Table 2). The ASR latencies were not significantly different in patients compared with controls in orbicularis oculi (U = 202, Z = −1.15, p = 0.24), masseter (U = 24, Z = −1.70, p = 0.08), sternocleidomastoid (U = 87, Z = −0.15, p = 0.88), deltoid (U = 9, Z = −0.61, p = 0.54), abductor pollicis brevis (U = 26, Z = −0.17, p = 0.86) and quadriceps (U = 0, Z = −1.70, p = 0.08) (Table 2). Particularly in the distal muscles, the latencies of the controls are not reliable because there were not many trials in which responses occurred (Table 2).
Siblings
In the nonaffected siblings of the patients with anxiety disorders, the combined response probability of all muscles was not significantly different compared with controls (F1,30 = 2.16, p = 0.15) (Fig. 2). However, the sympathetic skin response was significantly enlarged in siblings compared with controls (F1,27.9 = 5.52, p = 0.026) (Fig. 3).
Sex and age effects
There was no significant effect of sex on the multiple muscle response probability (F1,23 = 1.10, p = 0.30), combined area under the curve (F1,23.7 = 1.50, p = 0.69), blink response (F1,19.0 = 0.78, p = 0.38) or sympathetic skin response (F1, 23.1 = 2.0, p = 0.16) among patients with anxiety disorders. Similarly, in patients with anxiety disorders, there was no significant effect of age on the multiple-muscle response probability (F9,15 = 0.70, p = 0.69), combined area under the curve (F9,15.6 = 0.29, p = 0.96), blink response (F8,12.6 = 0.24, p = 0.97) or sympathetic skin response (F9,14.3 = 0.64, p = 0.74).
Discussion
To our knowledge, ours is the first study to show that the ASR is abnormally enlarged in young patients with anxiety disorders. The multiple-muscle ASR (response probability and area under the curve) or whole-body ASR was enlarged among patients compared with controls of the same age and sex. In contrast, the blink response (response probability and area under the curve) showed no abnormalities in patients compared with controls. The autonomic reactivity (as assessed by the sympathetic skin response) in young patients with anxiety disorders was also enlarged compared with controls. The results were not due to an investigator bias, as investigation of fixed time window parameters showed similar results.
The ASR measured over multiple muscles is thought to be a better tool for detecting ASR abnormalities in patients with anxiety disorders. The failure in the present study to find enlarged blink responses is in accordance with similar negative findings in young patients with anxiety disorders,30–32 highly anxious children78 and children with a behaviourally inhibited temperament (a vulnerability factor for the development of anxiety disorders)79 and with the results of studies in adults.29 The contrasting results of the multiple-muscle ASR (whole-body ASR) and blink response in our study confirm that, in children, the blink response cannot be simply equated to the ASR, which occurs in the whole body.36 The measurement over multiple (distal) muscles gives a different, more complete representation of the ASR than the blink response alone.
Both patients with anxiety disorders and their nonaffected siblings had a significantly enhanced autonomic response (as assessed by electrodermal activity of the sympathetic skin response) compared with controls. Autonomic hyperreactivity in children with anxiety disorders has been reported in previous studies.7,8,12,13 As our sample of siblings was small, the results give only preliminary evidence of a shared characteristic of patients and siblings, which may be a vulnerability factor or endophenotype for anxiety disorders.80 However, previous studies support our findings. At-risk offspring of parents with anxiety disorders have been reported to show enlarged electrodermal activity when exposed to fear stimuli.81 Both children with conduct disorders and their fathers have shown a reduced sympathetic skin response (similarly quantified in the present study) following auditory stimuli.58,82 Finally, twin studies have shown a significant heritability for phasic electrodermal activity.83,84 However, other studies investigating at-risk children and young patients with anxiety disorders did not find enlarged autonomic reactivity following auditory stimuli.32,78 In these studies, the electro-dermal activity was not standardized to the intra-individual maximum or mean,56,77 which could explain the findings of Waters and colleages.32,78 The ASR (multiple-muscle response probability) was almost as large in siblings as in patients, but the sample was too small to statistically establish that it was abnormally enlarged in siblings compared with controls. Blink response studies have shown enlarged orbicularis oculi responses in nonaffected offspring of patients with anxiety disorders,85,86 but not always.32
Like in our previous study in healthy children,41 in the present sample we did not find sex and age effects on the ASR, which are present in adults.55 As most participants included in our studies are children and not adolescents, the explanation that sex- and age-specific variations of the ASR may develop after childhood is plausible.41
Our study has several implications. First, our extensive investigation of the ASR in patients with anxiety disorders strengthens the association between enlarged ASRs and pathological anxiety in humans. The results point toward a hypersensitive central nervous system in childhood anxiety disorders. More specifically, as the amygdala (modulated by the prefrontal cortex) is a key structure involved in pathological anxiety18,87 and is associated with fear-potentiated ASRs in animals23,24 and thus humans,88 abnormal function of the amygdala or its modulating structures may explain the enlarged ASRs. Second, our findings provide evidence for a preattentive hyperresponsiveness to auditory stimuli in young patients with anxiety disorders — an early (within 200 ms poststimulus) sensorimotor processing alteration at the brainstem level.87 Similarly, in adults with anxiety disorders, excessive amygdala and medial prefrontal cortex/anterior cingulate cortex activity has been found during the processing of emotional stimuli without awareness.89,90 This supports the idea that patients with anxiety disorders have an increased response of brain arousal systems to (emotional) sensory stimuli early in the time course (100–150 ms post-stimulus).18 Third, the multiple-muscle ASR is recommended to assess ASR abnormalities in patients with anxiety disorders. Finally, ASR abnormalities serve as candidate endophenotypes for anxiety disorders in children.80
Limitations
Our sample was of a moderate size. In addition, the comparison of the ASR paradigm that we used to the psychophysiological ASR paradigms30,31 was limited because the interstimulus interval was longer and the number of presented stimuli was smaller in our study than in those using the psychophysiological ASR paradigms. That is, if more stimuli would have been presented, as is usual in blink response studies, perhaps the blink response would also have been abnormally enlarged in the present sample of children with anxiety disorders. In spite of this limitation, our results show that the ASR measured over multiple muscles is more sensitive in detecting ASR abnormalities in patients with anxiety disorders than the blink response.
Footnotes
Competing interests: None declared for Drs. Bakker, van der Meer, Koelman and Boer. Dr. Tijssen reports having received travel assistance from Boehringer Ingelheim.
Contributors: Drs. Bakker, Tijssen, Koelman and Boer designed the study. Dr. Bakker acquired the data and wrote the article. All authors analyzed the data, reviewed the article and approved its publication.
References
- 1.Rosen JB, Schulkin J. From normal fear to pathological anxiety. Psychol Rev. 1998;105:325–50. doi: 10.1037/0033-295x.105.2.325. [DOI] [PubMed] [Google Scholar]
- 2.leDoux JE. Adult Publishing Group. 1. New York (NY): Simon and Schuster; 1996. The emotional brain. [Google Scholar]
- 3.McClure EB, Monk CS, Nelson EE, et al. Abnormal attention modulation of fear circuit function in pediatric generalized anxiety disorder. Arch Gen Psychiatry. 2007;64:97–106. doi: 10.1001/archpsyc.64.1.97. [DOI] [PubMed] [Google Scholar]
- 4.Thomas KM, Drevets WC, Dahl RE, et al. Amygdala response to fearful faces in anxious and depressed children. Arch Gen Psychiatry. 2001;58:1057–63. doi: 10.1001/archpsyc.58.11.1057. [DOI] [PubMed] [Google Scholar]
- 5.Monk CS, Telzer EH, Mogg K, et al. Amygdala and ventrolateral prefrontal cortex activation to masked angry faces in children and adolescents with generalized anxiety disorder. Arch Gen Psychiatry. 2008;65:568–76. doi: 10.1001/archpsyc.65.5.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Bellis MD, Casey BJ, Dahl RE, et al. A pilot study of amygdala volumes in pediatric generalized anxiety disorder. Biol Psychiatry. 2000;48:51–7. doi: 10.1016/s0006-3223(00)00835-0. [DOI] [PubMed] [Google Scholar]
- 7.Monk C, Kovelenko P, Ellman LM, et al. Enhanced stress reactivity in paediatric anxiety disorders: implications for future cardiovascular health. Int J Neuropsychopharmacol. 2001;4:199–206. doi: 10.1017/S146114570100236X. [DOI] [PubMed] [Google Scholar]
- 8.Dietrich A, Riese H, Sondeijker FE, et al. Externalizing and internalizing problems in relation to autonomic function: a population-based study in preadolescents. J Am Acad Child Adolesc Psychiatry. 2007;46:378–86. doi: 10.1097/CHI.0b013e31802b91ea. [DOI] [PubMed] [Google Scholar]
- 9.Yeragani VK, Rao KA, Pohl R, et al. Heart rate and QT variability in children with anxiety disorders: a preliminary report. Depress Anxiety. 2001;13:72–7. doi: 10.1002/da.1019. [DOI] [PubMed] [Google Scholar]
- 10.Dobkin PL, Treiber FA, Tremblay RE. Cardiovascular reactivity in adolescent boys of low socioeconomic status previously characterized as anxious, disruptive, anxious-disruptive or normal during childhood. Psychother Psychosom. 2000;69:50–6. doi: 10.1159/000012366. [DOI] [PubMed] [Google Scholar]
- 11.Kallen VL, Tulen JH, Utens EM, et al. Associations between HPA axis functioning and level of anxiety in children and adolescents with an anxiety disorder. Depress Anxiety. 2008;25:131–41. doi: 10.1002/da.20287. [DOI] [PubMed] [Google Scholar]
- 12.Boyce WT, Quas J, Alkon A, et al. Autonomic reactivity and psychopathology in middle childhood. Br J Psychiatry. 2001;179:144–50. doi: 10.1192/bjp.179.2.144. [DOI] [PubMed] [Google Scholar]
- 13.Rogeness GA, Cepeda C, Macedo CA, et al. Differences in heart rate and blood pressure in children with conduct disorder, major depression, and separation anxiety. Psychiatry Res. 1990;33:199–206. doi: 10.1016/0165-1781(90)90074-f. [DOI] [PubMed] [Google Scholar]
- 14.Granger DA, Weisz JR, Kauneckis D. Neuroendocrine reactivity, internalizing behavior problems, and control-related cognitions in clinic-referred children and adolescents. J Abnorm Psychol. 1994;103:267–76. doi: 10.1037//0021-843x.103.2.267. [DOI] [PubMed] [Google Scholar]
- 15.Gerra G, Zaimovic A, Zambelli U, et al. Neuroendocrine responses to psychological stress in adolescents with anxiety disorder. Neuropsychobiology. 2000;42:82–92. doi: 10.1159/000026677. [DOI] [PubMed] [Google Scholar]
- 16.van Lang ND, Tulen JH, Kallen VL, et al. Autonomic reactivity in clinically referred children attention-deficit/hyperactivity disorder versus anxiety disorder. Eur Child Adolesc Psychiatry. 2007;16:71–8. doi: 10.1007/s00787-006-0575-y. [DOI] [PubMed] [Google Scholar]
- 17.Greaves-Lord K, Ferdinand RF, Oldehinkel AJ, et al. Higher cortisol awakening response in young adolescents with persistent anxiety problems. Acta Psychiatr Scand. 2007;116:137–44. doi: 10.1111/j.1600-0447.2007.01001.x. [DOI] [PubMed] [Google Scholar]
- 18.Williams LM, Gordon E. Dynamic organization of the emotional brain: responsivity, stability, and instability. Neuroscientist. 2007;13:349–70. doi: 10.1177/10738584070130040801. [DOI] [PubMed] [Google Scholar]
- 19.Valls-Sole J. Function and dysfunction of the startle reaction in humans. Rev Neurol. 2004;39:946–55. [PubMed] [Google Scholar]
- 20.Oguro K, Aiba H, Hojo H. Different responses to auditory and somaesthetic stimulation in patients with an excessive startle: a report of pediatric experience. Clin Neurophysiol. 2001;112:1266–72. doi: 10.1016/s1388-2457(01)00568-5. [DOI] [PubMed] [Google Scholar]
- 21.Wilkins DE, Hallett M, Wess MM. Audiogenic startle reflex of man and its relationship to startle syndromes. A review. Brain. 1986;109:561–73. doi: 10.1093/brain/109.3.561. [DOI] [PubMed] [Google Scholar]
- 22.Landis C, Hunt W. The startle pattern. New York (NY): Farrar and Rinehart; 1939. [Google Scholar]
- 23.Davis M, Gendelman DS, Tischler MD, et al. A primary acoustic startle circuit: lesion and stimulation studies. J Neurosci. 1982;2:791–805. doi: 10.1523/JNEUROSCI.02-06-00791.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis M. The role of the amygdala in fear-potentiated startle: implications for animal models of anxiety. Trends Pharmacol Sci. 1992;13:35–41. doi: 10.1016/0165-6147(92)90014-w. [DOI] [PubMed] [Google Scholar]
- 25.Rauch SL, Shin LM, Wright CI. Neuroimaging studies of amygdala function in anxiety disorders. Ann N Y Acad Sci. 2003;985:389–410. doi: 10.1111/j.1749-6632.2003.tb07096.x. [DOI] [PubMed] [Google Scholar]
- 26.Morgan CA, III, Grillon C, Southwick SM, et al. Exaggerated acoustic startle reflex in Gulf War veterans with posttraumatic stress disorder. Am J Psychiatry. 1996;153:64–8. doi: 10.1176/ajp.153.1.64. [DOI] [PubMed] [Google Scholar]
- 27.Ludewig S, Geyer MA, Ramseier M, et al. Information-processing deficits and cognitive dysfunction in panic disorder. J Psychiatry Neurosci. 2005;30:37–43. [PMC free article] [PubMed] [Google Scholar]
- 28.Butler RW, Braff DL, Rausch JL, et al. Physiological evidence of exaggerated startle response in a subgroup of Vietnam veterans with combat-related PTSD. Am J Psychiatry. 1990;147:1308–12. doi: 10.1176/ajp.147.10.1308. [DOI] [PubMed] [Google Scholar]
- 29.Grillon C, Baas J. A review of the modulation of the startle reflex by affective states and its application in psychiatry. Clin Neurophysiol. 2003;114:1557–79. doi: 10.1016/s1388-2457(03)00202-5. [DOI] [PubMed] [Google Scholar]
- 30.Ornitz EM, Pynoos RS. Startle modulation in children with post-traumatic stress disorder. Am J Psychiatry. 1989;146:866–70. doi: 10.1176/ajp.146.7.866. [DOI] [PubMed] [Google Scholar]
- 31.Lipschitz DS, Mayes LM, Rasmusson AM, et al. Baseline and modulated acoustic startle responses in adolescent girls with post-traumatic stress disorder. J Am Acad Child Adolesc Psychiatry. 2005;44:807–14. doi: 10.1097/01.chi.0000166379.60769.b6. [DOI] [PubMed] [Google Scholar]
- 32.Waters AM, Craske MG, Bergman RL, et al. Developmental changes in startle reactivity in school-age children at risk for and with actual anxiety disorder. Int J Psychophysiol. 2008;70:158–64. doi: 10.1016/j.ijpsycho.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 33.Winslow JT, Parr LA, Davis M. Acoustic startle, prepulse inhibition, and fear-potentiated startle measured in rhesus monkeys. Biol Psychiatry. 2002;51:859–66. doi: 10.1016/s0006-3223(02)01345-8. [DOI] [PubMed] [Google Scholar]
- 34.Blumenthal TD, Cuthbert BN, Filion DL, et al. Committee report: guidelines for human startle eyeblink electromyographic studies. Psychophysiology. 2005;42:1–15. doi: 10.1111/j.1469-8986.2005.00271.x. [DOI] [PubMed] [Google Scholar]
- 35.Filion DL, Dawson ME, Schell AM. The psychological significance of human startle eyeblink modification: a review. Biol Psychol. 1998;47:1–43. doi: 10.1016/s0301-0511(97)00020-3. [DOI] [PubMed] [Google Scholar]
- 36.Brown P, Rothwell JC, Thompson PD, et al. New observations on the normal auditory startle reflex in man. Brain. 1991;114:1891–902. doi: 10.1093/brain/114.4.1891. [DOI] [PubMed] [Google Scholar]
- 37.Maschke M, Drepper J, Kindsvater K, et al. Involvement of the human medial cerebellum in long-term habituation of the acoustic startle response. Exp Brain Res. 2000;133:359–67. doi: 10.1007/s002210000417. [DOI] [PubMed] [Google Scholar]
- 38.Muller J, Rinnerthaler M, Poewe W, et al. Auditory startle reaction in primary blepharospasm. Mov Disord. 2007;22:268–72. doi: 10.1002/mds.21270. [DOI] [PubMed] [Google Scholar]
- 39.Kofler M, Muller J, Reggiani L, et al. Influence of gender on auditory startle responses. Brain Res. 2001;921:206–10. doi: 10.1016/s0006-8993(01)03120-1. [DOI] [PubMed] [Google Scholar]
- 40.Carlsen AN, Dakin CJ, Chua R, et al. Startle produces early response latencies that are distinct from stimulus intensity effects. Exp Brain Res. 2007;176:199–205. doi: 10.1007/s00221-006-0610-8. [DOI] [PubMed] [Google Scholar]
- 41.Bakker MJ, Boer F, van der Meer JN, et al. Quantification of the auditory startle reflex in children. Clin Neurophysiol. 2009;120:424–30. doi: 10.1016/j.clinph.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 42.Gironell A, Kulisevsky J, Roig C, et al. Diagnostic potential of acoustic startle reflex, acoustic blink reflex, and electro-oculography in progressive supranuclear palsy: a prospective study. Mov Disord. 2003;18:1273–9. doi: 10.1002/mds.10529. [DOI] [PubMed] [Google Scholar]
- 43.Muller J, Kofler M, Wenning GK, et al. Auditory startle response in cervical dystonia. Mov Disord. 2003;18:1522–6. doi: 10.1002/mds.10609. [DOI] [PubMed] [Google Scholar]
- 44.Brown P, Rothwell JC, Thompson PD, et al. The hyperekplexias and their relationship to the normal startle reflex. Brain. 1991;114:1903–28. doi: 10.1093/brain/114.4.1903. [DOI] [PubMed] [Google Scholar]
- 45.Kofler M, Muller J, Wenning GK, et al. The auditory startle reaction in parkinsonian disorders. Mov Disord. 2001;16:62–71. doi: 10.1002/1531-8257(200101)16:1<62::aid-mds1002>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 46.Kofler M, Muller J, Seppi K, et al. Exaggerated auditory startle responses in multiple system atrophy: a comparative study of parkinson and cerebellar subtypes. Clin Neurophysiol. 2003;114:541–7. doi: 10.1016/s1388-2457(02)00390-5. [DOI] [PubMed] [Google Scholar]
- 47.Meincke U, Morth D, Voss T, et al. Electromyographical differentiation between the acoustic blink and startle reflex. Implications for studies investigating startle behavior. Eur Arch Psychiatry Clin Neurosci. 2002;252:141–5. doi: 10.1007/s00406-002-0375-4. [DOI] [PubMed] [Google Scholar]
- 48.Williams DR, Doyle LM, Lees AJ, et al. The auditory startle response in parkinsonism may reveal the extent but not type of pathology. J Neurol. 2008;255:628–32. doi: 10.1007/s00415-008-0758-1. [DOI] [PubMed] [Google Scholar]
- 49.Cruccu G, Deuschl G. The clinical use of brainstem reflexes and hand-muscle reflexes. Clin Neurophysiol. 2000;111:371–87. doi: 10.1016/s1388-2457(99)00291-6. [DOI] [PubMed] [Google Scholar]
- 50.Kofler M, Muller J, Valls-Sole J. Auditory startle responses as a probe of brainstem function in healthy subjects and patients with movement disorders. Suppl Clin Neurophysiol. 2006;58:232–48. doi: 10.1016/s1567-424x(09)70072-8. [DOI] [PubMed] [Google Scholar]
- 51.Meincke U, Light GA, Geyer MA, et al. On the waveform of the acoustic startle blink in the paradigm of prepulse inhibition —methodological and physiological aspects. Neuropsychobiology. 2005;52:24–7. doi: 10.1159/000086174. [DOI] [PubMed] [Google Scholar]
- 52.Bakker MJ, Van Dijk JG, van den Maagdenberg AM, et al. Startle syndromes. Lancet Neurol. 2006;5:513–24. doi: 10.1016/S1474-4422(06)70470-7. [DOI] [PubMed] [Google Scholar]
- 53.Meinck HM. Startle and its disorders. Neurophysiol Clin. 2006;36:357–64. doi: 10.1016/j.neucli.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 54.Rothwell JC. The startle reflex, voluntary movement, and the reticulospinal tract. Suppl Clin Neurophysiol. 2006;58:223–31. doi: 10.1016/s1567-424x(09)70071-6. [DOI] [PubMed] [Google Scholar]
- 55.Kofler M, Muller J, Reggiani L, et al. Influence of age on auditory startle responses in humans. Neurosci Lett. 2001;307:65–8. doi: 10.1016/s0304-3940(01)01908-5. [DOI] [PubMed] [Google Scholar]
- 56.Lykken DT, Rose R, Luther B, et al. Correcting psychophysiological measures for individual differences in range. Psychol Bull. 1966;66:481–4. doi: 10.1037/h0023922. [DOI] [PubMed] [Google Scholar]
- 57.Claus D, Schondorf R. Sympathetic skin response. The International Federation of Clinical Neurophysiology. Electroencephalogr Clin Neurophysiol Suppl. 1999;52:277–82. [PubMed] [Google Scholar]
- 58.Herpertz SC, Vloet T, Mueller B, et al. Similar autonomic responsivity in boys with conduct disorder and their fathers. J Am Acad Child Adolesc Psychiatry. 2007;46:535–44. doi: 10.1097/chi.0b013e3180306286. [DOI] [PubMed] [Google Scholar]
- 59.Gogan P. The startle and orienting reactions in man. A study of their characteristics and habituation. Brain Res. 1970;18:117–35. doi: 10.1016/0006-8993(70)90460-9. [DOI] [PubMed] [Google Scholar]
- 60.Siegelaar SE, Olff M, Bour LJ, et al. The auditory startle response in posttraumatic stress disorder. Exp Brain Res. 2006;174:1–6. doi: 10.1007/s00221-006-0413-y. [DOI] [PubMed] [Google Scholar]
- 61.Kaviani H, Gray JA, Checkley SA, et al. Affective modulation of the startle response in depression: influence of the severity of depression, anhedonia, and anxiety. J Affect Disord. 2004;83:21–31. doi: 10.1016/j.jad.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 62.Silverman WK, Albano AM. Anxiety disorders interview schedule for children for DSM-IV, child and parent versions. San Antonio (TX): Psychological Corporation; 1996. [Google Scholar]
- 63.Diagnostic and statisical manual of mental disorders. 4. American Psychiatric Association; Washington (DC): The Association; 1994. [Google Scholar]
- 64.Nauta MH, Scholing A, Rapee RM, et al. A parent-report measure of children’s anxiety: psychometric properties and comparison with child-report in a clinic and normal sample. Behav Res Ther. 2004;42:813–39. doi: 10.1016/S0005-7967(03)00200-6. [DOI] [PubMed] [Google Scholar]
- 65.Voordecker P, Mavroudakis N, Blecic S, et al. Audiogenic startle reflex in acute hemiplegia. Neurology. 1997;49:470–3. doi: 10.1212/wnl.49.2.470. [DOI] [PubMed] [Google Scholar]
- 66.Hilz MJ, Dutsch M. Quantitative studies of autonomic function. Muscle Nerve. 2006;33:6–20. doi: 10.1002/mus.20365. [DOI] [PubMed] [Google Scholar]
- 67.Aramideh M, Eekhof JL, Bour LJ, et al. Electromyography and recovery of the blink reflex in involuntary eyelid closure: a comparative study. J Neurol Neurosurg Psychiatry. 1995;58:692–8. doi: 10.1136/jnnp.58.6.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Eekhof JL, Aramideh M, Bour LJ, et al. Blink reflex recovery curves in blepharospasm, torticollis spasmodica, and hemifacial spasm. Muscle Nerve. 1996;19:10–5. doi: 10.1002/(SICI)1097-4598(199601)19:1<10::AID-MUS2>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 69.Van Opstal AJ, Van Gisbergen JA, Eggermont JJ. Reconstruction of neural control signals for saccades based on an inverse method. Vision Res. 1985;25:789–801. doi: 10.1016/0042-6989(85)90187-7. [DOI] [PubMed] [Google Scholar]
- 70.Bour LJ, Aramideh M, de Visser BW. Neurophysiological aspects of eye and eyelid movements during blinking in humans. J Neurophysiol. 2000;83:166–76. doi: 10.1152/jn.2000.83.1.166. [DOI] [PubMed] [Google Scholar]
- 71.Fowles DC, Christie MJ, Edelberg R, et al. Committee report. Publication recommendations for electrodermal measurements. Psychophysiology. 1981;18:232–9. doi: 10.1111/j.1469-8986.1981.tb03024.x. [DOI] [PubMed] [Google Scholar]
- 72.Gutrecht JA. Sympathetic skin response. J Clin Neurophysiol. 1994;11:519–24. doi: 10.1097/00004691-199409000-00006. [DOI] [PubMed] [Google Scholar]
- 73.Dindo L, Fowles DC. The skin conductance orienting response to semantic stimuli: Significance can be independent of arousal. Psychophysiology. 2008;45:111–8. doi: 10.1111/j.1469-8986.2007.00604.x. [DOI] [PubMed] [Google Scholar]
- 74.Turpin G, Schaefer F, Boucsein W. Effects of stimulus intensity, risetime, and duration on autonomic and behavioral responding: implications for the differentiation of orienting, startle, and defense responses. Psychophysiology. 1999;36:453–63. [PubMed] [Google Scholar]
- 75.Elie B, Guiheneuc P. Sympathetic skin response: normal results in different experimental conditions. Electroencephalogr Clin Neurophysiol. 1990;76:258–67. doi: 10.1016/0013-4694(90)90020-k. [DOI] [PubMed] [Google Scholar]
- 76.Arunodaya GR, Taly AB. Sympathetic skin response: a decade later. J Neurol Sci. 1995;129:81–9. doi: 10.1016/0022-510x(94)00265-p. [DOI] [PubMed] [Google Scholar]
- 77.Lykken DT. Range correction applied to heart rate and to GSR data. Psychophysiology. 1972;9:373–9. doi: 10.1111/j.1469-8986.1972.tb03222.x. [DOI] [PubMed] [Google Scholar]
- 78.Waters AM, Neumann DL, Henry J, et al. Baseline and affective startle modulation by angry and neutral faces in 4–8-year-old anxious and non-anxious children. Biol Psychol. 2008;78:10–9. doi: 10.1016/j.biopsycho.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 79.Schmidt LA, Fox NA, Schulkin J, et al. Behavioral and psycho-physiological correlates of self-presentation in temperamentally shy children. Dev Psychobiol. 1999;35:119–35. [PubMed] [Google Scholar]
- 80.Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003;160:636–45. doi: 10.1176/appi.ajp.160.4.636. [DOI] [PubMed] [Google Scholar]
- 81.Turner SM, Beidel DC, Roberson-Nay R. Offspring of anxious parents: reactivity, habituation, and anxiety-proneness. Behav Res Ther. 2005;43:1263–79. doi: 10.1016/j.brat.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 82.Herpertz SC, Wenning B, Mueller B, et al. Psychophysiological responses in ADHD boys with and without conduct disorder: implications for adult antisocial behavior. J Am Acad Child Adolesc Psychiatry. 2001;40:1222–30. doi: 10.1097/00004583-200110000-00017. [DOI] [PubMed] [Google Scholar]
- 83.Crider A, Kremen WS, Xian H, et al. Stability, consistency, and heritability of electrodermal response lability in middle-aged male twins. Psychophysiology. 2004;41:501–9. doi: 10.1111/j.1469-8986.2004.00189.x. [DOI] [PubMed] [Google Scholar]
- 84.Lykken DT, Iacono WG, Haroian K, et al. Habituation of the skin conductance response to strong stimuli: a twin study. Psychophysiology. 1988;25:4–15. doi: 10.1111/j.1469-8986.1988.tb00949.x. [DOI] [PubMed] [Google Scholar]
- 85.Grillon C, Dierker L, Merikangas KR. Fear-potentiated startle in adolescent offspring of parents with anxiety disorders. Biol Psychiatry. 1998;44:990–7. doi: 10.1016/s0006-3223(98)00188-7. [DOI] [PubMed] [Google Scholar]
- 86.Merikangas KR, Avenevoli S, Dierker L, et al. Vulnerability factors among children at risk for anxiety disorders. Biol Psychiatry. 1999;46:1523–35. doi: 10.1016/s0006-3223(99)00172-9. [DOI] [PubMed] [Google Scholar]
- 87.Liddell BJ, Brown KJ, Kemp AH, et al. A direct brainstem-amygdala-cortical ‘alarm’ system for subliminal signals of fear. Neuroimage. 2005;24:235–43. doi: 10.1016/j.neuroimage.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 88.Brown P. Physiology of the normal startle response. In: Valls-Sole J, Tolosa E, editors. First European meeting on brainstem reflexes and functions. Madrid: Litofinter; 1998. pp. 107–18. [Google Scholar]
- 89.Rauch SL, Whalen PJ, Shin LM, et al. Exaggerated amygdala response to masked facial stimuli in posttraumatic stress disorder: a functional MRI study. Biol Psychiatry. 2000;47:769–76. doi: 10.1016/s0006-3223(00)00828-3. [DOI] [PubMed] [Google Scholar]
- 90.Bryant RA, Kemp AH, Felmingham KL, et al. Enhanced amygdala and medial prefrontal activation during nonconscious processing of fear in posttraumatic stress disorder: an fMRI study. Hum Brain Mapp. 2008;29:517–23. doi: 10.1002/hbm.20415. [DOI] [PMC free article] [PubMed] [Google Scholar]