Abstract
Objectives
To describe the integration of a first- and second-year introductory pharmacy practice experience (IPPE) involving direct patient contact in hospitals and clinics as a means of more efficiently using academic and preceptor resources.
Design
Two IPPE courses were integrated in fall 2004 to accomodate increasing enrollment in classes and limited clinical practice sites and preceptors, as well as to meet the increased need for students and clinicians to practice principles of self-education. P1 and P2 students interviewed patients and presented patient cases; preceptor expectations were structured by instructional objectives. Student and preceptor course evaluations were assessed from survey data.
Assessment
During the assessment period, all students passed the courses. Following integration of the IPPEs, both courses received positive evaluations from students and preceptors. Initial advanced pharmacy practice experience (APPE) grades for students completing the courses further suggests that the integrated IPPEs were beneficial to students.
Conclusion
The successful integration of first- and second- year IPPE courses resulted in more efficient use of academic and preceptor resources and created a model for other colleges of pharmacy to consider.
Keywords: introductory pharmacy practice experiences (IPPE), experiential education, experiential courses
INTRODUCTION
The Accreditation Council for Pharmacy Education (ACPE) standards and guidelines state that introductory pharmacy practice experiences (IPPE) must involve actual practice experiences in community and institutional settings.1 Descriptions of such IPPE courses have included various activities such as immunizations, patient telephone interviews, and health awareness education.2-7
Kolb describes experiential learning as a 4-element cycle consisting of involvement in a new experience, reflection on that experience, integration/conceptualization of what is learned from the experience and repeating the cycle.8 Consistent with Kolb's description of experience as a source of learning, some IPPE courses provide students with direct patient contact within an educational setting (eg, small group session) where they can discuss new knowledge and experience with a variety of other students and practitioners. Thus, students can question, refine, and reflect on newly acquired information and skills. In this environment, students experience metacognition, an awareness and understanding of their thinking and cognitive processes.
At the University of Tennessee College of Pharmacy, all P1 students take Introduction to Patient Care, a required 1-semester, 1-credit hour IPPE course. In this course, students interview patients in hospitals and clinics, review medical records, write a 2-page case summary, and present the patient's case in a small group setting. Another IPPE course, Applied Therapeutics, is a required experiential course in the spring semester of the P2 year and the fall semester of the P3 year. Similar to activities in the first-year course, students interview patients, review medical records, write a SOAP (subjective, objective, assessment, and plan) note, and present patients in small groups. In both courses, students operate under the supervision of licensed pharmacist preceptors. In recent years, with increasing class sizes, these 2 courses had begun to compete for clinical sites and preceptors, leading the course directors to integrate the 2 IPPEs. This paper describes that process.
DESIGN
Background on the Courses
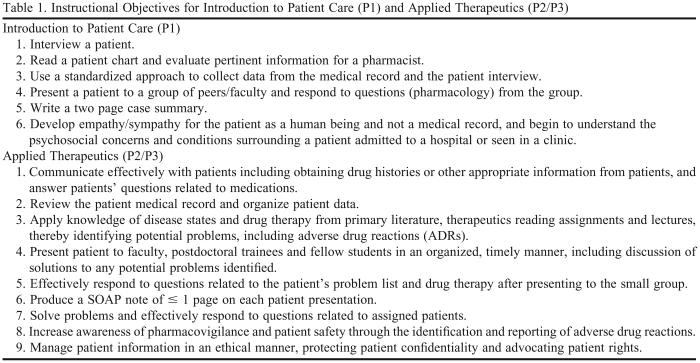
Instructional objectives for Introduction to Patient Care and Applied Therapeutics are provided in Table 1. Both IPPE courses were graded on a pass/fail basis. Since the early 1990s, all University of Tennessee College of Pharmacy students have taken Applied Therapeutics, a 2-semester, 2-credit hour experiential course in which students see and interview patients and present those patients in small group discussions. Applied Therapeutics was initially taught across the P3 year, however, since the spring of 2006, the course has been taught in the spring semester of the P2 year and the fall semester of the P3 year. This change was made secondary to a revised curriculum that had pharmacy students entering experiential education sites after the fall semester of the P3 year. Applied Therapeutics students attend a classroom and clinical site orientation to the course, and then students are assigned a patient every other week over a 10-week period. Applied Therapeutics students are required to attend every group session and to see 5 patients and present 5 patient cases across each semester. If students do not receive a passing grade for a given patient presentation, they are required to present another patient case until they have successfully presented 5 patient cases in a semester. When students present patient cases in Applied Therapeutics sessions, upper level (P3 and P4) students on clinical APPEs lead the discussions about disease states and therapeutics, along with postdoctoral residents and faculty preceptors. Thus, students benefit from the knowledge and skills of current students and recent graduates who now are practitioners in the patient care arena.
Table 1.
Instructional Objectives for Introduction to Patient Care (P1) and Applied Therapeutics (P2/P3)
Abbreviations: SOAP = subjective, objective, assessment and plan
Since 2002, Applied Therapeutics students also have been required to formally report an adverse drug reaction (ADR) identified in the institution or clinic. Students submit their identified ADR on an adverse drug event reporting form, which includes a causality assessment, using the Naranjo scale,9 as well as a severity rating and preventability assessment. The ADR form is approved and cosigned by the pharmacist preceptor prior to submission. Students cannot pass the course without submitting at least 1 ADR report.
Beginning in the late 1990s, University of Tennessee College of Pharmacy P1 students were required to take Introduction to Patient Care (initially named Introductory Clerkship), a 1-semester, 1-credit hour IPPE. Similar to Applied Therapeutics, Introduction to Patient Care is a pass/fail course. Initially this course was designed to familiarize students with taking medication histories and evaluating patient medical records. While some of the practice sites in the early years of this course were in hospitals and clinics, many were nursing homes and extended care facilities. Introduction to Patient Care students were assigned 2 patients to present for this early course. Introduction to Patient Care students would interview their patients and go through the patients' medical records at the practice site. However, patient presentations and small group discussions were actually conducted in a College of Pharmacy classroom with faculty preceptors who were typically not practitioners in the assigned practice sites and therefore not familiar with the patient cases being presented. Due to P1 students having taken a limited number of didactic courses at this point in the curriculum, questions asked primarily focused on knowledge of pharmacology, such as mechanism of action and major adverse effects. The course was originally taught in the fall semester of the P2 year; however, with the revised curriculum, it was moved to the spring semester of the P1 year in 2005.
Integration of the Courses
As class sizes increased from 100 students in the late 1990s to 125 early in this decade, and then to 175 and 200 students, it became evident that these 2 IPPE courses were competing for some of the same clinical sites and preceptors. Therefore, the course directors discussed how the courses could be integrated while maintaining the quality of the courses and the integrity of the small group setting. A proposal was developed that combined the recitation sessions for the courses, and approved by the University of Tennessee College of Pharmacy Curriculum Committee. The initial plan was simply to use the same sites and preceptors for the courses but require the students in each course to see and interview different patients.
While this approach solved the problem of keeping the number of clinical sites and preceptors at a more practical level, 2 further issues became apparent. The first issue was having sufficient numbers of interesting teaching cases for 4 or 5 students per group each week at each clinical site (some large hospitals take 5 to 6 groups of students/semester). The second issue was how to conduct 4 to 5 thorough patient presentations and discussions in a 2-hour session (an important consideration for full-time and part-time faculty preceptors). Both of these concerns were allayed by a faculty preceptor, Dr. Joyce Broyles, who used what is referred to as the Broyles Model, in which both P1 and P2 students interview and give a presentation on the same patient. The P1 student presents the patient, the patient's hospital course, and fields questions regarding pharmacology, while the P2 student presents a SOAP note and fields more complex questions regarding therapeutics. Although the Broyles Model was initially suggested as an option, all faculty members now use this model at each clinical site.
The course directors saw a distinct advantage to integrating the Applied Therapeutics and Introduction to Patient Care courses. This advantage was especially true for the Introduction to Patient Care course because of the enhanced clinical experience for the P1 students. With the integration of the courses, Introduction to Patient Care students interviewed and reviewed the medical records of 2 patients in hospitals and clinics and presented patient cases in small group discussions with faculty preceptors and residents (as well as pharmacy students on APPEs) who practiced in the assigned site. When not presenting, students benefited from hearing classmates and Applied Therapeutics students present. Active participation in the discussion was encouraged.
After classroom and site orientations, 100 of the 200 students in the P1 class were sent to 25 clinical sites in the greater Memphis area for the first 5 weeks of the course (ie, 4 students at each of 25 preceptor groups located in hospitals and clinics), and the other 100 students were assigned to those same sites for the second 5 weeks of the semester. The first week of each half of the semester, the P1 students observed while the P2 students presented patients. The following week, the P1 students began presenting patients with the P2 students. While it would have been beneficial to have P1 students attend all 10 weeks with the P2 students in Applied Therapeutics, the sheer numbers of students made that a logistical problem. The course directors knew that smaller groups facilitated advanced discussion and larger groups created space problems in conference rooms. In addition, too many pharmacy students congregating at nurses' stations to read charts would have hindered the flow of patient care and created negative perceptions of pharmacy students in the health care setting.
With respect to Applied Therapeutics, 5 students were assigned to each of the 25 preceptor groups for the entire semester. Despite the class size of 200, it was possible to maintain 5 Applied Therapeutics students per preceptor group since 75 students moved to the Knoxville campus annually after completion of the P1 year on the Memphis campus (began in 2007). Applied Therapeutics students on the Knoxville campus were assigned to preceptor groups (ie, 15 groups of 5 students each) in hospitals and clinics in the greater Knoxville area. Since there were no P1 students on the Knoxville campus, the Applied Therapeutics students at the Knoxville campus completed both semesters of Applied Therapeutics as a nonintegrated course (ie, group sessions were not combined with Introduction to Patient Care students).
At the end of each semester for 2004-2008, students assessed Introduction to Patient Care and Applied Therapeutics via an online course evaluation system. The specific evaluations for each course allowed students to state whether the courses met the instructional objectives and also to give subjective comments on the strengths and weaknesses of the courses. At the end of the 2008 spring semester, preceptors for the courses were surveyed. The online survey assessed preceptors' opinions on the effectiveness of both IPPE courses in terms of student attainment of instructional objectives. In addition, preceptors were asked whether the Introduction to Patient Care course was effective overall in helping P1 students as they enter Applied Therapeutics as P2 students. Furthermore, preceptors were asked, from their perspective as APPE preceptors, whether Applied Therapeutics helped to prepare students to perform better in their first APPE. Finally, preceptors were asked to assess Applied Therapeutics student competencies following the integration of these courses. Specifically, they were asked to compare the competencies of Applied Therapeutics students who had Introduction to Patient Care as P1 students combined with Applied Therapeutics (ie, post-integration) to those students who had Introduction to Patient Care alone (ie, pre-integration).
For those students who completed both Introduction to Patient Care and Applied Therapeutics after integration of the courses, their performance (ie, letter grade) on their first patient care APPE was assessed.
ASSESSMENT
During the assessment period, all students passed the 2 IPPE pass/fail courses. Each student interviewed and satisfactorily presented 2 patients (Introduction to Patient Care students) or 5 patients (Applied Therapeutics students). In addition, Applied Therapeutics students turned in an acceptable ADR report.
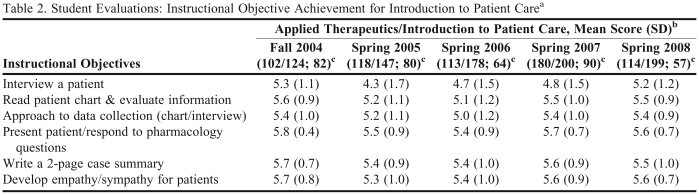
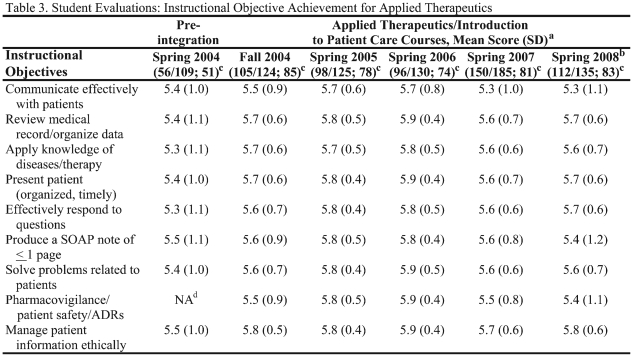
The data for 2004-2008 were extracted from the student course evaluation system and analyzed. The results of the instructional objective attainment are reported on a scale of 1 to 6, with 1 being the lowest and 6 being the highest score. The scores for both courses are reported in Tables 2 and 3. General subjective comments with respect to strengths of the courses are voluminous and outside the scope of this paper; however, specific subjective comments by Introduction to Patient Care students with respect to integration of the courses were favorable.
Table 2.
Student Evaluations: Instructional Objective Achievement for Introduction to Patient Carea
Abbreviations: AT = Applied Therapeutics; IPC = Introduction to Patient Care
Pre-integration course evaluation scores were not included for IPC since a different format and objectives were used.
bData are presented as mean score (SD). Reported score (on a scale of 1 to 6) derived from percentage of responses that an individual instructional objective was attained. Scores correspond to the following percentages: 1 = < 50%; 2 = 50-59%; 3 = 60-69%; 4 = 70-79%; 5 = 80-89%; 6 = > 90%
cNumbers are (responses received/responses expected; response rate).
Table 3.
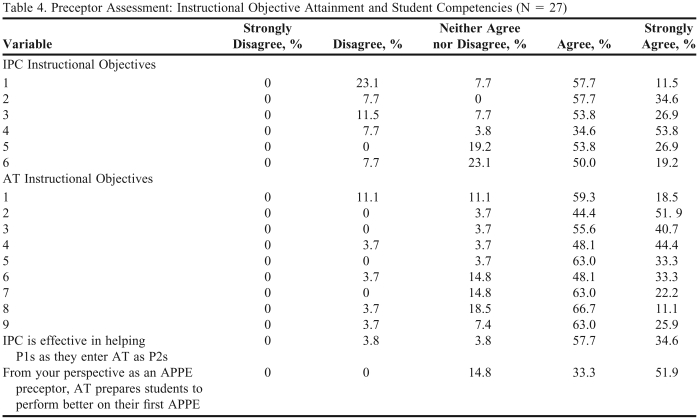
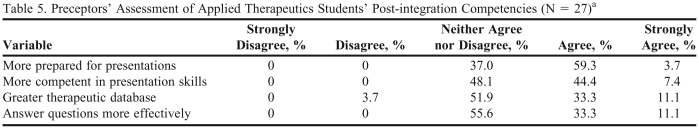
The response rate for the preceptor survey conducted at the end of spring 2008 was 66% (27 of 41 preceptors). Table 4 reports preceptor assessment of the effectiveness of both IPPE courses in terms of student attainment of instructional objectives. In addition, 92% of respondents agreed that the Introduction to Patient Care course was effective in helping P1 students as they enter Applied Therapeutics as P2 students and over 85% of respondents agreed that Applied Therapeutics helped to prepare students to perform better in their first APPE. Table 5 reports preceptor assessment of Applied Therapeutics student competencies following the integration of these courses. Preceptors generally agreed or were unable to give an opinion with respect to these questions.
Table 4.
Preceptor Assessment: Instructional Objective Attainment and Student Competencies (N = 27)
Instructional objectives for each course are numbered and correspond with those outlined in Table 1
Evaluation conducted at the end of the spring semester 2008
AT = Applied Therapeutics; IPC = Introduction to Patient Care; APPE = advanced pharmacy practice experience
Table 5.
Preceptors' Assessment of Applied Therapeutics Students' Post-integration Competencies (N = 27)a
Preceptors were asked to assess Applied Therapeutics (AT) students who had Introduction to Patient Care (IPC) in their P1 year combined with AT compared to earlier AT students who did not have IPC as P1s combined with AT. The evaluation was conducted at the end of spring semester 2008.
In the 2007 spring semester, 97% of P3 students who were enrolled in the integrated IPPE courses in their P1 and P2 years received letter grades of either A or B on their first APPE. Likewise, in the spring of 2008, 97.4% of P3 students received either A or B on their first patient care APPE.
DISCUSSION
Experiential learning is essential in educating pharmacy students to care for patients. As defined earlier, Kolb describes experiential learning as a 4 element cycle: experience, reflection, integration/conceptualization, and repetition/refining.8 The integrated IPPE courses described in this paper provided students not only direct patient contact, but also an educational setting (ie, small group discussion) where they could follow this experiential model of learning. Baker et al described Kolb's Learning Style Inventory as it applied in medical education.10 Pharmacy students learn and process skills as they become more aware of the necessity of such skills in reaching their full potential within the profession. After students saw patients, read the medical record, and wrote a brief summary, they presented patient cases in small groups. In these small groups, students (P1, P2, P3, P4), postdoctoral residents, and faculty preceptors discussed, probed, addressed, and otherwise offered input from a range of perspectives, thus experiential learning became truly synergistic (in that the whole became greater that the sum of its parts).
Since the introduction of Applied Therapeutics in the College of Pharmacy curriculum in the early 1990s, student evaluations for this course have been consistently high. Students routinely express that they learn more in a semester of Applied Therapeutics than in multiple semesters of didactic classes. After the integration of these courses, student evaluations suggested that the experience attained through Applied Therapeutics had not been hindered by the addition of Introduction to Patient Care students to the group sessions. Student evaluations further suggested that the Introduction to Patient Care students recognized the value of early exposure to the clinical practice site, particularly through the mentorship of upper class students. Finally, the level of student performance on their first APPEs further suggested that the integrated IPPE courses were beneficial to students.
The courses described in this paper present obvious logistical challenges, including the need for preceptors at 25 sites in the greater Memphis area. In addition, the course directors encountered further challenges to integrating these courses because of changes occurring in the College of Pharmacy during the same period of time (implementation of a revised curriculum, increasing class size, and opening of another campus on the other side of the state). Despite these problems, the courses have continued to offer early experiential education because of the strong commitment and efforts of the faculty preceptors. Furthermore, the response from preceptors for the 2 courses has been quite favorable, and these same individuals are preceptors for advanced pharmacy practice experiences (APPEs).
A potential limitation of both the student and preceptor evaluation data is the lack of a 100% response rate. Thus, the overall scores and responses could have been different had all the students and preceptors participated in the evaluation process. On the other hand, more than 50% of students responded in all of the years reported (greater than 75% of students responded in most years) and 66% of faculty preceptors responded; therefore, the response rate was relatively strong.
The integration of the 2 courses has succeeded in creating a strong foundation early in the PharmD curriculum. The foundation is then strengthened and enhanced with each successive course experience. The group discussions are structured to allow the P3 and P4 students, who follow the assigned patients daily in the clinical practice site, to lead the discussion. Questions posed by these upper class students are guided by the knowledge and experience level that each class of students is expected to possess (ie, pharmacology in the P1 class and therapeutics and pharmacotherapy in the P2 class). This approach not only supports the learning of the P1 and P2 students, but also allows the P3 and P4 students to discuss topics they should have mastered, thereby enhancing their understanding of topics through teaching. Residents and faculty preceptors are available to assist with the discussion and elaborate on points where students require help. Clarification by faculty preceptors further facilitates the education of the students as well as the residents. This multi-level approach works for all through an unimposing environment where most students feel comfortable with active participation. This process allows the P1 a gradual introduction to the hospital environment, to interacting with patients, and to medical terminology and language. The P2 student, having already had Introduction to Patient Care, provides guidance to the P1 student and learns the fundamentals of communication with health care professionals through preparing SOAP notes. Furthermore, students are asked to provide a rational thought process for their decisions. Students benefit greatly from having introductory on-site experiences where they are required to assess an individual patient, devise and present a pharmacotherapy plan, and join in discussions with individuals across all levels of pharmacy training. A school of pharmacy incorporating courses of this nature into the curriculum would provide students with an invaluable learning experience.
SUMMARY
IPPE courses conducted in clinical practice sites provide students an educational experience that is gradually built upon as they advance through the PharmD curriculum. This learning environment is best optimized in a small group setting. Many challenges face today's pharmacy educators, namely increasing numbers of pharmacy schools and students, threatening the ability to provide a quality curriculum of pharmacy practice experiences that still maintain the integrity of small group courses. This paper describes the successful integration of 2 IPPE courses whereby the quality of the experiences were certainly maintained and potentially enhanced by the integration. The described model provides a framework for the incorporation of IPPE courses that take place in clinical practice sites into the PharmD curriculum.
ACKNOWLEDGEMENTS
We would like to acknowledge all of the excellent University of Tennessee College of Pharmacy faculty preceptors who committed their time, energy, and expertise to these courses. We also thank Dr Raoul Arreola for his assistance with the faculty preceptor assessment.
REFERENCES
- 1. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Am J Pharm Educ. 2007;71 (1) Article 03. Accreditation Council for Pharmacy Education, 2006. http://www.acpe-accredit.org/pdf/acpe_revised_pharmd_standards_adopted_jan152006.pdf. Accessed February 4, 2009.
- 2.Hak EB, Foster SL, McColl MP, Bradberry JP. Evaluation of student performance in an immunization continuing education certificate program incorporated in a pharmacy curriculum. Am J Pharm Educ. 2000;64:184–7. [Google Scholar]
- 3.Turner CJ. An introductory pharmacy practice experience emphasizing student-administered vaccinations. Am J Pharm Educ. 2007;71:3. doi: 10.5688/aj710103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turner CJ, Jarvis C, Altiere R, Clark L. A patient-focused and outcomes-based experiential course for first-year pharmacy students. Am J Pharm Educ. 2000;64:312–9. [Google Scholar]
- 5.Jarvis C, James VL, Giles J, Turner CJ. Nutrition and nutrition: a service-learning nutrition pharmacy course. Am J Pharm Educ. 2004;68 Article 43. [Google Scholar]
- 6.Turner CJ, Altiere R, Clark L, Dwinnell B, Bartin AJ. An interdisciplinary introductory pharmacy practice experience course. Am J Pharm Educ. 2004;68 Article 10. [Google Scholar]
- 7.Turner CJ, Altiere R, Clark L, Maffeo C, Valdez C. Competency-based introductory pharmacy practice experiential courses. Am J Pharm Educ. 2005;69 Article 21. [Google Scholar]
- 8.Kolb DA. Experiential Learning Experience as the Source of Learning and Development. Englewood Clifts, NJ: Prentice-Hall; 1984. [Google Scholar]
- 9.Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharm Ther. 1981;30:239–45. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 10.Baker JD, Wallace CT, Bryans WO, Klapthor LB. Analysis of learning style. South Med J. 1985;78:1494–7. doi: 10.1097/00007611-198512000-00021. [DOI] [PubMed] [Google Scholar]