Abstract
Genomic studies of cannabis use disorders have been limited. The cannabinoid receptor 1 gene (CNR1) on chromosome 6q14–15 is an excellent candidate gene for cannabis dependence due to the important role of the G-protein coupled receptor encoded by this gene in the rewarding effects of Δ9-tetrahydrocannabinol. Previous studies have found equivocal evidence for an association between SNPs in CNR1 and a general vulnerability to substance use disorders. We investigate the association between 9 SNPs spanning CNR1 and cannabis dependence in 1,923 individuals. Two SNPs that were previously associated with cannabis dependence in other studies were also significant with this phenotype in our analyses [rs806368 (p = 0.05) and rs806380 (p = 0.009)]. Haplotype analyses revealed the association to be largely driven by the SNP rs806380. These results suggest a role for the cannabinoid receptor 1 gene in cannabis dependence.
Keywords: CNR1, cannabis dependence, COGA, pedigree disequilibrium test, association
Between 1992 and 2002, cannabis use disorders increased by 18% in the United States (Compton et al. 2004). The treatment episode data sets reveal that 289,532 (about 15%) of all admissions to chemical dependency treatment facilities in the United States were cannabis-related (Treatment Episode Data Set (TEDS) 2003). Additionally, cannabis use disorders are associated with the comorbid occurrence of alcohol dependence (Stinson et al. 2006), other drug dependence (Agrawal et al. 2007) and psychopathology (Grant 1995; Copeland 2006; Compton et al. 2005).
Family (Bierut et al. 1998; Merikangas et al. 1998) and twin studies (Kendler and Prescott 1998; Tsuang et al. 2001; Agrawal and Lynskey 2006) have demonstrated that genetic influences play an important role in shaping liability to cannabis dependence. Despite this, efforts to identify the genes that might contribute to this genetic liability have been limited. The cannabinoid receptor 1 gene (CNR1) on chromosome 6q14–15 encodes a G-protein coupled receptor for Δ9-tetrahydrocannabinol, and therefore is an excellent candidate gene for affecting susceptibility to cannabis dependence. The endogenous cannabinoid system is thought to regulate dopamine reward circuits that are believed to play an important role in reward processes involved in addiction (Mechoulam et al., 1994; Onaivi et al., 2002; Zhang et al., 2004). The G-protein coupled receptor encoded by CNR1 is negatively coupled to adenylate cyclase, thus inhibiting cyclic AMP production. Further supporting the role of CNR1 in substance dependence is Rimonabant (SR141716A), a cannabinoid receptor 1 antagonist, that is being investigated for its potential role in alcohol, nicotine and drug dependence (Benyamina et al. 2008; Nides 2008; Jagerovic et al. 2008; Gelfand and Cannon 2006; Cahill and Ussher 2007).
A recent linkage study identified the region on chromosome 6 in which this gene lies as linked with cannabis dependence (Agrawal et al. 2008b). Previous studies have also reported evidence for the association between single nucleotide polymorphisms (SNPs) in CNR1 and a general vulnerability to substance use disorders. Zhang et al. (2004) tested for an association between 19 SNPs and the risk for polysubstance use disorders in European and African-American populations and found that three SNPs (rs806379-rs1535255-rs2023239) provided evidence of association when analyzed singly or as a haplotype (T-A-G haplotype). More recently, Hopfer and colleagues (2006) found that a SNP (rs806380 – intron 2) proximal to the TAG haplotype was associated with the development of cannabis dependence symptoms (protective effect of G-allele) and that certain haplotypes (rs6454674-rs806380-rs806377-rs1049353) were associated with the development of fewer cannabis dependence problems while others were associated with an increased risk for cannabis dependence. More recently, SNPs in CNR1, especially rs6454674 and rs806368, were found to be associated with alcohol and illicit drug dependence in European Americans (Zuo et al. 2007). Two recent studies also allude to the effects of SNPs in CNR1 on nicotine dependence and alcohol-related behaviors (Kendler et al., 2008; Hutchison et al., 2008). In contrast, the case control study of Herman et al. (2006) failed to find an association between cannabis, cocaine, opioid or polysubstance dependence and SNPs in CNR1. Negative association results have previously been reported by others (Li et al. 2000; Heller et al. 2001; Covault et al. 2001).
High levels of cannabis dependence have been reported in samples ascertained for alcohol dependence, including the Collaborative Study on the Genetics of Alcoholism (COGA) (Agrawal et al. 2008a). Using a family based test of association, we tested the hypothesis that SNPs in CNR1 are associated with cannabis dependence in this sample.
Data collection occurred at six centers across the United States (Begleiter et al. 1995) and was approved by the institutional review boards of all participating centers. Probands were identified from alcohol treatment clinics. A subset of families with alcohol dependent probands as well as at least two first-degree relatives meeting criteria for both DSM-III-R alcohol dependence and Feighner criteria for definite alcoholism were selected for genotyping. We analyzed only the 219 families of self-reported European-American ancestry, which included 1,923 genotyped individuals. There were considerable differences between the European American and African American participants in the minor allele frequencies of SNPs in CNR1 (e.g. for rs806368, 20% in EA vs. 8% in AA; for rs1049353, 27% in EA vs. 7% in AA); therefore the African American families were excluded from all analyses.
Informed consent was obtained from all participants prior to the administration of the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA) interview (Hesselbrock et al. 1999; Bucholz et al. 1994). DSM-III-R cannabis dependence (American Psychiatric Association 1994) was coded dichotomously as ‘affected’ if the participant endorsed 3 or more DSM-III-R dependence criteria (with the exclusion of withdrawal) and ‘unaffected’ otherwise. Of the 1,923 genotyped participants (53% female), 379 met criteria for DSM-III-R cannabis dependence, 1,472 were unaffected (1005 of which did not meet criteria for DSM-III-R alcohol dependence) and the remainder (N=72) were missing data. The mean age of the cannabis dependent individuals in COGA was 33.1 [range 18–73] years while the unaffected individuals (neither alcohol nor cannabis dependence) had a mean age of 42.1 [range 18–92] years. Men were considerably more likely to meet criteria for cannabis dependence (30% vs. 12.4%, p < 0.0001) as were those with alcohol dependence (39% vs. 7.3%, p < 0.0001). Of those with cannabis dependence, 79.2% also met criteria for alcohol dependence. We also divided the sample into those aged 18–30 (lower 25%) and those aged 31 and older and computed the correlation between cannabis dependence and alcohol dependence. In the younger and older ‘cohorts’, the correlation between cannabis dependence and alcohol dependence was 0.61 and 0.65 respectively. This argues that there is no significant difference across age in the relationship between these disorders.
Eleven SNPs in CNR1 and in flanking regions were identified from publicly available databases (dbSNP, HapMap) and genotyped using a modified single nucleotide extensions reaction, with allele detection by mass spectometry (Sequenom MassArray system: Sequenom, San Diego, CA). All genotyped SNPs were checked for Mendelian inheritance using PEDCHECK (O'Connell and Weeks 1998). Marker allele frequencies and heterozygosities were computed using USERM13 (Boehnke 1991). One SNP, rs16880261, was monomorphic in this sample, and therefore was excluded from analyses. Tests for Hardy-Weinberg equilibrium, and linkage disequilibrium statistics, were computed in Haploview (Barrett et al. 2005). SNP rs806377 had a significant deviation from Hardy-Weinberg equilibrium and was excluded from further analyses.
To test for the association between single SNPs and haplotypes with DSM-III-R cannabis dependence in the extended, multiplex COGA pedigrees, we used the Pedigree Disequilibrium Test (PDT) (Martin et al. 2001) implemented in pdtphase, part of the genetic analysis package UNPHASED (Dudbridge 2003). SNP physical positions were determined using NCBI build 36.1. For single SNP association analyses, both ‘sum’ and ‘avg’ (average) statistics were computed. The ‘sum’ statistic allows for larger families to have greater weight than smaller families, while the ‘avg’ statistic weighs all families equally in the computation of the test statistic. The ‘sum’ statistic is more powerful when analyzing less prevalent disorders, such as cannabis dependence (Martin et al. 2001). Hence, we only report single SNP and haplotype association results based on the ‘sum’ statistics, which were largely similar to the statistical results obtained from the ‘avg’ option. Haplotypes were constructing using sliding windows of varying width including 2 to 4 consecutive SNPs. Association analysis was carried out using UNPHASED. Rare haplotypes (frequency less than 5%) were excluded from the association analyses. In addition to utilizing the transmission of alleles from heterozygous parent to affected offspring, PDT statistics are also influenced by the transmission of alleles to the affected sibling in discordant sib-pairs.
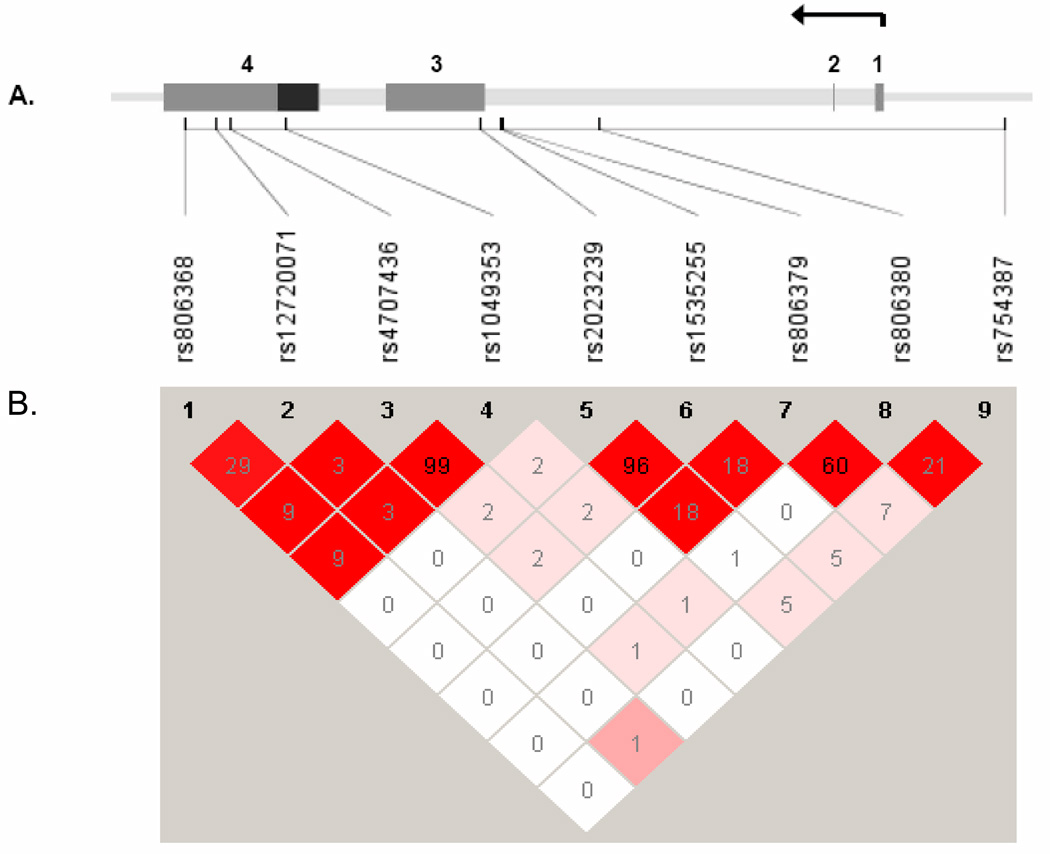
Nine SNPs were analyzed across the 29 kb region of CNR1, extending 4 kb upstream of the gene (Figure 1). D’ across adjacent SNPs was high (except between rs1049353 and rs2023239) while r2 ranged from 0.03 to 0.99. A similar pattern of LD was observed in the HapMap database. To determine whether the SNPs adequately assessed the variation within CNR1, the program Tagger (de Bakker et al., 2005) was used to examine the coverage by the 9 SNPs. Seven of the nine were in the HapMap database. The average r2 of these 7 SNPs with all 30 known HapMap SNPs (MAF ≥ 0.1) in the region was 0.66; r2 was greater than 0.5 for 80% of the SNPs and greater than 0.8 for 40% of the SNPs. Because 2 additional SNPs were genotyped, but were not in the HapMap database, our actual coverage of CNR1 was even better.
Figure 1.
A. The gene structure of CNR1 was based on the annotation of Zhang et al (Molecular Psychiatry, 2004; 9:916–931), and is shown across the top of the figure with SNPs positioned below. Exons are numerically labeled with coding region in black and the untranslated regions in grey. The arrow denotes direction of transcription. B. Pairwise linkage disequilibrium between the genotyped SNPs is numerically represented as r2. The color coding reflects D’ with red reflecting a D’=1. The arrow represents the direction of transcription.
Results of the association analyses are provided in Table 1. SNP rs806380 was significantly associated with cannabis dependence (p=0.009) as was rs806368 (p=0.05), while one SNP, rs806379, was marginally significant (p=0.08). SNP rs806368 was in low LD with rs806379 and rs806380, suggesting independent effects. Because there might be some common genetic risk factors affecting several addictive disorders, we carried out secondary analyses in which we excluded (coded as unknown) from the sample of unaffected subjects those individuals who met criteria for DSM-III-R alcohol dependence. In these secondary analyses, the statistical significance was somewhat reduced (rs806380 p = 0.03) but the pattern of association was consistent.
Table 1.
Association between 9 single nucleotide polymorphisms in the cannabinoid receptor 1 (CNR1) gene and DSM-IIIR cannabis dependence.
| Marker Name | Physical position (bp) | Alleles* | MAF | Z-statistic | PDT-sum pvalue |
|---|---|---|---|---|---|
| rs806368 | 88,906,819 | C/T | 0.20 | 1.923 | 0.05 |
| rs12720071 | 88,907,900 | T/C | 0.08 | 0.759 | 0.45 |
| rs4707436 | 88,908,470 | A/G | 0.27 | 0.130 | 0.9 |
| rs1049353 | 88,910,354 | C/T | 0.27 | 0.130 | 0.9 |
| rs2023239 | 88,917,201 | C/T | 0.15 | 0.381 | 0.7 |
| rs1535255 | 88,917,927 | G/T | 0.15 | 0.591 | 0.55 |
| rs806379 | 88,917,986 | A/T | 0.47 | 1.770 | 0.08 |
| rs806380 | 88,921,372 | A/G | 0.35 | 2.608 | 0.009 |
| rs754387 | 88,935,578 | C/A | 0.28 | 1.136 | 0.26 |
The minor allele appears first (minor/major).
2-SNP sliding window analyses found evidence for over-transmission of the G-C haplotype of rs806380 and rs754387 to unaffected individuals and over-transmission of the A-C haplotype to affected individuals (haplotype p-values 0.005, global p-value 0.004). Since the allele at rs754376 is the same in both haplotypes, we speculate that the association is primarily due to rs806380. No additional information was gained from increasing the window width. We also tested a haplotype formed by rs806368, rs806379 and rs806380. T-A-A was overtransmitted to affecteds (p=0.06) while T-T-G was overtransmitted to unaffecteds (p=0.06).
We demonstrate association between polymorphisms in the CNR1 gene (rs806380, rs806368 and rs754387) and DSM-III-R cannabis dependence. It should be noted that most of the cannabis dependent individuals in this sample were also alcohol dependent. Thus, the comorbid phenotype was the most common. There was no evidence for association of these SNPs with alcohol dependence per se. Our results suggest that variation in CNR1 may contribute to the risk of cannabis dependence. This finding is in keeping with previous studies of CNR1 and its influence on the liability to substance use disorders, however, these findings have been equivocal, with positive (p < 0.0001) (e.g., Zhang et al., 2004) and negative (p = 0.19 – 0.54) (e.g., Herman et al., 2006) results. In addition to consistency across sampling strategies (i.e. both Hopfer et al., 2006 and Zuo et al., 2007 used a case-control design), our results also replicate findings with specific SNPs. In an adolescent/young adult sample Hopfer and colleagues (2006) found that the G allele of rs806380 was overtransmitted to individuals (p=0.034) with no symptoms of DSM-IV cannabis dependence (cases were defined as those with 1+ dependence symptoms). This fits well with our finding that the A allele was more common in cannabis-dependent individuals while the G allele was more common in those not meeting criteria for cannabis dependence. They also report that certain haplotypes (rs6454674, rs806380, rs806377, rs1049353: G-G-C-C) were associated with developing fewer dependence problems and others (T-A-C-C and G-A-C-C) were associated with an increased risk for cannabis dependence. Additionally, rs806368, marginally significant in our study, was found to significantly influence liability to substance dependence via an interaction with rs6454674 in an independent study (Zuo et al., 2007).
Although our data show that rs806380 provided the strongest evidence of association, that does not indicate it is a causative allele. There are 7 known HapMap SNPs in CNR1 with a linkage disequilibrium estimate of r2 ≥ 0.50 with rs806380: six of which were not genotyped and one (rs806379, r2=0.60) which was marginally associated with cannabis dependence in our study.
Some limitations of the current study need to be considered. First, our analyses were restricted to the participants of European American ancestry –this association should be tested in other samples. Second, COGA ascertained densely affected multiplex families, and the genetic underpinnings of cannabis dependence in such a sample may not generalize to the population. Third, it was not possible to test for cannabis dependence exclusive of comorbid alcohol dependence, due to the high density of alcohol dependent individuals in COGA. However, even in a nationally representative survey of U.S. adults (NESARC) (Grant et al., 2003), 69.3% of those with cannabis dependence also met criteria for alcohol dependence, suggesting similar levels of comorbidity in the general population. A fourth limitation is that rs806380, with which we detect significant association, had a Hardy-Weinberg p-value of 0.01; however, there was no evidence for an increased dropout rate (1.6%) and the observed heterozygosity was 0.46, close to the predicted value. Replication studies will, as always, prove invaluable.
In summary, this sample ascertained for alcoholism validates converging evidence from several independent studies suggesting that polymorphisms in CNR1 may be associated with cannabis dependence. The action of these polymorphisms, which so far have not been attributed to any structural or functional effects on cannabis use and misuse, is still unknown. Our findings, in addition to the extant literature, encourage further research into the etiologic contributions of the CNR1 gene to cannabis dependence.
Acknowledgements
The Collaborative Study on the Genetics of Alcoholism (COGA), Co-Principal Investigators B. Porjesz, V. Hesselbrock, H. Edenberg, L. Bierut, includes nine different centers where data collection, analysis, and storage take place. The nine sites and Principal Investigators and Co-Investigators are: University of Connecticut (V. Hesselbrock); Indiana University (H.J. Edenberg, J. Nurnberger Jr., P.M. Conneally, T. Foroud); University of Iowa (S. Kuperman, R. Crowe); SUNY Downstate (B. Porjesz); Washington University in St. Louis (L. Bierut, A. Goate, J. Rice); University of California at San Diego (M. Schuckit); Howard University (R. Taylor); Rutgers University (J. Tischfield); Southwest Foundation (L. Almasy). Zhaoxia Ren serves as the NIAAA Staff Collaborator. This national collaborative study is supported by the NIH Grant U10AA008401 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the National Institute on Drug Abuse (NIDA). Arpana Agrawal is also supported by DA023668.
In memory of Henri Begleiter and Theodore Reich, Principal and Co-Principal Investigators of COGA since its inception; we are indebted to their leadership in the establishment and nurturing of COGA, and acknowledge with great admiration their seminal scientific contributions to the field.
Reference List
- Agrawal A, Lynskey M. The Genetic Epidemiology of Cannabis Use, Abuse and Dependence: A Review. Addiction. 2006;101:801–812. doi: 10.1111/j.1360-0443.2006.01399.x. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Hinrichs A, Dunn G, Bertelsen S, Dick D, Saccone SF, Saccone NL, Grucza R, Wang JC, Cloninger CR, Edenberg H, Foroud T, Hesselbrock V, Kramer J, Bucholz K, Kuperman S, Nurnberger J, Porjesz B, Schuckit M, Goate A, Bierut L. Linkage scan for quantitative traits identifies new regions of interest for substance dependence in the Collaborative Study on the Genetics of Alcoholism (COGA) Sample. Drug Alcohol Depend. 2008a;93:12–20. doi: 10.1016/j.drugalcdep.2007.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Lynskey MT, Madden PA, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2007;102:94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Pergadia ML, Saccone SF, Lynskey MT, Wang JC, Martin NG, Henders A, Campbell M, Garcia R, Broms U, Todd RD, Goate A, Rice J, Kaprio J, Heath AC, Montgomery GW, Madden PA. An Autosomal Linkage Scan for Cannabis Use Disorders in the Nicotine Addiction Genetics Project. Arch Gen Psychiatry. 2008b doi: 10.1001/archpsyc.65.6.713. in press. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- Begleiter H, Reich T, Hesselbrock V, Porjesz B, Li TK, Schuckit M, Edenberg H, Rice JP. The collaborative study on the genetics of alcoholism. Alcohol Health Res World. 1995;19:228–236. [PMC free article] [PubMed] [Google Scholar]
- Benyamina A, Lecacheux M, Blecha L, Reynaud M, Lukasiewcz M. Pharmacotherapy and psychotherapy in cannabis withdrawal and dependence. Expert Rev Neurother. 2008;8:479–491. doi: 10.1586/14737175.8.3.479. [DOI] [PubMed] [Google Scholar]
- Bierut LJ, Dinwiddie SH, Begleiter H, Crowe RR, Hesselbrock V, Nurnberger JI, Jr, Porjesz B, Schuckit MA, Reich T. Familial transmission of substance dependence: alcohol, marijuana, cocaine, and habitual smoking: a report from the Collaborative Study on the Genetics of Alcoholism. Arch Gen Psychiatry. 1998;55:982–988. doi: 10.1001/archpsyc.55.11.982. [DOI] [PubMed] [Google Scholar]
- Boehnke M. Allele frequency estimation from data on relatives. Am J Hum Genet. 1991;48:22–25. [PMC free article] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret RJ, Cloninger RC, Dinwiddie SH, Hesselbrock V, Nurnberger JI, Reich T, Schmidt I, Schuckit MA. A New, Semi-Structured Psychiatric Interview For Use In Genetic Linkage Studies. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Cahill K, Ussher M. Cannabinoid type 1 receptor antagonists (rimonabant) for smoking cessation. Cochrane Database Syst RevCD005353. 2007 doi: 10.1002/14651858.CD005353.pub2. [DOI] [PubMed] [Google Scholar]
- Chen X, Williamson VS, An SS, Hettema JM, Aggen SH, Neale MC, Kendler KS. Cannabinoid receptor 1 gene association with nicotine dependence. Arch Gen Psychiatry. 2008;65:816–824. doi: 10.1001/archpsyc.65.7.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- Copeland J. Cannabis use, depression and public health. Addiction. 2006;101:1380. doi: 10.1111/j.1360-0443.2006.01640.x. [DOI] [PubMed] [Google Scholar]
- Covault J, Gelernter J, Kranzler H. Association study of cannabinoid receptor gene (CNR1) alleles and drug dependence. Mol Psychiatry. 2001;6:501–502. doi: 10.1038/sj.mp.4000925. [DOI] [PubMed] [Google Scholar]
- de Bakker PI, Yelensky R, Pe'er I, Gabriel SB, Daly MJ, Altshuler D. Efficiency and power in genetic association studies. Nat Genet. 2005;37:1217–1223. doi: 10.1038/ng1669. [DOI] [PubMed] [Google Scholar]
- Dudbridge F. Pedigree disequilibrium tests for multilocus haplotypes. Genet Epidemiol. 2003;25:115–121. doi: 10.1002/gepi.10252. [DOI] [PubMed] [Google Scholar]
- Gelfand EV, Cannon CP. Rimonabant: a selective blocker of the cannabinoid CB1 receptors for the management of obesity, smoking cessation and cardiometabolic risk factors. Expert Opin Investig Drugs. 2006;15:307–315. doi: 10.1517/13543784.15.3.307. [DOI] [PubMed] [Google Scholar]
- Grant BF. Comorbidity between DSM-IV drug use disorders and major depression: results of a national survey of adults. J Subst Abuse. 1995;7:481–497. doi: 10.1016/0899-3289(95)90017-9. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan K, Shepard J, Moore T. Source and Accuracy Statement for Wave 1 of the 2001–2002 of the National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- Heller D, Schneider U, Seifert J, Cimander KF, Stuhrmann M. The cannabinoid receptor gene (CNR1) is not affected in German I.V. drug users. Addict Biol. 2001;6:183–187. doi: 10.1080/13556210020040271. [DOI] [PubMed] [Google Scholar]
- Herman AI, Kranzler HR, Cubells JF, Gelernter J, Covault J. Association study of the CNR1 gene exon 3 alternative promoter region polymorphisms and substance dependence. Am J Med Genet B Neuropsychiatr Genet. 2006;141:499–503. doi: 10.1002/ajmg.b.30325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA--a comparison with the SCAN. Addiction. 1999;94:1361–1370. doi: 10.1046/j.1360-0443.1999.94913618.x. [DOI] [PubMed] [Google Scholar]
- Hopfer CJ, Young SE, Purcell S, Crowley TJ, Stallings MC, Corley RP, Rhee SH, Smolen A, Krauter K, Hewitt JK, Ehringer MA. Cannabis receptor haplotype associated with fewer cannabis dependence symptoms in adolescents. Am J Med Genet B Neuropsychiatr Genet. 2006;141:895–901. doi: 10.1002/ajmg.b.30378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchison KE, Haughey H, Niculescu M, Schacht J, Kaiser A, Stitzel J, Horton WJ, Filbey F. The incentive salience of alcohol: translating the effects of genetic variant in CNR1. Arch Gen Psychiatry. 2008;65:841–850. doi: 10.1001/archpsyc.65.7.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagerovic N, Fernandez-Fernandez C, Goya P. CB1 cannabinoid antagonists: structure-activity relationships and potential therapeutic applications. Curr Top Med Chem. 2008;8:205–230. doi: 10.2174/156802608783498050. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA. Cannabis use, abuse, and dependence in a population-based sample of female twins. Am J Psychiatry. 1998;155:1016–1022. doi: 10.1176/ajp.155.8.1016. [DOI] [PubMed] [Google Scholar]
- Li T, Liu X, Zhu ZH, Zhao J, Hu X, Ball DM, Sham PC, Collier DA. No association between (AAT)n repeats in the cannabinoid receptor gene (CNR1) and heroin abuse in a Chinese population. Mol Psychiatry. 2000;5:128–130. doi: 10.1038/sj.mp.4000670. [DOI] [PubMed] [Google Scholar]
- Martin ER, Bass MP, Kaplan NL. Correcting for a potential bias in the pedigree disequilibrium test. Am J Hum Genet. 2001;68:1065–1067. doi: 10.1086/319525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Stolar M, Stevens DE, Goulet J, Preisig MA, Fenton B, Zhang H, O'Malley SS, Rounsaville BJ. Familial transmission of substance use disorders. Arch Gen Psychiatry. 1998;55:973–979. doi: 10.1001/archpsyc.55.11.973. [DOI] [PubMed] [Google Scholar]
- Nides M. Update on pharmacologic options for smoking cessation treatment. Am J Med. 2008;121:S20–S31. doi: 10.1016/j.amjmed.2008.01.016. [DOI] [PubMed] [Google Scholar]
- O'Connell JR, Weeks DE. PedCheck: a program for identification of genotype incompatibilities in linkage analysis. Am J Hum Genet. 1998;63:259–266. doi: 10.1086/301904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stinson FS, Ruan WJ, Pickering R, Grant BF. Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychol Med. 2006;36:1447–1460. doi: 10.1017/S0033291706008361. [DOI] [PubMed] [Google Scholar]
- Treatment Episode Data Set (TEDS) Substance Abuse Treatment Admissions by Primary Substance of Abuse, According to Sex, Age Group, Race, and Ethnicity, funded by the Substance Abuse and Mental Health Services Administration, DHHS. 2003 The latest data are available at 800-729-6686 or online at www.samhsa.gov.
- Tsuang MT, Bar JL, Harley RM, Lyons MJ. The Harvard Twin Study of Substance Abuse: what we have learned. Harv Rev Psychiatry. 2001;9:267–279. [PubMed] [Google Scholar]
- Zhang PW, Ishiguro H, Ohtsuki T, Hess J, Carillo F, Walther D, Onaivi ES, Arinami T, Uhl GR. Human cannabinoid receptor 1: 5' exons, candidate regulatory regions, polymorphisms, haplotypes and association with polysubstance abuse. Mol Psychiatry. 2004;9:916–931. doi: 10.1038/sj.mp.4001560. [DOI] [PubMed] [Google Scholar]
- Zuo L, Kranzler HR, Luo X, Covault J, Gelernter J. CNR1 Variation Modulates Risk for Drug and Alcohol Dependence. Biol Psychiatry. 2007;62:616–626. doi: 10.1016/j.biopsych.2006.12.004. [DOI] [PubMed] [Google Scholar]