Abstract
Since the anthrax attacks of 2001, the emphasis on developing animal models of aerosolized select agent pathogens has increased. Many scientists believe that nonhuman primate models are the most appropriate to evaluate pulmonary response to, vaccines for, and treatments for select agents such as Yersinia pestis (Y. pestis), the causative agent of plague. A recent symposium concluded that the cynomolgus macaque (Macaca fascicularis) plague model should be characterized more fully. To date, a well-characterized cynomolgus macaque model of pneumonic plague using reproducible bioaerosols of viable Y. pestis has not been published. In the current study, methods for creating reproducible bioaerosols of viable Y. pestis strain CO92 (YpCO92) and pneumonic plague models were evaluated in 22 Indonesian-origin cynomolgus macaques. Five macaques exposed to doses lower than 250 CFU remained free of any indication of plague infection. Fifteen macaques developed fever, lethargy, and anorexia indicative of clinical plague. The 2 remaining macaques died without overt clinical signs but were plague-positive on culture and demonstrated pathology consistent with plague. The lethal dose of plague in humans is reputedly less than 100 organisms; in this study, 66 CFU was the dose at which half of the macaques developed fever and clinical signs (ED50), The Indonesian cynomolgus macaque reproduces many aspects of human pneumonic plague and likely will provide an excellent model for studies that require a macaque model.
Yersinia pestis is the causative agent of plague. Likely more people worldwide have died from Y. pestis infections than from any other single infectious disease.26,27 Bubonic plague, the most common form of the disease, results when the bacterium is inoculated into the skin, typically by means of flea bites. The resulting cutaneous infection spreads to local lymph nodes; the swollen lymph nodes are known as bubos and often serve as a source of systemic infection. Although less common, the bacterium also can spread by aerosol, causing pneumonic plague. Pneumonic plague can result from pulmonary spread of systemic infection or from deliberate dissemination and is associated with nearly 100% human mortality if left untreated. Y. pestis is susceptible to commonly available antibiotics if treatment begins soon after infection. However, depending on the route of infection, the time at which infection is confirmed is often too late for antibiotics to prevent significant morbidity or mortality.10 Because pneumonic plague is the form most likely to be seen in bioterrorism events,16 interest in animal models has arisen to support development of vaccines and improved therapeutics.
Potential vaccines and therapeutic agents for plague must protect against the pneumonic disease, but contemporary published data regarding disease pathogenesis using aerosolized Y. pestis pathogenesis in nonhuman primates are scant.4,9,21,23,24 In the United States, when vaccine or antibiotic efficacy cannot be evaluated in humans, an animal species that is reasonably expected to recapitulate human disease must be used.9 For many biothreat agents such as plague, a nonhuman primate model often is required. Although some laboratories have examined the cynomolgus macaque model of aerosolized plague briefly,1 no published reports fully characterize this model. Published studies have examined plague in the African green monkey or vervet (Chlorocebus spp., formerly Cercopithecus aethiops) and rhesus macaque (Macaca mulatta).1 Vervets reportedly are more sensitive to plague than are macaques,4,24 such that some vervets are susceptible to infection with vaccine strains, casting some doubt on applicability of this species for plague studies.1 The disease in rhesus macaques differs from that in humans in that rhesus macaques frequently develop disseminated intravascular coagulation (DIC) and chronic pneumonia as a result of pneumonic plague while humans usually develop acute pneumonia without DIC.1,7
Many participants at a recent symposium sponsored by the Food and Drug Administration and National Institute of Allergy and Infectious Disease endorsed the development of a cynomolgus macaque pneumonic plague model to support plague therapeutic and vaccine studies.8 The current study was undertaken to evaluate the Indonesian cynomolgus macaque as a model of aerosolized Y. pestis Colorado 92 (YpCO92) for subsequent vaccine and therapeutic trials. We also sought to determine whether fever development could be used to determine a humane endpoint to the study, as an alternative to LD50 methods.
Materials and Methods
Animals.
Young adult (2 to 3 kg; males and females) Indonesian cynomolgus macaques were obtained from Scientific Resources (Reno, NV). All animals were tuberculin test-negative and seronegative for Cercopithecine herpesvirus 1 (B virus), simian retrovirus, SIV, simian T-lymphotropic virus, and simian foamy virus. On receipt at the Lovelace Respiratory Research Institute, animals underwent a 30-d quarantine and tuberculosis testing prior to housing in individual 4.3 ft2 cages in the biosafety level 3 building. Animals had contact with cohorts through allogrooming panels in cages, had a 12:12-h light:dark cycle, and were fed a commercial primate diet (Global Primate Diet 2050, Harlan Teklad, Madison, WI). All work was approved by the Lovelace Respiratory Research Institute Institutional Animal Care and Use Committee.
Preparation of viable bioaerosols.
Yersinia pestis strain Colorado 92 (YpCO92) was generously provided by C Richard Lyons (School of Medicine, University of New Mexico, Albuquerque, NM). YpCO92 seed stock was grown from a single colony in brain–heart infusion broth at 28 °C (C-24 Benchtop Incubator, New Brunswick, Edison, NJ) for 48 h. Viable cells were inoculated onto tryptose–blood agar base slants and incubated an additional 48 h at 28 °C. Cells harvested from slants were rinsed with 1% peptone broth. Viable cells were centrifuged, washed in PB and resuspended in cryoprotective medium (1% peptone broth plus 15% glycerol) and frozen in 1-ml aliquots at –80 °C. YpCO92 working stock was prepared by direct inoculation of tryptose–blood agar base slants from 1 vial of seed stock.
For aerosol exposure, a loopful of working stock was inoculated onto each of 5 tryptose–blood agar base slants, which were incubated 48 to 96 h at 28 °C. Immediately prior to exposure of the macaques, cells were harvested by rinsing each slant with approximately 2 ml 1% peptone broth and by combining the contents of the 5 tubes into a single 50-ml conical tube. The cells were centrifuged for 20 to 25 min at 2000 × g (Biofuge Stratos, Sorvall, Newtown, CT) and resuspended in 4 ml 1% peptone broth. The optical density at 600 nm of a 1:100 dilution of cell suspension in 1% peptone broth was determined (SmartSpec 20, Bio-Rad Laboratories, Hercules, CA) and compared against a previously prepared growth curve and a 1% peptone broth control. Viable titers from the initial tryptose–blood agar base suspension, each spray, and each impinger were determined by plating triplicate 0.1-ml samples of serial dilutions of cell suspensions on trypticase soy agar plates (100 × 15 mm). For some low-titer impinger samples, 0.5 ml of undiluted impinger fluid was plated in triplicate on 150 × 20 mm trypticase soy agar plates. All plates were counted after at least 48 h of growth at 28 °C.
Aerosol system.
Cynomolgus macaques were exposed to Y. pestis in a head-only exposure system contained in a class III biosafety cabinet. Bacteria were aerosolized by using Collision nebulizers and were delivered to the animals as previously described.14 Bacterial dilutions for aerosols were calculated according to a published formula13 (Vm = 2.10 × body weight [kg]0.75), and total doses were delivered based on minute volumes measured by using plethysmography (Buxco Research Systems, Buxco Electronics, Wilmington, NC). Inhaled bacterial concentrations were adjusted such that target doses were administered in 6 l of inhaled aerosol. Bacterial doses to the macaques were confirmed through bacterial culture of all-glass impinger samples. The target particle size for deep pulmonary distribution was 2 to 5 μm. The aerosols in this study were generated with a collision nebulizer (model MRE/CN24, 3-jet collision nebulizer, BGI, Waltham, MA).
Dose-range determination.
Other studies have suggested that the ED50 of Y. pestis Colorado 92 (YpCO92) is 4.0 × 102.1,28 Effective dose testing is a refinement of lethal dose testing in which humane endpoints are chosen for euthanasia rather than allowing animals to die. We chose this 4.0 × 102 dose to begin characterizing the YpCO92ED50 in our laboratory. Monkeys were anesthetized with 5 mg/kg tiletamine–zolazepam (Telazol, Fort Dodge Animal Health, Fort Dodge, IA) and were exposed to target doses of 0.25 to 100 ED50 (1.0 × 102 to 4.0 × 105 CFU), with actual delivered doses ranging from 0.03 to 70 ED50 (1.0 × 101 to 2.7 × 105 CFU) according to the principles of the up–down method.5 ED50 values and confidence intervals were characterized by using logistic regression (see Statistical analysis section).
Postexposure monitoring and determination of ED50.
Animal care personnel monitored the macaques after exposure to Y. pestis; monitoring included at least twice-daily evaluation of mentation, appetite, and activity and once-daily temperature assessment. Rectal temperature was taken soon after the light cycle began each day; animals were anesthetized with 10 mg/kg ketamine for thermometry. Early exposures in our laboratory demonstrated that, consistent with data from others,28 macaques that develop a fever of at least 39.7 °C after exposure die within 48 h after fever detection. Therefore, all subsequent animals were euthanized 30 to 36 h after development of fever of 39.7 °C or greater.
Necropsy and histology.
All animals were necropsied immediately after euthanasia or within 8 h of death. At necropsy, gross lesions were recorded, and samples were collected for bacteriology. Samples collected included blood, spleen, liver, right middle lung lobe, tracheobronchial lymph nodes, and additional organs with lesions. Samples from tracheobronchial lymph nodes, liver, and spleen were collected and fixed in 10% neutral-buffered formalin for histology. Lung samples were infused with formalin after collection of sections for microbiologic evaluation culture. Tissues were processed routinely, and 5-μm tissue sections were stained with hematoxylin and eosin for histopathologic analysis.
Microbiologic evaluation of blood and tissues.
Nonquantitative blood cultures were performed prior to exposure, daily for 5 d after exposure and twice weekly thereafter when applicable. Approximately 1 ml of blood was added to a tube containing 5 ml tryptone–soy broth and incubated at least 48 h at 28 to 37 °C. A loop of this resuspension then was plated for colony isolation on blood agar plates, which were incubated at least 48 h and examined for growth of typical Y. pestis colonies. Suspect colonies were Gram-stained and evaluated microscopically to qualitatively confirm presence or absence of YpCO92. Tissue samples from lungs, liver, spleen, and pulmonary lymph nodes were obtained aseptically at necropsy for microbiologic evaluation. Tissue samples were placed in 6 ml of sterile PBS and then into a second plastic bag and were homogenized by using a stomacher (Seward Limited, Norfolk, UK). After homogenization, a loopful of homogenate was streaked for isolation on a blood agar plate. Blood agar plates were incubated at least 48 h and evaluated semiquantitavely (scale, 1 to 4) for viable Y. pestis as described in Table 1.
Table 1.
Qualitative analysis of Y. pestis bacteremiaa from samples taken daily on days 1 to 7 postinoculation or by semiquantitative analysis of tissue colonization after euthanasia
| Tissue colonization |
||||||
| Y. pestis dose (no. CFU) | Bacteremia | Lung | TBLN | Spleen | Liver | Gram stain of pulmonary tissue |
| 12 | – | – | – | – | – | – |
| 16 | – | – | – | – | – | – |
| 35 | + (3, 4) | ++ | ++ | ++ | + | ++ |
| 58 | ++++ | – | – | – | – | – |
| 122 | + (6, 7) | + | ++ | + | + | ++++ |
| 169 | +++ | +++ | ++ | ++ | ++ | ++ |
| 174 | – | – | – | – | – | +++ |
| 198 | – | – | – | – | – | – |
| 208 | + (3, 4) | ++ | ++ | + | + | +++ |
| 227 | – | – | – | – | – | – |
| 262 | + (5, 6) | +++ | ++ | + | ++ | ND |
| 264 | + (6, 7) | +++ | ++ | ++ | ++ | ND |
| 295 | + (4, 5) | ++++ | ++++ | ++ | +++ | ND |
| 353 | +++ | ++++ | +++ | +++ | +++ | ND |
| 374 | ++++ | ++++ | ++ | ++ | ++ | ND |
| 479 | – | +++ | ++ | – | + | ND |
| 759 | – | +++ | ++ | – | – | ND |
| 3050 | ++++ | ++++ | ++++ | ++++ | ++++ | ND |
| 4410 | + (4, 7) | +++ | + | + | + | ND |
| 4850 | ++++ | ++++ | ++++ | ++++ | ++++ | ND |
| 12400 | + (3, 4) | ND | ND | ND | ND | ND |
| 42700 | +++ | ND | ND | ND | ND | ND |
–, no growth; + = 1 to 100 CFU; ++ = 101 to 1000 CFU; +++ = 1001 to 100,000 CFU; ++++ = more than 100,000 CFU); ND, not done; TBLN, tracheobronchiolar lymph nodes.
Days on which bacteremia was seen are noted in parentheses.
Statistical analysis.
Each animal was denoted with or without expression of fever or death. The ED50 (that is, the dose where 50% of the animals had fever of at least 39.7 °C or died) and its corresponding 95% asymmetric confidence interval was estimated by using a logistic regression model. The model was parameterized as
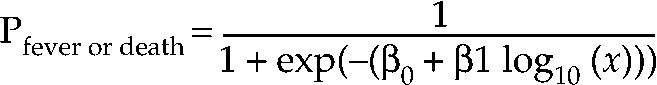 |
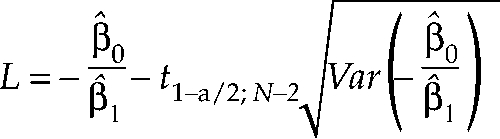
where x is the dose of Y. pestis (in CFU), and 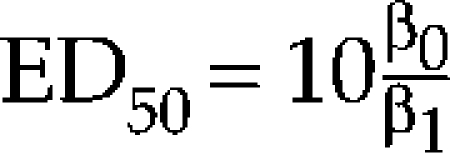 . Parameter estimates were found by using the method of maximum likelihood based on a binary likelihood using the delta method of PROC NLMIXED (SAS version 9.1, SAS Institute, Cary, NC). The asymmetric 95% confidence interval on the ED50 was estimated as [10L, 10u]where
. Parameter estimates were found by using the method of maximum likelihood based on a binary likelihood using the delta method of PROC NLMIXED (SAS version 9.1, SAS Institute, Cary, NC). The asymmetric 95% confidence interval on the ED50 was estimated as [10L, 10u]where
 |
and
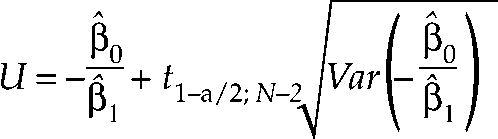 |
and 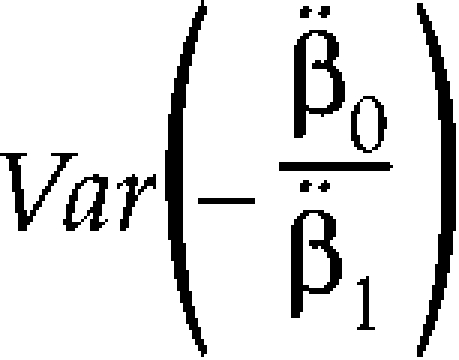 was found by using the delta method of PROC NLMIXED, SAS version 9.1. An asymmetric confidence interval on the log10 scale was used in the calculation of L and U.
was found by using the delta method of PROC NLMIXED, SAS version 9.1. An asymmetric confidence interval on the log10 scale was used in the calculation of L and U.
Results
To evaluate potential for Indonesian cynomolgus macaques to serve as a reproducible model of human pneumonic plague by using humane endpoints, 22 macaques were challenged with aerosolized doses of Y. pestis Colorado 92 ranging from 12 to 42,700 CFU. The macaques then were evaluated for clinical disease, bacteremia, and pathology. Of the 22 macaques, 17 developed plague (Tables 1, 2). Of these 17, 2 died with no premonitory signs; the remaining 15 plague-positive macaques developed fever (39.7 °C or greater) as the initial clinical sign of disease. All of these 15 animals also developed subsequent clinical signs of lethargy and anorexia 24 to 30 h after fever detection (Table 2). Lethargy manifested as sitting at the bottom of the cage, reticence to move around the cage, reluctance to use enrichment devices, and lack of normal interaction with the care staff. Five macaques exposed to doses lower than 250 CFU remained plague-free; 3 of these animals were dosed at less than 60 CFU (Table 2). One macaque that remained plague-free by our criteria was exposed to 198 CFU; this macaque developed fever and lethargy and was euthanized 7 d after exposure but had no bacteriologic, gross, or histologic evidence of plague infection.
Table 2.
ED50 determination according to the up–down method5
| Challenge dose (no. of CFU) | Clinical course | Time of euthanasia (no. of days postexposure) |
| 12 | No signs | NA |
| 16 | No signs | NA |
| 35 | Fever, followed by lethargy | 4 |
| 58 | No signs | NA |
| 122 | Fever, followed by lethargy and anorexia | 7 |
| 169 | Fever, followed by lethargy and anorexia | 5 |
| 174 | Fever followed by lethargy and anorexia | 5 |
| 198 | Fever followed by lethargy and anorexia | 7 |
| 208 | No signs | Died at 4 d postinoculation |
| 227 | No signs | NA |
| 262 | Fever followed by lethargy and anorexia | 7 |
| 264 | Fever followed by lethargy and anorexia | 7 |
| 295 | Fever followed by lethargy and anorexia | 5 |
| 353 | Fever followed by lethargy and anorexia | 4 |
| 374 | Fever followed by lethargy and anorexia | 7 |
| 479 | Fever followed by lethargy and anorexia | 3 |
| 759 | Fever followed by lethargy and anorexia | 4 |
| 3050 | No signs | Died at 5 d postinoculation |
| 4410 | Fever followed by lethargy and anorexia | 7 |
| 4850 | Fever followed by lethargy and anorexia | 4 |
| 12400 | Fever followed by lethargy and anorexia | Died at 5 d postinoculation |
| 42700 | Fever followed by lethargy and anorexia | Died at 5 d postinoculation |
NA, not applicable; these animals were euthanized at day 11 postexposure.
Each data point represents 1 animal.
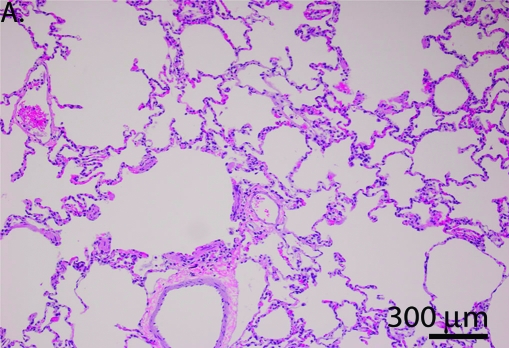
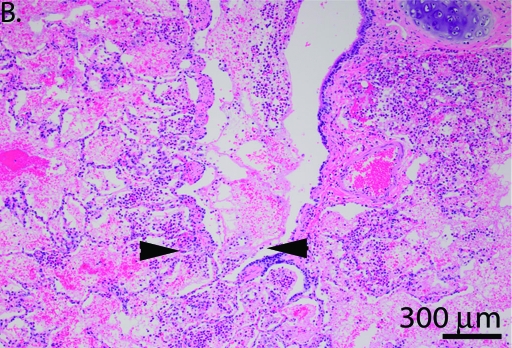
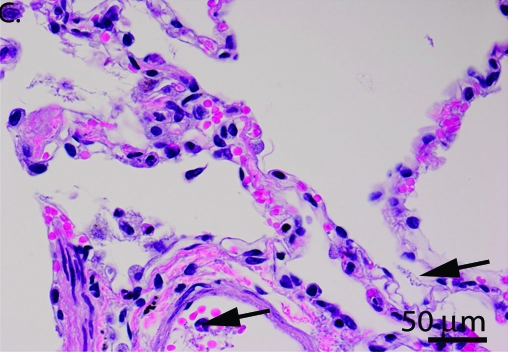
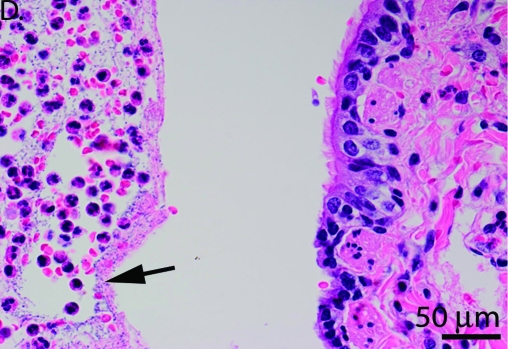
Blood cultures obtained on days 1 through 5, 7, and 11 (when applicable) after exposure confirmed Y. pestis bacteremia in animals that later succumbed to infection (Table 1). Culture of tissues revealed Y. pestis in lungs, tracheobronchial lymph nodes, or spleens of all animals that had developed bacteremia (Table 1). Severity of gross lesions correlated with delivered dose and clinical course at doses higher than 264 CFU; the correlation was less consistent at doses below this level. Distribution of the pneumonia (that is right versus left lung, cranial versus caudal lung) was random among animals (Table 3). Gross lymphadenopathy was limited to the tracheobronchial lymph nodes. Histologic lesions included suppurative bronchopneumonia, fibrinous interstitial pneumonia, splenic leukocytosis, suppurative splenitis, and tracheobronchial lymphadenitis (Table 4, Figure 1).
Table 3.
Gross lesions induced after challenge with Y. pestis
| Dose of Y. pestis (CFU) | Gross necropsy findings |
| 12 | No significant gross lesions |
| 16 | No significant gross lesions |
| 35 | Moderate to marked bilateral fibrinous pneumonia |
| 58 | No significant gross lesions (myometrial congestion) |
| 122 | Moderate bilateral pneumonia; moderate hepatomegaly; moderate splenomegaly |
| 169 | Marked widespread bilateral fibrinous pneumonia; mild fibrinous pleural effusion; moderate splenomegaly |
| 174 | Moderate right unilateral pneumonia; marked splenomegaly |
| 198 | No significant gross lesions |
| 208 | Moderate bilateral pneumonia |
| 227 | No significant gross lesions |
| 262 | Moderate bilateral pneumonia |
| 264 | Moderate bilateral pneumonia; moderate splenomegaly |
| 295 | Marked bilateral pneumonia |
| 353 | Marked bilateral pneumonia |
| 374 | Marked bilateral pneumonia; moderate splenomegaly |
| 479 | Marked multifocal bilateral suppurative pneumonia; mild splenomegaly |
| 759 | Marked multifocal bilateral suppurative pneumonia; moderate TBLN lymphadenomegaly; mild spenomegaly |
| 3050 | Marked bilateral pneumonia; mild fibrinous pleural effusion; mild TBLN lymphadenomegaly; mild splenomegaly |
| 4410 | Marked left unilateral pneumonia with pleural/pericardial adhesions; moderate TBLN lymphadenomegaly; moderate splenomegaly |
| 4850 | Marked bilateral pneumonia; moderate TBLN lymphadenomegaly |
| 12400 | Mild bilateral epistaxis; marked bilateral pneumonia; marked, diffuse TBLN lymphadenopathy; moderate splenomegaly |
| 42700 | Marked bilateral pneumonia; marked TBLN lymphadenopathy; moderate splenomegaly |
TBLN, tracheobronchial lymph nodes.
Table 4.
Histologic grade of lesions
| Y. pestis dose (CFU) | Suppurative broncho-pneumonia | Fibrinous interstitial pneumonia; bacteremia | Splenic histiocytosis and plasmacytosis | Suppurative splenitis | Tracheobronchial lymphadenitis |
| 12 | 0 | 0 | 0 | 0 | 0 |
| 16 | 0 | 0 | 0 | 0 | 0 |
| 35 | 3 | 2 | 0 | 2 | 3 |
| 58 | 0 | 0 | 0 | 0 | 0 |
| 122 | 4 | 4 | 0 | 0 | 3 |
| 169 | 4 | 4 | 0 | 0 | 4 |
| 174 | 4* | 1 | 0 | 2 | 0 |
| 198 | 0 | 0 | 0 | 0 | 0 |
| 208 | 4* | 4 | 0 | 0 | 0 |
| 227 | 0 | 0 | 0 | 0 | 0 |
| 262 | 0 | 4 | 1 | 1 | 0 |
| 264 | 0* | 0 | 0 | 0 | 0 |
| 295 | 3 | 4 | 0 | 0 | 4 |
| 353 | 4 | 3 | 0 | 3 | 4 |
| 374 | 3 | 0 | 0 | 2 | 2 |
| 479 | 2 | 3 | 0 | 3 | 2 |
| 759 | 4 | 0 | 0 | 1 | 3 |
| 3050 | 4 | 3 | 3 | 0 | 4 |
| 4410 | 4 | 0 | 0 | 0 | 2 |
| 4850 | 4 | 0 | 0 | 2 | 4 |
| 12400 | 4 | 4 | 4 | 0 | 4 |
| 42700 | 4 | 4 | 3 | 0 | 3 |
Lesions were graded on a scale of 0 to 4: 0, no noteworthy lesions; 1, minimal lesions that were focal to multifocal; 2, mild, focal to multifocal lesions; 3, moderate multifocal lesions; and 4, severe multifocal lesions. An asterisk indicates that Gram staining of a tissue sample revealed gram-negative bacteria in alveolar capillaries.
Figure 1.
(A and C) Acute fibrinous interstitial pneumonia with bacteria in major pulmonary vessels and septal capillaries, consistent with hematogenous seeding of lung. (B and D) Acute suppurative bronchopneumonia consistent with primary pneumonia rather than hematogenous seeding of lung. Arrows point to bacteria, and arrowheads point to fibrin and neutrophils in a bronchiole; this animal also had slight alveolar hemorrhage. Magnification, ×40 (A and B), ×100 (C and D).
Except in the 2 cynomolgus macaques that died without premonitory signs, euthanasia was successful as a humane endpoint, as expected when choosing humane endpoints for an ED50 study rather than using death as a definitive endpoint as in a traditional LD50 study.25 On the basis of these data, the macaques exposed to 12, 16, 58, 198, or 227 CFU were considered to have survived exposure to YpCO92. The ED50 calculation was based on a logistic regression model on log10(dose). A Hosmer–Lemeshow goodness-of-fit test was not significant (P = 0.99), indicating no evidence of lack of fit of the model to the data. The estimated ED50 was 66 CFU, with a 95% asymmetric confidence interval of 19 to 228 CFU (Table 5).
Table 5.
Estimated ED50, ED90, and ED99 of Y. pestis in cynomolgus monkeys
| Case 1 | Case 2 | |
| ED50 | 66 (19, 228) | 43 (16, 114) |
| ED90 | 343 (83, 1424) | 99 (29, 338) |
| ED99 | 2068 (106, 40253) | 247 (30, 2004) |
Corresponding 95% asymmetric confidence intervals are shown in parentheses; calculations were based on the logistic regression model with maximum likelihood estimation.
Case 1 assumes that the monkeys challenged with 198 and 227 CFU survived plague. Case 2 assumes that these 2 monkeys were not actually exposed to plague.
Discussion
The goal of this study was to evaluate the cynomolgus macaque model of pneumonic plague with humane endpoints. Indonesian cynomolgus macaques demonstrated several aspects of human pneumonic plague. These animals developed clinical disease 36 to 48 h after exposure to Y. pestis aerosol. Subsequent dissemination from lung to lymphoid tissues including liver and spleen, as seen in our Indonesian macaques, is consistent with human disease but has not been consistently reported for rhesus and vervet models.1,15,20
The first sign of infection in 15 plague-positive macaques was fever (Table 2), and 2 additional macaques died with no premonitory signs. Fever as the initial sign of plague is consistent with previous studies of YpCO92 in macaques,28 in which the animals died within 48 h of fever development. Therefore, we considered that detection of fever was an indication that animals were bacteremic and would not survive. In the current study, macaques were euthanized 30 to 36 h after detection of fever exceeding 39.7 °C. As in the rhesus model, 7 survival time was not directly correlated with bacterial dose, but unlike the rhesus model, in which fever was unreliable,16 fever development in cynomolgus macaques mirrors human symptoms. The 15 cynomolgus macaques that developed fever remained clinically normal for approximately 24 h after fever development, after which they demonstrated lethargy, anorexia, and decreased cage exploration. Unlike previous published reports of pneumonic plague in rhesus1,6,7 and unpublished reports in cynomolgus macaques,28 the macaques in the current study did not show tachypnea or other clinical signs of respiratory distress. Although respiratory distress was not evident clinically, the gross and histologic lesions in our animals indicated significant respiratory pathology. The difference in clinical signs may reflect host immune variance, as discussed later.
Although the Indonesian macaque model appears to successfully mimic the human disease, the study highlights several challenges faced in developing aerosol studies of bacterial pathogens with humane endpoints. The first challenge inherent in aerosol pathogen studies is determining the success of the aerosol methods. Although the basic techniques are well established, aerosolization involves shear forces and desiccation, which inevitably kill an undefined percentage of the initial bacterial culture. Exposure doses typically are evaluated through sampling downstream of animal exposure. Such sampling likely provides reasonable estimates of viable bacteria delivered to the animal's nares but is insufficient to evaluate the effect of bacterial degradation products inhaled by animals; these degradation products have an unknown effect on host immune responses. Another critical variable is particle droplet size. Although aerosolization equipment standardizes droplet size, deviations of 1 to 2 μm alter the number of viable bacteria and the likelihood that bacteria enter the deep lung versus bronchi or nares. The methods used in the current study were designed to create a droplet size of 5 μm for reliable pulmonary deposition, similar to sizes reported to result in reliable midpulmonary deposition.3 Historic studies of pneumonic plague in rhesus and vervets used less precise aerosolization techniques,6,7,14,30 likely resulting in greater variability in particle size. Although such differences do not support or negate results from a particular laboratory, they must be taken into account when comparing data between laboratories, and they compound the challenge of developing a single standard model for evaluating biothreat treatments and vaccines.
Similarly, delivered dose is determined by indirect downstream sampling. Therefore, when specific animals fail to demonstrate expected disease development, whether they survived challenge or did not receive the challenge dose must be ascertained. In the present study, the status of 2 cynomolgus macaques—those exposed to 198 and 227 CFU—is ambiguous. To account for this ambiguity—that is, whether the cynomolgus macaques survived plague or were not exposed—both options are explored statistically in Table 5, which shows that the conclusions of this study are not significantly altered by whether these animals were plague survivors or nonexposures. Inclusion or exclusion of these 2 macaques alters the ED50 calculation by 23 CFU (66 versus 43 CFU). This difference is not significant from a microbiologic perspective, and the result is consistent with previous unpublished reports of the infective dose of YpCO92.1,29 This dose range is similar to that reported for humans but is lower than those from reports of rhesus models of pneumonic plague.1,6,7,21
Unlike traditional LD50 studies, the current study was designed to evaluate earlier ED50 studies, which generally are considered more humane than are LD50 endpoints. Unlike LD50 studies, in which the endpoint is unambiguous, ED50 studies require choosing endpoints that minimize animal pain and distress but from which animals will not recover. The clinical data (Table 2) and the bacteriologic and histologic data (Tables 1 and 5) from the current study together indicate that an endpoint of 30 to 36 h after the first detection of fever appears appropriate. Nonetheless, 2 macaques (challenge doses of 208 and 3050 CFU) died with no detected premonitory signs, and 1 (challenge dose, 198 CFU) developed fever and anorexia but had no demonstrable evidence of plague infection. As discussed later, sophisticated instrumentation likely would not have altered disease detection in the 2 cases that died without detection of clinical signs. The macaque that was euthanized without evidence of plague does not alter the data analysis but highlights the challenge of ensuring no complicating physiologic alterations for infectious disease studies in outbred animals. In sum, these 3 variances do not alter the results of this model development but highlight the challenges inherent in developing humane endpoints and aerosol models of highly pathogenic bacteria.
Because fever was the first sign of disease in this model, we considered several methods for thermometry, including rectal and infrared thermometers, microchip thermometry, and telemetric systems. Infrared thermometry has been reported to be unreliable in cynomolgus macaques.32 In preliminary work for the current study, we discovered microchips could not be read inside primate metal cages, necessitating removal of the macaques to obtain readings. In addition, the readings from the microchips differed from rectal thermometry by as much as 2 °C, with the differences being inconsistent even in the same animal. Telemetry can provide accurate, continuous thermometry, but inexpensive telemetry systems generally are not any more accurate than microchips, and quality telemetry systems require cage modifications and investment beyond the reach of many laboratories. On the basis of information from other investigators, we expected fever to develop between 36 and 48 h prior to death from plague.28 Development of our model required detection of fever, but determining the hour of onset was not critical. Therefore, rectal thermometry was sufficient for our goals of model development and analysis. As previously mentioned, 2 macaques (challenge doses, 208 and 3050 CFU) succumbed to infection with no fever or other clinical signs. Given the 48-h expected course for fever in this model, telemetry likely would not have helped to detect disease in these 2 macaques.
Although animals in the present study demonstrated no respiratory clinical signs, the gross and histologic pathology suggest that additional clinical evaluation with thoracic radiography or ultrasonography may be a useful refinement for this model. Severity of pulmonary lesions could be evaluated while animals are restrained for thermography. Given the lack of fever in 2 animals (dosed with 208 and 3050 CFU) with gross and histologic evidence of pneumonia, thoracic imaging likely would enhance this model. However, considering the size constraints in many biosafety level 3 select agent laboratories, the space necessary for such imaging modalities may limit their utility. Although such imaging capability would be a welcome enhancement to the model, the model as described is useful and has been subsequently used in our laboratory to evaluate plague vaccine candidates in the cynomolgus macaque.22
A final category that provides challenge to standardizing endpoints for large animal models of aerosolized pathogens is the outbred nature of the host. Mauritian cynomolgus macaques frequently are used for infectious disease studies and safety testing.12,31 The restricted availability of Mauritian cynomolgus macaques limits their utility for studies. However, Mauritian cynomolgus macaques are derived from Indonesian macaques,18 suggesting Indonesian origin animals may be appropriate for studies for which Mauritian cynomolgus macaques are desired. The macaques used in the present study were of Indonesian origin. In previously published studies, the geographic origin of the macaques used in plague pathogenesis studies is rarely discussed. Recent publications indicate that the geographic origin of cynomolgus macaques may have marked effect on major histocompatibility class I and II alleles.17,19 Additional recent published data suggest major histocompatibility allelelic variance can affect response to several Yersinia virulence determinants and alter host responses in models of aerosolized plague.2,7,11,21,23,24,29,33 Therefore, cynomolgus macaques of varying geographic origin cannot be assumed to respond similarly to plague infections, and the potential effects of geographic origin on plague susceptibility require systematic evaluation.
In summary, Indonesian cynomolgus macaques appear to offer an excellent model for studying human pneumonic plague. Fever is an effective indicator for euthanasia, and the development of telemetric methods and use of additional clinical assessments (for example, radiography) to support these studies likely will increase the efficacy of clinical signs for further refinement of this model. This model likely will be a valuable tool for evaluating potential vaccines and therapeutics.
Acknowledgments
We would like to acknowledge the contributions of Jose Bayardo and Carol Emerson for clinical support and Liz Frye, Rebecca Wisecup, Trevor Brasel, Gil Vigil, Steve Storch, Penny Armijo, Rhonda Garlick, and Leslie Myers, who performed much of the animal work as well as the aerosol exposures and necropsies. This work was performed under the Trans-RCE Nonhuman Primate Aerobiology Core NIAID contract (NIAID U54-AL-057156).
References
- 1.Adamovicz JJ, Worsham PL. 2006. Plague. In: Swearengen J. Biodefense research metholodogy and animal models. Boca Raton: Taylor & Francis; p 107–135 [Google Scholar]
- 2.Bubeck SS, Cantwell AM, Dube PH. 2007. Delayed inflammatory response to primary pneumonic plague occurs in both outbred and inbred mice. Infect Immun 75:697–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clark AR, Chambers CB, Muir D, Newhouse MT, Paboojian S, Schuler C. 2007. The effect of biphasic inhalation profiles on the deposition and clearance of coarse (6.5 μm) bolus aerosols. J Aerosol Med 20:75–82 [DOI] [PubMed] [Google Scholar]
- 4.Davis KJ, Fritz DL, Pitt ML, Welkos SL, Worsham PL, Frielander AM. 1996. Pathology of experimental pneumonic plague produced by fraction-1-positive and fraction-1-negative Yersinia pestis in African green monkeys (Cercopithecus aethiops). Arch Pathol Lab Med 120:156–162 [PubMed] [Google Scholar]
- 5.Dixon WJ. 1965. The up–down method for small samples. J Am Stat Assoc 60:967–978 [Google Scholar]
- 6.Finegold MJ. 1969. Pneumonic plague in monkeys. An electron microscopic study. Am J Pathol 54:167–185 [PMC free article] [PubMed] [Google Scholar]
- 7.Finegold MJ, Petery JJ, Berendt RF, Adams HR. 1968. Studies on the pathogenesis of plague. Blood coagulation and tissue responses of Macaca mulatta following exposure to aerosols of Pasteurella pestis. Am J Pathol 53:99–114 [PMC free article] [PubMed] [Google Scholar]
- 8.Food and Drug Administration, Department of Health and Human Services 2002. New drug and biological products: evidence needed to demonstrate effectiveness of new drugs when human efficacy studies are not ethical or feasible. Fed Regist 67:37988–37998 [PubMed] [Google Scholar]
- 9.Food and Drug Administration, National Institute of Allergy and Infectious Disease, and Department of Health and Human Services October 13–14, 2004. Proceedings of the Animal Models and Correlates of Protection for Plague Vaccines Workshop Marriott Gaithersburg Washingtonian Center, Gaithersburg (MD): Department of Health and Human Services [Google Scholar]
- 10.Gage KL, Dennis DT, Tsai TF. 1996. Prevention of plague: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep 45(RR-14):1–15 [PubMed] [Google Scholar]
- 11.Girard JM, Wagner DM, Vogler AJ, Keys C, Allender CJ, Drickamer LC, Keim P. 2004. Differential plague-transmission dynamics determine Yersinia pestis population genetic structure on local, regional, and global scales. Proc Natl Acad Sci U S A 101:8408–8413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gonder JC. 2003. Demands for rhesus monkeys in biomedical research: a workshop report. ILAR J 44:222–235 [DOI] [PubMed] [Google Scholar]
- 13.Guyton AC. 1947. Measurement of respiratory volumes of laboratory animals. Am J Physiol 150:70–77 [DOI] [PubMed] [Google Scholar]
- 14.Hartings JM, Roy CJ. 2004. The automated bioaerosol exposure system: preclinical platform development and a respiratory dosimetry application with nonhuman primates. J Pharmacol Toxicol Methods 49:39–55 [DOI] [PubMed] [Google Scholar]
- 15.Honko AN, Sriranganathan N, Lees CJ, Mizel SB. 2006. Flagellin is an effective adjuvant for immunization against lethal respiratory challenge with Yersinia pestis. Infect Immun 74:1113–1120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inglesby TV, Dennis DT, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Koerner JF, Layton M, McDade J, Osterholm MT, O'Toole T, Parker G, Perl TM, Russell PK, Schoch-Spana M, Tonat K. 2000. Plague as a biological weapon, medical and public health management. JAMA 283:2281–2290 [DOI] [PubMed] [Google Scholar]
- 17.Krebs KC, Jin ZY, Rudersdorf R, Hughes AL, O'Connor DH. 2005. Unusually high frequency MHC class I alleles in Mauritian-origin cynomolgus macaques. J Immunol 175:5230–5239 [DOI] [PubMed] [Google Scholar]
- 18.Lawler SH, Sussman RW, Taylor LL. 1995. Mitochondrial DNA of Mauritian macaques (Macaca fascicularis): an example of the founder effect. Am J Phys Anthropol 96:133–141 [DOI] [PubMed] [Google Scholar]
- 19.Leuchte N, Berry N, Kohler B, Almond N, LeGrand R, Thorstensson R, Titti F, Sauermann U. 2004. MhcDRB sequences from cynomolgus macaques (Macacca fascicularis) of different origin. Tissue Antigens 63:529–537 [DOI] [PubMed] [Google Scholar]
- 20.Marketon MM, DePaolo RW, DeBord KL, Jabri B, Schneewind O. 2005. Plague bacteria target immune cells during infection. Science 309:1739–1741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marshall JD, Jr, Harrison DN, Rust JH, Jr, Cavanaugh DC. 1971. Serological response of rhesus monkeys (Macaca mulatta) to immunization and infection with Pasteurella pestis. Proc Soc Exp Biol Med 138:738–741 [DOI] [PubMed] [Google Scholar]
- 22.Mett V, Lyons J, Musiychuk K, Chichester JA, Brasil T, Couch R, Sherwood R, Palmer GA, Streatfield SJ, Yusibov V. 2007. A plant-produced plague vaccine candidate confers protection to monkeys. Vaccine 25:3014–3017 [DOI] [PubMed] [Google Scholar]
- 23.Meyer KF, Smith G, Foster L, Brookman M, Sung M. 1974. Live, attenuated Yersinia pestis vaccine: virulent in nonhuman primates, harmless to guinea pigs. J Infect Dis 129Suppl:S85–S112 [DOI] [PubMed] [Google Scholar]
- 24.Meyer KF, Smith G, Foster LE, Marshall JD, Jr, Cavanaugh DC. 1974. Plague immunization. IV. Clinical reactions and serologic response to inoculations of Haffkine and freeze-dried plague vaccine. J Infect Dis 129Suppl:S30–S36 [DOI] [PubMed] [Google Scholar]
- 25.Olfert E, Godson DL. 2000. Humane endpoints for infectious disease animal models in humane endpoints for animals used in biomedical research and testing. ILAR Journal 41:99–104 [DOI] [PubMed] [Google Scholar]
- 26.Overheim KA, DePaolo W, DeBord KL, Morrin EM, Anderson DM, Green NM, Brubaker RR, Jabri B, Schneewind O. 2005. LcrV plague vaccine with altered immunomodulatory properties. Infect Immun 73:5152–5159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perry RD, Fetherston JD. 1997Yersinia pestis—etiologic agent of plague. Clin Microbiol Rev 10:35–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pitt L. 2006. Personal communication.
- 29.Roggenkamp A, Geiger AM, Leitritz L, Kessler A, Heesemann J. 1997. Passive immunity to infection with Yersinia spp. mediated by anti-recombinant V antigen is dependent on polymorphisms of V antigen. Infect Immun 65:446–451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roy CJ, Pitt LM. 2006. Infectious disease aerobiology: aerosol challenge methods. In: Swearengen J. Biodefense research metholodogy and animal models. Boca Raton: Taylor & Francis; p 61–76 [Google Scholar]
- 31.Sibal LR, Samson KJ. 2001. Nonhuman primates: a critical role in current disease research. ILAR J 42:74–84 [DOI] [PubMed] [Google Scholar]
- 32.Sikoski P, Banks ML, Gould R, Young RW, Wallace JM, Nader MA. 2007. Comparison of rectal and infrared thermometry for obtaining body temperature in cynomolgus macaques (Macaca fascicularis). J Med Primatol 36:381–384 [DOI] [PubMed] [Google Scholar]
- 33.Starnbach MN, Bevan MJ. 1994. Cells infected with Yersinia present an epitope to class I MHC-restricted CTL. J Immunol 153:1603–1612 [PMC free article] [PubMed] [Google Scholar]