Abstract
Objectives
To assess preceptors' opinions of the impact of quality assurance projects.
Methods
Students were given the opportunity to directly apply material learned in class in a “real world” environment by completing a quality assurance project in a community or health-system pharmacy. All preceptors (n = 38) were contacted via telephone and given the opportunity to respond to open-ended questions concerning their experience with student-team quality assurance projects.
Results
Preceptors indicated the quality assurance projects benefited their practice sites by providing additional resources (53%, n = 19), decreased medication errors (22%, n = 8), and increased awareness of the importance of quality assurance (22%, n = 8). Ninety-four percent of respondents (n = 34) perceived the projects had a positive impact on patient care and 92% (n = 33) perceived a positive impact on themselves.
Conclusions
Preceptors felt that quality assurance projects performed by pharmacy-student teams were beneficial to patient care, the practice site, and themselves. The quality assurance projects have broad applications and can be added to a medication safety class or to the introductory pharmacy practice experience (IPPE) sequence.
Keywords: preceptor, quality assurance, curriculum
INTRODUCTION
The Institute of Medicine (IOM) has specified its vision of how quality issues in health care should be addressed: “All health professionals should be educated to deliver patient-centered care as a member of an interdisciplinary team, emphasizing evidence-based practice, quality improvement approaches, and informatics.”1 This and subsequent reports spurred other organizations and accrediting bodies to make similar recommendations.2 The American Association of Colleges of Pharmacy (AACP) Center for the Advancement of Pharmaceutical Education (CAPE) 2004 Educational Outcomes3 call for colleges and schools of pharmacy to prepare students to: (1) apply quality assurance (QA) strategies and research processes to minimize drug problems and (2) use QA to identify and resolve medication use problems.
Because of these recommendations, colleges and schools of pharmacy in the United States have begun to implement educational strategies to help future pharmacists increase medication safety.4,5 One such class for doctor of pharmacy (PharmD) students at Midwestern University Chicago College of Pharmacy, entitled Quality Assurance and Effective Pharmacy Practice (QA & EPP), has been described previously in the Journal.4
The QA & EPP instructional sequence was designed to give students the opportunity to directly apply material learned in class in a “real world” environment. To accomplish this, students self-selected project teams and were assigned to a preceptor in a community or health-system pharmacy via lottery. Except in rare circumstances, each preceptor had only 1 project team per year. Preceptors were identified and recruited by the course director. In many cases, the QA & EPP preceptors were not MWU College of Pharmacy preceptors.
Teams met with their preceptors in the second week of the quarter to develop site-specific QA projects. During the remainder of the quarter, student teams met with their preceptor at the pharmacy practice site weekly (3 hours per week) to collect, analyze, and evaluate data to measure the plan's impact. Results were presented at a poster forum during the last week of the quarter. Between 2002 and 2004, approximately 500 students received training in QA & EPP. Each project team was comprised of 4 to 7 students, with 100 student-team projects completed over the 3-year period. Thirty QA & EPP preceptors participated during the first 2 years. This number was increased to 38 in the third year due to an increase in class size.
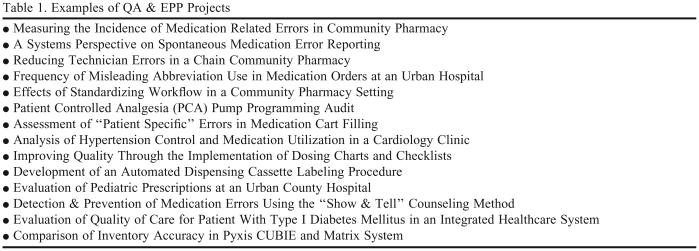
QA & EPP student teams and preceptors were given latitude to select a QA project that would directly benefit each pharmacy practice site. There was significant variation in project topics and approaches, yet consistent themes emerged. For example, one of the most common QA team projects involved the implementation of the Pharmacy Quality Commitment Sentinel System or its component parts. The Sentinel System is a systematic continuous quality improvement program that uses standardization of workflow, risk management techniques, and internal problem documentation and analysis as mechanisms to assist community pharmacists in identifying, evaluating, and preventing medication errors. Other common QA team project interventions included the implementation and evaluation of: process standardization, checklists, or other decision aids, pharmacy stock reorganization, open-ended patient counseling techniques, protocol development, use of risk management techniques, and standard documentation. Examples of student-team projects are included in Table 1.
Table 1.
Examples of QA & EPP Projects
Because projects were implemented in clinical settings, success was dependent upon the participation of both the students and site preceptors. Formal QA education is somewhat new to pharmacy curricula and few pharmacist preceptors received formal training in these techniques while in pharmacy school. Anecdotal evidence suggests that, in addition to teaching their students, preceptors also learn from them. Therefore, as the course director, the author was hopeful that QA & EPP students would help preceptors update their QA skills and that the projects would facilitate practice improvement. The overall objective of this study was to assess what, if any, benefits the preceptors gained from the QA projects. Medical and pharmacy preceptor perceptions about the benefits and costs of precepting to the individual and to the clinical site have been described in the literature previously.6-12 However, to the author's knowledge, this is the first article to discuss preceptor perceptions of the value of QA.
METHODS
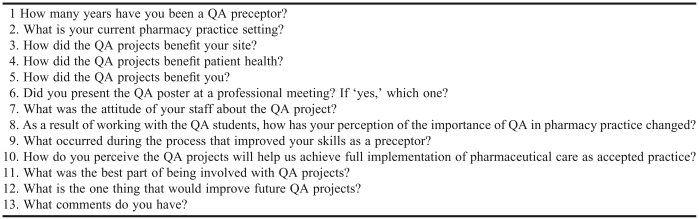
This study involved a telephone survey of QA preceptors. In an effort to allow preceptors leeway when responding, 13 open-ended questions were developed based on informal preceptor comments and feedback. A pilot survey was designed and tested on 8% of preceptors and the final survey was revised based on these data. It was hoped that when responding to survey questions preceptors would provide candid opinions concerning projects, students, and the class overall. Questions focused on the potential benefits of the projects to the practice site, patient health, and the preceptor themselves.
In the fall of 2004, after 3 years of class projects were completed, project preceptors received written notification that a telephone survey was planned and then a telephone call to schedule a convenient time for them to participate. The course director contacted the preceptors at the scheduled time and administered the survey. Preceptors were given the opportunity to provide only 1 response to each question (Appendix 1); therefore, response percents for all questions equaled 100%.
During each telephone survey, preceptor's answers and comments were typed verbatim into a word processing program. These responses were immediately read back to the preceptor to ensure accuracy then de-identified (ie, the respondents name or identifying information was removed from the response).13 Specific qualitative data classification techniques were employed. Descriptive coding was used for evaluating preceptor demographic characteristics. This was followed by the grouping of responses according to subject (ie, topic coding). Topic coding was accomplished in 2 phases: general categorization followed by refinement to incorporate more specific subcategories. Data quality was ensured via recoding of responses and checking for consistency with the original coding of 10% of data at a later date. SPSS statistical analysis system version 11.5 for Windows (SPSS Inc, Chicago, IL) was used to calculate demographic statistics and for calculation of frequencies of categories or themes. The Interval Review Board at the Midwestern University Chicago College of Pharmacy granted approval for this research project.
RESULTS
Thirty-eight preceptors were contacted and given the opportunity to participate in this study. Thirty-six preceptors agreed to participate in the survey, 1 preceptor did not reply, and 1 moved without leaving forwarding information, yiedling a total response rate of 95%. The average responder had served as a QA & EPP preceptor for 1.9 years (SD = 0.91, median = 2). That is, the majority of the QA & EPP preceptors mentored student QA teams in subsequent years. Most QA & EPP preceptors were practicing in community settings (61%, n = 22) or inpatient hospital settings (31%, n = 11), while the remaining 8% (n = 3) were practicing in other ambulatory care settings, such as within a pharmacist-run anticoagulation clinic.
To the question, “How did the QA projects benefit your site?” preceptors responded by providing additional personnel resources (53%, n = 19), decreased medication errors (22%, n = 8), or increased awareness of QA issues (22%, n = 8). The remaining 3% (n = 1) thought the projects improved relationships with other health care providers. Typical comments included “[It] allowed us to hone in on a project we wanted to do but did not have manpower for.” and “After [they] implemented their project, the number of errors was significantly lower for both internal and external errors.”
Because the QA projects were individualized on a site-by-site basis, answers to “How did the QA projects benefit patient health?” varied widely and did not lend themselves to aggregation. Responses ranged from “the projects provided general benefits” to more specific examples such as “[the projects] lowered errors and the problems from errors.” While 94% (n = 34) of preceptor believed the projects benefitted patient health, 6% (n = 2) perceived no impact.
When asked “How did the QA projects benefit you?” 58% (n = 21) reported that they learned during the process; 28% (n = 10) reported that working on the QA projects with the students was “fun” or “rewarding”; and 6% (n = 2) reported a non-specific personal benefit. A representative comment was: “It made me a better pharmacist.” Preceptors who indicated no impact (8%, n = 3) quantified their precepting or QA experience as “extensive” and commented “Every time I work with students, I learn.”
Thirty-nine percent of the preceptors (n = 14) indicated they and their student teams had presented their QA poster at least once in addition to the required presentation at the QA poster forum and an additional 19% (n = 7) were planning to present their poster in another setting. Of those who had made additional presentations (n = 14), 9 presentations were at national meetings, 4 were at regional meetings, and 5 were at other administrative meetings on a local level. Two manuscripts authored by students and preceptors stemming from the QA projects were in progress and some preceptors and students utilized the same poster for encore presentations at several venues, while others presented a different team poster each year.
Seventy-two percent of preceptors (n = 26) reported that his/her staff responded positively to the QA projects, 17% (n = 6) cited a mixed response, 8% (n = 3) perceived neutral staff attitudes, and 3% (n = 1) perceived negative staff attitudes. Several preceptors who indicated a mixed staff reaction underscored this point by stating, “After getting on the same page, the staff loves it!” Another preceptor commented that “Staff attitudes benefit both from having attention paid to their issues and from the perception that their work and opinions are important enough for a research project.”
When asked, “As a result of working with the QA students, how has your perception of the importance of QA in pharmacy practice changed?” 69% (n = 25) indicated that working with the students increased his/her perception of the importance, impact, or urgency of QA in pharmacy practice. On preceptor commented: “[It] changed dramatically. I knew QA was important but did not know how much small projects could help.”
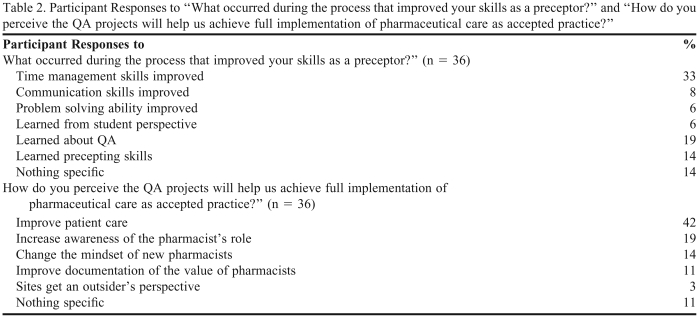
When answering “What occurred during the process that improved your skills as a preceptor?” 47% (n = 17) noted that working with a QA & EPP group helped improve his/her time management, communication, or problem-solving skills. More detailed results appear in Table 2. Some preceptors learned about QA, gained insight from the students' perspective, or were first-time preceptors and indicated a general gain in precepting skills.
Table 2.
Participant Responses to “What occurred during the process that improved your skills as a preceptor?” and “How do you perceive the QA projects will help us achieve full implementation of pharmaceutical care as accepted practice?”
Responses to “How do you perceive the QA projects will help us achieve full implementation of pharmaceutical care as accepted practice?” were varied and ranged from “the QA projects will lead to improved patient care” to “projects will help to change the mind-set of new pharmacists.” Additional results appear in Table 2. A representative comment was: “These QA projects are a step in the right direction but something more universal needs to be done for this connection to be made. For example, this class needs to be expanded to all schools of pharmacy.” Another telling comment was: “The QA projects help show importance of pharmacists in error prevention but it has to be presented to the public. We need to advertise to our patients all the good we are doing.”
Sixty-nine percent (n = 25) of preceptors indicated that interacting with the students or seeing project results was the best part of being involved with the QA projects. Thirty-six percent (n = 13) of preceptors specifically stated they enjoyed getting to know the students and 19% (n = 7) cited student enthusiasm as the biggest perk, while the remaining 14% (n = 5) said the student's perspective or transformation was the best part of the process. Examples of preceptor comments include: “The students create a sense of urgency, focus, and passion to get change made” and “Five people can get a lot of work done!”
When asked what would improve future QA projects, preceptors provided various responses: 8 preceptors recommended a change in the manner in which project topics were selected (ie, 7 requested less flexibility while 1 preceptor requested more); 6 preceptors suggested changing the amount of time students spent at the practice site (5 recommended students have more practice-site time while 1recommended less site time).
DISCUSSION
Most of the QA & EPP preceptors had a positive opinion of the QA & EPP projects and their impact prior to survey administration. As the course director, the author worked closely with the QA & EPP preceptors to develop a relationship of trust and openness; if the preceptor had a negative impression he/she seemed willing to candidly voice that opinion.
During the first class administration in fall of 2002, there was mutual concern on the part of the preceptors and the author because student teams were relatively large (ie, 4 to 7 students per team). While many preceptors would prefer smaller teams, they thought the QA projects provided benefits to the practice site. Many preceptors mentioned that the teams provided needed manpower resources. This is important to the future of teaching such skills because, in order to recruit and maintain preceptors and sites, a perceived benefit to the site is essential.6
Preceptors reported an overwhelmingly positive personal impact from the QA projects. Nevertheless, the course coordinator initially had a rather difficult time convincing pharmacists to participate as QA team project preceptors. This task was especially challenging because the coordinator was new to Chicago and knew few pharmacists in the area, and because the class size was large and many students needed to be placed. Pharmacists were recruited to precept through an assortment of mechanisms: (1) advertisements in state, local, and alumni pharmacy newsletters; (2) professional networking at meetings; and (3) referrals from other faculty members. One of the biggest hurdles to preceptor recruitment was the concerns of pharmacists about their personal lack of QA training and knowledge. This concern was addressed by the development of a preceptor manual and training program. Also, preceptors came to understand that they did not have to have all the answers for their students and that this actually aided the discovery process for all involved. While the recruitment process was laborious and took 7 months, it was beneficial because at the conclusion of the team projects, preceptors had positive attitudes about the project and the personal benefits of precepting QA team projects. This was not entirely unexpected, as several articles have described the positive personal benefits of precepting in medicine and pharmacy.6-12 This attitude was evident in the preceptor recruiting trends over the 3-year period; it became easier to recruit and maintain preceptors as word of mouth concerning the QA projects and their benefits spread among the local pharmacy practice community. By the third year, many potential new preceptors called the course director to volunteer without solicitation.
One of the potential benefits of the QA projects is the possibility for increased pharmacist, site, and program exposure on a local and national level. In addition to the required poster presentation at the end of the class, many preceptors and students opted to present their findings elsewhere. While the percentage of preceptors who utilized QA posters for additional presentations increased each year, some preceptors indicated they were not aware of this opportunity.
Although overall staff attitudes toward the QA & EPP projects were positive, there were mixed reactions at some sites. This may be partly attributed to preceptors volunteering their sites and staff participation without involving or informing staff members about the project until the students arrived at the pharmacy. To address this problem, the author incorporated suggestions for staff communication into QA & EPP preceptor training sessions since staff participation and support of the projects is essential to QA progress.
For the most part, preceptors reported that working with the students changed their perception of the importance of QA in pharmacy practice. One common misconception held by students and preceptors was that only changes of a large scope are beneficial. Therefore, the author was pleased that the message that small changes could produce a positive impact was internalized by its intended audience. This inspires hope that such an attitudinal alteration may lead to the completion of additional QA projects. Ultimately, it is not the role of the student to undertake all QA work; it is the role of the pharmacist or the pharmacy profession as a whole. However, because preceptors learned that small changes are beneficial in improving practice, they may be more likely to engage in QA projects even when students are not available to assist.
Most preceptors agreed that the QA & EPP projects will help the profession of pharmacy achieve full implementation of pharmaceutical care by improving patient care, increasing awareness of the pharmacist's role, or by changing the mindset of new pharmacists. However, almost all agreed that additional action needs to be taken to this end. The author agrees that the public is largely unaware of the positive contributions pharmacists make to patient care. Patients and other members of the health care team need to be educated about quality pharmaceutical care and the value the pharmacist adds to the medication use system. Perhaps then patients will appreciate, demand, and pay for higher quality pharmaceutical care.
Of those that offered suggestions for future class improvements, the most frequently mentioned was a change in the manner of project topic selection. Each QA project was site specific and teams had corresponding latitude in topic selection. Consequently, some project teams reported having a difficult time focusing on or choosing a topic. Some preceptors recommended narrowing the possible topics by providing examples of previous projects or assigning topics. The author hesitated to do this for fear of decreasing benefits to the sites or stifling creativity. However, there may be a compromise. That is, it may be useful to have a list of possible general topics that students can use if they are having difficulty in topic identification and/or selection. None of the preceptors commented on the personal or work time it took to mentor the projects. It is the author's interpretation that this was because the preceptors felt that, in general, the benefit they got from the projects outweighed the costs.
Many colleges of pharmacy in the United States are contemplating the addition of medication safety curricular content.5 The QA projects fit nicely into a medication error reduction class as described in this manuscript. Alternatively, because the projects require no specific therapeutic knowledge, they could be placed in an introductory pharmacy practice experience (IPPE) sequence.
Limitations
This study has several limitations. First, there is the potential for acquiescent response bias. That is, it is possible that a few preceptors gave the answers they thought would please the study investigator. This is especially a concern because the questions were phrased in a positive manner and asked by the preceptor coordinator (the author). In the event that this evaluation is repeated, an alternative method may be used such as having another researcher or trained interviewer conduct the interviews. A structured self-administered questionnaire will also be considered. Second, this survey assessed only the preceptor's subjective opinion of the impact of the QA & EPP projects. An in-depth quantitative assessment was beyond the scope of this study. Third, this study was a one-time case study and as such assessed only the short-term impact of the projects. It would be interesting to follow the graduates as a cohort to assess the impact of the QA projects on their long-term attitudes and actions.
CONCLUSIONS
QA & EPP preceptors felt that the projects performed were beneficial to patient care, the practice site, and themselves. In addition, preceptors had the opportunity to utilize student work hours to start or expand their QA plans. The quality assurance projects have broad applications and can be added to a medication safety class or to an IPPE sequence.
ACKNOWLEDGEMENTS
The author recognizes the contributions of Dr. Terrence R. Jackson on the conception and implementation of this project. In addition, the author acknowledges the support of Dr. Janis MacKichan, Dr. Tom Reutzel, Ken Baker, Dr. Pat Lurvey, Dr. Amy Grizzle, Ms. Sunita Arora, Ms. Bonnie Pearsall, Ms. Sue Yeater, and the 38 pharmacist preceptors.
Appendix 1. QA Preceptor Survey Questions
REFERENCES
- 1.Committee on Health Professions Education. Health Professions Education: A Bridge to Quality. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Institute of Medicine (IOM) Washington, DC: The National Academies Press; 2006. Preventing Medication Errors. [Google Scholar]
- 3. American Association of Colleges of Pharmacy (AACP) Center for the Advancement of Pharmaceutical Education (CAPE). Educational outcomes. Alexandria, VA; May 2004. http://www.aacp.org/resources/education/Pages/CAPEEducationalOutcomes.aspx.
- 4.Jackson TL. Applications of quality assurance principles: Teaching mediation error reduction skills in a “real world” environment. Am J Pharm Educ. 2003;68(1) Article 17. [Google Scholar]
- 5.Johnson MS, Latif DA, Gordon B. Medication error instruction in schools of pharmacy curricula: A descriptive study. Am J Pharm Educ. 2002;66:364–71. [Google Scholar]
- 6.Skrabel MZ, Kahaleh AA, Nemire RE, Boxer H, Broshes Z, Harris M, Cardello E. Preceptors' Perspectives on Benefits of Precepting Student Pharmacists to Students, Preceptors, and the Profession. J Am Pharm Assoc. 2006;46(5):605–12. doi: 10.1331/1544-3191.46.5.605.skrabal. [DOI] [PubMed] [Google Scholar]
- 7.Shannon S, Walker-Jeffreys M, Newbury JW, Cayetano T, Brown K, Petkov J. Rural clinician opinion on being a preceptor. Rural Rem Health. 2006;6 Article 490. [PubMed] [Google Scholar]
- 8.Zachary TE, Smith-Barbaro P. Value of a family medicine preceptorship/clerkship to students, preceptors, and communities: observations from a 25-year-old program. Fam Med. 2001;33(7):500–1. [PubMed] [Google Scholar]
- 9.Ferenchick GS, Chamberlain J, Alguire P. Community-based teaching: Defining the added value for students and preceptors. Am J Med. 2002;112(6):512–7. doi: 10.1016/s0002-9343(02)01093-8. [DOI] [PubMed] [Google Scholar]
- 10.Baldor RA, Brooks WB, Warfield ME, O'Shea K. A survey of primary care physicians' perceptions and needs regarding the precepting of medical students in their offices. Med Educ. 2001;35(8):789–95. doi: 10.1046/j.1365-2923.2001.00980.x. [DOI] [PubMed] [Google Scholar]
- 11.Grayson MS, Klein M, Lugo J, Visintainer P. Benefits and costs to community-based physicians teaching primary care to medical students. J Gen Internal Med. 1998;13(7):485–8. doi: 10.1046/j.1525-1497.1998.00139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crouse BJ, Norris TE, Wolff LT. Rural physicians as educators: Why take on another job? Am Fam Phys. 1996;54(5):1457–60. [PubMed] [Google Scholar]
- 13.Richards L. Handling Qualitative Data: A Practical Guide. London: Sage Publications, Ltd; 2005. pp. 85–103. [Google Scholar]