Abstract
Objective: The purpose of this health technology assessment (HTA), commissioned by the German Agency for HTA at the German Federal Ministry of Health and Social Security, was to systematically review the evidence on effectiveness and cost-effectiveness of antiviral treatment (AVT) for initial chronic hepatitis C (CHC) and to apply these data in the context of the German health care system.
Methods: A systematic literature search was conducted to identify randomised controlled trials (RCTs), meta-analyses, and HTAs that evaluated initial AVT for CHC. A modified version of the German Hepatitis C Model (GEHMO) -- a decision-analytic Markov model -- was used to determine long-term morbidity, life expectancy, quality of life, costs and cost-effectiveness of different treatment strategies. Model parameters were derived from German databases, international RCTs, and a Cochrane Review.
Results: Overall, 9 RCTs, 2 HTA reports, 1 Cochrane review, and 2 meta-analyses examining medical effectiveness of antiviral combination therapy, as well as 7 economic evaluations, met the inclusion criteria. These studies indicate that combination therapy with peginterferon plus ribavirin produced the highest sustained virological response rates (54-61%), followed by interferon plus ribavirin with 38-54%, and interferon monotherapy with 11-21%. Based on international cost-effectiveness studies, interferon plus ribavirin is cost-effective compared to interferon monotherapy. No published articles were available regarding cost-effectiveness of peginterferon plus ribavirin. In our decision analysis, these findings were confirmed and the discounted incremental cost-effectiveness ratio for peginterferon plus ribavirin was € 9,800 per quality-adjusted life-year gained compared to interferon monotherapy (as the next best non-dominated strategy). Sensitivity analyses showed robust results across a wide range of model parameters.
Conclusions: This HTA suggests that initial combination therapy prolongs life, improves quality of life, and is cost-effective in patients with CHC. Combination of peginterferon and ribavirin is the most effective and efficient treatment strategy among the examined options.
Keywords: Ribavirin, Interferon
Abstract
Ziel: Gegenstand dieses Health Technology Assessments (HTA), welches im Auftrag der Deutschen Agentur für HTA (DIMDI/Bundesministerium für Gesundheit und Soziale Sicherung) durchgeführt wurde, war die systematische Bewertung der medizinischen Effektivität und der Kosteneffektivität antiviraler Therapien bei therapienaiven Patienten mit chronischer Hepatitis C im Kontext des deutschen Gesundheitswesens.
Methoden: Es wurde eine systematische Literaturrecherche zur Identifikation von randomisierten klinischen Studien (RCT), Metaanalysen und HTAs zur initialen antiviralen Therapie bei chronischer Hepatitis C durchgeführt. Mit einer modifizierten Version des German Hepatitis C Model (GEHMO), einem entscheidungsanalytischen Markov-Modell, wurden Langzeitmorbidität, Lebenserwartung, qualitätskorrigierte Lebensjahre (QALY), Lebenszeitkosten und das inkrementelle Kosten-Nutzwert-Verhältnis (IKNV) für verschiedene Therapiestrategien ermittelt. Die Modellparameter wurden deutschen Datenbanken, internationalen RCTs und einem Cochrane-Review entnommen.
Ergebnisse: Insgesamt erfüllten 9 RCTs, 2 HTA-Berichte, 1 Cochrane Review und 2 Metaanalysen zur medizinischen Effektivität sowie 7 ökonomische Evaluationen die Einschlusskriterien dieses HTA. Die Sustained Virological Response Raten (SVR) waren am höchsten für Peginterferon plus Ribavirin mit 54-61%, gefolgt von Interferon plus Ribavirin mit 38-54% und der Interferon-Monotherapie mit 11-21%. In internationalen Kosten-Effektivitäts-Studien wurde die Kombinationstherapie mit Interferon und Ribavirin im Vergleich zur Interferon-Monotherapie als kosteneffektiv eingeschätzt. Publizierte Studien zur Kosteneffektivität der Kombinationstherapie mit Peginterferon und Ribavirin wurden im Recherchezeitraum nicht identifiziert. Die Ergebnisse dieses Reviews wurden in unserer entscheidungsanalytischen Modellierung bestätigt. Die Kombinationstherapie mit Peginterferon und Ribavirin erzielte im Vergleich zur Interferon-Monotherapie ein IKNV von 9.800 €/QALY. In Sensitivitätsanalysen zeigten sich robuste Ergebnisse über weite Bereiche der relevanten Modellparameter.
Schlussfolgerung: Basierend auf den Ergebnissen dieses HTAs ist davon auszugehen, dass antivirale Kombinationstherapien bei therapienaiven Patienten die Lebenserwartung erhöhen, die Langzeit-Lebensqualität verbessern und als kosteneffektiv einzustufen sind. Die Kombinationstherapie mit Peginterferon und Ribavirin besitzt unter den untersuchten Therapien die höchste Effektivität und ist im Vergleich zu anderen im deutschen Gesundheitswesen akzeptierten medizinischen Verfahren als kosteneffektiv zu bewerten.
Introduction
Chronic hepatitis C (CHC) is an emerging problem in public health. Hepatitis C virus (HCV) infects an estimated 170 million persons world-wide, with 5 million in Western Europe [1]. In Germany, the prevalence of HCV has been estimated to be 0.5% and the incidence to be 5000 new infected persons per year, resulting in more than 400,000 prevalent cases of chronic hepatitis C [2], [3].
The virus imposes significant personal and social burdens on infected individuals, as well as substantial costs to society. Progression to chronic disease occurs in the majority of HCV-infected persons [4]. Approximately 20% of patients with CHC develop compensated liver cirrhosis within 20 - 30 years [5], [6], [7], [8], [9], [10], [11], [12], which is associated with high mortality risk due to liver failure.
Antiviral combination therapy with interferon alpha and ribavirin has been considered the standard of care for treatment-naïve patients with chronic hepatitis C infection and elevated alanine amino transferase (ALT) levels [5], [13], [14], but recent multinational randomised controlled clinical trials [15], [16] showed that combination therapy with peginterferon alpha and ribavirin yielded higher sustained virological response rates.
However, antiviral combination therapy is relatively expensive, raising the question of whether its clinical benefit supports the costs. With rising medical costs and limited health care budgets, attention is increasingly being focused not only on the clinical benefits of new drugs but also on their economic impact. To date no systematic evaluation of the medical benefits and economic effects of antiviral therapy for patients with CHC has been undertaken in Germany.
Therefore, the German Agency for Health Technology Assessment at DIMDI and the German Federal Ministry of Health and Social Security commissioned this health technology assessment (HTA). Its objectives were (1) to systematically review the evidence on effectiveness and cost-effectiveness of initial antiviral combination therapy in patients with CHC, (2) to develop a decision-analytic Markov model for treatment-naïve patients with CHC for the context of the German health care system and (3) to analyse the effectiveness and cost-effectiveness of initial antiviral therapy in patients with CHC and elevated ALTs in Germany.
Research Questions
All research questions of this study were based on a population of treatment naïve patients with chronic hepatitis C and elevated ALT levels. The following specific research questions were examined.
1. How does the effectiveness regarding sustained virological response rate (SVR) compare between the evaluated antiviral treatment strategies?
2. How does the effectiveness compare between the evaluated antiviral treatment strategies regarding the following long-term outcomes?
• Compensated liver cirrhosis
• Decompensated liver cirrhosis
• Hepatocellular carcinoma
• Liver transplantation
• CHC-related mortality
• Total mortality
• Quality-adjusted life expectancy
3. What is the incremental cost-effectiveness of each antiviral therapy in comparison to the next best strategy?
4. Which antiviral therapy can be recommended as standard therapy for the German health care context according to effectiveness and cost-effectiveness?
Methods
Systematic Review
Electronic databases, HTA-information networks, and bibliographic sources were systematically searched to identify randomised controlled trials (RCT), meta-analyses, or HTA reports that evaluated initial antiviral combination therapy in patients with CHC (see appendix for search code in Notes). The time horizon of the literature search was limited from 1990 to 2002. Study quality and transferability to the German context were assessed using instruments developed by the German Scientific Working Group Technology Assessment for Health Care [17], [18], [19]. The information was qualitatively summarised in evidence tables [20]. Results are reported in country-specific currencies. To facilitate comparison across countries, all results were additionally converted to US dollars (US$) of the index year of each study. As currency conversion methods in the individual studies were poorly described, we used exchange rates expressed as national currency units per US$ instead of applying Purchasing Power Parities (PPPs) [21].
A meta-analysis of randomised clinical trials on the medical effectiveness of antiviral combination therapy with peginterferon plus ribavirin was performed using random and fixed effects models (REM, FEM). Based on the standards of the Cochrane Collaboration [22], the pooled relative risk (RR) for the outcome "No Sustained Virological Response" with its 95% confidence interval (CI) was reported. Results were presented as forest plot.
Collaboration and HTA Expert Panel on Hepatitis C
During this HTA, collaboration was established with the following institutions:
• Cochrane Hepato-Biliary Group, Copenhagen Trial Unit, Centre for Clinical Intervention Research, Copenhagen, Denmark
• Canadian Coordinating Office for Health Technology Assessment (CCOHTA)
• Robert Koch-Institute, Berlin, Germany
• Federal Institute for Drugs and Medical Devices, Bonn, Germany
• National Association of Statutory Health Insurance Physicians, Cologne, Germany
• Hep-Net - German Network of Excellence for Viral Hepatitis
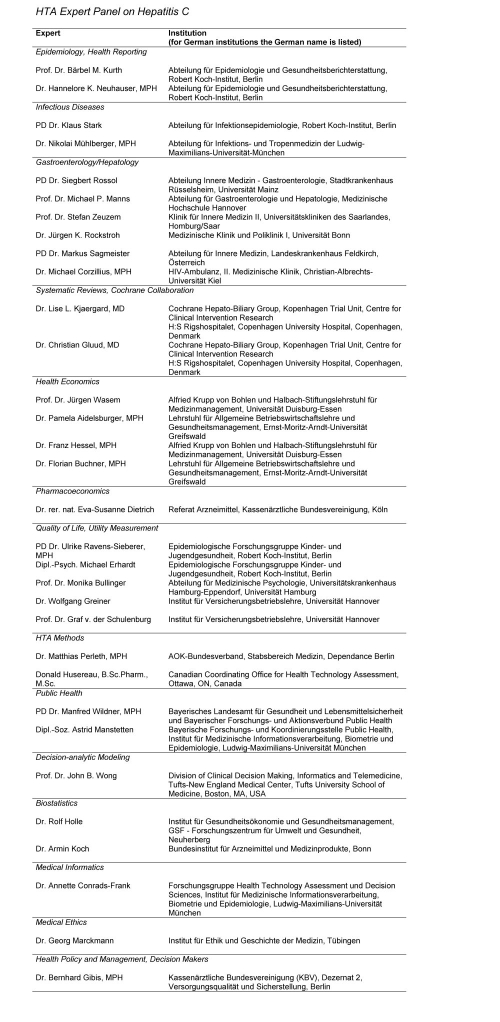
Furthermore, the HTA Expert Panel on Hepatitis C was established for this HTA. This interdisciplinary panel included members of the German Hepatitis C Model (GEHMO) Group and further experts from different areas who consulted information concerning actual unpublished data and studies and methodological issues. The list "HTA Expert Panel on Hepatitis C" (see Notes) gives the names, affiliations, and assigned areas of the expert panel members.
Decision Analysis
A modified version of the German Hepatitis C Model (GEHMO) was used. This model was designed to include pooled effectiveness data from meta-analyses, as well as benefits and costs, for employing different antiviral treatment strategies for patients with chronic hepatitis C. Pooled effectiveness data were derived from meta-analyses performed by the Hepato-Biliary Cochrane Group [23], [24] and additional meta-analyses were performed by the authors. GEHMO is a decision-analytic Markov model based on a previously published and validated Markov model for the natural history of disease [25], [26] and modified for the German health-care system and German hepatitis C-specific practice patterns.
The model was used to determine long-term morbidity, life expectancy, quality-adjusted life expectancy, lifetime costs, and discounted incremental cost-utility ratios (ICUR) of the following strategies: (1) no antiviral therapy, (2) interferon monotherapy (3x3 MU/week) for 48 weeks, (3) combination therapy with interferon (3x3 MU/week) and ribavirin (1000-1200 mg/day) for 48 weeks, and (4) combination therapy with peginterferon (180 μg/week for peginterferon alpha 2a; 1.5 μg/kg for peginterferon alpha 2b) plus ribavirin (800-1200 mg/day) for 48 weeks. According to the European guidelines [5], interferon monotherapy was stopped after 12 weeks and combination therapies were stopped after 24 weeks if no virological response was observed at this time. Dosing was based on European recommendations for patients with chronic hepatitis C and European drug approved labelling [5].
Natural history data were estimated from several published studies and have been described elsewhere [25], [26]. Histological classification as mild or moderate chronic hepatitis or compensated cirrhosis was defined by the modified histology activity index of Knodell [27], [28]. For the German context, demographic and clinical parameters as well as utilities were based on original data from a quality-of-life survey in CHC patients (n=428) [29], [30]. Utility data included empirically estimated relative reductions in short-term quality-of-life due to positive HCV status (2%) and adverse events during antiviral treatment (5% for interferon plus ribavirin and 10% for peginterferon plus ribavirin).
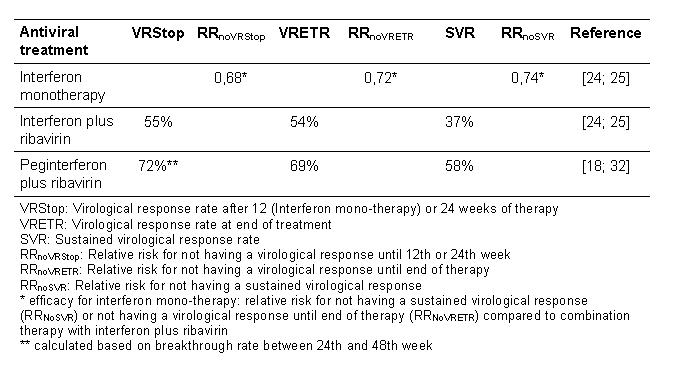
Our model included pooled short-term outcomes (overall sustained virological response rates and respective relative risks) from recently published RCTs and meta-analyses. Relative virological response rates of interferon monotherapy and combination therapy with interferon alpha plus ribavirin were based on a recently published meta-analysis [23] and a Cochrane Review [24]. We performed a meta-analysis to derive pooled virological response rates of combination therapy with peginterferon plus ribavirin published in two randomised clinical multicentre trials [15], [16] (see (Tab. 1)).
Table 1. Efficacy data used in the Markov model.
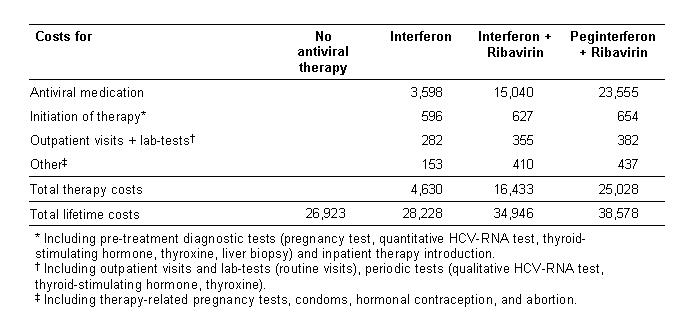
Direct annual costs were calculated based on frequencies of inpatient and outpatient visits, diagnostic and laboratory testing, medication, and procedures related to the specific health states (Tab. 2). Health resource utilisation frequencies were derived from a German expert panel (n = 10) and an economic survey in chronic hepatitis C patients (n = 196). Costs were derived from healthcare databases and currently applicable pharmaceutical prices of interferon alpha, peginterferon alpha, and ribavirin in Germany (Tab. 3).
Table 2. Annual treatment costs for HCV-related health states.
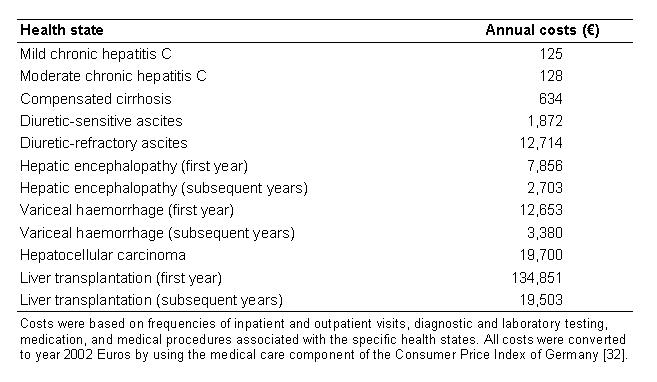
Table 3. Medication prices for antiviral treatment [60].
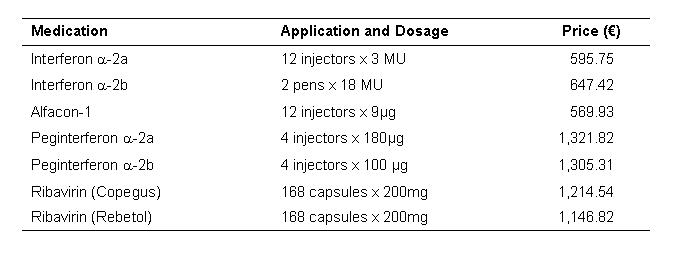
A 5% deduction from pharmaceutical prices for the proportion of persons insured by the social health insurance in Germany was performed. For modelling the costs of liver transplantation, a study [31] based on German patient data for the year 1993 was used. All costs were converted to year 2002 Euros (1 Euro = 1.95583 DM) by using the medical care component of the Consumer Price Index for Germany [32]. An annual discount rate of 3% was applied to costs and effectiveness based on international recommendations [33], [34] and varied in sensitivity analyses between 0% and 10% regarding German recommendations [35].
Model Validation
The decision model was validated on three levels:
• Technical validation: 'clean up' of the software program from potential programming bugs
• Internal validation: comparison of model predictions with epidemiological and clinical data used in the model
• External validation: comparison of model predictions with published epidemiological data not used in the model
The technical validation using different routine tests (e.g. setting SVR equal for all strategies, eliminating antiviral treatment costs, eliminating CHC-related mortality, etc.) yielded the expected results. In the internal validation, all data values used were reproduced exactly by the decision model (e.g. SVR rates, progression incidences, background mortality).
In the external validation, the incidence of developing compensated liver cirrhosis in patients with mild chronic hepatitis C was adjusted for the spontaneous HCV-remission rate of 31% in patients with acute HCV-infection [36]. The model predicted a 20-year incidence of developing compensated liver cirrhosis of 19% in patients with initial HCV-infection. This result is consistent with published data from prospective studies [4], [37].
As the spontaneous HCV remission rate and the incidence of liver cirrhosis have been extracted from different sources, using different values for spontaneous HCV remission could lead to a proportional deviation from the cirrhosis incidence used in the validation. However, different rates for spontaneous HCV remission would not influence results from this model because the target cohort of our analysis are patients with chronic hepatitis C.
Sensitivity Analyses
To assess the robustness of base-case results, univariate sensitivity analyses were performed for all model parameters based either on 95% confidence intervals or on ranges used in the literature. Costs were halved and doubled to obtain lower and upper limits. In addition to univariate sensitivity analyses, multivariate sensitivity analyses were performed on the entire set of disease progression rates. As it has been shown that the progression of hepatitis C observed in epidemiologic studies varies and strongly depends on the study design [8], we performed conservative sensitivity analyses with extremely low progression rates. Furthermore, we analysed a worst-case scenario using extremely conservative estimates for benefits and costs for the combination therapy with peginterferon and ribavirin.
Software
Decision analytic calculations were performed with DATA Pro for Health Care (TreeAge Software Inc., Williamstown, MA), SAS 8.1 (SAS Institute Inc., Cary, NC). Systat 10 (SPSS, Inc., Chicago, IL) was used for statistical analyses of primary data.
Results
Systematic Review
Twelve studies regarding the medical efficacy of combination therapy with interferon plus ribavirin compared to interferon monotherapy were included; herein 2 HTA reports [38], [39] 1 systematic Cochrane review [24], 2 meta-analyses [23], [40] and 7 controlled randomised clinical trials [41], [42], [43], [44], [13], [14], [45]. Two controlled randomised multicentre studies [15], [16] regarding medical efficacy of combination therapy with peginterferon and ribavirin compared to interferon plus ribavirin were identified and included.
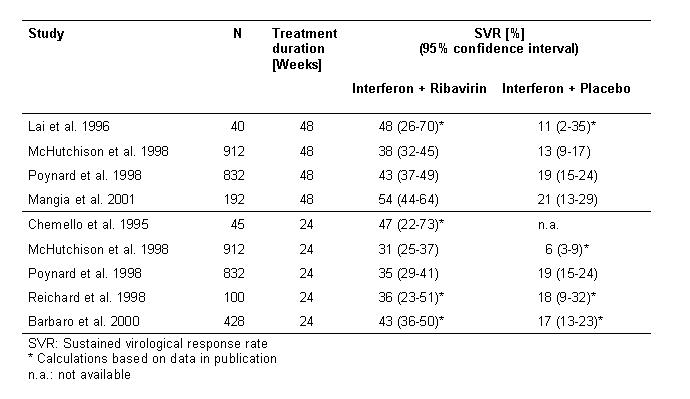
All included studies reported significantly higher SVR for combination therapy with interferon and ribavirin compared with interferon monotherapy (38-54% vs. 11-21%) (Tab. 4). Meta-analyses reported SVRs of 32-41% for interferon in combination with ribavirin compared to 8-16% for interferon monotherapy.
Table 4. Sustained virological response rates (SVR) for interferon plus ribavirin versus interferon monotherapy - primary studies.
For peginterferon combined with ribavirin, multicentre clinical trials reported SVRs of 54% vs. 47% (p-value 0.01) [16] and 56% vs. 44% (p-value < 0.001) [15] compared to standard combination therapy, respectively (Tab. 5). In a subgroup data analysis, one multicentre study [16] showed that patients treated with a dosage of 10.6 mg or more ribavirin per kg body weight had higher SVRs. Sixty-one percent of patients treated with peginterferon plus ribavirin compared to 48% patients treated with interferon plus ribavirin achieved a sustained virological response. The pooled relative risk for the outcome 'no sustained virological response' for the combination therapy with peginterferon plus ribavirin versus interferon plus ribavirin was 0.83 (95% CI 0.76-0.91 for fixed effects model and 0.75-0.91 for random effects model). Figure 1 (Fig. 1) shows the forest plot for the fixed effects model.
Table 5. Sustained virological response rates (SVR) for peginterferon plus ribavirin versus interferon plus ribavirin.
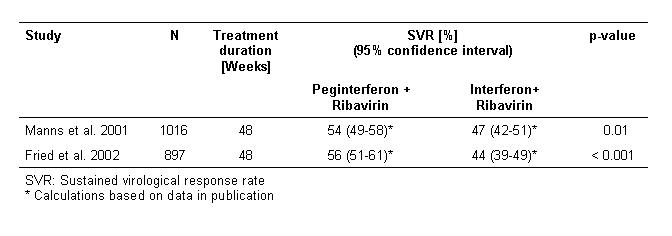
Figure 1. Meta-analysis.
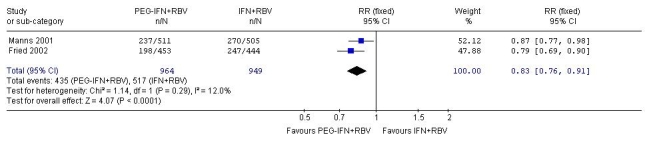
Forest Plot and pooled relative risk (RR) for no sustained virological response (SVR) for peginterferon plus ribavirin (PEG-IFN+RBV) versus interferon plus ribavirin (INF+RBV)
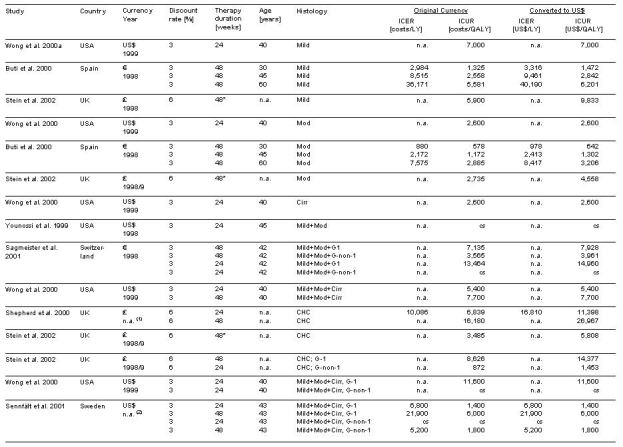
Seven studies including one HTA report [46], [47], [48], [39], [49], [50], [51] regarding cost-effectiveness of antiviral combination therapy with interferon and ribavirin in patients with chronic hepatitis C were identified in the search period of this HTA (January 1990 - December 2002), but no publications were found examining cost-effectiveness of antiviral combination therapy with peginterferon and ribavirin.
Incremental cost-effectiveness ratios varied over a wide range depending on discount rate, treatment duration, and population characteristics (Tab. 6). All studies considered antiviral therapy with interferon plus ribavirin seemed to be reasonably cost-effective.
Table 6. Discounted incremental cost-effectiveness-ratios (ICER) and discounted incremental cost-utility-ratios (ICUR) for combination therapy with interferon plus ribavirin (24 or 48 weeks) vs. interferon monotherapy (48 weeks) in treatment-naïve patients with chronic hepatitis C.
For full evidence tables and results on study quality and transferability see the online HTA, the full text of which is available at www.dimdi.de [52].
German Decision Analysis
Based on our decision analysis, initial antiviral therapy compared to no treatment in patients with chronic hepatitis C saved 1.1 life years for interferon monotherapy, 2.9 life years for interferon plus ribavirin, and 4.6 life years for peginterferon plus ribavirin (Tab. 7), and reduced the 20-year-risk of dying from liver failure by 12% for interferon alone, 29% for interferon plus ribavirin, and 46% for peginterferon plus ribavirin (Tab. 8). Compared to no antiviral therapy, interferon monotherapy saved 1.2 quality-adjusted life years (QALY), while combination therapy with interferon and ribavirin saved 3.0 QALYs and peginterferon plus ribavirin saved 4.8 QALYs.
Table 7. Undiscounted therapy costs and lifetime treatment costs in € (base-case analysis).
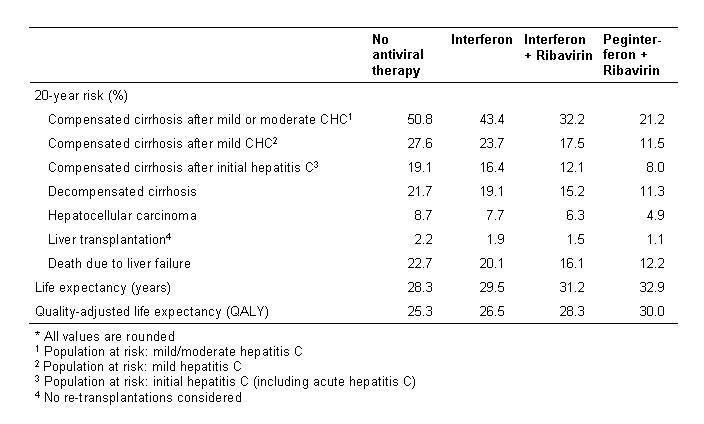
Table 8. Twenty-year-risk for clinical events, life expectancy, and quality-adjusted life expectancy (undiscounted).*.
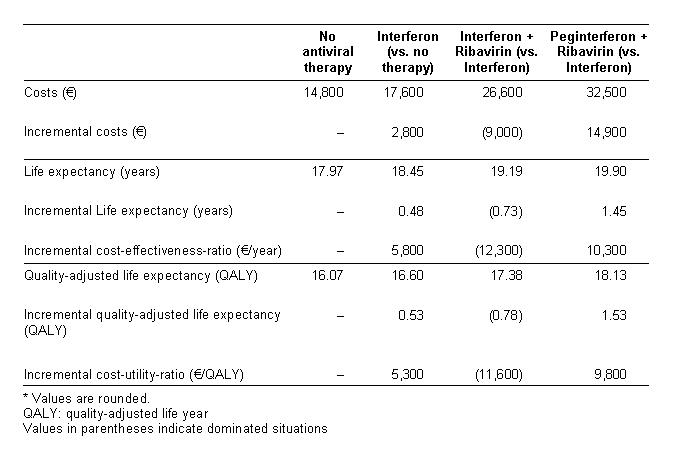
After discounting for future benefits, interferon monotherapy gained 0.53 QALYs with additional costs of € 2,800 resulting in an ICUR of € 5,300 per QALY compared to no antiviral therapy (Tab. 9). Moving from interferon monotherapy to interferon plus ribavirin was associated with 0.78 QALYs gained, additional costs of € 9,000, and an ICUR of 11,600 €/QALY. Compared to interferon monotherapy (as the next best non-dominated strategy), peginterferon plus ribavirin gained 1.53 QALYs and increased costs by € 14,900 yielding an ICUR of 9,800 €/QALY. Therefore, combination therapy with peginterferon plus ribavirin was the most effective treatment strategy and was more efficient than interferon plus ribavirin. To facilitate comparison with ICURs presented in Table 6 (Tab. 6), we converted the model-based ICURs for Germany to 2002 US dollars using the currency exchange rate (US$1 equals €1.07) [21]. When compared to interferon monotherapy, the ICURs of interferon plus ribavirin and peginterferon plus ribavirin were 10,800 US$/QALY and 9,200 US$/QALY, respectively.
Table 9. Base-case analysis: absolute and incremental discounted costs and efficacy, discounted incremental cost-effectiveness-ratio and discounted incremental cost-utility-ratio for different treatment strategies at annual 3% discount rate*.
In sensitivity analyses, results were robust when varying most relevant model parameters. Even when reducing SVR to 50%, combination therapy with peginterferon plus ribavirin was still the most effective strategy. Peginterferon plus ribavirin remained the most effective and cost-effective strategy when varying the proportion of patients with compensated cirrhosis from 0% to 52%, the proportion of male CHC-patients from 20% to 100%, or when body weight was increased by 20%.
Several sensitivity analyses were performed on progression rates. In a conservative scenario, the 20-year incidence of compensated cirrhosis was set to 7% as reported in a meta-analysis of results from community-based studies [8]. This scenario is conservative, because the study population of community-based studies included 38% of patients with normal ALT levels which is associated with a reduced risk of developing liver cirrhosis compared to our target population of CHC-patients with elevated ALT levels [53]. Figure 2 (Fig. 2) demonstrates the impact of progression on the ICUR of antiviral combination therapy. Even with a 20-year-incidence of cirrhosis of only 7%, as reported in community studies [8], peginterferon plus ribavirin was the most effective therapy and, with an ICUR of 21,100 €/QALY, was still reasonably cost-effective. When we further removed the 2% quality-of-life reduction due to HCV-infection in viral-positive CHC patients in this conservative scenario, the ICUR increased to 26,200 €/QALY.
Figure 2. Influence of disease progression rate on the incremental cost-utility-ratio of antiviral combination therapy.
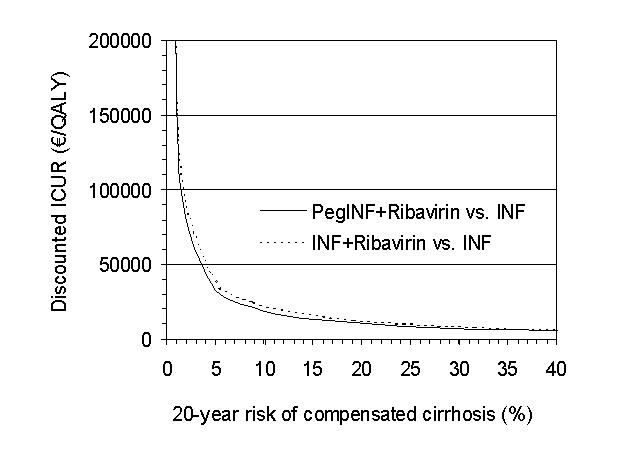
Disease progression is described as 20-year incidence of compensated liver cirrhosis in initial HVC-infected patients (including acute hepatitis C).
In the worst-case scenario, which was performed to obtain extremely conservative estimates for benefits (e.g., SVR) and costs for the combination therapy with peginterferon and ribavirin, peginterferon plus ribavirin was the most effective treatment strategy and resulted in an ICUR of 27,300 €/QALY compared to the next best non-dominated strategy (i.e., interferon monotherapy).
Discussion
In this health technology assessment, a systematic evaluation of the medical efficacy and cost-effectiveness of antiviral combination therapy as an initial treatment for patients with chronic hepatitis C was performed. In addition, a modified version of the German Hepatitis C Model (GEHMO) was applied to predict the 20-year risks of CHC-related liver diseases, life expectancy, quality-adjusted life expectancy, lifetime costs, and incremental cost-utility ratio for different antiviral treatment strategies and for the German health care context.
Several randomised trials [41], [42], [43], [44], [13], [14], [45] and meta-analyses [23], [24], [40] reported combination therapy with interferon plus ribavirin to be more efficient than interferon monotherapy (SVR: 32-54% vs. 8-21%). Two randomised multicentre studies [15], [16] reported a higher SVR for peginterferon plus ribavirin compared to combination therapy with interferon plus ribavirin (54-56% vs. 44-47%).
In terms of life expectancy and quality-adjusted life expectancy combination therapy with interferon plus ribavirin was more effective and also reasonably cost-effective when compared to interferon monotherapy, based on international cost-effectiveness studies [46], [47], [48], [39], [49], [50], [51].
In our decision analysis for the context of the German health care system, initial antiviral therapy with interferon and ribavirin compared to interferon monotherapy had a discounted ICUR of 11,600 €/QALY. Compared to interferon monotherapy, peginterferon plus ribavirin cost € 14,900 and gained 1.53 QALYs, resulting in an ICUR of 9,800 €/QALY. Therefore, combination therapy with peginterferon plus ribavirin was the most effective and cost-effective treatment strategy.
Compared to other well-accepted medical interventions, e.g., hemodialysis [54] or coronary artery bypass grafts [55] with ICURs of 50,000 to 60,000 €/QALY, combination therapy with peginterferon and ribavirin can be considered as cost-effective.
As is the case with all model-based cost-effectiveness analyses, ours has several limitations due to the availability of data on the natural history of chronic hepatitis C. The risk of progression to cirrhosis is especially controversially. In a recently published review of 57 studies on the natural history of hepatitis C [8], the authors classified the identified studies into four categories of study design and used regression analysis to derive pooled progression estimates for each category. The estimated 20-year risk of cirrhosis was 24% for post-transfusion cohorts, 22% for liver clinic series, 7% for community-based cohorts, and 4% for blood donors. Adjusting for demographic and clinical characteristics explained only a small part of the heterogeneity. It has been argued that biases such as referral bias and selection bias may explain the high cirrhosis risks in liver series and post-transfusion cohorts as well as the low estimates in blood donors [7]. The fraction of patients with elevated ALT levels varied between these different settings and was as low as 62% in the community-based studies [8].
The target population of our study was a patient cohort with elevated ALT values and a mix of different histological stages as observed in clinical trials and routine clinical practice in the absence of systematic screening. Post-transfusion studies were the only category that required the presence of clinical or biochemical hepatitis, and thus may be the category that best represents the advanced disease stage of the population we studied. However, transfusion may be associated with underlying chronic disease, which itself may influence the progression of hepatitis [7]. In community-based studies, most patients had normal ALT values, and some studies included patients with acute hepatitis C. Thus, these studies do not reflect the decision context and the population we studied. However, even after reducing the progression rates of our model to the extent that 20-year cirrhosis risk was only 7% (i.e., reflecting the community-based estimate), the ICUR for combination therapy with peginterferon plus ribavirin remained below 22,000 €/QALY. This indicated the robustness regarding the optimal choice among the evaluated strategies even under very conservative assumptions.
However, the results may be different for patients with normal ALT levels, with acute hepatitis C, or in populations in which a systematic screening for HCV was performed and, therefore, most cases were detected in a very early stage of the disease. For an evaluation in these populations, the decision model and its data must be adapted to the specific context. In particular, this means that even if future studies yield good SVRs in screened patients or patients with normal ALT values, long-term effectiveness or cost-effectiveness cannot be automatically inferred from these results without additional decision analyses.
For peginterferon plus ribavirin, the estimation of medical efficacy was based on only 2 studies [15], [16], the only published randomised clinical multicentre trials. However, the results of these two trials were similar, and our decision analysis results remained robust when varying the SVR in sensitivity analyses. More evidence should be retrieved from additional randomised clinical trials comparing combination therapy with peginterferon plus ribavirin to standard combination therapy.
Severe adverse events may occur more frequently in patients treated with peginterferon plus ribavirin than in patients treated with interferon plus ribavirin [15], [16]. As the absolute number of adverse events was small, and no utility data were available for each type of adverse event, we were unable to develop a micromodel for severe adverse events. Instead, we empirically estimated the overall relative reduction in quality of life due to different antiviral treatment regimens from the German CHC quality-of-life survey.
Our economic analysis likely underestimates disease-related costs for several reasons, and therefore likely underestimates treatment-related savings due to prevented future complications. First, we used variable costs and did not consider fixed costs nor costs due to productivity loss. Second, our model does not include the cost of future liver biopsies and further therapy for non-responders. Third, we did not consider histology normalisation in responders, nor reduced incidence of hepatocellular carcinoma in non-responders.
This analysis applied average age, gender distribution, genotype distribution, and histology to avoid potential biases related to patient-level variation in the different treatment groups of the trials and applied a consistent resource utilisation structure in the model and institutional assignment (where different institutions across Germany may vary in their economic efficiencies and accounting practices).
Country to country differences in sociodemographic structure, distribution of patient's clinical characteristics, utility profiles, resource utilisation, and prices make it difficult, if not impossible, to transfer the results of our qualitative review of economic evaluations to other health-care systems and countries [56], [57], [58], [19], [59]. However, the cost-effectiveness patterns for interferon and ribavirin in other industrialised countries were similar to the results derived from the German decision model. As none of the included economic evaluations examined the cost-utility ratio of peginterferon plus ribavirin, the German model results are currently the only data for this new treatment.
Future studies should examine the efficacy and the need for antiviral therapy in patients with normal ALT levels, with histological mild hepatitis C, and with certain risk and comorbidity profiles (e.g., HIV infection, intravenous drug users, haemophilia, etc.). All clinical trials used the sustained virological response rate as a surrogate marker for the clinical efficacy. Further epidemiological studies evaluating long-term clinical outcomes (e.g., incidence of cirrhosis, mortality) should be performed to provide more evidence on the long-term benefit of antiviral therapy.
Furthermore, further research is needed regarding the natural progression of the disease considering different prognostic factors. More observational long-term studies on the natural history of hepatitis C and the medical effectiveness of different therapeutic strategies should be performed, as well as prospective studies assessing actual cost for treatment and side effects in the routine health care setting.
Conclusions
This HTA suggests that initial combination therapy for chronic hepatitis C should prolong life, improve quality-adjusted life expectancy, and be cost-effective. The combination of pegylated interferon and ribavirin is currently the most effective and efficient antiviral treatment for CHC.
However, because not all chronic hepatitis C patients will develop progressive liver disease, a thorough assessment of the eligibility and appropriateness of treatment with combination therapy requires a careful discussion between patients and physicians. This discussion must consider the demographic and clinical characteristics of the patient and the trade-offs between the expected prognosis, side effects, and the willingness to consider antiviral treatment to prevent potential future liver complications.
Notes
Appendix: Literature Search Strategy
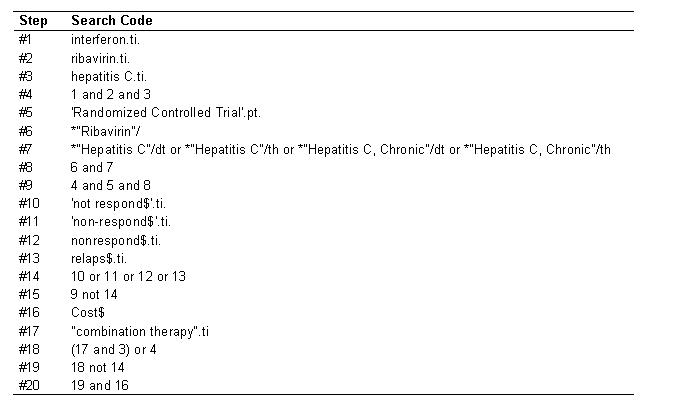
The code in (Tab. 10) represents the OVID search strategy used for identifying clinical and economic studies on antiviral combination therapy for chronic hepatitis C in MEDLINE and PreMEDLINE. Similar searches were performed in EMBASE, Cochrane Library, Best Evidence, NHS HTA databases (DARE, NHS EED, HTA), EconLit, Health Services Research Projects in Progress (HSRPROJ), Health Services/Technology Assessment (HSTAT), International Health Technology Assessment (IHTA), Catalog Online (CATLINE), and Science Citation Index (Science Citation Index Expanded, Social Science Citation Index and Arts & Humanities Citation Index). The HTA covered documents published between 1990 and December 2002. Line #15 and line #20 represent the final codes for studies on clinical effectiveness and economic studies, respectively.
Table 10. Search Strategy.
HTA Expert Panel on Hepatitis C
Table 11. HTA Expert Panel on Hepatitis C.
Acknowledgements
This work was commissioned and funded by the German Agency for Health Technology Assessment at the German Institute for Medical Documentation and Information (DAHTA@DIMDI), German Federal Ministry of Health and Social Security [Grant No. 05 / 01.2.].
References
- 1.WHO. Global Surveillance and control of hepatitis C. Report of a WHO Consultation organized in collaboration with the Viral Hepatitis Prevention Board, Antwerp, Belgium. J Viral Hepatitis. 1999;6:35–47. [PubMed] [Google Scholar]
- 2.Robert Koch Institut. Zur Situation bei wichtigen Infektionskrankheiten in Deutschland: Virushepatitis B und C bis zum Jahr 2001. Epidemiol Bull. 2002;44:360–376. [Google Scholar]
- 3.Schreier E, Höhne M. Hepatitis C - Epidemiologie und Prävention. Bundesgesundheitsblatt. 2001;44:554–561. [Google Scholar]
- 4.Alter HJ, Seeff LB. Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis. 2000;20:17–35. doi: 10.1055/s-2000-9505. [DOI] [PubMed] [Google Scholar]
- 5.European Association for the Study of the Liver. EASL International Consensus Conference on Hepatitis C. Paris, 26-28, February 1999, Consensus Statement. J Hepatol. 1999;30:956–961. [PubMed] [Google Scholar]
- 6.Di Bisceglie AM, Goodman ZD, Ishak KG, Hoofnagle JH, Melpolder JJ, Alter HJ. Long-term clinical and histopathological follow-up of chronic posttransfusion hepatitis. Hepatology. 1991;14:969–974. doi: 10.1016/0270-9139(91)90113-a. [DOI] [PubMed] [Google Scholar]
- 7.Dore GJ, Freeman AJ, Law M, Kaldor JM. Is severe liver disease a common outcome for people with chronic hepatitis C. J Gastroenterol Hepatol. 2002;17:423–430. doi: 10.1046/j.1440-1746.2002.02730.x. [DOI] [PubMed] [Google Scholar]
- 8.Freeman AJ, Dore GJ, Law MG, Thorpe M, Von Overbeck J, Lloyd AR, Marinos G, Kaldor JM. Estimating progression to cirrhosis in chronic hepatitis C virus infection. Hepatology. 2001;34:809–816. doi: 10.1053/jhep.2001.27831. [DOI] [PubMed] [Google Scholar]
- 9.Hopf U, Moller B, Kuther D, Stemerowicz R, Lobeck H, Ludtke-Handjery A, Walter E, Blum HE, Roggendorf M, Deinhard F. Long-term follow-up of posttransfusion and sporadic chronic hepatitis non-A, non-B and frequency of circulating antibodies to hepatitis C virus (HCV) J Hepatol. 1990;10:69–76. doi: 10.1016/0168-8278(90)90075-3. [DOI] [PubMed] [Google Scholar]
- 10.Koretz RL, Abbey H, Coleman E, Gitnick G. Non-A, non-B post-transfusion hepatitis. Looking back in the second decade. Ann Intern Med. 1993;119:110–115. doi: 10.7326/0003-4819-119-2-199307150-00003. [DOI] [PubMed] [Google Scholar]
- 11.Mattsson L, Sonnerborg A, Weiland O. Outcome of acute symptomatic non-A, non-B hepatitis: a 13-year follow-up study of hepatitis C virus markers. Liver. 1993;13:274–278. doi: 10.1111/j.1600-0676.1993.tb00644.x. [DOI] [PubMed] [Google Scholar]
- 12.Tremolada F, Casarin C, Alberti A, Drago C, Tagger A, Ribero ML, Realdi G. Long-term follow-up of non-A, non-B (type C) post-transfusion hepatitis. J Hepatol. 1992;16:273–281. doi: 10.1016/s0168-8278(05)80657-9. [DOI] [PubMed] [Google Scholar]
- 13.McHutchison JG, Gordon SC, Schiff ER, Shiffman ML, Lee WM, Rustgi VK, Goodman ZD, Ling MH, Cort S, Albrecht JK. Interferon alfa-2b alone or in combination with ribavirin as initial treatment for chronic hepatitis C. Hepatitis Interventional Therapy Group. N Engl J Med. 1998;339:1485. doi: 10.1056/NEJM199811193392101. [DOI] [PubMed] [Google Scholar]
- 14.Poynard T, Marcellin P, Lee SS, Niederau C, Minuk GS, Ideo G, Bain V, Heathcote J, Zeuzem S, Trepo C, Albrecht J. Randomised trial of interferon alpha2b plus ribavirin for 48 weeks or for 24 weeks versus interferon alpha2b plus placebo for 48 weeks for treatment of chronic infection with hepatitis C virus. International Hepatitis Interventional Therapy Group (IHIT) Lancet. 1998;352:1426–132. doi: 10.1016/s0140-6736(98)07124-4. [DOI] [PubMed] [Google Scholar]
- 15.Fried MW, Shiffman ML, Reddy KR, Smith C, Marinos G, Goncales FL, Jr, Haussinger D, Diago M, Carosi G, Dhumeaux D, Craxi A, Lin A, Hoffman J, Yu J. Peginterferon Alfa-2a plus Ribavirin for Chronic Hepatitis C Virus Infection. N Engl J Med. 2002;347:975–982. doi: 10.1056/NEJMoa020047. [DOI] [PubMed] [Google Scholar]
- 16.Manns MP, McHutchison JG, Gordon SC, Rustgi VK, Shiffman M, Reindollar R, Goodman ZD, Koury K, Ling M, Albrecht JK. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 2001;358:958–965. doi: 10.1016/s0140-6736(01)06102-5. [DOI] [PubMed] [Google Scholar]
- 17.Lühmann D, Siebert U, Droste S, von der Leyen U, Perleth M German Scientific Working Group Technology Assessment for Health Care, editor. Toolkit. Informationsmaterial für Verfasser von HTA-Berichten. Hannover: 1999. Konzeption zur Anpassung und Erstellung von Technologiebewertungen in der deutschen Arbeitsgruppe Verfahrensbewertung in der Medizin. [Google Scholar]
- 18.Siebert U, Behrend C, Mühlberger N, Wasem J, Greiner W, v. d. Schulenburg JM, et al. Entwicklung eines Kriterienkataloges zur Beschreibung und Bewertung ökonomischer Evaluationsstudien in Deutschland. In: Leidl R, v. d. Schulenburg JM, Wasem J, editors. Ansätze und Methoden der ökonomischen Evaluation - eine internationale Perspektive. Baden-Baden: Nomos; 1999. pp. 156–170. [Google Scholar]
- 19.Welte R, Leidl R. Übertragung der Ergebnisse ökonomischer Evaluationsstudien aus dem Ausland auf Deutschland: Probleme und Lösungsansätze. In: Leidl R, v. d. Schulenburg JM, Wasem J, editors. Ansätze und Methoden der ökonomischen Evaluation - eine internationale Perspektive. Baden-Baden: Nomos; 1999. pp. 171–202. [Google Scholar]
- 20.Siebert U, Mühlberger N, Behrend C, Wasem J. Technology assessment for health care: a tool for explicitly evaluating economic studies. GMDS-Tagungsband der 44. Jahrestagung der GMDS; September 1999; Heidelberg. München: MMV Medizin; 1999. [Google Scholar]
- 21.Organisation for Economic Co-operation and Development. OECD Health Data 2003: a comparative analysis of 30 countries. Paris: OECD; 2000. [Google Scholar]
- 22.Cochrane Collaboration. Cochrane Collaboration open learning material for reviewers. 2002 Available from: http://www.cochrane-net.org/openlearning/HTML/mod11-4.htm.
- 23.Kjaergard LL, Krogsgaard K, Gluud C. Interferon alfa with or without ribavirin for chronic hepatitis C: systematic review of randomised trials. BMJ. 2001;323:1151–1155. doi: 10.1136/bmj.323.7322.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kjaergard LL, Krogsgaard K, Gluud C. Ribavirin with or without alpha interferon versus no intervention, placebo or alpha interferon for chronic hepatitis C (Cochrane Review) Cochrane Database Syst Rev. 2002;1:CD002234. doi: 10.1002/14651858.CD002234. [DOI] [PubMed] [Google Scholar]
- 25.Bennett WG, Inoue Y, Beck JR, Wong JB, Pauker SG, Davis GL. Estimates of the cost-effectiveness of a single course of interferon-alpha 2b in patients with histologically mild chronic hepatitis. Ann Intern Med. 1997;127:855–865. doi: 10.7326/0003-4819-127-10-199711150-00001. [DOI] [PubMed] [Google Scholar]
- 26.Wong JB, Davis GL, Pauker SG. Cost-effectiveness of ribavirin/interferon alfa-2b after interferon relapse in chronic hepatitis C. Hepatology. 1998;28 (Suppl 4, Pt 2):591A. doi: 10.1016/s0002-9343(00)00303-x. [DOI] [PubMed] [Google Scholar]
- 27.Desmet VJ, Gerber M, Hoofnagle JH, Manns M, Scheuer PJ. Classification of chronic hepatitis: diagnosis, grading, and staging. Hepatology. 1994;19:1513–1520. [PubMed] [Google Scholar]
- 28.Knodell RG, Ishak KG, Black WC, Chen TS, Craig R, Kaplowitz N, Kiernan TW, Wollman J. Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology. 1981;1:431–435. doi: 10.1002/hep.1840010511. [DOI] [PubMed] [Google Scholar]
- 29.Siebert U, Greiner W, Ravens-Sieberer U, Sroczynski G, Wong J, von der Schulenburg J, et al. Preference-based quality-of-life values in patients with chronic hepatitis C: Results from the German hepatitis C quality-of-life study. J Hepatol. 2003;38 Suppl 2:596. [Google Scholar]
- 30.Siebert U, Ravens-Sieberer U, Greiner W, Sroczynski G, Wong JB, Kuntz KM, et al. Patient-based health-related quality of life in different health stages of chronic hepatitis C [Abstract] Hepatology. 2001;34 (pt 2):222A. [Google Scholar]
- 31.Greiner W. Ökonomische Evaluation von Gesundheitsleistungen: Fragestellungen, Methoden und Grenzen dargestellt am Beispiel der Transplantationsmedizin. Baden-Baden: Nomos-Verlags-Gesellschaft; 1999. [Google Scholar]
- 32.Statistisches Bundesamt. Preisindex für Arzt-, Krankenhaus- und sonstige Dienstleistungen für die Gesundheitspflege. 2000. [Google Scholar]
- 33.Drummond MF, et al. Methods for the economic evaluation of health care programmes. 2nd ed. New York: Oxford University Press; 1997. [Google Scholar]
- 34.Gold MR, et al., editors. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 35.Hannoveraner Konsensus Gruppe. Deutsche Empfehlungen zur gesundheitsökonomischen Evaluation - Revidierte Fassung des Hannoveraner Konsensus. Gesundheitsökonomie und Qualitätsmanagement. 1999;4:A62–A65. [Google Scholar]
- 36.Alter MJ, Kruskon-Moran D, Nainan OV, McQuillan GM, Gao F, Moyer LA, Kaslow RA, Margolis HS. The prevalence of hepatitis C virus infection in the United States 1988 through 1994. N Engl J Med. 1999;341:556–562. doi: 10.1056/NEJM199908193410802. [DOI] [PubMed] [Google Scholar]
- 37.Liang TJ, Rehermann B, Seeff LB, Hoofnagle JH. Pathogenesis, natural history, treatment, and prevention of hepatitis C. Ann Intern Med. 2000;132:296–305. doi: 10.7326/0003-4819-132-4-200002150-00008. [DOI] [PubMed] [Google Scholar]
- 38.Gebo KA, et al. Management of chronic hepatitis C. Prepared by the John Hopkins Evidence-based Practice Center under Contract No 290-97-0006. Rockeville, MD: Agency for Healthcare Research and Quality; 2002. (Evidence report/technology assessment, no. 60. AHRQ publication, no. 02-E030). [Google Scholar]
- 39.Shepherd J, Waugh N, Hewitson P. Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review. Health Technol Assess. 2000;4(33):1–67. [PubMed] [Google Scholar]
- 40.McHutchison JG, Poynard T. Combination therapy with interferon plus ribavirin for the initial treatment of chronic hepatitis C. Semin Liver Dis. 1999;19 Suppl 1:57–65. [PubMed] [Google Scholar]
- 41.Barbaro G, Di Lorenzo G, Soldini M, Giancaspro G, Pellicelli A, Grisorio B, Barbarini G. Evaluation of long-term efficacy of interferon alpha-2b and ribavirin in combination in naive patients with chronic hepatitis C: an Italian multicenter experience. Ribavirin-Interferon in Chronic Hepatitis Italian Group Investigators. J Hepatol. 2000;33:448–455. doi: 10.1016/s0168-8278(00)80281-0. [DOI] [PubMed] [Google Scholar]
- 42.Chemello L, Cavalletto L, Bernardinello E, Guido M, Pontisso P, Alberti A. The effect of interferon alfa and ribavirin combination therapy in naive patients with chronic hepatitis C. J Hepatol. 1995;23 Suppl 2:8–12. [PubMed] [Google Scholar]
- 43.Lai MY, Kao JH, Yang PM, Wang JT, Chen PJ, Chan KW, Chu JS, Chen DS. Long-term efficacy of ribavirin plus interferon alfa in the treatment of chronic hepatitis C. Gastroenterology. 1996;111:1307–1312. doi: 10.1053/gast.1996.v111.pm8898645. [DOI] [PubMed] [Google Scholar]
- 44.Mangi A, Villani MR, Minerva N, Leandro G, Bacca D, Cela M, Carretta V, Attino V, Ventrella F, Giangaspero F, Andriulli A. Efficacy of 5 MU of interferon in combination with ribavirin for naive patients with chronic hepatitis C virus: a randomized controlled trial. J Hepatol. 2001;34:441–446. doi: 10.1016/s0168-8278(00)00024-6. [DOI] [PubMed] [Google Scholar]
- 45.Reichard O, Norkrans G, Fryden A, Braconier JH, Sonnerborg A, Weiland O. Randomised, double-blind, placebo-controlled trial of interferon alpha-2b with and without ribavirin for chronic hepatitis C. The Swedish Study Group. Lancet. 1998;351(9096):83–87. doi: 10.1016/s0140-6736(97)06088-1. [DOI] [PubMed] [Google Scholar]
- 46.Buti M, Casado M, Fosbrook L, Wong JB, Esteban R. Cost-effectiveness of combination therapy for naive patients with chronic hepatitis C. J Hepatol. 2000;33:651–658. doi: 10.1034/j.1600-0641.2000.033004651.x. [DOI] [PubMed] [Google Scholar]
- 47.Sagmeister M, Wong JB, Mullhaupt B, Renner E. A pragmatic and cost-effective strategy of a combination therapy of interferon alpha-2b and ribavirin for the treatment of chronic hepatitis C. Eur J Gastroenterol Hepatol. 2001;13:483–488. doi: 10.1097/00042737-200105000-00004. [DOI] [PubMed] [Google Scholar]
- 48.Sennfalt K, Reichard O, Hultkrantz R, Wong JB, Jonsson D. Cost-effectiveness of interferon alfa-2b with and without ribavirin as therapy for chronic hepatitis C in Sweden. Scand J Gastroenterol. 2001;36:870–876. doi: 10.1080/003655201750313414. [DOI] [PubMed] [Google Scholar]
- 49.Stein K, Rosenberg W, Wong J. Cost effectiveness of combination therapy for hepatitis C: a decision analytic model. Gut. 2002;50:253–258. doi: 10.1136/gut.50.2.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wong JB, Poynard T, Ling MH, Albrecht JK, Pauker SG. Cost-effectiveness of 24 or 48 weeks of interferon alpha-2b alone or with ribavirin as initial treatment of chronic hepatitis C. International Hepatitis Interventional Therapy Group. Am J Gastroenterol. 2000;95:1524–1530. doi: 10.1111/j.1572-0241.2000.2089_1.x. [DOI] [PubMed] [Google Scholar]
- 51.Younossi ZM, Singer ME, McHutchison JG, Shermock KM. Cost effectiveness of interferon alpha2b combined with ribavirin for the treatment of chronic hepatitis C. Hepatology. 1999;30:318–324. doi: 10.1002/hep.510300518. [DOI] [PubMed] [Google Scholar]
- 52.Siebert U, Sroczynski G German Hepatitis C Model (GEHMO) Group. Antivirale Therapie bei Patienten mit chronischer Hepatitis C in Deutschland. Medizinische und ökonomische Evaluation der initialen Kombinationstherapie mit Interferon/Peginterferon und Ribavirin] [Antiviral therapy in patients with chronic hepatitis C in Germany. Clinical and economic evaluation of the initial combination therapy with interferon/peginterferon and ribavirin]. Köln: German Institute for Medical Documentation and Information; 2003. (HTA Series of the German Institute for Medical Documentation and Information, commissioned by the Federal Ministry of Health and Social Security). (Ger). (in print) [Google Scholar]
- 53.Marcellin P, Asselah T, Boyer N. Fibrosis and disease progression in hepatitis C. Hepatology. 2002;36 (5 Suppl 1):47–56. doi: 10.1053/jhep.2002.36993. [DOI] [PubMed] [Google Scholar]
- 54.Weinstein MC. High-priced technology can be good value for money. Ann Intern Med. 1999;130:857–858. doi: 10.7326/0003-4819-130-10-199905180-00021. [DOI] [PubMed] [Google Scholar]
- 55.Wong JB, Sonnenberg FA, Salem DN, Pauker SG. Myocardial revascularization for chronic stable angina. Analysis of the role of percutaneous transluminal coronary angioplasty based on data available in 1989. Ann Intern Med. 1990;113:852–871. doi: 10.7326/0003-4819-113-11-852. [DOI] [PubMed] [Google Scholar]
- 56.Baltussen R, Ament A, Leidl R. Making cost assessments based on RCTs more useful to decision-makers. Health Policy. 1996;37:163–183. doi: 10.1016/s0168-8510(96)90023-8. [DOI] [PubMed] [Google Scholar]
- 57.Drummond MF, Bloom BS, Carrin G, Hillman AL, Hutchings HC, Knill-Jones RP, de Pouvourville G, Torfs K. Issues in the cross-national assessment of health technology. Int J Technol Assess Health Care. 1992;8:671–682. doi: 10.1017/s0266462300002361. [DOI] [PubMed] [Google Scholar]
- 58.Haycox A, Dubois D, Butterworth M. Customising an international disease management model to the needs of individual countries. Application to upper gastrointestinal disease. Pharmacoeconomics. 1998;14 Suppl 2:39–56. doi: 10.2165/00019053-199814002-00005. [DOI] [PubMed] [Google Scholar]
- 59.Willke RJ, Glick HA, Polsky D, Schulman K. Estimating country-specific cost-effectiveness from multinational clinical trials. Health Econ. 1998;7:481–493. doi: 10.1002/(sici)1099-1050(199809)7:6<481::aid-hec353>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 60.Rote Liste Service GmbH. Rote Liste: Arzneimittelverzeichnis für Deutschland. Aulendorf: Editio Cantor Verlag; 2002. [Google Scholar]