Abstract
Background: Evidence-based patient information (EBPI) is a prerequisite for informed decision-making. However, presentation of EBPI may lead to irrational reactions causing avoidance, minimisation and devaluation of the information.
Objective: To explore whether the theory of cognitive dissonance is applicable to medical decision-making and useful to explain these phenomena.
Setting and participants: 261 volunteers from Hamburg (157 women), ≥50 years old without diagnosis of colorectal cancer.
Design and variables: Within an experiment we simulated information seeking on colorectal cancer screening. Consumers’ attitudes towards screening were surveyed using a rating scale from -5 (participate in no way) to +5 (participate unconditionally) (independent variable). Using a cover story, participants were asked to sort 5 article headlines according to their reading preferences. The headlines simulated the pro to contra variety of contents to be found in print media about colorectal cancer screening. The dependent variable was the sequence of article headlines.
Results: Participants were very much in favour of screening with scores for faecal occult blood test of 4.0 (0.1) and for colonoscopy 3.3 (0.1). According to our hypothesis we found statistically significant positive correlations between the stimuli in favour of screening and attitudes and significant negative correlations between the stimuli against screening and attitudes.
Conclusion: The theory of cognitive dissonance is applicable to medical decision-making. It may explain some phenomena of irrational reactions to evidence-based patient information.
Keywords: evidence-based patient information, cognitive dissonance, information seeking
Abstract
Hintergrund: Evidenzbasierte Patienteninformation (EBPI) ist eine Voraussetzung für die informierte Entscheidung. Jedoch kann die Präsentation von EBPI irrationale Reaktionen hervorrufen, die zur Vermeidung, Minimierung und Abwertung der Information führen kann.
Zielsetzung: Überprüfung, ob die Theorie der kognitiven Dissonanz im Bereich des medical decision making anwendbar ist und hilft, diese Phänomene zu erklären.
Setting und Teilnehmer: 261 freiwillige Hamburger (157 Frauen), ≥50 Jahre alt ohne Diagnose eines kolorektalen Karzinoms.
Design und Variable: Wir simulierten die Informationssuche zum Screening auf kolorektale Karzinome in einem Experiment. Die Einstellung der Verbraucher zum Screening wurde anhand einer Skala von -5 (in keinem Fall teilnehmen) bis +5 (in jedem Fall teilnehmen) (unabhängige Variable) erhoben. Eingebunden in eine Coverstory wurden die Teilnehmer gebeten 5 Artikelüberschriften nach ihrer Lesepräferenz zu sortieren. Die Überschriften simulierten die in Printmedien vorkommende Varianz an pro- und kontra-Inhalten zum kolorektalen Screening. Die Sequenz der sortierten Artikelüberschriften stellte die abhängige Variable dar.
Ergebnisse: Die Teilnehmer, die sehr stark pro kolorektales Screening eingestellt waren, zeigten Werte für den Okkultbluttest von 4.0 (0.1) und für das Koloskopiescreenig 3.3 (0.1). In Übereinstimmung mit unserer Hypothese fanden wir statistisch signifikante positive Korrelationen zwischen den Stimuli pro Screening und den Einstellungen sowie signifikante negative Korrelationen zwischen den Stimuli gegen Screening und den Einstellungen.
Fazit: Die Theorie der kognitiven Dissonanz kann im Bereich des medical decision making angewandt werden. Sie kann einige der Phänomene irrationalen Verhaltens gegenüber evidenzbasierter Patienteninformation erklären.
Background
Evidence-based patient information (EBPI) is essential for informed choice and shared decision-making [1], [2]. Various criteria for the quality of contents and the development process of EBPI have been described in scientific and ethical literature [3], [4], [5], [6]. However, an agreement on the definition of evidence-based patient information is still lacking [7]. Therefore, little is known about how and to what extent consumers perceive such information.
Results of studies that have explored the effects of decision aids or patient information are hardly applicable since mostly they focused on the analysis of information material and development processes. Some studies that reported irrational reactions of patients towards information did not appreciate these phenomena adequately [8]. In psychology information processing is widely accepted as a constructivist process. But, in medical decision-making this aspect is still not sufficiently taken into account [9]. Farrell et al. identified 7 common beliefs that significantly influence the decision on participation in PSA (prostate specific antigen) screening: "… fear of cancer, relevance of salient anecdotes and analogies, distrust of statistics, enthusiasm for “prevention”, protection from “bad luck”, faith in science and valuating PSA as knowledge for its own sake" [10]. Uptake in PSA screening was high by study participants despite their understanding that there was no evidence for a benefit [10]. Even physicians may experience cognitive dissonance after being given evidence-based information [11]. In a recent focus group study we have presented EBPI on colorectal cancer screening to healthy volunteers who mainly opted for traditional information that guides them. When they were nevertheless given EBPI we observed phenomena of not noticing, minimising and devaluating the information [12]. The effort to enhance consumers’ autonomy in medical decision-making by providing evidence-based information might provoke such phenomena.
In social psychology, the theory of cognitive dissonance was applied to explain phenomena in information processing [13], [14]. The theory is based on the assumption that people taking up information try to achieve consistency between cognitive elements. Cognitive dissonance is closely connected with aversive emotions, which motivates different behavioural strategies to reduce dissonance. One paradigm of the theory (selective exposure) predicts that people seek consonant and avoid dissonant information [13], [15], [16].
This study explored whether the theory of cognitive dissonance is applicable to the context of medical decision-making and therefore appropriate to explain the phenomena of information avoidance. According to the theory, we experimentally simulated information seeking particularly for colorectal cancer screening.
Methods
Participants and design
We included people of the target group for colorectal cancer screening: ≥50 years old, without diagnosis of colorectal cancer, without known genetic disposition to colorectal cancer. Inclusion criteria were checked immediately after the experiment in order to conceal the main goal of the study. Exclusion criteria were participation in an earlier focus group study on EBPI and for the 2nd part of the experiment we excluded those who participated in the 1st part [12].
Since information seeking is a complex issue we chose an experiment as study design to control for potential confounders. In order to test our hypotheses, whether information seeking is performed according to the theory of cognitive dissonance, we had to simulate information seeking. The choice of test persons will show whether the information was chosen consonant or dissonant to existing attitudes.
Recruitment
First sample
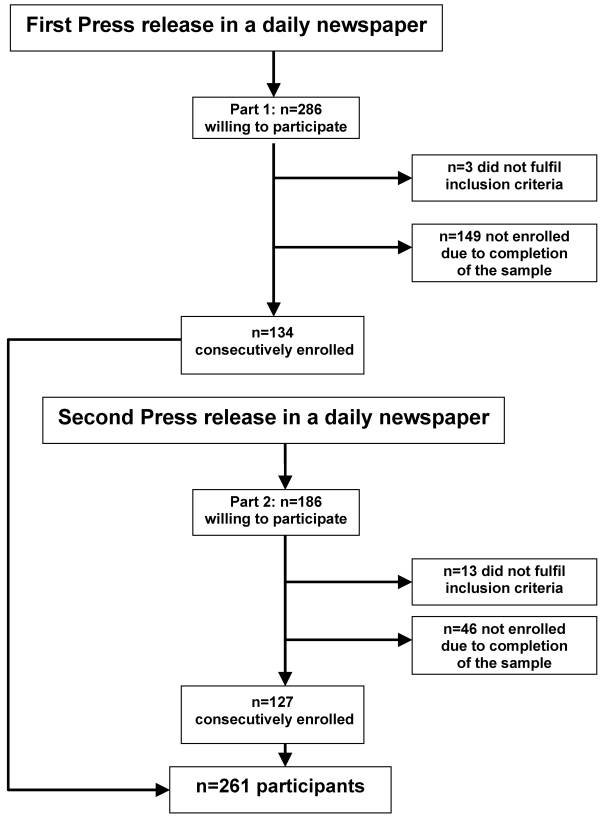
Figure 1 shows the flow of recruitment. We consecutively included people who responded to our announcement in a local newspaper in Hamburg until the sample was completed. Participants of this first part of the experiment were only informed that the study dealt with the subject "health information“. We did not focus the specific topic of colorectal cancer screening to avoid selection bias. However, consumers were aware of our institutional background of health sciences. Appointments were made within the first telephone call. Participants also received a written invitation after the1st telephone call. After the experiment each person received € 20 as allowance.
Figure 1. Flow of recruitment.
Second sample
Because the announcement in the local newspaper did not achieve sufficient variance in attitudes towards screening we recruited a second sample. This time, participants were not aware of our institutional background. As address, we used the University of Hamburg without further details, and we installed a new phone number exclusively for recruitment. The content of the press release was modified. Participants were told that the study was about information in media. We also changed the place for the experiment to prevent consumers from realizing an affiliation with our institute.
Procedure and variables
The experiments were carried out between November 2003 and March 2004 at the University of Hamburg, Germany. Study conditions were standardized in terms of room setup and procedure. We simulated the "pro" to "contra" variety of information contents to be found in print media about colorectal cancer screening. The experiments lasted about 15 minutes for each participant and were performed by a single researcher (AS) using a face-to-face approach. Duration of the experiments was not limited. To disguise the study question, we initially surveyed data on participants’ sources of information seeking on health topics. Afterwards we collected data on previous uptake of a variety of screening tests including colorectal cancer screening.
A questionnaire was used to survey attitudes towards colorectal cancer screening and for further screening tests. Attitude was used as the independent variable. Participants rated what kind of advice they would give to a close friend who asked whether he or she should participate in screening using a scale from -5 (participate in no way) to +5 (participate unconditionally). This procedure results in answers that are similar to personal attitudes but free of irrelevant motivations [12]. According to theory the impact of attitude on behaviour is defined by an addition of the extent of its value and its strength, which usually is operationalised by resistance, stability or subjective rating. Due to our study design, strength of attitude is measured as control, using a subjective rating [17], [18].
We introduced the main task of the experiment with a cover story. Participants were asked to imagine they were waiting in an office to handle anything like identity card or passport application. Further, we told them that they find 5 newspaper articles. Since they do not know how long they will have to wait, they have to decide which article they like to begin with. The articles might be gone by the time they get out of the office. The available articles are presented with their headlines only. Then, participants had to establish a sequence of these 5 article headlines that correspond to their reading preference. The chosen order was noted. The sequence of article headlines is the dependent variable.
After the experiment participants were fully informed about our study.
Stimulus materials
We developed a set of 10 article headlines to represent the different stimuli from very strongly in favour to very strongly against colorectal cancer screening. All material was pre-tested with lay people (n=10). We isolated five eligible headlines, which were again pre-tested with other lay people (n=10). In order to test feasibility, lay people were asked to interpret the headlines and than sort them according to the headlines statements in terms of strongly in favour or strongly against screening. A think-aloud protocol helped to identify and remove language problems and conceptual constraints. The final five headlines were as follows:
A. Participation in screening reduces death rate: colorectal cancer is the second leading cause of death among cancer diseases. (Very strongly in favour)
B. Colorectal cancer screening – that is how you can easily and effectively lower death rate. (Strongly in favour)
C. Up-to-date information about benefits and harms of colorectal cancer screening. (Neutral)
D. Experts advise against uncritical use of colorectal cancer screening. (Strongly against)
E. Beware colorectal cancer screening: the test carries the danger of severe side-effects. (Very strongly against)
Data analysis
Pearson-correlations were calculated for the main question of our study, the relation between the independent variable (attitude towards colorectal cancer screening: faecal occult blood test (FOBT) and/or colonoscopy) and the dependent variable (sequence of article headlines). Attitudes towards screening tests were surveyed on a scale from -5 to +5 and expressed as mean values (SD). Calculations were performed using SPSS. A p-value <.05 was regarded as significant.
Hypotheses
The application of the theory of cognitive dissonance will show correlations between attitudes and stimuli.
Therefore, participants with an attitude in favour of uptake of colorectal cancer screening choose information, which supports the attitude in favour of screening. Participants with an attitude against uptake of colorectal cancer screening choose information, which supports the attitude against screening.
Sample size calculation
We hypothesized that the attitude towards colorectal cancer screening is unequally distributed within the target group (in favour of screening is about twice as frequent as critical towards screening). We wanted to detect a difference of a three-quarter standard deviation in information seeking between the two groups (in favour of screening or against screening). In a sample of 125 persons (100 + 25 assumed drop outs), the hypothesized difference could be detected with a power of 80% at a two tailed α of 0.05.
Ethics Committee
The study was approved by the ethics committee of the Hamburg chamber of physicians and the regional data protection office.
Results
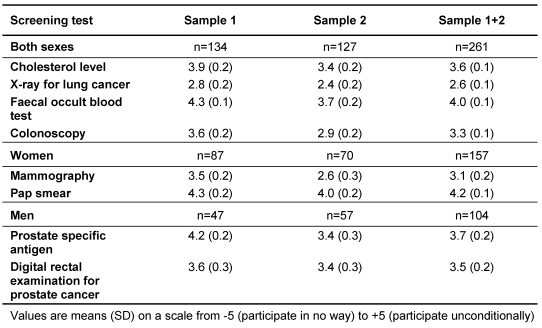
A total of 261 participants (157 women) were recruited. Figure 1 shows the flow of recruitment. Participants of both samples showed strong attitudes in favour towards colorectal cancer screening (colonoscopy and FOBT) and also towards the set of further screening tests surveyed, except lung cancer screening, which is not promoted in Germany. There was little variance in both samples. Attitudes tended to be higher in the first sample but the differences between the two samples were not statistically significant. Table 1 shows attitudes towards the surveyed screening tests for both samples.
Table 1. Attitudes of participants towards different screening tests.
Self reported previous participation in screening is prescribed in Table 2. Most participants (sample 1+2:72%) had taken part in colorectal cancer screening before. Differences between the two samples were not statistically significant. Therefore, we combined both parts for further analysis.
Table 2. Self reported previous participation in screening.
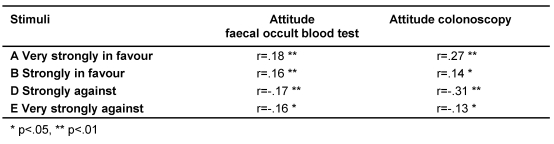
Table 3 shows the correlations between the independent variable "attitude towards colorectal cancer screening" and the dependent variable "sequence of article headlines". The pattern of the correlations is consistent. The correlations are all significant according to our hypothesis. The strength of attitude was analogue to attitude and therefore not reported.
Table 3. Correlations between attitudes and stimuli (n=261).
Discussion
This experiment shows significant correlations between attitudes towards colorectal cancer screening and information seeking. Consumers sought information on colorectal cancer screening according to the assumptions of the theory of cognitive dissonance. Study participants preferred information consonant to their personal attitudes. Therefore, the theory might explain some variance of dissonance reduction.
Both our recruitment strategies led to samples with insufficient variance in attitudes towards screening. Most participants had taken part in colorectal cancer screening before. According to the theory of cognitive dissonance, previous participation influences attitudes and information seeking in order to avoid dissonance. Therefore, our results are limited to this group extremely in favour of screening. On the other hand, maybe the distribution of attitudes towards screening in Germany is comparable to the USA. Schwartz et al. have reported a distinct enthusiasm towards screening among the US people. Almost 90% of adults believe that routine cancer screening is almost always a good idea [19]. However, in Germany participation rates in colorectal cancer screening are poor [20].
The major limitation of the experiment is due to the probably non-existent variance in attitudes towards screening in Germany. In addition, according to the experimental design some participants probably have chosen only the first stimulus according to their reading preference but might have followed different criteria, such as complexity of information or degree of popularity, when explicitly asked to order the article headlines. Thus, our experimental procedure probably leads to an underestimation of the existing effect. If it were possible to simulate information seeking more precisely, we would expect correlations to increase.
This has been the first attempt to apply the theory of cognitive dissonance to medical decision making. The study results suggest that selective information seeking might be one aspect beside others to explain phenomena of not noticing and avoiding EBPI. The field of medical decision-making needs to consult further theories to better understand information processing. Alaszewski et al. stated that misleadingly most approaches to communication of risk are based on the assumption that the target audience comprises individuals who rationally review evidence to identify and choose the course of action that will maximise benefit to health. Factors that influence consumers’ reactions on risk information have been explored. Beside the nature of specific arguments, the social context influences risk perception [21]. The theory of cognitive dissonance is only one theory out of many that can help to explain information processing. Unfortunately, knowledge about risk communication from social science has rarely been applied to the medical field [21].
In conclusion, communicating EBPI we have to consider that information processing is an individual constructivist process. There is no way to avoid cognitive dissonance. However, it could be a starting point for a constructive learning process.
Notes
Conflicts of interest
None declared.
References
- 1.Entwistle VA, Sheldon TA, Sowden A, Watt IS. Evidence-informed patient choice. Practical issues of involving patients in decisions about health care technologies. Int J Technol Assess Health Care. 1998;14(2):212–225. doi: 10.1017/s0266462300012204. [DOI] [PubMed] [Google Scholar]
- 2.Coulter A. Evidence based patient information. is important, so there needs to be a national strategy to ensure it. BMJ. 1998;317(7153):225–226. doi: 10.1136/bmj.317.7153.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sackett DL, Strauss SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine: how to practice and teach EBM. Edinburgh: Churchill Livingstone; 2000. [Google Scholar]
- 4.General Medical Council. [cited 2004 Sep 1];Protecting patients, guiding doctors. Seeking patients' consent: the ethical considerations [Internet] Available from: http://www.gmc-uk.org.
- 5.Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ. 2002;324(7341):827–830. doi: 10.1136/bmj.324.7341.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffrage U, Lindsey S, Hertwig R, Gigerenzer G. Medicine. Communicating statistical information. Science. 2000;290(5500):2261–2262. doi: 10.1126/science.290.5500.2261. [DOI] [PubMed] [Google Scholar]
- 7.Steckelberg A, Berger B, Köpke S, Heesen C, Mühlhauser I. Kriterien für evidenzbasierte Patienteninformationen. Z Arztl Fortbild Qualitatssich. 2005;99:343–351. [PubMed] [Google Scholar]
- 8.Coulter A, Entwistle VA, Gilbert D. Informing patients: an assessment of the quality of patient information materials. London: King's Fund; 1998. [Google Scholar]
- 9.Davey HM, Lim J, Butow PN, Barratt AL, Houssami N, Higginson R. Consumer information materials for diagnostic breast tests: women's views on information and their understanding of test results. Health Expect. 2003;6(4):298–311. doi: 10.1046/j.1369-7625.2003.00227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farrell MH, Murphy MA, Schneider CE. How underlying patient beliefs can affect physician-patient communication about prostate-specific antigen testing. Eff Clin Pract. 2002;5(3):120–129. [PubMed] [Google Scholar]
- 11.Robinson P, Purves I, Wilson R. Learning support for the consultation: information support and decision support should be placed in an educational framework. Med Educ. 2003;37(5):429–433. doi: 10.1046/j.1365-2923.2003.01498.x. [DOI] [PubMed] [Google Scholar]
- 12.Steckelberg A, Kasper J, Redegeld M, Mühlhauser I. Risk information - barrier to informed choice? A focus group study. Soz Praventivmed. 2004;49(6):375–380. doi: 10.1007/s00038-004-3153-4. [DOI] [PubMed] [Google Scholar]
- 13.Festinger L. A theory of cognitive dissonance. Stanford: Stanford University Press; 1957. [Google Scholar]
- 14.Hornung R. Krebs: Wissen, Einstellungen und präventives Verhalten der Bevölkerung. Psychosoziale Determinanten der Inanspruchnahme von Krebsfrüherkennungsuntersuchungen. Das Rauchen und seine psychische Bewältigung. Bern: Huber; 1986. [Google Scholar]
- 15.Frey D. Different levels of cognitive dissonance, information seeking, and information avoidance. J Pers Soc Psychol. 1982;43:1175–1183. [Google Scholar]
- 16.Frey D, Gaska A. Die Theorie der kognitiven Dissonanz. In: Frey D, Irle M, editors. Theorien der Sozialpsychologie I. Kognitive Theorien. 2. ed. Bern, Göttingen, Toronto, Seattle: Hans Huber; 1993. [Google Scholar]
- 17.Ajzen I, Timko C, White JB. Self-monitoring and the attitude-behavior relation. J Pers Soc Psychol. 1982;42:426–435. [Google Scholar]
- 18.Petty RE, Cacioppo IT, Goldman R. Personal involvement as a determinant of argument-based persuasion. J Pers Soc Psychol. 1981;41:847–855. [Google Scholar]
- 19.Schwartz LM, Woloshin S, Fowler FJ, Jr, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004;291(1):71–78. doi: 10.1001/jama.291.1.71. [DOI] [PubMed] [Google Scholar]
- 20.Scheffer S, Dauven S, Sieverding M. Soziodemografische Unterschiede in der Teilnahme an Krebsfrüherkennungsuntersuchungen (KFU) in Deutschland - Eine Übersicht. Gesundheitswesen. 2006;68(3):139–146. doi: 10.1055/s-2006-926641. [DOI] [PubMed] [Google Scholar]
- 21.Alaszewski A, Horlick-Jones T. How can doctors communicate information about risk more effectively? BMJ. 2003;327(7417):728–731. doi: 10.1136/bmj.327.7417.728. [DOI] [PMC free article] [PubMed] [Google Scholar]