Abstract
Normal urinary bladder function requires contraction and relaxation of the detrusor smooth muscle (DSM). The DSM undergoes compensatory hypertrophy in response to partial bladder outlet obstruction (PBOO) in both men and animal models. Following bladder hypertrophy, the bladder either retains its normal function (compensated) or becomes dysfunctional (decompensated) with increased voiding frequency and decreased void volume. We analyzed the contractile characteristics of DSM in a rabbit model of PBOO. The protein kinase C (PKC) agonist Phorbol 12, 13-dibutyrate (PDBu) elicited similar levels of contraction of DSM strips from normal or compensated bladders. However, PDBu-induced contraction decreased significantly in DSM strips from decompensated bladders. The expression and activity of PKC α were also lowest in decompensated bladders. The PKC specific inhibitor bisindolylmaleimide-1 (Bis) blocked PDBu-induced contraction and PKC activity in all three groups. Moreover, the phosphorylation of the phosphoprotein inhibitor CPI-17 was diminished in DSM from the decompensated bladder, which would result in less inhibitory potency of CPI-17 on myosin light chain phosphatase activity and contribute to less contractility. Immunostaining revealed the co-localization of PKC and phosphorylated CPI-17 in the DSM and confirmed the decreases of these signaling proteins in the decompensated bladder. Our results show a differential PKC-mediated DSM contraction with corresponding alterations of PKC expression, activity and the phosphorylation of CPI-17. Our finding suggests a significant correlation between bladder function and PKC pathway. An impaired PKC pathway appears to be correlated with bladder severe dysfunction observed in decompensated bladders.
Keywords: bladder outlet obstruction, CPI-17, PDBu-induced contraction, PKC
Introduction
Partial urinary bladder outlet obstruction (PBOO) is caused by benign prostatic hyperplasia (BPH). PBOO results in an impaired ability of the urinary bladder to store and empty urine. PBOO in a rabbit model results in bladder dysfunction and in alterations of the mechanistic steps involved in detrusor smooth muscle (DSM) contractility, similar to those found in men with BPH.(1;2) In response to PBOO, the DSM undergoes compensatory hypertrophy to produce the increased force necessary to expel urine against an obstruction. In some rabbits, bladder wall hypertrophy and the associated remodeling of the DSM is sufficient to maintain nearly normal bladder function, while other rabbits develop severe bladder dysfunction, resulting in changes in voiding frequency, void volume, and residual volume.(3;4) Interestingly, BPH-induced DSM hypertrophy in men also produces either nearly normal or severely defective bladder function.
Several studies have described the alterations in DSM contractility and expression of contractile and regulatory proteins after two weeks of PBOO. Metabolic cage monitoring of bladder function following PBOO revealed a decreased void volume and increased voiding frequency, consistent with over-expression of the N-terminal myosin isoform SM-A (low ATPase, compared to the SM-B isoform) and less smooth muscle myosin heavy chain.(5) Besides the change of contractile protein in DSM, PBOO also induces a change of regulatory protein, such as Rho-kinase(3) and sarcoplasmic reticulum proteins.(6;7) Protein kinase C (PKC) is another important regulatory protein in smooth muscle contractility.(8-10) PDBu induces rabbit DSM contraction by activating PKC.(11;12) The activated PKC can phosphorylate a 17kDa protein called PKC potentiated inhibitor protein-17 kDa (CPI-17).(13) Phosphorylation of CPI-17 at Thr-38 by PKC produces over a 1000-fold increase in the inhibitory potency of CPI-17. Thus, phosphorylated CPI-17 inhibits myosin phosphatase activity,(14) leading to increased phosphorylation of myosin light chain and contraction of smooth muscle.(15) A recent study shows that PBOO selectively abolishes PKC induced contraction of rabbit DSM.(16)
This study is designed to evaluate whether there is a differential PKC-induced contraction in DSM from compensated and decompensated bladders and whether this change is related with PKC function including PKC expression, activity and CPI-17 phosphorylation. Our results demonstrate that there is no significant change on PKC-induced contraction and PKC function in compensated bladder compared with control. However, decompensated bladders generate significantly less PKC-induced contraction which is accompanied by a significant decrease in PKC expression, PKC activity and CPI-17 phosphorylation compared with control. This finding suggests that the down-regulation of PKC signaling is one of the underlying molecular mechanism involved in the transition from compensated to decompensated.
METHODS
Partial Bladder Outlet Obstruction
The protocol for animal experiments was approved by the University of Pennsylvania's Institutional Animal Care Use Committee (IACUC). The surgical procedure to create PBOO was described in our previous publication.(6) Adult male New Zealand White rabbits weighing approximately 3 kg were anesthetized with ketamine/xylazine (25 mg/10 mg; i.m.). Surgical anesthesia was maintained with pentobarbital (25 mg/kg; i.v.). Under sterile conditions, the urinary bladder was catheterized with an 8-french Foley catheter, and the bladder was exposed through a midline incision. PBOO was initiated by placing a 0-silk ligature around the catheterized urethra. The catheter was removed and the incision was closed with a 3-0 silk. After PBOO, rabbits were kept for two weeks and then sacrificed for bladder tissue collection. One day before sacrifice, rabbits were placed in metabolic cages with free access to food and water to monitor bladder voiding patterns. Frequency was determined as voids per 24 hours. Average voided volume is expressed as ml per void. Selection criteria for decompensated bladders include greater than 30 voids/day and an average voided volume of less than 4 ml. On the other hand, the compensated group had less than 30 voids/day and an average voided volume of more than 4 ml. (7) Analyzed metabolic cage data for animals in two groups are shown in Table 1.
Table 1.
PBOO induced changes on voiding pattern
| Normal | Compensated | Decompensated | |
|---|---|---|---|
| Voiding frequency (voids/ 24 hrs) | 4 ± 3 | 16 ± 8 | 43 ± 13 |
| Voided volumes (ml/void) | 26.0 ± 16.0 | 8.7 ± 4.5 | 2.5 ± 1.0 |
Force Measurements
Bladder smooth muscle strips were prepared by removing the mucosal and serosal layers from the middle bladder body. Longitudinal muscle strips (3 × 10 mm) were suspended in 15 ml of Tyrode's buffer (124.9 mM NaCl, 2.5 mM KCl, 23.8 mM NaHCO3, 0.5 mM MgCl2, 0.4 mM NaH2PO4, 1.8 mM CaCl2, and 5.5 mM dextrose) in organ bath (Radnoti) to equilibrate for 1 hour in 95% O2 and 5% CO2. Grass Model 7D Polygraph was used to record force generation. The length of optimal force development (Lo) was determined by increasing the length of each strip in 1.5 mm increments until maximal contractile force to electrical field stimulation was achieved (17;18). Next, the force generation profile in response to 125 mM KCl was determined. After strips were washed three times with buffer, increasing concentrations of PDBu (0.03 μM, 0.1 μM, 0.3 μM, 1 μM and 3 μM; Calbiochem) were added and the response to 1μM PDBU was recorded. Next, the specific PKC inhibitor Bisindolylmaleimide (Bis) I (10 μM, Calbiochem) was pre-incubated with muscle strips for 20 minutes before the addition of PDBu, to confirm that the PDBu-induced contraction is mediated by PKC.
Tissue preparation for the measurement of PKC activity
Muscle strips were placed in organ baths containing Tyrode's buffer equilibrated with 95% O2 - 5% CO2 at 37°C. Individual strips were snap-frozen in liquid nitrogen for 30 seconds, 1 minute or 3 minutes after the addition of 3μM PDBu. Each strip in a second set of experiment was first pre-incubated with 10 μM Bis for 20 minutes and then snap-frozen in liquid nitrogen for 30 seconds, 1 minute or 3 minutes after the addition of 3μM PDBu. Untreated strips were used as control. Frozen tissues were saved in liquid nitrogen for subsequent PKC assay.
PKC assay
PKC activity was measured using the PepTag Assay kit from Promega, according to the manufacturer's protocol. PepTag C1 peptide is a brightly colored, fluorescent peptide substrate of PKC. Phosphorylation of C1 peptide by PKC alters its charge from +1 to -1. On an agarose gel, the phosphorylated C1 migrated toward the positive electrode and the non-phosphorylated C1 toward the negative electrode.
Tissue extracts for PKC analysis were prepared by homogenizing tissue in cold PKC extraction buffer. The supernatant was collected after centrifuging the lysate for 5 minutes at 14,000 × g. A PKC assay standard was prepared by diluting purified PKC enzyme in dilution buffer. For each sample, the assay mix consisted of reaction buffer, C1 peptide and activation buffer. After adding sample or standard to the assay mix, the reaction tubes were incubated at 30°C for 30 minutes. The reaction was stopped by placing the reaction tubes in a boiling water bath for 10 minutes. The samples were then ready to load onto the gel.
Protein Extraction and Western Blot Analysis
Total protein was extracted from frozen bladder tissue (~50 mg) using 1 ml extraction buffer, which contained 50 mM Tris, pH 6.8, 20% glycerol, 1%SDS and protease inhibitors (0.8 mM PMSF, 10 μM pepstatin, 1 μM antipain and 0.1 mg/ml trypsin inhibitor). Protein concentration was determined by DC protein assay kit (Bio-Rad). Equal amounts of total protein (20μg) were separated on 14% SDS-PAGE gels and transferred to a PVDF membrane (Millipore; Bedford, MA) overnight at 30 V (Bio-Rad mini-transfer unit). After blocking with 5% fat free milk in PBS (phosphate buffered saline) for 1 hour, the membrane was incubated with primary antibodies, including mouse monoclonal PKCα antibody (from ABR Affinity BioReagents, 1:2000 dilution), goat polyclonal CPI-17 and goat polyclonal phospho-CPI-17 (Thr38) (from Santa Cruz, 1:2000 dilution), and mouse monoclonal α-actin antibody (Sigma, 1:5000 dilution) for 2 hours at room temperature. The membrane was then washed and incubated with secondary horseradish peroxidase-linked anti-mouse antibody or anti-goat antibody (1:5,000 dilution) for 1 hour. Membranes were washed thoroughly with PBS containing 0.05% Tween 20 (Sigma) between incubations. Target proteins were detected using an enhanced chemiluminescence kit (ECL) from Amersham Life Sciences. The amounts of PKC, CPI-17 and phosphor-CPI-17 were determined by reflectance scanning densitometry using Bio-Rad GS-800 Calibrated Densitometer and Quantity 1 software (Bio-Rad). Smooth muscle α-actin was used as an internal control to normalize western blot data.
Immunohistochemistry
Cross-sections (5μM) of bladder from sham and PBOO rabbits were made from paraffin blocks. Tissue sections were deparaffinized, put into descending grades of alcohol (100%, 95%, 70%, 30% and 1X PBS), and blocked 30 minutes in 1% BSA solution. After blocking, sections were incubated with antibodies (described above) specific for PKC α/CPI-17 (PKC α and CPI-17 were used for double staining on the same section) and phosphor-CPI-17 (a serial section from the same block). For each antibody, the incubation time is two hours at room temperature and the dilution is 1:200. Sections were washed three times in PBS after primary antibody incubation and treated with secondary antibodies (anti-mouse FITC, anti-goat cy3 and anti-goat FITC, Sigma) at a dilution of 1:400 for 1 h. Sections were washed again three times with PBS and mounted with a drop of mounting medium (Aqua-Mount, Lerner Labs; Pittsburgh, PA). Sections were viewed under Olympus Confocal Laser Scanning Biological Microscope. Images were captured using Fluoview FV1000 software. Negative controls to confirm the specificity of immunostaining were prepared using mouse or goat serum in place of the primary antibodies.
Statistical Analysis
All data are expressed as the mean plus or minus standard error of the mean (SEM) and analyzed by one-way ANOVA. Two types of PBOO were compared with control by Dunnett test, p<0.05 considered statistically significantly. Each n refers to a set of normal, compensated, and decompensated rabbits.
RESULTS
Compensated vs. decompensated bladder function following PBOO
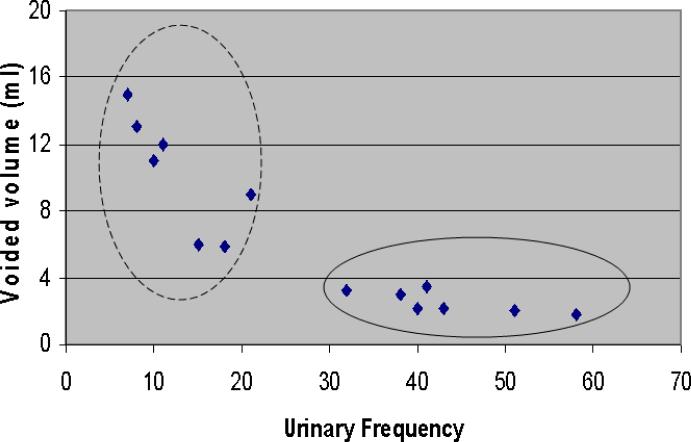
PBOO induces detrusor hypertrophy and alters bladder function. Although characterization of function after PBOO-induced DSM hypertrophy as compensated and decompensated is difficult, some bladders maintain nearly normal function (compensated), while others show severe dysfunction, including increased urinary frequency and decreased void volume (decompensated). In normal rabbit, the average voiding volume and frequency is ~ 26 ml and ~ 4 voids/day. PBOO can increase the frequency to ~43 voids/day and reduce the volume to ~2.5 ml. Figure 1 shows a distinct distribution of obstructed rabbits. One group has lower urinary frequency (less than 30 voids/day) and high voiding volume, which is considered as compensated. The other group has high frequency (more than 30 voids/day) and low voiding volume (less than 2.5 ml per void), which is decompensated. We have noticed a difference in PKC expression and activity between the compensated and decompensated bladders as shown below.
Figure 1. PBOO altered rabbit voiding frequency and volume per void.
The obstructed animals were plotted by voiding frequency and urinary volume per void. The distribution shows two distinct groups: one group with high volume/low frequency (compensated) and the other group with low volume and high frequency (decompensated).
PBOO-induced differential DSM contraction in response to KCl and PDBu
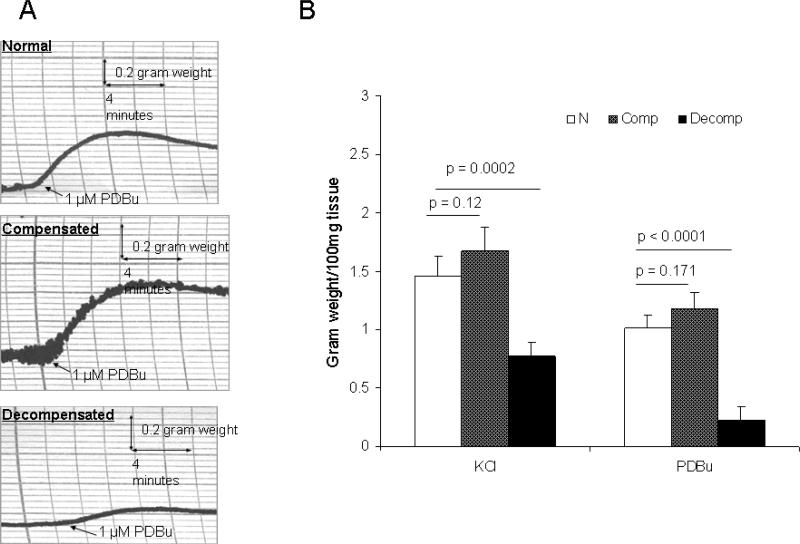
The compensated and decompensated bladder function after PBOO suggested a corresponding alteration in DSM contractility.We measured DSM contraction in response to 125 mM KCl, which directly caused muscle contraction by depolarized DSM membrane. DSM strips from compensated bladders produced similar force compared with normal, while DSM strips from decompensated bladders generated much less force compared to normal controls (Figure 2B). The decreased KCl-induced contraction in decompensated DSM may be due to the loss of smooth muscle myosin heavy chain. Our previous study shows a significantly decreased expression of smooth muscle myosin heavy chain mRNA (1.57 ± 0.19 × 108 copies/100 ng total RNA), compared with sham control (2.04 ± 0.15 × 108 copies/100 ng total RNA).(5) This result indicates that the alteration of contractile protein in decompensated DSM causes impaired DSM contractility despite smooth muscle hypertrophy after PBOO.
Figure 2. PBOO induced differential alteration of DSM contraction.
Panel A: Representative force generation profiles of DSM strips from normal, compensated and decompensated bladders in response to 1μM PDBu (2 horizontal boxes = 4 minutes, 5 small vertical boxes = 0.2 gram weight). Panel B: Analyzed force generation from four experiments (n = 4 animals per group) in response to 125 mM KCl and 1 μM PDBu. Force is normalized by the weight of muscle strips. There is a significant decrease of DSM contractility in decompensated bladder.
Besides the contractile proteins, regulatory proteins also play an important role in DSM contractility. We further examined the PKC-mediated DSM contraction by giving a PKC agonist, PDBu. Figure 2A shows the representative force profiles of DSM from normal, compensated and decompensated bladders in response to 1 μM PDBU. DSM from normal and compensated bladder bladders produced similar levels of force, while PDBu-induced contraction was remarkably decreased in DSM from decompensated bladders. Figure 2B shows the analyzed result of DSM contractility in response to KCl and PDBu. The contractility was significantly decreased in DSM from decompensated bladders compared to normal or compensated groups (n = 4, p < 0.01). There is about 50% decrease in KCl-induced contraction in decompensated bladder. Interestingly, the DSM from these bladders showed about 80% decrease in PDBu-induced contraction. This result suggests an impaired PKC signaling in decompensated DSM which leads to a larger decrease in PDBu-induced contraction than that seen in KCl-induced contraction. Pre-incubation with Bis, a PKC inhibitor, abolished PDBu-induced contraction in DSM from normal and compensated bladders (data not shown). This confirmed that PDBu induces bladder smooth muscle contraction via the PKC pathway.
Alterations in the expression of PKC and the phosphorylation of CPI-17
PDBu induces DSM contraction via the PKC-mediated signal transduction pathway. PKC phosphorylates CPI-17. The phosphorylated CPI-17 inhibits myosin phosphatase, raising the level of myosin light chain phosphorylation. The differential PDBu contraction by DSM from compensated and decompensated bladders indicates that PBOO may alter the PKC pathway differentially.
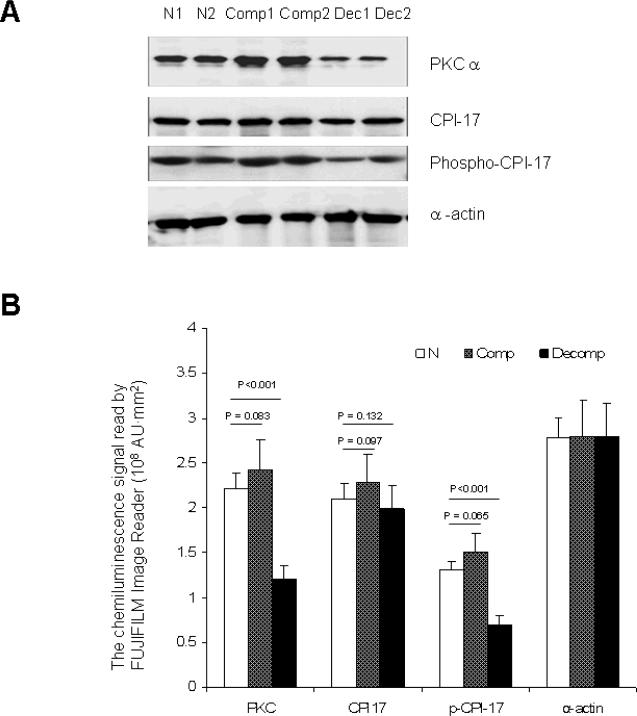
To examine changes in the PKC pathway, the expression of two key factors (PKC and CPI-17) and the phosphorylation of CPI-17 were determined. Figure 3 shows a representative Western blot image and quantification analysis for the target proteins. Smooth muscle specific α-actin was used as an internal control since our previous study showed that PBOO did not alter α-actin expression at either the mRNA or protein level (19). The expression of PKC α was significantly decreased in decompensated bladder compared with normal and compensated bladders. However, there were no significant differences in CPI-17 expression in DSM among decompensated, normal, and compensated bladders. There was no significant difference in phosphor-CPI-17 expression between normal and compensated bladders. However, decompensated bladder DSM showed a significantly reduction in the amount of phospho-CPI-17. The decreased phosphor-CPI-17 in decompensated DSM leads to less myosin light chain phosphorylation which may contribute to less PDBu contraction.
Figure 3. Alteration in the expression of PKC α and the phosphorylation of CPI-17.
Panel A: Representative western blots for PKC α, CPI-17, phosphorylated CPI-17 (Phospho-CPI-17) and smooth muscle α-actin (used as an internal control). Western blots from normal (lanes 1 & 2), compensated (lanes 3 & 4), and decompensated (lanes 5 & 6) bladders are shown. Panel B: Quantification analysis of ECL signal which represents the amount of target protein (n = 6 animals per group). PKC α expression and Phospho-CPI-17 were significantly (P < 0.001) decreased in the decompensated bladder DSM.
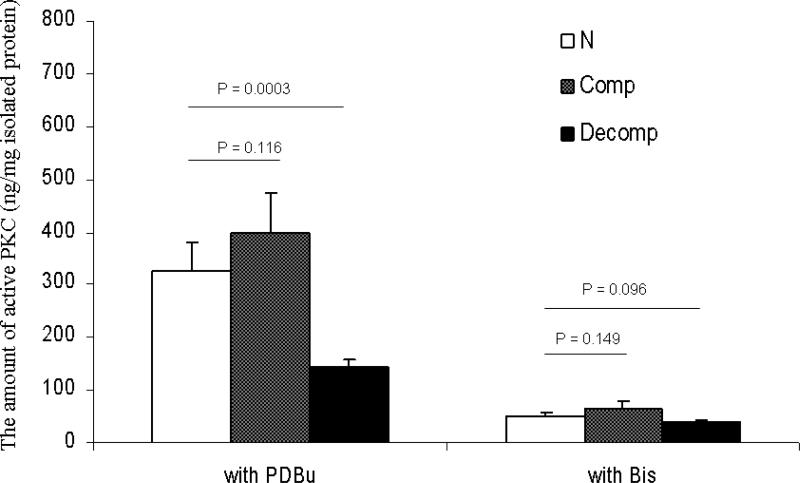
Alterations of PKC activity in DSM induced by PBOO
Western blot analysis revealed a significant decrease in PKC expression and the phosphorylation of CPI-17 in the DSM from decompensated bladders indicating a decreased PKC activity. In order to quantify the change of PKC activity, PKC activity was measured in the presence of the PKC agonist PDBu or the PKC inhibitor bisindolylmaleimide-1 (Bis) in DSM extracts prepared from normal, compensated and decompensated bladders (Figure 4) using PKC assay kit. Purified PKC protein was used as standard and the unit of PKC activity is expressed as ng purified PKC protein per mg isolated protein from tissue. There was a significant decrease in PKC activity in decompensated DSM compared with compensated or normal. The level of decreased enzyme activity is associated with the decrease in protein expression, which indicates that decreased enzyme activity is due to decreased protein expression. PKC activity was inhibited by Bis, confirming again that PDBu stimulation is mediated by PKC.
Figure 4. Comparison of PKC activity in normal, compensated, and decompensated bladders.
PKC activity in DSM from normal, compensated, and decompensated bladders was measured using a PKC assay kit (Promega) in the presence of PDBu or Bis. Purified PKC protein was used as standard in the assay. Therefore, the unit of PKC activity is expressed as the amount of purified PKC (ng) per mg isolated protein from different sample. There is a significant decrease in PKC activity in the decompensated bladder DSM, compared to normal or compensated bladders (n = 4, p<0.01). PKC activity was inhibited in the presence of PKC inhibitor (Bis) in all groups.
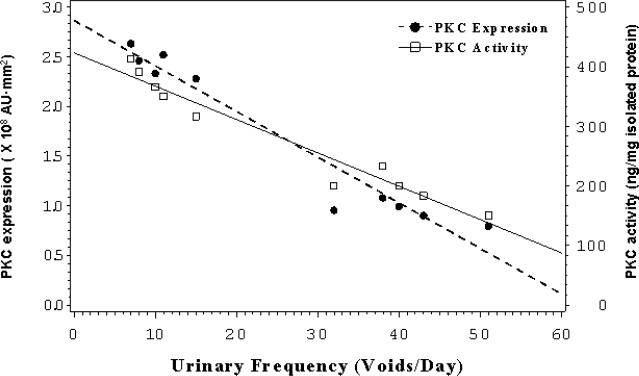
Correlation between PKC function and bladder function
Figure 5 shows that both PKC α expression and PKC activity are correlated with urinary frequency. The decrease of PKC expression or activity in PBOO animal is accompanied by the increase of urinary frequency. This result indicates that PKC function is critical to bladder function. Impaired PKC function is correlated with bladder decompensation.
Figure 5. The correlation between PKC function (the expression of α isoform and PKC activity) and urinary frequency.
The expression of PKC α and PKC activity were plotted to against urinary frequency. Both plots show an increased urinary frequency is correlated with a decreased PKC function.
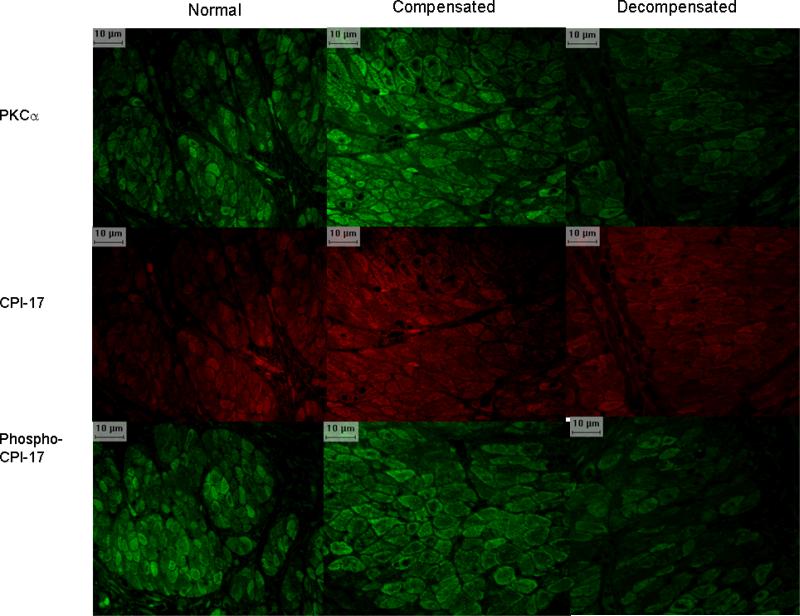
Immunostaining of PKC and CPI-17 in bladder sections from normal, compensated and decompensated rabbits
Paraffin sections from normal, compensated and decompensated bladders were prepared for confocal immunofluorescence microscopy. Representative images of the localization of PKC α (top panels), CPI-17 (middle panels) and phospho-CPI-17 (lower panels) are shown in Figure 6. Images were taken under the identical conditions. The intensity of fluorescent staining is related to the amount of target protein. Decompensated bladder sections showed weak PKC α and phospho-CPI-17 staining, compared to normal and compensated bladder sections. This supports the hypothesis that down-regulation of the PKC pathway plays a role in bladder dysfunction. CPI-17 immunostaining levels were not remarkably different among the three groups. PKC α and phosphor-CPI-17 were primarily expressed in the smooth muscle bundle area, especially around smooth muscle cell membranes. CPI-17 was located in both smooth muscle cytoplasm and cell membrane.
Figure 6. Confocal immunofluorescence micrographs of DSM sections for PKC α, CPI-17 and phospho-CPI-17.
Confocal micrographs of bladder sections from normal (left column), compensated (middle column), and decompensated (right column) animals. In situ localization of PKC α (top panels) and CPI-17 (middle panels) were done on same section. Phospho-CPI-17 (lower panes) was prepared on the serial section from the same block. All images were taken using a confocal microscope under the same exposure time and brightness. Negative controls were prepared using pre-immune serum instead of the primary antibody (not shown; no signal).
DISCUSSION
BPH induces significant alterations in the morphology and physiology of the urinary bladder wall. We have studied rabbit model of PBOO to examine the mechanism involved in altered bladder contractility that contributes to impaired bladder function. Normal bladder function requires bladder smooth muscle to produce enough force to empty urine quickly and completely. Following PBOO, the DSM undergoes hypertrophy, accompanied by a remarkable alteration in bladder function. Two week obstructed animals can be placed in metabolic cages to evaluate the effects of PBOO on bladder function. Some rabbits show relatively normal bladder functions because DSM hypertrophy produces more force to overcome the outlet obstruction (compensated group). Other rabbits show slow and incomplete bladder emptying because DSM can not generate sufficient force despite of DSM hypertrophy (decompensated group). Although there are many studies on compensation/decompensation in heart, the information about this issue in bladder is very limited. There are only a few studies from Zderic's group to show that bladder decompensation is highly associated with a loss of sarcoplasmic reticulum function. (6;7)
In the present study, we did side by side comparison of PKC-mediated signaling in compensated and decompensated DSM. PKC is activated by PDBu and then phosphorylates its downstream effector protein CPI-17. CPI-17, in turn, regulates myosin light chain phosphatase and the phosphorylation level of the myosin light chain, which is a prerequisite for force generation in smooth muscle.(20-22) Therefore, we first examined PDBu-induced contraction and then we measured the related signals including the expression and activity of PKC expression and the phosphorylation of CPI-17. We show that PBOO induces differential alterations in PKC-mediated DSM contractility. The PKC-mediated signal transduction pathway plays an important role in the regulation of smooth muscle contraction through myosin light chain phosphorylation. Force generation occurs via PKCα translocation.(11;12;23-25) Compensated DSM can generate normal force in response to PDBu stimulation, while decompensated DSM produces limited PDBu contraction (Figure 2). Reduced PDBu contraction is consistent with the finding reported by Moreland's group.(16) We also blocked PDBU-induced contraction by pre-incubation of muscle strips with a PKC inhibitor to confirm that PDBu-induced bladder smooth muscle contraction is acting via the PKC pathway. This result indicates that loss of PKC-mediated contraction might be responsible for the bladder dysfunction seen in the decompensated group.
We further investigated the molecular basis of the loss of PKC-mediated contraction in the decompensated bladder. The protein expression of PKCα and the enzymatic activity of PKC were significantly reduced in the decompensated bladder (Figures 3 & 4). In vascular smooth muscle, both PKC α and δ isoforms phosphorylate CPI-17, especially the PKC δ isoform.(23) There are no change of β isoform induced by PBOO and the expression of θ and ζ are very limited in rabbit bladder (data not shown). Our preliminary data show that PKC α is the major PKC isoform in rabbit DSM. Expression of the PKC α isoform in the decompensated bladder decreased ~60% compared to normal bladders. Likewise, PKC activity was reduced ~60% in the decompensated bladder. Therefore, it is reasonable to conclude that the loss of PKC activity in the decompensated bladder is due, at least in part, to the down-regulation of PKC α.
CPI-17 is a protein that play an important role in the calcium sensitization cascade that maintains force in smooth muscles without additional increases in cytosolic Ca2+.(13) CPI-17 is a downstream effector or PKC. There was a significant decrease in the phosphorylated CPI-17 in the decompensated bladder (Figure 2), although total CPI-17 was not changed. Rho-kinase and PKC are involved in bladder smooth muscle contraction.(26;27) Rho-kinase has been reported to phosphorylate CPI-17 in vitro.(28) We have previously shown the over-expression of Rho-kinase in PBOO DSM (3). If Rho-kinase also directly phosphorylates CPI-17, the up-regulation of Rho-kinase would be expected to compensate for the down-regulation of PKC. However, it appears that Rho-kinase doesn't increase phosphor-CPI-17 level in decompensated DSM. Our finding is consistent with a recent study in vascular smooth muscle demonstrating that Rho-kinase does not directly phosphorylate CPI-17 in vivo.(29) The present study shows that PDBu-induced contraction is associated with the expression of PKC α, PKC activity, and CPI-17 phosphorylation. Loss of PDBu-induced contraction in decompensated bladders may result from the down-regulation of the PKC-mediated regulatory pathway. Decreased PKC expression leads to a loss of PKC activity and CPI-17 phosphorylation. This loss of CPI-17 phosphorylation leads to low myosin light chain phosphorylation and less force generation. Thus, we show that one of the downstream effectors in the PKC pathway is involved in the regulation of myosin light chain phosphorylation, which is a prerequisite for bladder smooth muscle contraction.
Both compensated and decompensted stages exist in the progress of many diseases but most attention has been paid to heart research. Na+-K+-ATPase and sarcoplasmic reticulum are well studied in heart failure. The expression of Na+-K+-ATPase α2-isoform is increased in compensated heart whereas it is relatively decreased in decompensated heart in guinea pig.(30) Sarcoplasmic reticulum proteins show similar bimodal regulation in rat and human heart.(31;32) Although compensation and decompensation in bladder is not life threatening, similar responses to PBOO are observed in men with BPH. Bladder dysfunction is present in some men with BPH, while others have compensated function.(33;34) The differential responses to PBOO depicted in the rabbit model provide a better understanding of compensated and decompensated bladder function. Zderic et al show that decreased sarcoplasmic reticulum protein expression is associated with decompensated bladder function and the recovery of bladder function after obstruction reversal is related with the expression of ryanodine receptor (one of the sarcoplasmic reticulum protein.(6;7) Hence, we demonstrate that the loss of PKC-mediated contraction and decreased PKC function occurred in decompensated bladder but not compensated bladder. The PKC function is correlated with bladder function (Figure 5). The loss of PKC signaling also occurred during the transition of the bladder from compensated to decompensated. Moreover, our preliminary study about PBOO reversal shows a very interesting result. After removing the urethral ligation, some reversal animals with improved bladder function have improved PDBu-induced contraction and PKC-α expression. While some reversal animals still remain decompensated and there is no increase of PDBu-induced contraction and PKC expression. Our future study will focus on the detailed mechanism for this phenomenon.
In summary, we show that the loss of PDBu-induced DSM contraction and the decreased PKC function correlated with the change in bladder function from compensated to decompensated stage. Therefore, the loss of PKC signaling is one of the underlying mechanisms of bladder dysfunction. This information will be helpful for a better understanding how the bladder becomes decompensated. Thus, a new strategy to manage bladder dysfunction associated with PBOO may be developed based on the better understanding of bladder decompensation.
Acknowledgements
This work was supported by the George O'Brien Urology Research Center grant (P50 DK52620) from the National Institute of Diabetes and Digestive and Kidney Diseases. We thank Dr. Moreland for his helpful suggestions and discussions during the course of this study. We thank Jocelyn McCabe for her assistance in the preparation of this manuscript. We also thank Xianqun Luan for his help on data analysis.
This work was supported by National Institute of Diabetes and Digestive and Kidney Diseases Grants P50 DK52620
ABBREVIATIONS
- (BPH)
benign prostatic hyperplasia
- (Bis)
bisindolylmaleimide-1
- (CPI-17)
a 17-kDa PKC-potentiated inhibitory protein of protein phosphatase-1
- (PBOO)
partial bladder outlet obstruction
- (PDBu)
Phorbol 12,13-dibutyrate
- (PKC)
protein kinase C
Reference List
- 1.Levin RM, Longhurst PA, Monson FC, et al. Effect of bladder outlet obstruction on the morphology, physiology, and pharmacology of the bladder. Prostate Suppl. 1990;3:9–26. doi: 10.1002/pros.2990170503. [DOI] [PubMed] [Google Scholar]
- 2.Levin RM, Haugaard N, O'Connor L, et al. Obstructive response of human bladder to BPH vs. rabbit bladder response to partial outlet obstruction: a direct comparison. Neurourol Urodyn. 2000;19:609–629. doi: 10.1002/1520-6777(2000)19:5<609::aid-nau7>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 3.Bing W, Chang S, Hypolite JA, et al. Obstruction-induced changes in urinary bladder smooth muscle contractility: a role for Rho kinase. Am J Physiol Renal Physiol. 2003;285:F990–F997. doi: 10.1152/ajprenal.00378.2002. [DOI] [PubMed] [Google Scholar]
- 4.Zhang EY, Stein R, Chang S, et al. Smooth muscle hypertrophy following partial bladder outlet obstruction is associated with overexpression of non-muscle caldesmon. Am J Pathol. 2004;164:601–612. doi: 10.1016/S0002-9440(10)63149-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiSanto ME, Stein R, Chang S, et al. Alteration in expression of myosin isoforms in detrusor smooth muscle following bladder outlet obstruction. Am J Physiol Cell Physiol. 2003;285:C1397–C1410. doi: 10.1152/ajpcell.00513.2002. [DOI] [PubMed] [Google Scholar]
- 6.Stein R, Gong C, Hutcheson JC, et al. The decompensated detrusor III: impact of bladder outlet obstruction on sarcoplasmic endoplasmic reticulum protein and gene expression. J Urol. 2000;164:1026–1030. doi: 10.1097/00005392-200009020-00026. [DOI] [PubMed] [Google Scholar]
- 7.Stein R, Hutcheson JC, Krasnopolsky L, et al. The decompensated detrusor V: molecular correlates of bladder function after reversal of experimental outlet obstruction. J Urol. 2001;166:651–657. doi: 10.1016/s0022-5347(05)66037-5. [DOI] [PubMed] [Google Scholar]
- 8.Matsumoto T, Nishiyama M, Kobayashi T, et al. Effect of phorbol 12,13-dibutyrate on smooth muscle tone in rat stomach fundus. J Smooth Muscle Res. 2005;41:107–116. doi: 10.1540/jsmr.41.107. [DOI] [PubMed] [Google Scholar]
- 9.Walsh MP, Andrea JE, Allen BG, et al. Smooth muscle protein kinase C. Can J Physiol Pharmacol. 1994;72:1392–1399. doi: 10.1139/y94-201. [DOI] [PubMed] [Google Scholar]
- 10.Walsh MP, Horowitz A, Clement-Chomienne O, et al. Protein kinase C mediation of Ca(2+)-independent contractions of vascular smooth muscle. Biochem Cell Biol. 1996;74:485–502. doi: 10.1139/o96-053. [DOI] [PubMed] [Google Scholar]
- 11.Woodsome TP, Eto M, Everett A, et al. Expression of CPI-17 and myosin phosphatase correlates with Ca(2+) sensitivity of protein kinase C-induced contraction in rabbit smooth muscle. J Physiol. 2001;535:553–564. doi: 10.1111/j.1469-7793.2001.t01-1-00553.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoshida M, Nishi K, Machida J, et al. Effects of phorbol ester on lower urinary tract smooth muscles in rabbits. Eur J Pharmacol. 1992;222:205–211. doi: 10.1016/0014-2999(92)90856-y. [DOI] [PubMed] [Google Scholar]
- 13.Eto M, Senba S, Morita F, et al. Molecular cloning of a novel phosphorylation-dependent inhibitory protein of protein phosphatase-1 (CPI17) in smooth muscle: its specific localization in smooth muscle. FEBS Lett. 1997;410:356–360. doi: 10.1016/s0014-5793(97)00657-1. [DOI] [PubMed] [Google Scholar]
- 14.Eto M, Kitazawa T, Brautigan DL. Phosphoprotein inhibitor CPI-17 specificity depends on allosteric regulation of protein phosphatase-1 by regulatory subunits. Proc Natl Acad Sci U S A. 2004;101:8888–8893. doi: 10.1073/pnas.0307812101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Somlyo AP, Somlyo AV. Ca2+ sensitivity of smooth muscle and nonmuscle myosin II: modulated by G proteins, kinases, and myosin phosphatase. Physiol Rev. 2003;83:1325–1358. doi: 10.1152/physrev.00023.2003. [DOI] [PubMed] [Google Scholar]
- 16.Stanton MC, Austin JC, Delaney DP, et al. Partial bladder outlet obstruction selectively abolishes protein kinase C induced contraction of rabbit detrusor smooth muscle. J Urol. 2006;176:2716–2721. doi: 10.1016/j.juro.2006.07.137. [DOI] [PubMed] [Google Scholar]
- 17.Chang S, Hypolite JA, Zderic SA, et al. Enhanced force generation by corpus cavernosum smooth muscle in rabbits with partial bladder outlet obstruction. J Urol. 2002;167:2636–2644. [PubMed] [Google Scholar]
- 18.Hypolite JA, DiSanto ME, Zheng Y, et al. Regional variation in myosin isoforms and phosphorylation at the resting tone in urinary bladder smooth muscle. Am J Physiol Cell Physiol. 2001;280:C254–C264. doi: 10.1152/ajpcell.2001.280.2.C254. [DOI] [PubMed] [Google Scholar]
- 19.Kim YS, Wang Z, Levin RM, et al. Alterations in the expression of the beta-cytoplasmic and the gamma-smooth muscle actins in hypertrophied urinary bladder smooth muscle. Mol Cell Biochem. 1994;131:115–124. doi: 10.1007/BF00925947. [DOI] [PubMed] [Google Scholar]
- 20.Butler TM, Siegman MJ. Control of cross-bridge cycling by myosin light chain phosphorylation in mammalian smooth muscle. Acta Physiol Scand. 1998;164:389–400. doi: 10.1046/j.1365-201X.1998.00450.x. [DOI] [PubMed] [Google Scholar]
- 21.Dillon PF, Aksoy MO, Driska SP, et al. Myosin phosphorylation and the cross-bridge cycle in arterial smooth muscle. Science. 1981;211:495–497. doi: 10.1126/science.6893872. [DOI] [PubMed] [Google Scholar]
- 22.Kamm KE, Hsu LC, Kubota Y, et al. Phosphorylation of smooth muscle myosin heavy and light chains. Effects of phorbol dibutyrate and agonists. J Biol Chem. 1989;264:21223–21229. [PubMed] [Google Scholar]
- 23.Eto M, Kitazawa T, Yazawa M, et al. Histamine-induced vasoconstriction involves phosphorylation of a specific inhibitor protein for myosin phosphatase by protein kinase C alpha and delta isoforms. J Biol Chem. 2001;276:29072–29078. doi: 10.1074/jbc.M103206200. [DOI] [PubMed] [Google Scholar]
- 24.Patil SB, Bitar KN. RhoA- and PKC-alpha-mediated phosphorylation of MYPT and its association with HSP27 in colonic smooth muscle cells. Am J Physiol Gastrointest Liver Physiol. 2006;290:G83–G95. doi: 10.1152/ajpgi.00178.2005. [DOI] [PubMed] [Google Scholar]
- 25.Weng TI, Chen WJ, Liu SH. Bladder instillation of Escherichia coli lipopolysaccharide alters the muscle contractions in rat urinary bladder via a protein kinase C-related pathway. Toxicol Appl Pharmacol. 2005;208:163–169. doi: 10.1016/j.taap.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Durlu-Kandilci NT, Brading AF. Involvement of Rho kinase and protein kinase C in carbachol-induced calcium sensitization in beta-escin skinned rat and guinea-pig bladders. Br J Pharmacol. 2006;148:376–384. doi: 10.1038/sj.bjp.0706723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ratz PH, Meehl JT, Eddinger TJ. RhoA kinase and protein kinase C participate in regulation of rabbit stomach fundus smooth muscle contraction. Br J Pharmacol. 2002;137:983–992. doi: 10.1038/sj.bjp.0704952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koyama M, Ito M, Feng J, et al. Phosphorylation of CPI-17, an inhibitory phosphoprotein of smooth muscle myosin phosphatase, by Rho-kinase. FEBS Lett. 2000;475:197–200. doi: 10.1016/s0014-5793(00)01654-9. [DOI] [PubMed] [Google Scholar]
- 29.Seko T, Ito M, Kureishi Y, et al. Activation of RhoA and inhibition of myosin phosphatase as important components in hypertension in vascular smooth muscle. Circ Res. 2003;92:411–418. doi: 10.1161/01.RES.0000059987.90200.44. [DOI] [PubMed] [Google Scholar]
- 30.Trouve P, Carre F, Belikova I, et al. Na(+)-K(+)-ATPase alpha(2)-isoform expression in guinea pig hearts during transition from compensation to decompensation. Am J Physiol Heart Circ Physiol. 2000;279:H1972–H1981. doi: 10.1152/ajpheart.2000.279.4.H1972. [DOI] [PubMed] [Google Scholar]
- 31.Arai M, Suzuki T, Nagai R. Sarcoplasmic reticulum genes are upregulated in mild cardiac hypertrophy but downregulated in severe cardiac hypertrophy induced by pressure overload. J Mol Cell Cardiol. 1996;28:1583–1590. doi: 10.1006/jmcc.1996.0149. [DOI] [PubMed] [Google Scholar]
- 32.Hasenfuss G, Reinecke H, Studer R, et al. Relation between myocardial function and expression of sarcoplasmic reticulum Ca(2+)-ATPase in failing and nonfailing human myocardium. Circ Res. 1994;75:434–442. doi: 10.1161/01.res.75.3.434. [DOI] [PubMed] [Google Scholar]
- 33.Steele GS, Sullivan MP, Sleep DJ, et al. Combination of symptom score, flow rate and prostate volume for predicting bladder outflow obstruction in men with lower urinary tract symptoms. J Urol. 2000;164:344–348. [PubMed] [Google Scholar]
- 34.Sullivan MP, Yalla SV. Detrusor contractility and compliance characteristics in adult male patients with obstructive and nonobstructive voiding dysfunction. J Urol. 1996;155:1995–2000. [PubMed] [Google Scholar]