Abstract
Objective
To examine the long-term efficacy of both fear-inducing arguments and HIV counseling and testing at encouraging and maintaining knowledge about HIV transmission and prevention, as well as condom use.
Design
Analyses were conducted with a sample of 150 treatment groups and 34 controls and included measures of change at an immediate follow-up and a delayed follow-up.
Main outcome measures
The main outcome measures were perceived risk of HIV infection, knowledge about HIV, and condom use.
Results
Results indicated that receiving fear-inducing arguments increased perceptions of risk at the immediate follow-up but decreased knowledge and condom use, whereas resolving fear via HIV counseling and testing decreased perceptions of risk and increased knowledge and condom use at both the immediate and delayed follow-ups. The effects on perceived risk and knowledge decreased over time, but the effects on condom use became more pronounced.
Conclusion
Inducing fear is not an effective way to promote HIV-relevant learning or condom use either immediately following the intervention or later on. However, HIV counseling and testing can provide an outlet for HIV-related anxiety and, subsequently, gains in both knowledge and behavior change immediately and longitudinally.
Keywords: longitudinal behavior change, HIV prevention, fear appeals, HIV counseling and testing, meta-analysis
Much past research has tested the effectiveness of intervention programs targeting a reduction of HIV/AIDS risk and an increase in HIV/AIDS-related knowledge among various populations (for reviews, see Albarracín et al., 2003, 2005; B. T. Johnson, Carey, Marsh, Levin, & Scott-Sheldon, 2003; W. D. Johnson et al., 2002). Of the various ways of achieving these objectives, appeals to increase perceptions of risk and the administration of an HIV test have enjoyed considerable popularity for a number of years (see Albarracín et al., 2003; Albarracín, Kumkale, & Johnson, 2004; Fisher & Fisher, 1992).
Fear appeals usually describe the threat of HIV as significant, or even imminent, given the stated audience's risk for contracting the disease (Fisher, Fisher, Bryan, & Misovich, 2002; Kelly, St. Lawrence, Hood, & Brasfield, 1989). Ideally, because fear is arousing, these strategies should facilitate learning and, eventually, behavior change. Two prior meta-analyses of HIV-prevention interventions, however, have indicated that fear-inducing arguments do not produce increases in behavior change (Albarracín et al., 2005; Durantini, Albarracín, Mitchell, Earl, & Gillette, 2006). This finding is consistent with a potential side effect of fear appeals. If recipients attempt to control their fear by not paying attention to the intervention content (McGuire, 1968; see also Williams, Mark, Mathews, & MacLeod, 1996, for a review of the “emotional Stroop effect”), then fear appeals should deter from gains in both HIV knowledge and condom use. However, the potential effects of fear-inducing arguments on knowledge gains, or, for that matter, on risk perceptions themselves, were never explored in those prior reviews.
Another finding from the Albarracín et al. (2005) meta-analysis is that HIV counseling and testing successfully increase condom use. It is important, however, to note that no direct comparison between the effects of fear-inducing arguments and HIV counseling and testing was provided. This omission is important because such comparisons are meaningful to understand the effects of risk perceptions in behavior change. In particular, all clients who freely seek an HIV test must have concluded that they may be infected, even when approximately 98% of U.S. individuals undergoing testing will find out that they are actually HIV negative (Centers for Disease Control and Prevention [CDC], 2001a). In other words, the initial risk sensitization followed by the favorable resolution of the fear may be pleasantly surprising to many of the individuals who seek testing. Thus, whereas the initial fear may motivate individuals to avoid the experience of fear in the future, the resolution of the fear may free up cognitive resources for the processing of the recommendations the counselor delivers. If this is the case, HIV counseling and testing should be much more successful at increasing knowledge and changing behavior than the presentation of fear-inducing arguments. This advantage should be present even after controlling for various differences in the techniques used in these two strategies.
In this article, we provide a detailed examination of the efficacy of fear-inducing arguments and HIV counseling and testing over a period of time. Specifically, we synthesized the impact of these strategies on (a) perceived risk of contracting HIV, (b) knowledge about HIV transmission and prevention, and (c) actual condom use. This detailed approach consisted of examining various shapes of the influence of fear-inducing arguments, including direct and reverse linear relations, as well as curvilinear and moderated patterns. With respect to the time span we considered, the effects of any intervention can require time to manifest themselves. Thus, we analyzed change at the time of an immediate follow-up and also a delayed follow-up. In this regard, the negative or positive effects of an intervention on behavior could spiral, becoming more pronounced later rather than earlier in the change process (for a meta-analysis of sleeper effects in the experimental persuasion literature, see Kumkale & Albarracín, 2004). To our knowledge, however, such hypothetical patterns have never been studied in a meta-analysis of behavior change, which led us to synthesize studies of HIV-prevention outcomes reporting data from two measures following the intervention. We used the data set analyzed by Albarracín et al. (2005), except that effect sizes were calculated for two follow-ups instead of one and studies were added because of a later cutoff date in the bibliographic search.
Hypothetical Effects of Fear-Inducing Arguments
Although the role of fear appeals has been debated for decades, the effectiveness of threatening the recipients of health recommendations is unclear. On one hand, fear can motivate individuals to learn to shun risky behaviors (see e.g., Hovland, Janis, & Kelley, 1953; Hull, 1943; Miller & Dollard, 1941). This prediction implies that risk-reduction behavior is a direct function of fear. In the context of our research, recipients of fear-inducing arguments may be particularly motivated to attend to the intervention content. Therefore, those participants may have gains in knowledge about both HIV and condom use.
On the other hand, there is a diversity of empirical findings that contradicts the intuitive hypothesis that fear facilitates risk-reduction behavior. Empirical tests of this hypothesis have actually proven inconclusive, to the point of showing that fear can also depress behavior change (see Albarracín et al., 2005). Janis and Feshbach (1953), for example, reported that increasing the degree of threatening material in the content of messages about dental hygiene ironically decreased compliance. Along the same lines, McGuire (1968, 1972), who postulated various steps of information processing in persuasion, highlighted the possibility that fear might have antagonistic effects on attending and subsequently yielding to the intervention's recommendation.
Thus, fear-inducing interventions to prevent HIV may be detrimental rather than beneficial. As Rothman and Salovey (1997) suggested, messages designed to maintain health, such as condom use to prevent infection with HIV, might be undermined by describing outcomes in terms of what may be lost by not engaging in the targeted behavior (e.g., contracting HIV by not using a condom).1 Using a loss frame may even backfire, instead facilitating preferences for risky options (Rothman & Salovey, 1997).
Like many such controversies, it has been argued that fear appeals are effective only if the appropriate conditions are met. To begin, fear inducements may be effective only in the presence of a clear, feasible recommendation. After all, the drive reduction model (Hovland et al., 1953) suggests that, for fear appeals to be successful, the recommended behavior must be effective at diverting threat and possible for the recipients to implement. According to this model, then, people are likely to change their behavior if they are sufficiently scared plus they know and are able to do what they have to do to reduce their risk. The resulting prediction curve illustrates a curvilinear influence of the intensity of the fear-inducement argument on behavior change. In our meta-analysis, this relation was addressed by coding four levels of intensity on the basis of the number of fear appeals presented. In addition, we weighted these scores by the duration of the fear-inducing intervention, following the rationale that longer fear appeals may be more fear inducing than shorter ones.
The seminal ideas of Hovland et al. (1953) received attention years later when Leventhal (1970) proposed his parallel response model. Leventhal posited that fear appeals could independently induce both a response to control the fear (coping with the emotion) and a response to control the danger (coping with the problem). Therefore, reassuring recommendations could elicit attempts to control the danger (see also Fisher & Fisher, 1992), whereas the absence of such recommendations could force recipients to control the fear (see also Eppright, Hunt, Tanner, & Franke, 2002). In this light, we examined whether fear-inducing HIV-prevention interventions included (a) information about condom use as a means for protection and (b) behavioral skills arguments or training to facilitate condom use and, if so, whether these strategies interacted with the fear inducements.
Another postulated condition is the complexity of the intervention content. According to McGuire (1968), inducing fear when recommending a prevention strategy is likely to be successful if the fear itself does not hinder comprehension or enhance avoidance of the intervention content. For that reason, the intensity of the induced fear may interact with the complexity of the intervention content: Fear appeals should be more persuasive when the content is easy to comprehend but less persuasive when the content is difficult to comprehend. To test this prediction, we compared the effects of fear-inducing arguments when the audience had different levels of education, with the rationale that more-educated people should find it easier to comprehend all materials than less-educated people.
Finally, whatever impact fear-inducing interventions might have, these effects should be more pronounced when the recipients have good reasons to experience fear. For example, determining that one is at risk for HIV could be much more fear inducing when the problem is highly salient in the community as a whole. It also may be more fear inducing in highly affected areas where participants may be more likely to know someone who is HIV positive and, thus, have a vivid example of how devastating HIV can be. If this is so, the effects of fear-inducing arguments may be stronger in areas such as sub-Saharan Africa. The same effects, however, may be much smaller in communities that do not experience HIV as such a devastating and daily problem.
Hypothetical Effects of Resolving Fear Through HIV Counseling and Testing
Since 1994, the CDC (2001b) has recommended that all HIV tests include behavioral counseling. In the typical structure of the test administration, participants first provide a blood sample and self-assess their personal risk for contracting HIV and then await the results during a period that is generally filled with anxiety (Kelly, 1995; see also Carroll, Dockery, & Shepperd, in press). During the feedback session, the counselor reports the test results and makes suggestions for either remaining seronegative or coping with seropositivity.
Whereas the presentation of fear-inducing arguments is designed to heighten fear, for seronegative individuals, the testing situation initially increases fear but then can provide a favorable resolution of the fear. For instance, data from the CDC (2001a) indicate that an overwhelming majority of test takers in the United States receive a negative result. Thus, HIV counseling and testing may be particularly relieving compared with the possibility of an intervention designed to increase perceived HIV risk.
Of course, in areas with higher seropositivity rates, such as sub-Saharan Africa, the testing procedures may not always resolve the fear experienced in anticipation of the test. Moreover, the level of fear in anticipation of the test as well as the degree of relief experienced if the test is negative could be a function of the difference between seropositivity levels of the tested study group sample and of the population from which the study group sample is drawn. Overall, study groups undergoing HIV testing may be more likely to experience a reduction in fear when the level of seropositivity in the study group is lower than the level of seropositivity in the population. In contrast, there may be no such reduction when the level of seropositivity in the study group is higher than the level of seropositivity in the population. That is, at an individual level, experiencing a better than expected outcome may produce pleasantly surprising emotions, but experiencing a worse than expected outcome may produce disappointment (see, e.g., Albarracín, in press; Shepperd & McNulty, 2002). If emotions can motivate behavior change, then the experience of either pleasantly surprising emotions or disappointment may motivate participants to engage in risk-reduction behavior. Overall, then, these study groups should post higher positive changes in condom use relative to study groups with individuals whose outcomes match their expectations and, thus, do not experience these motivating emotions.
Although the results associated with a positive test can reduce risk behavior (e.g., Weinhardt, Carey, Johnson, & Bickham, 1999), the emotional state accompanying a negative test can also reduce risk behavior. Theoretically, after receiving a negative test result, participants will experience positive affect at the removal of an aversive stimulus like the possibility of being seropositive (Baum, 1994). In this case, participants would likely attend to and follow the counselor's recommendations with the objective of maintaining the positive affect they are experiencing (see, e.g., Isen, 1987). In other words, the positive affect induced by this fear resolution may increase the motivation to never experience the fear again, thus reducing risky behaviors and increasing associated knowledge.
Decay and Spiral of the Long-Term Effects of Fear-Inducing Arguments and HIV Counseling and Testing
According to McGuire (1972), people must retain the psychological change they experience for the change to crystallize in future, consistent behaviors. For instance, people must remember the intervention recommendation not only immediately after participation in a prevention program but also later, when the opportunity for engaging in the recommended behavior arises. For this reason, we were interested in verifying change in knowledge and behavior at two points in time, one closer and one farther away from exposure to the preventive intervention.
Two distinct longitudinal patterns may emerge for changes in condom use (a behavior) and changes in fear (an emotion). On one hand, the effect on behavior may spiral over time (i.e., those using condoms frequently will increase condom use, and those using condoms infrequently will decrease condom use). If HIV counseling and testing sessions successfully increase condom use, condom use may become habitual (Ouellette & Wood, 1998), the decision to use condoms may be reinforced (Bem, 1965, 1972; see more recently Albarracín & Wyer, 2001), and greater environmental rewards may be produced (Baum, 1994). Thus, using condoms may promote further condom use and strengthen the effect of the intervention as time elapses. By the same token, if fear appeals decrease condom use immediately after the intervention, this lack of behavioral success may become stronger at the time of longitudinal measures. On the other hand, emotions such as fear do not endure; they tend to fade away (Clore & Schnall, 2005). Thus, effects on risk perceptions immediately after fear-inducing arguments or HIV counseling and testing may be significantly smaller at the time of the delayed follow-up.
Method
Review and Inclusion Criteria
We conducted a thorough review of reports that were available by January 2005.2 For inclusion in this meta-analysis, studies had to meet several eligibility criteria.
Studies were included if they described the outcomes of a standard intervention to promote condom use. We excluded interventions to promote safer intravenous drug-related behaviors or abstinence from sex, except when they also included a condom use component.
Reports had to include pretest assessments to determine change over time.
The studies we included concerned long-term outcomes beyond the most immediate follow-up examined in other reviews (see, e.g., Albarracín et al., 2005). As such, we excluded studies in which the researchers only obtained or only reported outcomes for a single posttest.
Studies had to present appropriate statistics to calculate standardized effect sizes representing change from the pretest to the first and second posttests in our analyses. We excluded reports when the selected statistics could not be calculated.
Of the 735 research reports considered for inclusion in this meta-analysis, 76 met our inclusion criteria, providing 184 statistically independent groups or units.3 Of note, 175 of the 184 groups included in this meta-analysis were a subset of a larger sample of studies that generally included a single follow-up and were reported in another report (see Albarracín et al., 2005; cutoff date = September 2003). However, neither the longitudinal analyses nor the direct comparison of fear increment and fear resolution of interest here was presented in the earlier meta-analysis. The focus of the earlier meta-analysis was testing the effectiveness of different contents of interventions across different populations and contexts. Instead, the focus of the present meta-analysis was to contrast the immediate and longitudinal effects of fear-inducing arguments and HIV counseling and testing.
Coding of Study Characteristics
To examine the efficacy and longitudinal patterns of fear-inducing arguments and HIV counseling and testing, each report was coded for the inclusion of these strategies as well as other characteristics of the research. Two independent raters coded characteristics relevant to the report and the methods used in the studies. Intercoder agreement for all categories included in the coding sheet was 85%. Disagreements were resolved by discussion and further examination of the studies.
Fear-inducing arguments
We coded interventions for the presence or absence of risk arguments, which are designed to heighten participants’ awareness of their personal risk of contracting HIV (Kelly et al., 1989, 1992). These arguments typically describe the health problems associated with HIV/AIDS (Carey et al., 1997) or attempt to sensitize the audience to their own HIV risk (e.g., Brown, Reynolds, & Lourie, 1997). To assess the shape of the relation between fear inducements and behavior change, we split the data into four groups on the basis of number of fear-inducing arguments and analyzed the effects of delivery intensity. We first recorded the presence or absence of (a) an explicit mention of personal risk of contracting HIV or sexually transmitted infections (STIs), (b) an explicit mention of health problems associated with these diseases, and (c) other strategies, such as reminding participants of a known person who contracted an STD in the past year. We summed the presence or absence of these types of fear-inducing arguments (each dummy coded), creating a score that varied from 0 to 3. Second, we weighted the sum of the three fear-inducing arguments by the duration of the intervention (in minutes), with the rationale that longer, more intense interventions that include fear inducements might achieve higher levels of fear than shorter, less intense ones.4
HIV counseling and testing
We also coded for the presence or absence of HIV counseling and testing. HIV counseling and testing sessions generally include assessments of knowledge about HIV transmission and prevention, as well as personal risk of contracting HIV (e.g., CDC, 2001b). Often, the counselor and client discuss personal barriers to and resources available for risk reduction in an attempt to increase the behavioral skills that can promote change (e.g., Kelly, 1995). Thus, with the exception of the test administration, the counseling can comprise fear-inducing arguments as well as other intervention strategies that are used outside of the context of a test.5
Study group sample and population HIV rates
To test predictions about the effects of the strategies of interest as a function of the HIV rate of the population and/or the study group sample, we recorded the study group HIV infection rate whenever it was available. Furthermore, we retrieved population HIV infection rates from UNAIDS, UNICEF, and the World Health Organization (2004a, 2004b, 2004c), using country as the underlying population, and subtracted the study group sample rate from the population rate to analyze whether these differences moderate the impact of HIV counseling and testing.6
Retrieval of Effect Sizes
For each report, two raters independently calculated effect sizes. Disagreements were examined by a third researcher and resolved by discussion. Raters were instructed to calculate effect sizes representing change from the pretest to the first posttest for immediate effects and from the pretest to the second posttest for delayed effects. Efforts were made to calculate effect sizes for all measures of the constructs of interest measured in each report. When there was more than one measure of a construct in a particular study, we first calculated effect sizes for each one and then obtained the average, which was used as the effect size for that particular variable (B. T. Johnson, 1993).
To represent change from the pretest to the posttest measures, we used Becker's (1988) g, which is calculated by subtracting the mean at the earlier time (e.g., pretest) from the mean at the later time (e.g., the immediate posttest) and dividing the difference by the standard deviation of the earlier measure (e.g., the pretest). We calculated effect sizes representing change in perceived risk, knowledge, and condom use. In all cases, we considered the wording of the measures and not the authors’ labels for the constructs (see also Albarracín et al., 2003). Below we describe typical measures accepted as indexes of each variable.
Perceived risk
Perceived risk was typically measured with participants’ assessments of the likelihood that they could become infected with HIV in the future (e.g., “There is practically no chance I could get AIDS” [reverse-scored]; O'Leary, Jemmott, Goodhart, & Gebelt, 1996, p. 520).
Knowledge
Many studies assessed the participant's knowledge about HIV or AIDS using a series of statements that the participant evaluated as true or false (e.g., “The AIDS virus can be caught through ordinary close social contact, such as sitting next to an infected person”; Rigby, Brown, Anagnostou, Ross, & Rosser, 1989, p. 149). Knowledge scores in most cases were calculated by computing the percentage of questions a participant answered correctly. When researchers reported statistics for individual items, we calculated effect sizes for each question and then averaged those effects into a global measure of change in knowledge (see B. T. Johnson, 1993).
Condom use
Condom use measures included assessments of subjective frequency scales as well as reports of the number of times participants used condoms and the percentage of condom use over intercourse occasions. For example, the CDC AIDS Community Demonstration Projects Research Group (CDC, 1993) asked participants, “When you have vaginal sex with your main partner, how often do you use a condom?” (p. 11), and participants provided their response on a scale from 1 (every time) to 5 (never). Similarly, to obtain a more precise report of condom use, Ploem and Byers (1997) asked participants to report the frequency of sexual intercourse over the previous 4 weeks as well as the number of occasions of sexual intercourse for which condoms were used. The researchers then derived a percentage of condom use for each participant. In addition, many researchers analyzed change in the number of occasions of unprotected sex (Allen et al., 1992) or the percentage of times participants had unprotected sex during a given period of time (Collins, Kohler, DiClemente, & Wang, 1999). In these cases, change scores were reverse-scored to maintain a metric in which higher numbers indicated increases in protection from HIV.
Analytic Strategy
We calculated weighted mean effect sizes to examine change over time in treatment and control study groups and performed corrections for sample-size bias to estimate d. Statistics d are Becker's g (Mposttest – Mpretest/SDpre) adjusted for sample size. We used Hedges and Olkin's (1985) procedures to correct effects for their sample size and to calculate weighted mean effect sizes, d, and homogeneity statistics, QB, which test the hypothesis that the variance of the population effect size is no greater than what would be expected due to random error. QB is obtained from the sums of squares of an analysis of variance (ANOVA) and is a homogeneity index analogous to an F ratio that allows comparisons for differences between study groups. Calculations of the between-subjects variance followed procedures developed by Hedges and Olkin (1985). When designs were within-subject, we calculated the variance of effect sizes using Morris's (2000) procedures. We performed calculations for within-subject effect sizes using three alternate correlations between pre- and posttest measures (see Albarracín et al., 2003). Thus, we assumed r = .00 and r = .99 as the most extreme values and also imputed correlations from Project RESPECT (see Kamb et al., 1998), which provided moderate values of this association.
Computations of effect sizes were performed using fixed-effects procedures. In this case, one assumes a fixed population effect and estimates its sampling variance, which is an inverse function of the sample size of each group. The inverse of the effect size's variance is used to weight effect sizes prior to obtaining average values. Thus, effect sizes from studies with larger sample sizes are considered more precise and carry more weight than effect sizes obtained from studies with smaller sample sizes. These procedures are powerful and produce narrow confidence intervals (Rosenthal, 1995; Wang & Bushman, 1999).
The data were analyzed with a weighted ANOVA model, using the weighting scheme described above and controlling for other factors that may influence the relation between fear-inducing arguments or HIV counseling and testing and our dependent measures. Only those variables that had significant correlations with fear-inducing arguments and HIV counseling and testing were included in the analyses. Therefore, every analysis also included (a) the duration of the intervention, (b) the time between the end of the intervention and the first posttest, (c) the time between the first posttest and the second posttest (for delayed effects), (d) the presence or absence of informational arguments, (e) the presence or absence of attitudinal arguments, (f) the presence or absence of normative arguments, (g) the presence or absence of behavioral skills arguments, (h) the presence or absence of behavioral skills training, and (i) the presence or absence of condom distribution. These variables were always present in the models we tested in addition to the most critical factors in each focal analysis but are reported in detail elsewhere (see Albarracín et al., 2005).
Results
Samples of Studies and Study Groups
We included 76 reports, which provided 150 independent treatment study groups and 34 independent control study groups. Of the 76 reports, 13 provided a single data set, 39 provided 2 data sets, 11 provided 3 data sets, 8 provided 4 data sets, 2 provided 5 data sets, and 3 provided 6 data sets. In all cases, different data sets included different participants.
Longitudinal Effects of Control Versus Intervention Study Groups
We first examined change in perceived risk, knowledge, and condom use at the two posttests across intervention and control study groups. The weighted means, d, suggest that, in the sample of reports we analyzed, there was more change in knowledge and condom use in intervention than control study groups at both the immediate and delayed posttests. These patterns were confirmed by significant between-groups statistics for these two measures at both points of time (for knowledge at the immediate and delayed follow-ups: QBs(1) = 122.47 and 126.64, p < .001, respectively; for condom use at the immediate and delayed follow-ups: QBs(1) = 98.31 and 174.28, p < .001, respectively), as well as significant change relative to a zero standard for both measures in intervention conditions; for knowledge at the immediate and delayed follow-ups: 95% CI = 0.41, 0.46 and 0.45, 0.50, respectively; for condom use at the immediate and delayed follow-ups: 95% CI = 0.32, 0.36 and 0.35, 0.39, respectively.
Change in perceived risk, however, did not vary across intervention and control study groups. The mean change for perceived risk in interventions was 0.02 for the immediate posttest and – 0.07 for the delayed posttest. Neither of these indexes differed significantly from control study groups or from a zero standard representing stability; QB(1) < 1.10 in all cases.
Test of Hypotheses About Fear-Inducing Arguments and HIV Counseling and Testing at the Immediate and Delayed Follow-Ups
To examine the independent effects of fear-inducing arguments and HIV counseling and testing, we studied the effect sizes representing change as a function of (a) the presence or absence of fear-inducing arguments and (b) the presence or absence of HIV counseling and testing. Supplementary analyses considered the role of behavioral recommendations and intervention-content complexity in general and for a particular audience.
Effect of fear-inducing arguments on knowledge, perceived risk, and behavior
Fear-inducing arguments could promote or hinder the effectiveness of interventions to increase HIV-relevant knowledge and condom use because of the associated increases in perceived risk. Therefore, we first verified whether presenting fear-inducing arguments actually increased perceptions of personal risk of contracting HIV relative to not presenting these arguments. Consistent with the objectives underlying the use of fear inducements, the presence of fear-inducing arguments increased perceptions of risk at both posttests (see Table 1).
Table 1.
Adjusted Mean Change in Perceived Risk, Knowledge, and Behavior as a Function of Fear Inducement and HIV Counseling and Testing
| Immediate follow-up |
Delayed follow-up |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention strategy and change dimension | Presence | Absence | Difference | QB(1) | Presence | Absence | Difference | QB(1) | Comparison F |
| Fear-inducing arguments | |||||||||
| Perceived risk | 0.27 | −0.20 | 0.47 | 5.27* | 0.07 | −0.33 | 0.40 | 0.31 | 4.96** |
| Knowledge | 0.42 | 0.67 | −0.25 | 16.68*** | 0.43 | 0.59 | −0.16 | 6.87** | 9.81*** |
| Behavior | 0.08 | 0.51 | −0.43 | 57.79*** | 0.04 | 0.77 | −0.73 | 112.77*** | 54.98*** |
| HIV counseling and testing | |||||||||
| Perceived risk | −2.22 | 0.18 | −2.40 | 730.13*** | −2.65 | 0.00 | −2.65 | 202.53*** | 527.60*** |
| Knowledge | 0.61 | 0.49 | 0.12 | 35.17*** | 0.72 | 0.52 | 0.20 | 27.68*** | 7.49*** |
| Behavior | 0.66 | 0.13 | 0.53 | 173.06*** | 0.71 | 0.12 | 0.59 | 219.06*** | 46.00*** |
Note. d = weighted mean difference; QB = between-categories homogeneity index with number of levels of factor – 1 degree of freedom. Differences are differences between the d when the strategy was present versus absent. Significant QBs indicate significant effects of the interventions relative to control study groups. The first QB in the table compared the effect at the time of the immediate follow-up and the second at the time of the delayed follow-up. The comparison F reflects changes in QBs from immediate to delayed follow-up. The weighted means for control study groups at immediate follow-up were perceived risk d = 0.01, knowledge d = 0.08, and condom use d = 0.04. The weighted means for control study groups at delayed follow-up were perceived risk d = −0.07, knowledge d = 0.11, and condom use d = −0.03.
p < .05.
p < .01.
p < .001.
The next step was to determine whether the presence of fear-inducing arguments led to smaller or larger changes in knowledge and condom use than its absence. Supporting the negative linear hypothesis, the presence of fear-inducing arguments was associated with lesser increases in knowledge and condom use than the absence of fear-inducing arguments (i.e., for knowledge, d = 0.42 vs. 0.67 and d = 0.43 vs. 0.59 for the immediate and delayed follow-ups, respectively; for condom use, d = 0.08 vs. 0.51 and d = 0.04 vs. 0.77 for the immediate and delayed follow-ups, respectively; see Figure 1). In combination, these findings may imply that, at the time participants received the intervention, they were too preoccupied with their own fear of contracting HIV or other STIs to properly process the health information and recommendations.
Figure 1.
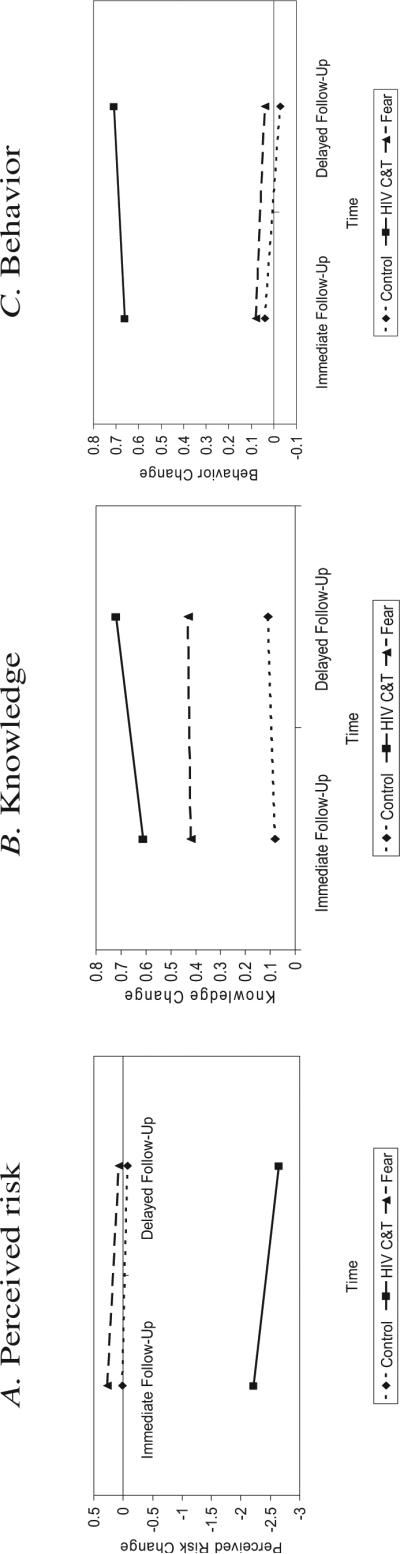
Change in perceived risk, knowledge, and condom use at the first and second posttests for control study groups, HIV counseling and testing (HIV&T), and fear-inducing arguments.
Support for the hypothesis of a reverse association between fear and behavior change, however, does not rule out the curvilinear and moderated hypotheses. Therefore, we first tested the possibility that increases of fear might be beneficial up to one point but detrimental after that. These analyses were conduced in two ways. First, we summed the presence or absence of three types of fear-inducing arguments (each dummy coded), creating a score that varied from 0 to 3. Second, we weighted the sum of the three fear-inducing arguments by the duration of the intervention (in minutes), with the rationale that longer, more intense interventions that include fear inducements might instill higher perceptions of risk than shorter, less intense ones.
The interventions we summarized had zero, one, two, or three fear-inducing arguments, thus mapping well onto a three-level distribution of fear. Yet, the level of behavior change associated with these three levels of fear did not follow the inverted-U pattern predicted by McGuire's (1968) model. Instead, behavior change was greater when the level of fear was none or low rather than moderate or high, QB(2) = 119.14, p < .001, at the immediate follow-up and QB(2) = 167.80, p < .001, at the delayed follow-up, with no difference verified between the moderate- and high-fear conditions, QB(1) = 0.36, ns, at the immediate follow-up and QB(1) = 0.43, ns, at the delayed follow-up. Contrary to the inverted-U hypothesis, even when the presence or absence of fear-inducing arguments was weighted by the length of the intervention in minutes, there was no consistent association between the intensity of the fear and behavior change, either when we fit a linear or a quadratic model regressing behavior change on the time-weighted arguments variable.
Finally, we examined two interactions that can shed light on the moderated hypothesis. First, because fear-inducing arguments may promote knowledge and behavior change only in the presence of a behavioral recommendation (see, e.g., Hovland et al., 1953), we assessed whether presenting fear-inducing arguments and risk-reduction recommendations together was linked to increased perceived risk, knowledge, and condom use. We used two indexes of presence of behavioral recommendations. First, treatments that had an explicit statement that one should use condoms to prevent HIV were classified as including a behavioral recommendation, whereas those that did not have this statement were not. In addition, because the behavioral recommendation must be feasible and because behavioral skills training presumably facilitates performance of the recommendation, we categorized the use of behavioral skills strategies as presence of a behavioral recommendation. Thus, the examination of this question involved 12 analyses of change, including 1 for each of the three dependent measures of interest (perceived risk, knowledge, and condom use) as a function of presence versus absence of fear inducements, each of the two indexes of presence of behavior recommendation, the interaction between the presence of fear and each index of presence of behavior recommendations, and the two follow-up measures. Although the interaction between the presence of fear and behavioral recommendations on condom use was significant in all cases, the direction of the findings reflected in this interaction did not support this hypothesis. In fact, the presence of a recommendation without fear was more successful than its presentation with fear (recommendation index I: for knowledge, d = 0.45 vs. 0.40 and d = 0.50 vs. 0.06 for the immediate and delayed follow-ups, respectively; for condom use, d = 1.22 vs. 0.08 and d = 1.23 vs. 0.06 for the immediate and delayed follow-ups, respectively; recommendation index II: for knowledge, d = 0.60 vs. 0.49 and d = 0.64 vs. 0.47 for the immediate and delayed follow-ups, respectively; for condom use, d = 0.92 vs. 0.08 and d = 0.90 vs. 0.08 for the immediate and delayed follow-ups, respectively).
The second interaction that bears on the moderated effects of fear takes into account the complexity involved in understanding the content of the intervention. To test this prediction, we examined the interaction between fear-inducing arguments and the education level of the target population. The results of these analyses revealed no significant interaction between education and fear-inducing arguments, lending even more credence to the possibility that greater cognitive ability of the audience did not alter the negative effects of fear inducements.
Effect of HIV counseling and testing on knowledge, perceived risk, and behavior
We hypothesized that the resolution of fear that is associated with a negative HIV test would effectively trigger knowledge and behavior change. Supporting this hypothesis, the presence of HIV counseling and testing was associated with significant increases in both knowledge and condom use (Table 1). Also as expected, these increases were accompanied by decreases in perceived risk, a finding that renders support for our fear-resolution hypothesis.
Moderating Effects of HIV Incidence as a Marker of the Intensity of HIV-Related Fear
One potential explanation for the divergent effects of fear-inducing arguments and HIV counseling and testing is disparate emotional effects. Therefore, one way of validating this assumption is to analyze the effects of the HIV rates in a given population in combination with the effects of fear-inducing arguments and HIV counseling and testing. For instance, fear-inducing arguments may induce greater fear among populations with higher rather than lower seropositivity because populations with higher rates of HIV are more likely to know people who are infected with HIV and, thus, to be sensitive to fear appeals. For the same reasons, HIV counseling and testing may offer greater emotional relief for populations with higher seropositivity baselines if (and only if) the sample has lower infection than expected on the basis of the population rates. To test these possibilities, we analyzed the effects of population and study group sample HIV rates and either fear-inducing arguments or HIV counseling and testing on behavior change.
The analysis of HIV rates and fear-inducing arguments consisted of examining behavior change as a function of the presence or absence of fear-inducing arguments, the population's HIV rate, and the interaction between the two. These analyses revealed significant interactions between fear-inducing arguments and infection rate at both the immediate (QB(1) = 9.08, p < .001) and delayed (QB(1) = 14.42, p < .001) follow-ups. As reported above, the presence of fear-inducing arguments resulted in smaller changes in behavior than the absence of fear-inducing arguments. However, this effect was stronger when the population HIV infection rate was higher than when it was lower; for immediate follow-up, QB(1) = 53.00, p < .001; for delayed follow-up, QB(1) = 71.76, p < .001.
For the analyses of the effects of HIV counseling and testing, we subtracted the baseline sample infection rate from the population rate, thus producing a continuous variable for which more positive numbers indicate higher infection rates in the population relative to the study group sample and, presumably, greater emotional relief in the study group sample. As expected, the interaction between the difference scores for HIV rates and the use of HIV counseling and testing sessions was significant; for the immediate follow-up, QB(1) = 12.41, p < .001; for the longitudinal follow-up, QB(1) = 31.68, p < .001. The pattern of means underlying this interaction was not exactly as expected, but it was nonetheless not inconsistent with our predictions. Following HIV counseling and testing sessions, bigger discrepancies between the sample and the population HIV infection rates, both positively and negatively, were associated with greater behavior change than were smaller discrepancies. That is, there was more behavior change when the sample rate was larger or smaller than the population rate than when they were equal; comparing the lowest level versus the moderate levels: for immediate follow-up, QB(1) = 43.00, p < .001, and for delayed follow-up, QB(1) = 19.54, p < .001; comparing the highest level versus the moderate levels: for immediate follow-up, QB(1) = 4.47, p < .05, and for delayed follow-up, QB(1) = 24.90, p < .001. In addition, however, greater positive discrepancies produced the most behavior change compared with all other levels of discrepancy; for immediate follow-up, QB(1) > 30.83, p < .001, and for delayed follow-up, QB(1) > 49.34, p < .001.
Decay and Spiral Effects in the Longitudinal Effectiveness of Fear-Inducing Arguments and HIV Counseling and Testing
Because we had hypotheses about potential increases and decreases in intervention effectiveness over time, we were interested in comparing the amount of change in perceived risk, knowledge, and condom use observed at each time. With this objective, we subtracted the QB at the delayed follow-up from the QB at the immediate follow-up in Table 1, thus creating differences that are distributed as an F ratio with 1 degree of freedom. As can be seen, there were significant differences for the effect of fear-inducing arguments on knowledge, perceived risk, and condom use at the time of the delayed follow-up relative to the time of the immediate follow-up. It is interesting that, as expected, the effect of HIV counseling and testing on condom use increased from the immediate to the delayed follow-up, whereas the effect of fear-inducing arguments decreased between these points in time. Also, the presence of HIV counseling and testing increased knowledge from the immediate to the delayed follow-up but decreased perceptions of risk across the same time span.
Discussion
To the best of our knowledge, this is the first meta-analysis to examine the influence of HIV-prevention interventions by looking at more than one follow-up, thus shedding light on the long-term outcomes of fear inducements and HIV counseling and testing. In addition, this research synthesis provides evidence concerning the nature of longitudinal changes following the immediate impact of an intervention in general. This objective was not accomplished by any prior synthesis of behavior-change interventions.
This Meta-Analysis in the Context of Prior Research on Long-Term Behavioral and Cognitive Change
We predicted and found support for different longitudinal patterns for perceived risk (an emotion) and condom use (a behavior). First, in every analysis we conducted comparing the effects of fear-inducing arguments over time, initial changes in risk perceptions decayed as time elapsed. This finding is clearly in line with earlier predictions about a rapid decay of the experience of emotions over time (Clore & Schnall, 2005). Although the effects of fear inducements on risk perceptions decayed, the corresponding decreases in behavior strengthened over time. Thus, increasing perceptions of risk resulted in even less condom use at the delayed than at the immediate follow-up, indicating that this lack of behavioral success can have serious long-term consequences.
HIV counseling and testing, which was associated with initial increases in condom use but decreases in perceived risk, showed similar changes in these patterns. That is, the initial decreases in risk perceptions faded, but condom use spiraled over time. Thus, this meta-analysis provides evidence that longer times provide an opportunity for people to reflect on their behavior. Longer times may also provide opportunities for the environment to reinforce the behavior elicited by an intervention (see Albarracín & McNatt, 2005; Baum, 1994). In this regard, our results are encouraging in that the ultimate goal of permanently changing behavior may be possible.
This Meta-Analysis in the Context of Prior Research on the Impact of Fear-Inducing Arguments
Past theories about the effect of fear-inducing arguments have predicted one of four possible relations: (a) a positive linear relation, with high-fear inducements being more persuasive than low-fear inducements; (b) a negative linear relation, with low-fear inducements being more persuasive than high-fear inducements; (c) a curvilinear relation, with moderate-fear inducements being more persuasive than either high- or low-fear inducements; and (d) a moderated relation, with the inclusion of a behavioral recommendation or the comprehensibility of the intervention content affecting the shape of the association between fear inducements and behavior change. Of these hypotheses, only a negative linear relation received support, revealing no single situation in which fear-inducing arguments were associated with behavior or knowledge increases.
An important theoretical development has been the suggestion that the fear inducements presented in a communication might be effective for some behaviors but not for others (Rothman & Salovey, 1997). For instance, interventions that focus on the possible benefits of engaging in a behavior (i.e., a gain frame) may be best when the natural tendency of the target behavior consists of performing an action rather than detecting a risk. In the case of condom use, a gain frame might discuss the benefits of condom use, such as maintaining a healthy lifestyle, whereas a loss frame might discuss the risks of having unprotected sex, such as disease acquisition or pregnancy. To the extent that the behavior we studied— condom use—is proactive, the failure of fear inducements to boost behavior change might be seen as providing partial support for Rothman and Salovey's (1997) hypothesis.
Implications for Practice
The results of this meta-analysis have several implications for the design of future health-promotion interventions. First, it is fortunate that an effective HIV-prevention intervention can promote increases in HIV-relevant knowledge and condom use. However, it is even more reassuring that the positive behavioral effects of an intervention can spiral over time, with behavior change strengthening beyond the immediate follow-up. This spiraling suggests that marginal effects at the time of the immediate follow-up may nonetheless be worthwhile in the longer term. Although a common observation from intervention research is that changes following a preventive intervention can decay after about 3 to 6 months, when an effective strategy is implemented, it is possible that this barrier can be overcome.
By the same token, our results highlight the possibility that the impact of ineffective intervention strategies may also get stronger (more negative) over time. To this extent, it is imperative that researchers use strategies that promote some positive changes immediately following the intervention. On the basis of the results of this meta-analysis, the effects of interventions associated with decreased condom use at the first follow-up may worsen. Hence, additional strategies may be necessary to prevent future deterioration as soon as negative effects are detected.
From a practical standpoint, in our meta-analysis, the effects of fear inducements and HIV counseling and testing were strongest for populations with high HIV seropositivity. This finding is contrary to the impression that study groups from these populations change less than others (see, e.g., Albarracín et al., 2005). In fact, in the high seropositive populations, behavior change we analyzed was weaker in response to fear-inducing arguments but stronger in response to HIV counseling and testing. Arguably, then, high-risk populations can change more than lower risk populations when one can provide closure for HIV-related anxiety.
Final Note
As our meta-analysis clearly shows, inducing fear is not an effective way to promote HIV-relevant learning or condom use either immediately following the intervention or later on. Although this conclusion may be disappointing given the widespread use of fear in HIV prevention, we are optimistic that the effects of resolving fear instead of inducing it may be beneficial in creating and maintaining healthy behaviors in an attempt to halt the spread of HIV/AIDS. In addition, our meta-analysis yielded the promising result that the effects of campaigns on behavior can sometimes spiral, contrary to the assumption that the best results are observed immediately after the intervention is implemented.
Acknowledgments
Earlier versions of some of the analyses described here were presented as a thesis by Allison Earl conducted under the direction of Dolores Albarracín. The research was supported by Grant K01-MH01861 from the National Institute of Mental Health and facilitated by Grants R03-MH58073 and R01-NR08325 from the National Institutes of Health. We thank Ece Kumkale, Cynthia Klein, Penny S. McNatt, Amy L. Mitchell, and G. Tarcan Kumkale for their invaluable assistance organizing this project. We also thank Matthew Lindberg and the project assistants during the years 1997−2004 and Barry R. Schlenker and Jesse Dallery for detailed comments on an earlier version of this article.
Footnotes
A complete list of all papers included in the meta-analysis, as well as additional tables and figures, are available at www.psych.ufl.edu/earl
Alternatively, a “gain,” or nonfear-arousing message may be more appropriate to stimulate people to engage in a proactive behavior rather than avoid a risk. However, our meta-analysis could not test this particular moderating hypothesis.
For a detailed description of the review and selection process, see Albarracín et al. (2005).
One-hundred thirteen reports were excluded because they did not include a condom use component, 112 were review or theoretical papers, 104 were survey papers, and 75 did not include a standardized intervention. An additional 74 reports were excluded because they did not include a pretest; 128 papers included only an immediate follow-up. Finally, 131 papers either presented qualitative data or lacked usable statistics from which to calculate effect sizes.
Although we would have liked to weight the inducements by the actual amount of time devoted to increasing fear throughout the intervention, most papers reported only overall intervention duration without a breakdown of time devoted to each strategy. As such, we used the overall duration of the study as a proxy for the percentage of time devoted to fear-inducing arguments. Although some interventions may focus more on other strategies, such as negotiation skills or social support, during this extra time, overall intervention duration may still be a viable proxy for the duration of fear-inducing arguments. Specifically, there were no systematic differences in duration across levels of fear inducements. Thus, it appeared that the strategy was reasonable, F = 0.28, p = .84.
However, because not all counseling sessions include fear-inducing arguments, multivariate analyses allowed us to separate the effects of the two types of strategies. This information was coded from the text of the reports included in the meta-analysis using the above-mentioned criteria. Of the 184 cases included in the meta-analysis, 11 contained both fear-inducing arguments and HIV counseling and testing, 60 included only fear-inducing arguments without HIV counseling and testing, 18 included only HIV counseling and testing without fear-inducing arguments, and 95 contained neither fear-inducing arguments nor HIV counseling and testing.
For the analyses of fear-inducing arguments, no study group infection rates were reported nor can one assume that participants know their serostatus. As a result, we used only the population rates in these analyses.
References
- Albarracín D. Unrealistic expectations: The ironic effects of expectancy disconfirmation in persuasion. In: Chadee D, Young JR, editors. Current themes and perspectives in social psychology. University of the West Indies Press; Trinidad: (in press) [Google Scholar]
- Albarracín D, Gillette J, Earl AN, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychological Bulletin. 2005;131:856–897. doi: 10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Kumkale GT, Johnson BT. Influences of social power and normative support on condom use decisions: A research synthesis. AIDS Care. 2004;16:700–723. doi: 10.1080/09540120412331269558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, McNatt PS. Maintenance and decay of the influences of past behavior: Anchoring attitudes on beliefs following inconsistent actions. Personality and Social Psychology Bulletin. 2005;31:719–733. doi: 10.1177/0146167204272180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, McNatt PS, Findley-Klein C, Ho R, Mitchell A, Kumkale GT. Persuasive communications to change actions: An analysis of behavioral and cognitive impact in HIV prevention. Health Psychology. 2003;22:166–177. doi: 10.1037//0278-6133.22.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Wyer RS. Elaborative and nonelaborative processing of a behavior-related communication. Personality and Social Psychology Bulletin. 2001;27:691–705. [Google Scholar]
- Allen S, Serufilira A, Bogaerts J, Van de Perre P, Nsengumuremyi F, Lindan C, et al. Confidential HIV testing and condom promotion in Africa. Journal of the American Medical Association. 1992;268:3338–3343. [PubMed] [Google Scholar]
- Baum WM. Understanding behaviorism: Science, behavior and culture. Allyn & Bacon; Boston: 1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker BJ. Synthesizing standardized mean-change measures. British Journal of Mathematical and Statistical Psychology. 1988;41:257–278. [Google Scholar]
- Bem DJ. An experimental analysis of self-persuasion. Journal of Experimental Social Psychology. 1965;1:199–218. [Google Scholar]
- Bem DJ. Self-perception theory. In: Berkowitz L, editor. Advances in experimental social psychology. Vol. 6. Academic Press; San Diego, CA: 1972. pp. 1–62. [Google Scholar]
- Brown LK, Reynolds LA, Lourie KJ. A pilot HIV prevention program for adolescents in a psychiatric hospital. Psychiatric Services. 1997;48:531–533. doi: 10.1176/ps.48.4.531. [DOI] [PubMed] [Google Scholar]
- Carey MP, Maisto SA, Kalichman SC, Forsyth AD, Wright EM, Johnson BT. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. Journal of Consulting and Clinical Psychology. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll P, Dockery K, Shepperd JA. Fluctuations in future outlooks. Review of General Psychology. (in press) [Google Scholar]
- Centers for Diseases Control and Prevention . Documentation for the brief street intercept and coffee shop interview questionnaires. Community Demonstration Projects Research Group; Atlanta, GA: 1993. [Google Scholar]
- Centers for Disease Control and Prevention . HIV counseling and testing in publicly funded sites annual report 1997 and 1998. Author; Atlanta, GA: 2001a. [Google Scholar]
- Centers for Disease Control and Prevention Revised guidelines for HIV counseling, testing, and referral. MMWR, Recommendations and Reports. 2001b;50(RR19):1–58. [PubMed] [Google Scholar]
- Clore GL, Schnall S. The influence of affect on attitude. In: Albarracín D, Johnson BT, Zanna MP, editors. Handbook of attitudes and attitude change. Erlbaum; Mahwah, NJ: 2005. pp. 437–489. [Google Scholar]
- Collins C, Kohler C, DiClemente R, Wang MQ. Evaluation of the exposure effects of a theory-based street outreach HIV intervention on African-American drug users. Evaluation and Program Planning. 1999;22:279–293. doi: 10.1016/s0149-7189(99)00018-x. [DOI] [PubMed] [Google Scholar]
- Durantini MR, Albarracín D, Mitchell AL, Earl AN, Gillette JC. Conceptualizing the influence of social agents of behavior change: A meta-analysis of the effectiveness of HIV-prevention interventionists for different groups. Psychological Bulletin. 2006;132:212–248. doi: 10.1037/0033-2909.132.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eppright DR, Hunt JB, Tanner JF, Jr., Franke GR. Fear, coping, and information: A pilot study on motivating a healthy response. Health Marketing Quarterly. 2002;20:51–73. doi: 10.1300/J026v20n01_05. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information–motivation– behavioral skills model-based HIV risk behavior change information for inner-city high school youth. Health Psychology. 2002;21:177–186. [PubMed] [Google Scholar]
- Hedges LV, Olkin I. Statistical methods for meta-analysis. Academic Press; Orlando, FL: 1985. [Google Scholar]
- Hovland CI, Janis IL, Kelley HH. Communication and persuasion: Psychological studies of opinion change. Yale University Press; New Haven, CT: 1953. [Google Scholar]
- Hull CL. Principles of behavior: An introduction to behavior therapy. Appleton-Century-Crofts; New York: 1943. [Google Scholar]
- Isen AM. Positive affect, cognitive processes, and social behavior. In: Berkowitz L, editor. Advances in experimental social psychology. Vol. 20. Academic Press; San Diego, CA: 1987. pp. 203–253. [Google Scholar]
- Janis IL, Feshbach S. Effects of fear-arousing communications. Journal of Abnormal and Social Psychology. 1953;48:78–92. doi: 10.1037/h0060732. [DOI] [PubMed] [Google Scholar]
- Johnson BT. DSTAT 1.10: Software for the meta-analytic review of research literatures. Erlbaum; Hillsdale, NJ: 1993. [Google Scholar]
- Johnson BT, Carey MP, Marsh KL, Levin KD, Scott-Sheldon LA. Interventions to reduce sexual risk for the human immunodeficiency virus in adolescents, 1985−2000: A research synthesis. Archives of Pediatrics & Adolescent Medicine. 2003;157:381–388. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- Johnson WD, Hedges LV, Ramirez G, Semann S, Norman LR, Sogolow E, et al. HIV prevention research for men who have sex with men: A systematic review and meta-analysis. Journal of Acquired Immune Deficiency Syndrome. 2002;30:18–29. [PubMed] [Google Scholar]
- Kamb ML, Fishbein M, Douglas JM, Jr., Rhodes F, Rogers J, Bolan G, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: A randomized controlled trial. Project RESPECT Study Group. Journal of the American Medical Association. 1998;280:1161–1167. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- Kelly JA. Changing HIV risk behavior: Practical strategies. Guilford Press; New York: 1995. [Google Scholar]
- Kelly JA, St. Lawrence JS, Hood HV, Brasfield TL. Behavioral intervention to reduce AIDS risk activities. Journal of Consulting and Clinical Psychology. 1989;57:60–67. doi: 10.1037//0022-006x.57.1.60. [DOI] [PubMed] [Google Scholar]
- Kelly JA, St. Lawrence JS, Stevenson LY, Hauth AC, Kali-chman SC, Diaz YE, et al. Community AIDS/HIV risk reduction: The effects of endorsements by popular people in three cities. American Journal of Public Health. 1992;82:1483–1489. doi: 10.2105/ajph.82.11.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumkale GT, Albarracín D. The sleeper effect in persuasion: A meta-analysis. Psychological Bulletin. 2004;130:143–172. doi: 10.1037/0033-2909.130.1.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal H. Findings and theory in the study of fear communication. In: Berkowitz L, editor. Advances in experimental social psychology. Vol. 5. Academic Press; New York: 1970. pp. 119–186. [Google Scholar]
- McGuire WJ. Personality and susceptibility to social influence. In: Borgatta EF, Lamber WW, editors. Handbook of personality theory and research. Rand McNally; Chicago: 1968. pp. 1130–1187. [Google Scholar]
- McGuire WJ. Attitude change: The information-processing paradigm. In: McClintock CG, editor. Experimental social psychology. Holt, Rinehart & Winston; New York: 1972. pp. 108–141. [Google Scholar]
- Miller NE, Dollard J. Social learning and imitation. Yale University Press; New Haven, CT: 1941. [Google Scholar]
- Morris SB. Distribution of the standardized mean change effect size for meta-analysis on repeated measures. British Journal of Mathematical and Statistical Psychology. 2000;53:17–29. doi: 10.1348/000711000159150. [DOI] [PubMed] [Google Scholar]
- O'Leary A, Jemmott LS, Goodhart F, Gebelt J. Effects of an institutional AIDS prevention intervention: Moderation by gender. AIDS Education and Prevention. 1996;8:516–528. [PubMed] [Google Scholar]
- Ouellette JA, Wood W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychological Bulletin. 1998;124:54–74. [Google Scholar]
- Ploem C, Byers ES. The effects of two AIDS risk-reduction interventions on heterosexual college women's AIDS-related knowledge, attitudes and condom use. Journal of Psychology & Human Sexuality. 1997;9:1–24. doi: 10.1300/j056v09n01_01. [DOI] [PubMed] [Google Scholar]
- Rigby K, Brown M, Anagnostou P, Ross MW, Rosser BRS. Shock tactics to counter AIDS: The Australian experience. Psychology and Health. 1989;3:145–159. [Google Scholar]
- Rosenthal R. Writing meta-analytic reviews. Psychological Bulletin. 1995;118:183–192. [Google Scholar]
- Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: The role of message framing. Psychological Bulletin. 1997;121:3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- Shepperd JA, McNulty JK. The affective consequences of expected and unexpected outcomes. Psychological Science. 2002;13:85–88. doi: 10.1111/1467-9280.00416. [DOI] [PubMed] [Google Scholar]
- UNAIDS, UNICEF, & World Health Organization Rwanda: Epidemiological fact sheets on HIV/AIDS and sexually transmitted infections. 2004a Retrieved February 2005 from http://www.unaids.org/html/pub/publications/fact-sheets01/rwanda_en_pdf.htm.
- UNAIDS, UNICEF, & World Health Organization United States of America: Epidemiological fact sheets on HIV/AIDS and sexually transmitted infections. 2004b Retrieved February 2005 from http://www.unaids.org/html/pub/publications/fact-sheets01/usa_en_pdf.htm.
- UNAIDS, UNICEF, & World Health Organization Zambia: Epidemiological fact sheets on HIV/AIDS and sexually transmitted infections. 2004c Retrieved February 2005 from http://www.unaids.org/html/pub/publications/fact-sheets01/zambia_en_pdf.htm.
- Wang MC, Bushman BJ. Integrating results through meta-analytic review using SAS software. SAS Institute; Cary, NC: 1999. [Google Scholar]
- Weinhardt LS, Carey MP, Johnson BT, Bickham NL. Effects of HIV counseling and testing on sexual risk behavior: A meta-analytic review of published research, 1985−1997. American Journal of Public Health. 1999;89:1397–1405. doi: 10.2105/ajph.89.9.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J, Mark G, Mathews A, MacLeod C. The emotional Stroop task and psychopathology. Psychological Bulletin. 1996;120:3–24. doi: 10.1037/0033-2909.120.1.3. [DOI] [PubMed] [Google Scholar]


