Abstract
Neural, endocrine and immune stress mediators are hypothesized to increase risks of diverse chronic diseases, including arthritis. Retrospective data from the World Mental Health Surveys (N=18,309) were employed to assess whether adult onset of arthritis was associated with childhood adversities and early onset psychological disorder. Cox proportional hazard models assessed the association of number of childhood adversities and the presence of early onset psychological disorder with arthritis age of onset. Controlling for age, sex and early onset mental disorder, relative to persons with no childhood adversities, persons with two adversities had increased risk of adult onset arthritis (Hazard ratio=1.27, 95% CI= 1.08, 1.50), while persons with three or more adversities had higher risk (HR=1.44, CI=1.24,1.67). Early onset depressive and/or anxiety disorder was associated with increased risk of adult-onset arthritis after controlling for childhood adversities (HR=1.43, CI=1.28, 1.61). Since psychosocial stressors may be broad spectrum risk factors that increase risks of diverse chronic conditions in later life (e.g., arthritis, heart disease, diabetes, asthma, chronic pain), prospective studies of childhood psychosocial stressors may be most productive if multiple disease outcomes are assessed in the same study. Results from this study provide methodological guidance for future prospective studies of the relationship between childhood psychosocial stressors and subsequent risk of adult onset arthritis.
PERSPECTIVE
Retrospective reports of early onset mood-anxiety disorder and multiple childhood adversities were independently associated with increased risk of adult onset arthritis. Carrying out prospective studies of these relationships entails significant challenges. Since childhood psychosocial stressors may be broad spectrum risk factors for diverse chronic conditions, multiple disease outcomes should be assessed in prospective studies assessing health consequences of childhood adversities.
Keywords: Arthritis, chronic disease, psychosocial stressors, psychological disorders, risk factors, epidemiology
Osteoarthritis is a multi-factorial disease involving trauma, genetic and inflammatory factors [15]. Allostatic load is the burden placed on homeostatic systems repeatedly activated and deactivated in response to chronic stressors [18,19]. Neural, endocrine and immune stress mediators are hypothesized to increase risks of diverse chronic diseases, including arthritis [20]. Pro-inflammatory cytokines, acting as negative regulatory signals, may play a pathogenic role in diverse chronic diseases [23], with crosstalk between brain and immune system through the hypothalamic-pituitary-adrenal axis involved in the pathogenesis of osteoarthritis [29]. Whether childhood adversities and psychological disorders influence risks of developing musculoskeletal pain has been studied, but their association with osteoarthritis has received only limited attention. Three prospective studies have found that psychosocial difficulties in childhood/young adulthood predict increased risks of developing back pain, with odds ratios (OR) ranging from 1.6-2.5 [10,22,25]. Children exposed to parental illness have been found to have increased risks of onset of unexplained physical symptoms in adulthood [9]. Raphael et al. [24] used court records to identify young adults with documented physical abuse, sexual abuse and neglect. In contrast to controls, they found non-significant increases in the occurrence of pain among documented cases of sexual abuse (OR=1.4), physical abuse (OR=1.2), and neglect (OR=1.2). However, pain symptoms were more strongly associated with retrospective reports of abuse. McBeth et al. [17] reported a case-control study of chronic widespread pain (CWP) with non-significant trends toward increased risk of CWP associated with parental loss (OR=1.8), hospitalization (OR=4.8) and abuse (OR=4.1). However, cases with chronic widespread pain were more likely to report undocumented hospitalizations, suggesting biased recall of life events.
In research specifically relevant to osteoarthritis, Danese et al. [3], found that maltreated children showed a significant increase in inflammatory markers (C-reactive protein) twenty years later (OR=1.80). Kopec and Sayre [14] found that, among 9,159 persons without arthritis at baseline, multiple childhood adversities were associated with increased risk of developing arthritis over a four year follow-up. They found that the presence of 2+ childhood adversities was associated with a hazard ratio (HR) of 1.27, which was of borderline significance. An extended hospital stay in childhood (HR=1.33) and being very scared in childhood (HR=1.29) were significantly associated with increased risk of arthritis onset. Given these results, further research assessing whether childhood psychosocial stressors are associated with increased risks of developing arthritis is warranted. This primary aim of this paper is to evaluate the association of childhood psychosocial stressors with risk of arthritis onset employing retrospective data with prospective (time-to-event) analyses. A secondary aim is to consider implications of study results for design of future prospective studies of the association of childhood psychosocial stressors with adult onset osteoarthritis.
METHODS
Samples
In this paper, we employ data from 10 countries participating in the World Mental Health Surveys to assess whether adult onset of arthritis is associated with retrospective reports of early onset psychological disorder and exposure to childhood adversities. The ten surveys included in the analyses reported here were those that collected data on childhood adversities and age of onset of arthritis. Theseten surveys were carried out in the Americas (Colombia, Mexico, United States), Europe (Belgium, France, Germany, Italy, Netherlands, Spain), and Asia (Japan). All surveys were based on multi-stage, clustered, area probability household samples. All interviews were carried out face-to-face by trained lay interviewers. Sample sizes ranged from 2372 (Netherlands) to 9282 (United States). Response rates ranged from 45.9% (France) to 87.7% (Colombia), with an average response rate of 66.7%.
Internal sub-sampling was used to reduce respondent burden and average interview time and cost by dividing the interview into two parts. Part-1 included the core diagnostic assessment of mental disorders with questions about age of onset for each mental disorder present on a lifetime basis. Part-2 included additional information relevant to a wide range of survey aims, including assessment of chronic physical conditions. All respondents completed part-1. All part-1 respondents who met criteria for any mental disorder and a probability sample of other respondents were administered part-2. Part-2 respondents were weighted by the inverse of their probability of selection for part-2 of the interview to adjust for differential sampling. Analyses in this article were based on the weighted part-2 subsample. Additional weights were used to adjust for differential probabilities of selection within households, adjust for non-response and to match the samples to population socio-demographic distributions.
Training and Field Procedures
The central World Mental Health (WMH) staff trained bilingual supervisors in each country. The WHO translation protocol was used to translate instruments and training materials. Some surveys were carried out in bi-lingual form (Belgium). Other surveys were carried out exclusively in the country’s official language. Persons who could not speak these languages were excluded. Quality control protocols, described in more detail elsewhere [13], were standardized across countries to check on interviewer accuracy and to specify data cleaning and coding procedures. The institutional review board of the organization that coordinated the survey in each country approved and monitored compliance with procedures for obtaining informed consent and protecting human subjects.
Mental disorder status
All surveys used the World Mental Health Survey version of the WHO Composite International Diagnostic Interview (WMH-CIDI, now CIDI 3.0) [12], a fully structured diagnostic interview, to assess mental disorder status. Methodological evidence collected in the WHO-CIDI Field Trials and later clinical calibration studies showed that all the disorders considered herein were assessed with acceptable reliability and validity in the original CIDI [31], and the CIDI 3.0 [7]. Disorders were assessed using the definitions and criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) [1]. CIDI organic exclusion rules were imposed (the diagnosis was not made if the respondent indicated that the episode of depressive or anxiety symptoms was due to physical illness or injury or use of medication, drugs or alcohol).
This paper includes anxiety disorders (generalized anxiety disorder, panic disorder and/or agoraphobia, post traumatic stress disorder, and social phobia) and depressive disorders (dysthymia and major depressive disorder) that were reported to have onset prior to age 21. A secondary analysis employed anxiety and depressive disorders that were present in the current (12 month) period. Anxiety and depressive disorders were aggregated into a single category denoted as depressive and anxiety disorders, on the basis of prior findings from the World Mental Health surveys that anxiety disorders and depressive disorders have similar relationships with a wide range of chronic physical conditions [26].
Assessment of childhood family adversity
The following childhood adversities were included in the present report: physical abuse, sexual abuse, neglect, parental death, parent divorce, other parental loss, parental mental disorder, parental substance use, parental criminal behavior, family violence, and family economic adversity. The aim was to assess the occurrence of childhood adversities occurring in the context of the family, not all possible childhood adversities. Thus natural disasters or exposure to war were not assessed. Those respondents who reported that an adversity occurred before the age of 18 and met the criteria specified for a given adversity were classified as having experienced a particular familial childhood adversity. Interpersonal losses were assessed with measures developed for the National Comorbidity Survey Replication [11] about parental death, divorces, and other parental separations (adoption, foster placement, living with other relatives instead of parents). Parental criminality, family economic adversity, and sexual abuse were also assessed with measures developed for the National Comorbidity Survey Replication. Parental mental illness (major depression, generalized anxiety disorder, panic disorder, antisocial personality disorder) and substance abuse were assessed with the Family History Research Diagnostic Criteria Interview [4]. Family violence and physical abuse of the respondent by parents were assessed with a modified version of the Conflict Tactics Scale [27]. Neglect was assessed using a battery of questions commonly used in studies of child welfare [2]. The rationale for focusing on adversities occurring in a family context was that these are more likely to be sustained over long periods of time and, thereby, more likely to have chronic health effects. A detailed description of the methods used to assess each of the childhood adversities is provided in Appendix A.
Assessment of arthritis
In a series of questions about chronic conditions adapted from the U.S Health Interview Survey, respondents were asked about the presence of selected chronic conditions. Respondents were asked whether they had ever had arthritis or rheumatism. Respondents with a history of arthritis were asked how old they were when the condition began. Only those reporting onset of arthritis after the age of 20 were used in the current analyses. Prior research offers support for the agreement of self-report and arthritis diagnoses in medical records [8] ] and clinically assessed arthritis [16]. In this paper, the term arthritis refers to self-reported arthritis by survey respondents, potentially including many forms of arthritis, but in general population samples the dominant condition is likely to be osteoarthritis
Data Analysis
The association of childhood adversities and early-onset mental disorders with adult-onset arthritis was studied with discrete-time survival analyses, using retrospective self-report of age of onset of arthritis. Persons who had not developed arthritis were censored at their current age. The start of the period at risk of adult-onset arthritis was set at age 20. Persons who reported that arthritis developed before age 21 were excluded.
First, Kaplan-Meier curves were developed for graphical comparison of the age-specific cumulative proportion of respondents reporting onset of arthritis comparing three categories of number of childhood adversities: none, one, and two or more adversities. Kaplan-Meier curves were also used to compare onset of arthritis for persons with and without early onset depression and/or early onset anxiety disorder. Cox proportional hazards models were then developed to estimate the relative risk of adult-onset of arthritis as a function of categories of number of childhood adversities and early-onset depression/anxiety disorder status. In these analyses, time to age of onset of arthritis from age 20 was the dependent variable. The number of different childhood adversities in four categories (none, 1, 2, 3+) and early onset mental disorder status were independent variables. The no adversities category and persons without early onset depression or anxiety disorder served as the reference groups. All associations were expressed as hazard ratios (HR), measuring the relative risk after adjustment for potential confounders including current age and sex. Since the French survey did not ask a question about educational attainment comparable to the other surveys, educational status was missing for France. We repeated the main analyses controlling for age, sex and education, with education entered as a dichotomous variable split at the median level for each country, for all surveys except France. The results were not different, so the analyses including the French survey are reported here.
To account for the possibility of differential recall of childhood adversities among those with a current mood or anxiety disorder, we performed an analysis assessing the association of childhood adversities with adult onset arthritis adjusting for current (12-month) anxiety or mood disorder. Childhood adversities and early onset mental disorders were included in the Cox models both singly and simultaneously to investigate to what extent they were independently associated with the risk of adult onset arthritis. We screened for interaction of childhood adversities and early onset mental disorders in predicting adult onset arthritis. We also estimated the hazard ratios for specific childhood adversities and for specific mental disorders (adjusted for age and sex with stratification by country).
Country was included in all analyses as a stratifying variable, which allowed each country to have a unique hazard function in analyses that provided pooled estimates of the hazard ratios across countries. Confidence intervals (95%) were estimated for all hazard ratios. Statistical significance was evaluated with p=0.05 for a two-sided test. The analyses were performed using the SURVIVAL procedure in SUDAAN statistical software to account for the complex sample design [28].
RESULTS
Across all 10 surveys, 18,309 World Mental Health Survey respondents were included in analyses assessing the association of childhood psychosocial stressors with risk of developing arthritis after age 21. The demographic characteristics of the sample, and weighted population estimates of the frequency of childhood adversities and early onset mood/anxiety disorder, are shown in Table 1. In the combined populations, the most common childhood adversities in the surveyed populations were death of a parent (12.8%), parental divorce (9.8%), physical abuse as a child (9.6%), and family violence (9.4 %). Almost half of the surveyed populations reported at least one childhood adversity, while 18.1 % reported two or more childhood adversities. About 10% of the population reported early onset mood or anxiety disorder, while 17.6% reported arthritis onset as an adult.
Table 1.
Sample characteristics (N=18309), weighted estimates
| Mean age | 45.5 (SD=16.2) |
|---|---|
| Female | 52.5 % |
| Completed secondary education | 61.6 % |
| Childhood adversities | |
| Parental death | 12.8 % |
| Parental divorce | 9.8 % |
| Other parental loss | 5.3 % |
| Physical abuse as a child | 9.6 % |
| Family violence | 9.4 % |
| Parental mental disorder | 7.1 % |
| Neglect as a child | 6.5 % |
| Family economic adversity | 5.8 % |
| Family criminal behavior | 3.3 % |
| Parental substance abuse | 5.0 % |
| Sexual abuse as a child | 2.5 % |
| Number of childhood adversities | |
| None | 56.3 % |
| One | 25.6 % |
| Two | 9.8 % |
| Three or more | 8.3 % |
| Early onset mood/anxiety disorder | 10.2 % |
| Adult onset arthritis | 17.6 % |
There was considerable cross-national variability in the prevalence of multiple childhood adversities and in the prevalence of adult onset arthritis (Table 2). To control for possible ecological correlation of childhood adversities and arthritis, the survival analyses were stratified by country so that a unique hazard function was estimated for each country, with hazard ratio estimates aggregated across country strata to provide pooled estimates.
Table 2.
Percent with two or more childhood adversities and early onset mood/anxiety disorder by country (weighted estimates and unweighted sample size).
| 2+ childhood adversities |
Adult onset arthritis |
(N unweighted) |
|
|---|---|---|---|
| Colombia | 35.7 % | 6.1 % | 2140 |
| Belgium | 11.3 % | 17.5 % | 970 |
| France | 15.2 % | 27.2 % | 1281 |
| Germany | 8.3 % | 10.4 % | 1284 |
| Italy | 6.7 % | 23.6 % | 1614 |
| Netherlands | 13.0 % | 10.7 % | 1054 |
| Spain | 5.2 % | 20.0 % | 1937 |
| Japan | 11.3 % | 7.4 % | 855 |
| Mexico | 25.5 % | 5.9 % | 2032 |
| United States | 24.3 % | 26.7 % | 5139 |
The risk of developing adult onset arthritis was substantially higher among persons who reported onset of a mood or anxiety disorder prior to age 21, as shown by the Kaplan-Meier curves in Figure 1. By age 65, the risk of developing arthritis by age 65 was around 60% for those with early onset psychological disorder, whereas it was less than 40% for those without. It should be noted that these estimates of lifetime risk of arthritis onset exclude persons with arthritis onset before age 21.
Figure 1.
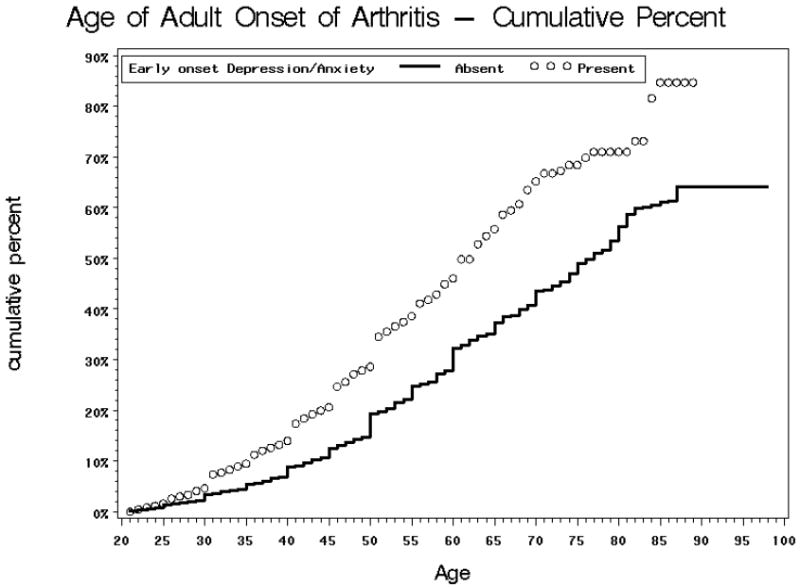
Cumulative percent with adult onset arthritis by presence or absence of early onset mood or anxiety disorder (persons reporting arthritis onset prior to age 21 excluded).
While there was essentially no difference in risk of adult onset arthritis between persons with no childhood adversities and those reporting a single childhood adversity, there was increased risk of arthritis among persons reporting two or more childhood adversities (see Figure 2). The risk of developing arthritis began to diverge for persons with multiple childhood adversities only after the age of 35. By age 65, about 45% of persons with multiple childhood adversities had developed arthritis, while about 35% of those without multiple childhood adversities had developed arthritis.
Figure 2.
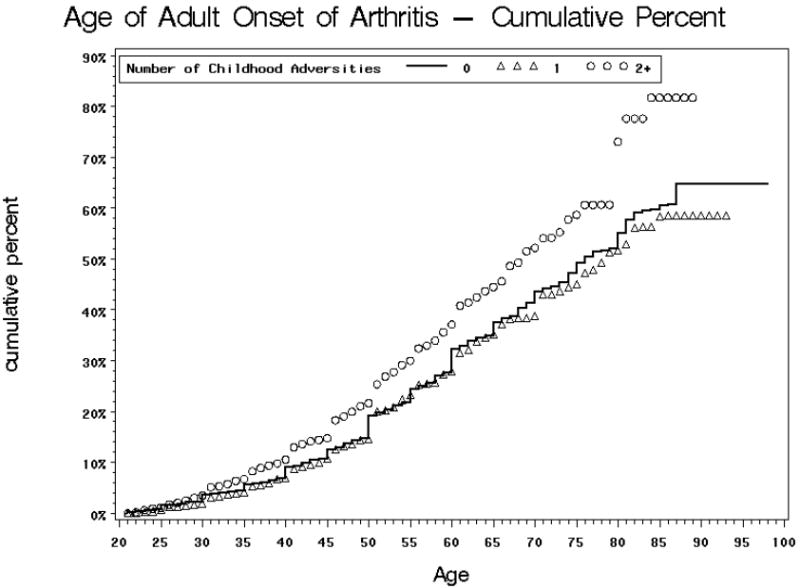
Cumulative percent with adult onset arthritis by number of childhood adversities (persons reporting arthritis onset prior to age 21 excluded).
As shown in Table 3, an initial multivariate analysis assessed whether the number of childhood adversities was associated with differences in risk of developing arthritis during adulthood. This initial analysis (see Model One) controlled for age, sex and country, but did not control for mental disorder status. Persons who reported two childhood adversities (relative to those with no childhood adversities, were at significantly increased risk of adult onset arthritis (hazard ratio=1.31), while persons reporting three or more childhood adversities were at still higher risk (hazard ratio=1.53). This suggests a dose-response relationship between number of childhood adversities and risk of adult onset of arthritis. Consistent with the descriptive analysis shown in Figure 2, the presence of a single childhood adversity was not associated with increased risk of developing arthritis in adulthood.
Table 3.
Survival analyses estimating hazard ratios (and 95% confidence intervals) for adult onset arthritis with stratification by country. [All models control for sex and current age and are stratified by country].
| Childhood adversities |
Early onset mood-anxiety disorder |
Current mood-anxiety disorder |
||||||
|---|---|---|---|---|---|---|---|---|
| None | One | Two | Three or More | Absent | Present | Absent | Present | |
| Model One: Effect of childhood adversities without controlling for mood/anxiety disorder | 1.00 | 1.02 [.89,1.16] | 1.31 [1.12,1.54] | 1.53 [1.31,1.78] | ||||
| Model Two: Effect of childhood adversities controlling for current mood/anxiety disorder | 1.00 | 1.01 [.88,1.15] | 1.28 [1.09,1.50] | 1.43 [1.24,1.60] | 1.00 | 1.43 [1.29,1.57] | ||
| Model Three: Effect of childhood adversities and early onset mood/anxiety disorder | 1.00 | 1.00 [.88,1.14] | 1.27 [1.08,1.50] | 1.44 [1.24,1.67] | 1.00 | 1.43 [1.28,1.61] | ||
| Model Four: Effect of early onset mood/anxiety disorder without controlling for childhood adversities | 1.00 | 1.52 [1.36,1.70] | ||||||
Notes: Interaction of early onset mood disorder and presence of multiple childhood adversities was non-significant.
An important methodological question is whether the association of childhood adversities and arthritis may be explained by the higher prevalence of mood and anxiety disorder among persons with arthritis. If mood disturbance resulted in increased likelihood of recalling negative childhood experiences, this could affect retrospective evaluation of the association of childhood adversities and risk of developing arthritis. We addressed this issue in a survival analysis controlling for current (12 month) mood and anxiety disorder (see Model Two in Table 3). After controlling for current mood and anxiety disorder, the hazard ratio estimates did not differ appreciably from estimates not controlling for current mood and anxiety disorder (Model One).
We evaluated whether early onset psychological disorder and exposure to multiple childhood adversities were independently associated with risk of adult onset arthritis. As shown in the survival analyses estimating effects of both early onset psychological disorder and childhood adversities (Model Three, Table 3), early onset depression or anxiety disorder was associated with increased risk of developing arthritis (hazard ratio of 1.43) after controlling for childhood adversities. Likewise, the presence of multiple childhood adversities was associated with increased risk of adult onset arthritis after controlling for early onset psychological disorder.
Survival analyses that estimated the risk of developing arthritis as a function of early onset psychological disorder that did not control for childhood adversities did not appreciably alter the hazard ratio estimates (Model Four compared to Model Three in Table 3). This suggests that early onset psychological disorder exerts its effect on risk of developing arthritis independently of the association of childhood adversities and early onset psychological disorder. Similarly, a survival analysis including number of childhood adversities but not early onset psychological disorder (Model One in Table 3) yielded hazard ratio estimates that were quite similar to those that controlled for early onset psychological disorder (Model Three in Table 3). Overall, these analyses suggest that early onset psychological disorder and exposure to multiple childhood adversities are independently associated with risk of developing arthritis in adulthood. The estimates reported in Table 3 control for age and sex, and are stratified by country, but do not control for education. Replication of these analyses controlling for education (excluding the French sample) yielded very similar results (data not shown). A survival analysis was also carried out estimating the interaction effect of multiple childhood adversities and early onset mood disorder on risk of adult onset arthritis. The interaction effects were non-significant (data not shown).
We examined which childhood adversities and which early onset psychological disorders were associated with increased risk of adult onset arthritis (see Table 4). The survival analyses for these hazard ratio estimates controlled for age and sex, and were stratified by country. Each of the childhood adversities was associated with increased risk of arthritis onset except for parental death, parental divorce and family economic adversity. Sexual abuse as a child was associated with the highest arthritis risk, while the hazard ratios for the other childhood adversities were similar to each other. Each of the early onset psychological disorders (major depression, generalized anxiety disorder, social phobia, post-traumatic stress disorder and panic disorder/agoraphobia) was associated with increased risk of adult onset arthritis. Post-traumatic stress disorder had the highest hazard ratio for adult onset arthritis.
Table 4.
Hazard ratios (and 95% confidence intervals) for adult onset arthritis for specific childhood adversities and specific early onset psychological disorders. [All models control for sex and current age and are stratified by country].
| Hazard Ratio | 95% confidence interval | |
|---|---|---|
| Sexual abuse as a child | 1.64 | (1.28, 2.09) |
| Physical abuse as a child | 1.42 | (1.22, 1.66) |
| Family violence | 1.39 | (1.16, 1.67) |
| Parental substance abuse | 1.38 | (1.14, 1.67) |
| Family criminal behavior | 1.36 | (1.07, 1.71) |
| Neglect as a child | 1.29 | (1.08, 1.55) |
| Parental mental disorder | 1.27 | (1.07, 1.51) |
| Other parental loss | 1.26 | (1.04, 1.54) |
| Family economic adversity | 1.08 | (0.93, 1.26) |
| Parental death | 1.02 | (0.89, 1.18) |
| Parental divorce | 1.02 | (0.86, 1.22) |
| Post Traumatic Stress Disorder | 1.91 | (1.50, 2.43) |
| Generalized anxiety disorder | 1.69 | (1.32, 2.17) |
| Panic Disorder/Agoraphobia | 1.68 | (1.38, 2.03) |
| Major depression | 1.53 | (1.26, 1.85) |
| Social Phobia | 1.54 | (1.34, 1.76) |
DISCUSSION
In this retrospective study, multiple childhood adversities and early onset psychological disorder were found to be independent risk factors for adult onset arthritis. This suggests that major childhood adversities may influence disease risks even when life events are not associated with a diagnosable psychological disorder. Further research is needed to better understand whether and how childhood adversities and early onset mood and anxiety disorders affect stress responses that may be implicated in risks of diverse chronic physical conditions.
There are, of course, significant limits on what can be confidently inferred from a retrospective study that relies on recall of the age of onset of psychological disorder, recall of childhood adversities, and on self-report of arthritis. The limitations of this research include reliance on self-report ascertainment of arthritis, recall of age of onset of arthritis, as well as retrospective recall of childhood adversities and age of onset of lifetime psychological disorders. Apart from problems with agreement of self-reported arthritis with a medically validated diagnosis, arthritis subsumes conditions which may be etiologically distinct (e.g. degenerative joint disease, rheumatoid arthritis, other autoimmune disorders). However, osteoarthritis accounts for the large majority of arthritis cases in the general population, and prior research suggests good agreement between self-report and clinically assessed osteoarthritis [8,16]. There is evidence supporting the validity of retrospective recall of major childhood adversities for the purposes of epidemiological research [6]. However, the propensity to recall adverse life experiences may be associated with either the presence of a painful condition or with the risk of developing painful conditions, which could explain the association of retrospectively recalled adversities with occurrence of painful conditions [24]. An additional limitation of a prospective analysis based on cross-sectional community survey data concerning age of onset of arthritis is that persons who died or who were institutionalized would not be included in the sample, potentially biasing estimates.
Acknowledging these limitations, the results of this research are consistent with prospective studies which have found that childhood psychosocial stressors are associated with increased risks of developing chronic pain conditions [9,10,22,25], with increased inflammatory markers in adulthood [3], and with risk of developing osteoarthritis [14]. Based on converging evidence, the hypothesis that childhood psychosocial stressors may increase risks of adult onset chronic pain and osteoarthritis deserves further research.
The analyses reported here provide a basis for understanding complexities in carrying out valid prospective studies to address whether childhood psychosocial stressors influence risks of developing osteoarthritis (or other chronic pain conditions) in adulthood. The challenges are substantial. Specifically, ascertainment of a single type of childhood adversity (e.g. sexual abuse, physical abuse or childhood neglect) may not be sufficient as disease risk was most strongly associated with multiple childhood adversities. Ascertainment of a limited number of childhood adversities from archival records of a child welfare agency or court records may not be adequate to assess the extent of exposure to the full range of childhood adversities. Moreover, the high prevalence of childhood adversities in the general population means that evaluation of childhood adversities in controls is necessary, because many control subjects will also have experienced significant childhood adversities. The estimated increment in risk among persons with multiple childhood adversities was modest, so large sample sizes would be needed to yield adequate statistical power, an additional difficulty with following up cases ascertained from agency or court records with comparison to controls. And, the duration of follow-up over the lifespan needs to be sufficient to identify an adequate number of disease onsets to evaluate risk differentials that may appear only as cohorts achieve middle age or older. A study that followed persons from childhood until age 35 might not be able to detect effects that would subsequently appear.
For a disease as common as arthritis, a modest increase in the hazard ratio would be associated with a clinically significant difference in cumulative disease onset rates over the lifespan, so a prospective study would ideally be powered to detect a hazard ratio of about 1.30. Given the potentially long latency between exposure to childhood adversities and onset of arthritis, a fully prospective study might take thirty years or more to complete. In light of the substantial difficulties in designing and carrying out such prospective studies, determining whether childhood psychosocial stressors increase risks of developing osteoarthritis may depend on the accumulation of evidence from diverse studies, each with its own limitations and strengths.
There is now suggestive evidence that early onset mental disorders and childhood adversities are associated with increased risks of developing diverse physical diseases, including diabetes, heart disease, and asthma, as well as arthritis and other chronic pain conditions [5,30]. A key question for future research is whether early onset psychological disorder and childhood adversities are chronic stressors that induce allostatic load, thereby increasing risks of diverse chronic physical disorders. From this perspective, early onset psychological disorder and significant childhood adversities may be broad spectrum risk factors potentially influencing risks of multiple chronic physical diseases in later life. This is analogous to tobacco use, obesity, and sedentary lifestyle being broad spectrum risk factors for diverse chronic diseases including heart disease, diabetes and cancer.
If early onset psychological disorder and major childhood adversities are potential broad spectrum risk factors for diverse chronic physical conditions, then it may be productive to organize prospective research that assesses the contribution of these childhood psychosocial stressors to risks of multiple physical disease outcomes in the same study. For example, Felitti et al. [5] assessed the relationship of number of childhood adversities to multiple causes of death and found increased mortality from heart disease, cancer, chronic lung disease, and liver disease. If exposure to chronic psychosocial stressors in childhood increases risks of diverse chronic physical diseases across the adult lifespan, it would have significant public health implications.
In conclusion, a retrospective analysis of data from ten countries participating in the World Mental Health Surveys found that multiple childhood adversities and early onset depressive and anxiety disorder were independently associated with increased risk of adult onset arthritis. In combination with research that suggests that psychosocial stressors in childhood may influence risks of diverse chronic physical diseases [5,30], these results support the need for rigorous prospective studies assessing the role of exposure to multiple childhood adversities and early onset mood and anxiety disorder in subsequent risks of developing osteoarthritis. Such research is also needed for other chronic physical diseases and chronic pain conditions whose risks are hypothesized to be influenced by chronic psychosocial stress and allostatic load.
Acknowledgments
The surveys included in this report were carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13- MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R01-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, and Bristol-Myers Squibb. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/. The Mexican National Comorbidity Survey (MNCS) is supported by The National Institute of Psychiatry Ramon de la Fuente (INPRFMDIES 4280) and by the National Council on Science and Technology (CONACyT-G30544- H), with supplemental support from the PanAmerican Health Organization (PAHO). The Lebanese survey is supported by the Lebanese Ministry of Public Health, the WHO (Lebanon) and unrestricted grants from Janssen Cilag, Eli Lilly, GlaxoSmithKline, Roche, Novartis, Fogerty (R03 TW0006481) and anonymous donations. The ESEMeD project was funded by the European Commission (Contracts QLG5-1999-01042; SANCO 2004123), the Piedmont Region (Italy), Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028), Ministerio de Ciencia y Tecnología, Spain (SAF 2000-158-CE), Departament de Salut, Generalitat de Catalunya, Spain, and other local agencies and by an unrestricted educational grant from GlaxoSmithKline. The Chinese World Mental Health Survey Initiative is supported by the Pfizer Foundation. The Colombian National Study of Mental Health (NSMH) is supported by the Ministry of Social Protection, with supplemental support from the Saldarriaga
Concha Foundation. The World Mental Health Japan (WMHJ) Survey is supported by the Grant for Research on Psychiatric and Neurological Diseases and Mental Health (H13-SHOGAI-023, H14-TOKUBETSU-026, H16-KOKORO-013) from the Japan Ministry of Health, Labour and Welfare. The New Zealand Mental Health Survey (NZMHS) is supported by the New Zealand Ministry of Health, Alcohol Advisory Council, and the Health Research Council. The South Africa Stress and Health Study (SASH) is supported by the US National Institute of Mental Health (R01-MH059575) and National Institute of Drug Abuse with supplemental funding from the South African Department of Health and the University of Michigan. The Ukraine Comorbid Mental Disorders during Periods of Social Disruption (CMDPSD) study is funded by the US National Institute of Mental Health (RO1-MH61905). The US National Comorbidity Survey Replication (NCS-R) is supported by the National Institute of Mental Health (NIMH; U01- MH60u0) with supplemental support from the National Institute of Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044780), and the John W. Alden Trust.
Appendix A
Methods of Assessing Childhood Adversities
Respondents were classified as having experienced physical abuse when they indicated that, when they were growing up, their father or mother (includes biological, step or adoptive parent) slapped, hit, pushed, grabbed, shoved or threw something at them, or that they were beaten up as a child by the persons who raised them. For sexual abuse, the following questions were asked “The next two questions are about sexual assault. The first is about rape. We define this as someone either having sexual intercourse with you or penetrating your body with a finger or object when you did not want them to, either by threatening you or using force, or when you were so young that you didn’t know what was happening. Did this ever happen to you?” or “Other than rape, were you ever sexually assaulted or molested?” Sexual abuse was the only adversity where information was not collected that would distinguish whether the perpetrator was a family member or someone else. However, previous research using a similar measure, but which did allow such a distinction, showed that a good indirect way to distinguish family versus non-family sexual abuse was to ask about number of instances of victimization, with cases involving one or two instances typically perpetrated by a stranger and those involving three or more instances typically perpetrated by a family member [21]. In the WMH surveys, respondents who reported that any of these experiences occurred to them three times or more were classified as having experienced sexual abuse (within the family context).
For the assessment of neglect, two neglect scales were created. These were based on responses to the neglect items: “How often were you made to do chores that were too difficult or dangerous for someone your age?”; “How often were you left alone or unsupervised when you were too young to be alone?”; “How often did you go without things you need like clothes, shoes, or school supplies because your parents or caregivers spent the money on themselves?”; “How often did your parents or caregivers make you go hungry or not prepare regular meals?”; “How often did your parents or caregivers ignore or fail to get you medical treatment when you were sick or hurt?”. The serious neglect scale was the sum of the number of neglect items where the respondent replied “often” or “sometimes”, plus 1 if the respondent rated either of his/her parents as having spent little or no effort in watching over them to ensure they had a good upbringing. The severe neglect scale is the sum of the number of neglect items where respondents replied “often” plus 1 if the respondent rated either of his/her parents as having spent no effort in watching over them to ensure they had a good upbringing. Both the serious and severe neglect scales ranged from 0-6. For the final definition of neglect, the respondent had to have a score of at least 1 on the severe neglect scale and at least 2 on the serious neglect scale. The coding of the neglect domain was determined empirically on the basis of frequency distributions, to derive estimates in keeping with existing literature on the prevalence of these experiences in the general population.
For parental death, parental divorce, or other parental loss, respondents were first asked whether they lived with both of their parents when they were brought up. If respondents replied in the negative, they were asked: “Did your biological mother or father die, were they separated or divorced, or was there some other reason?” According to their answers to these questions, respondents were classified as having experienced parental death (i.e. when they indicated that one or both parents died), parental divorce (i.e. when they indicated that their parents divorced), and other parental loss (i.e. when respondents replied that they were either adopted, went to boarding school, were in foster care, or that they left home before the age of sixteen). For parental mental illness the following questions were asked: Parental depression was assessed by the following items: “During the years you were growing up, did the person who raised you ever have periods lasting 2 weeks or more where she was sad or depressed most of the time?” and “During the time when his/her depression was at its worst, did he/she also have other symptoms like low energy, changes in sleep or appetite, and problems with concentration?” Parental generalised anxiety disorder (GAD) was assessed as follows: “During the time you were growing up, did the person who raised you ever have periods of a month or more when he/she was constantly nervous, edgy, or anxious?” and “During the time his/her nervousness was at its worst, did he/she also have other symptoms like being restless, irritable, easily tired, and difficulty falling asleep?” Parental panic disorder was assessed by the following item: “Did the person who raised you ever complain about anxiety attacks where all of a sudden she felt frightened, anxious, or panicky?” Respondents who replied positively on the diagnostic items for any of these mental disorders were then asked whether these symptoms (a) occurred at all or most of the time, (b) interfered a lot with the life or activities of the parent or the person who raised the respondent, (c) whether their parents sought professional help for this problem. If respondents replied affirmatively on (c), and either on (a) or (b), they were coded as respondents with parental depression, GAD, or panic disorder.
Similarly, parental substance disorder was assessed with the following items: (criterion a) “Did the person who raised you ever have a problem with alcohol or drugs” and (criterion b) “Did he/she have this problem during all, most, some, or only a little of your childhood?” Respondents who replied positively on the first and “all” and “most” on the second item were then asked whether the problem interfered a lot with life or activities of the man or woman who raised the respondent (criterion c), or whether they had sought professional help for this problem (criterion d). Those respondents who replied affirmatively on criteria (a) and (b), and on either (c) or (d) were coded as having had parents with a substance disorder.
Parental criminal behaviour was assessed by the following questions: “Was the person who raised you ever involved in criminal activities like burglary or selling stolen property?” and “Was the person who raised you ever arrested or sent to prison?” Respondents who replied positively on either question were classified as having experienced criminal behaviour in the family.
Respondents were coded as having experienced family violence when they indicated that they “were often hit, shoved, pushed, grabbed or slapped while growing up” or “witnessed physical fights at home, like when your father beat up your mother?”. Family economic adversity was coded positive if there was a positive response to either item a) or item b). Item a) was: “During your childhood and adolescence, was there ever a period of six months or more when your family received money from a government assistance program like Welfare, Aid to Families with Dependent Children, General Assistance, or Temporary Assistance for Needy Families?” (This item was modified to be relevant to the welfare programs in each country where the survey was administered). Item b) was: If there was no male head of the family and the female head did not work all or most of the time during respondent’s childhood; or if there was no female head of the family and the male head did not work all or most of respondent’s childhood, or if there was no female head and no male head of the family.
Footnotes
The authors have no conflicts of interest concerning the contents of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Michael Von Korff, Group Health Center for Health Studies; 1730 Minor Avenue, Suite 1600, Seattle WA 98101 USA, Vonkorff.m@ghc.org, 206-287-2874 (ph), 206-287-2871 (Fax)
Jordi Alonso, Health Services Research Unit Institut Municipal d’Investigacio Medica (IMIM), CIBER en Epidemiologia y Salud Publica, (CIBERESP), Barcelona, Spain jalonso@imim.es.
Johan Ormel, Professor of Social Psychiatry and Psychiatric Epidemiology, University Medical Center Groningen, Netherlands, j.ormel@med.umcg.nl.
Matthais Angermeyer, Department of Psychiatry, Leipzig University, Germany, angermeyer@aon.at.
Ronny Bruffaerts, Department of Neurosciences and Psychiatry, University Hospitals Gasthuisberg Leuven, Belgium ronny.bruffaerts@uz.kuleuven.ac.be.
Clara Fleiz, National Instituto on Psychiatry Ramon de la Fuente, Mexico City, Mexico fleiz@imp.edu.mx.
Giovanni de Girolamo, Health Care Research Agency, Emilia-Romagna Region, Bologna, Italy, GDeGirolamo@Regione.Emilia-Romagna.it.
Ronald C. Kessler, Department of Health Care Policy, Harvard Medical School, Boston, MA, Kessler@hcp.med.harvard.edu.
Viviane Kovess-Masfety, Directrice Fondation MGEN pour la santé publique, Université Paris Descartes, Paris, France, vkovess@mgen.fr.
José Posada-Villa, Ministry of Social Protection, Colegio Mayor de Cundinamarca University, Bogota, Colombia, latos98@yahoo.com.
Kate M. Scott, Department of Psychological Medicine; Otago University, Wellington; PO Box 7343, Wellington South, New Zealand, kate.scott@otago.ac.nz.
Hidenori Uda, Director General, Social Welfare, and Environmental Department Osumi Regional Promotion Bureau, Kagoshima Prefecture, Japan, udah@pref.kagoshima.lg.jp.
References
- 1.APA. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 2.Courtney ME, Piliavin I, Grogan-Kaylor A, Nesmith A. Foster Youth Transitions to Adulthood: A Lognitudinal View of Youth Leaving Care. Madison, WI: Institute for Research on Poverty; 1998. [PubMed] [Google Scholar]
- 3.Danese A, Parlante CM, Caspi A, Taylor A, Poulton R. Childhood maltreatment predicts adult inflammation in a life-course study. Proc Natl Acad Sci USA. 2007;23:1319–1324. doi: 10.1073/pnas.0610362104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Endicott J, Andreason N, Spitzer RL. Family History Research Diagnostic Criteria. New York, NY: Biometrics Research, New York State Psychiatric Institute; 1978. [Google Scholar]
- 5.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood adbuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 6.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 7.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine J-P, Mazzi F, Reneses B, Vilagut G, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health Surveys. International Journal of Methods in Psychiatric Research. 2006;15:167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.He YL, Zhang M, Lin EHB, Bruffaerts R, Posada-Villa P, Andemeyer MC, Levinson D, de Girolamo G, Uda H, Mneimneh Z, Benjet C, de Graaf R, Scott KM, Gureje O, Seedat S, Haro JM, Bromet EJ, Alonso J, Von Korff M, Kessler R. Mental disorders among persons with arthritis-Results from the World Mental Health Surveys. Psychological Medicine. 2008;26:1–12. doi: 10.1017/S0033291707002474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hotopf M. Childhood experiences of illness as a risk factor for medically unexplained symptoms. Scand J Psychol. 2002;43:139–146. doi: 10.1111/1467-9450.00279. [DOI] [PubMed] [Google Scholar]
- 10.Jones GT, Watson KD, Silman AJ, Symmons DP, MacFarlane GJ. Predictors of low back pain in British school children: a population-based prospective cohort study. Pediatrics. 2003;111:822–828. doi: 10.1542/peds.111.4.822. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC, Merikangas KR. The National Comorbidity Survey replication (NCS-R): Background and aims. The International Journal of Methods in Psychiatric Research. 2004;13:60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Ustun B. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kessler RC, Bergland P, Chiu WT, Demler O, Heeringa S, Hiripi E, Jin R, Pennell B-E, Walters EE, Zaslavsky A, et al. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. International Journal of Methods in Psychiatric Research. 2004;13 doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kopec JA, Sayre EC. Traumatic experiences in childhood and the risk of arthritis: a prospective cohort study. Canadian J Public Health. 2004;95:361–365. doi: 10.1007/BF03405147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krasnokutsky S, Samuels J, Abramson SB. Osteoarthritis in 2007. Bull NYU Hosp Jt Dis. 2007;65:222–228. [PubMed] [Google Scholar]
- 16.March LM, Scwarz JM, Carfae BH, Bagge E. Clinical validation of self-reported osteoarthritis. Osteoarthritis Cartilege. 1998;6:87–93. doi: 10.1053/joca.1997.0098. [DOI] [PubMed] [Google Scholar]
- 17.McBeth J, Morris S, Benjamin S, Silman AJ, MacFarlane GJ. Associations between adverse events in childhood and chronic widespread pain in adulthood: Are they explained by differential recall? J Rheumatology. 2001;28:2305–2309. [PubMed] [Google Scholar]
- 18.McEwen BS. Stress, adaptation, and disease: allostasis and allostatic load. Ann NY Acad Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 19.McEwen BS. Protective and damaging effects of stress mediators. NEJM. 1998;338:171–9. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 20.McEwen BS, Stellar E. Stress and the individual: Mechanisms leading to disease. Arch Intern Med. 1993;153:2093–101. [PubMed] [Google Scholar]
- 21.Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. Am J Public Health. 2001;91(5):753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mustard CA, Kalcevich C, Frank JW, Boyle M. Childhood and early adult predictors of risk of incident back pain: Ontario Child Health Study 2001 follow-up. Am J Epidemiology. 2005;162:779–786. doi: 10.1093/aje/kwi271. [DOI] [PubMed] [Google Scholar]
- 23.O’Connor JC, McCusker RH, Strle K, Johnson RW, Dantzer R, Kelley KW. Regulation of IGF-I function by proinflammatory cytokines: At the interface of immunology and endocrinology. Cell Immunology. 2008 doi: 10.1016/j.cellimm.2007.09.010. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raphael KG, Widom CS, Lange G. Childhood victimization and pain in adulthood: a prospective investigation. Pain. 2001;92:283–293. doi: 10.1016/s0304-3959(01)00270-6. [DOI] [PubMed] [Google Scholar]
- 25.Power C, Frank J, Hertzman C, Schierhout G, Li L. Predictors of low back pain onset in a prospective British study. Am J Public Health. 2001;91:1671–1678. doi: 10.2105/ajph.91.10.1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scott KM, Bruffaerts R, Tsang A, Ormel J, Alonso J, Angermeyer MC, Benjet C, Bromet E, de Girolamo G, de Graaf R, Gasquet I, Gureje O, Haro JM, He Y, Kessler RC, Levinson D, Mneimneh ZN, Oakley Browne MA, Posada-Villa J, Stein DJ, Takeshima T, Von Korff M. Depression-anxiety relationships with chronic physical conditions: results from the World Mental Health Surveys. J Affect Disord. 2007;103(13):113–120. doi: 10.1016/j.jad.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 27.Straus MA. Measuring introfamily conflict and violence: the Conflict Tactics (CT) Scales. J Marriage Fam. 1979:75–88. [Google Scholar]
- 28.SUDAAN: Software for the statistical analysis of correlated data [program] Research Triangle Park; North Carolina, USA: 1999. [Google Scholar]
- 29.Vassiloupoulos D, Mantzoukis D. Dialogue between the brain and the immune system in inflammatory arthritis. Ann NY Acad Science. 2006;1088:132–138. doi: 10.1196/annals.1366.031. [DOI] [PubMed] [Google Scholar]
- 30.Von Korff M, Scott K, Gureje O, editors. Global Perspectives on Mental Disorder and Physical Illness in the World Mental Health Surveys. Cambridge University Press; In press. [Google Scholar]
- 31.Wittchen H-U. Reliability and validity studies of the WHO Composite International Diagnostic Interview (CIDI): a critical review. Journal of Psychiatric Research. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]


