Abstract
Older African Americans have higher rates of vision impairment lower utilization rates of comprehensive eye care, compared to whites. InCHARGE© is an eye health education program for this population that promotes prevention through the annual, dilated comprehensive eye examination. This study, using a pre/post design, evaluated whether InCHARGE imparted knowledge about prevention and strategies for reducing barriers to care. The program was presented to 85 older African Americans in 5 senior centers in Montgomery, Alabama. Changes in attitudes about annual eye care were assessed by a questionnaire before and 3 months after InCHARGE. At baseline most (>85%) responded it would not be difficult for them to find an ophthalmologist or optometrist, and the exam cost was not a problem. 25% reported problems finding transportation to the doctor and covering the eyeglasses cost. 44% reported not having an eye exam in the past year; 13% reported not having one within 2 years. Three months after InCHARGE those who reported that they could find a way to get to the doctor increased. After InCHARGE, 72% said they either had received or scheduled an eye exam. Responses to a question about what was learned from InCHARGE indicated that the InCHARGE’s key messages about comprehensive eye care were successfully imparted to most. This study suggests that older African Americans in the urban South have positive attitudes about eye care, even before an eye health education presentation. Following InCHARGE, they identified transportation problems less frequently as a barrier, indicated that they learned InCHARGE’s key message, and had plans for seeking routine, preventive eye care. A next step is to verify through medical record review the extent to which the high rates of self-reported eye care utilization reflect behavior.
Keywords: health education, eye care utilization, aging, vision impairment, barriers to care
Introduction
Blindness and eye disease rates among older African Americans are two times higher than those of older whites, especially uncorrected refractive error (e.g., myopia, presbyopia), cataract, glaucoma, and diabetic retinopathy.1-3 The public health challenge is that if these eye problems had been detected early, much of this disease and vision impairment would be reversible and preventable with currently available ophthalmic treatments.1-6 For example, early detection and treatment of diabetic retinopathy can reduce the development and progression of the disease by at least 50%.4 Benefits to eye health and quality of life have been reported for early detection and treatment of glaucoma, cataract, and refractive error.7-10
Previous research has suggested that older African Americans are less likely to receive routine, comprehensive eye care, when newly emerging eye conditions could be detected and treated in a timely fashion,11-13 which could be contributing to their higher rates of eye disease and vision impairment. Factors underlying this lower utilization include inadequate knowledge of basic symptoms, risk factors, and treatments available, differences in financial resources, and numerous barriers to receiving eye care such as transportation and cost.14-18
Researchers in other medical specialties (e.g., diabetes, oncology, and dentistry) have successfully increased health care prevention practices and reduced impairment and disability through health education programs based in a community’s cultural context.19-21 Thus, it is reasonable that community-based eye health education programs might likewise be successful. The literature on health education/promotion in eye care has been sparse, with a few position papers underscoring its importance,22-24 and a few education initiatives25-28 and eye health screening studies.29, 30 There have been very few scientific evaluations of existing programs published in the peer-review literature. Providing eye health educational resources (booklet, video, phone counseling) in a clinic where eye care services are available doubled the eye exam rate among African Americans.25 A multimedia campaign in California combined with patient interaction increased the use of eye care services.27 It remains to be determined if eye health education initiatives targeted at elderly African American would have a similar positive outcome. A vision screening initiative in the community found only moderate success in getting those African Americans who underwent vision screening to subsequently go for complete eye exams. Screening by itself does not serve as comprehensive health education, leading to health behavior change.31-34 Thus it is probably unrealistic to expect vision screening initiatives on their own to raise the African American community’s awareness of the importance of routine, preventive eye care and lead to prevention practices.
Here we describe the first step in evaluating an eye health education program tailored for older African Americans. The program is called InCHARGE©, which stands for In Communities Helping African Americans Receive General Eye Care. It is designed for administration in a group setting in the community, such as in senior centers where older adults congregate. The primary message of InCHARGE is eye disease prevention through the annual, dilated comprehensive eye examination and strategies for removing barriers to care. The purpose of this study is to examine whether InCHARGE imparts knowledge to the target audience about the importance of preventive eye care and strategies for overcoming barriers to eye care.
Methods
The Montgomery Area Council on Aging facilitated our efforts in contacting 5 senior centers in metropolitan Montgomery that served predominantly African American communities and were open between May and July 2007. All 5 centers were located within churches. The Institutional Review Board at the University of Alabama at Birmingham approved the study protocol.
Approximately 1 week before the InCHARGE presentation at a senior center, posters announcing the upcoming event were posted, and brochures providing information on the purpose of InCHARGE were made available at the center’s front desk. The health educator, who would be delivering the presentation, visited the center before the day of the event to introduce herself to the center staff and to become familiar with the room set-up where InCHARGE would be held. In addition to the health educator who delivered the presentation, the InCHARGE team consisted of 2 to 3 assistants who helped greet attendees and assisted with distributing a short 7-item questionnaire to all attendees before the presentation began. The self-administered questionnaire asked about attitudes, beliefs, and perceived barriers with respect to issues involved in going to the ophthalmologist or optometrist, including “If you wanted to see an eye doctor, would it be hard to find one?”, “If you had an appointment at an eye doctor, would you have a way to get there?”, “Is the cost of having an eye exam a problem for you?”, “If you need to get new eye glasses, would cost be a problem for you”, “Are you comfortable talking to the eye doctor about your eyesight?”, “Do you think it is important to go to the eye doctor every year?”, and “Do you think the eye doctor cares about your eyesight?”. The response options were “yes” or “no”. Two additional items asked the respondent about the last time when he/she visited an eye doctor and about the quality of his/her eyesight (response choices of excellent, very good, good, fair, and poor).
The InCHARGE presentation started after all questionnaires were collected. The instructor stood in front of the group, and an easel was set up in front of the room and displayed a sequence of posters conveying key messages and themes of InCHARGE, synchronized in time with the instructor’s remarks. The presentation lasted 45 minutes and was interactive in that the instructor often posed questions and solicited comments from the audience to facilitate audience participation and rapport. As attendees left the event, each received a tote bag containing a booklet summarizing the InCHARGE key points made, contact information for ophthalmologists’ and optometrists’ offices and transportation services in their area, and a coupon from area optical shops for the purchase of new eyeglasses. Table 1 lists the content domains addressed by the InCHARGE curriculum. The curriculum’s content was based on the results of a content analysis of the discussions in focus groups with older African Americans in Birmingham and Montgomery, Alabama;16 the topic of discussion in these groups was attitudes and beliefs about vision and eye care and about the perceived barriers to care. Its structure was based on the empowerment model,35 the Health Belief Model,33 and Social Learning Theory.34
Table 1.
InCHARGE© curriculum
| Key Components |
|---|
| Being InCHARGE of your eye health |
| Understanding prevention |
| What is prevention and why it is advantageous to health |
| How a comprehensive eye exam can be a way to prevent eye problems |
| Common eye problems for older African Americans |
| Blurry vision (near-sightedness, far-sightedness, presbyopia, cataract) |
| Glaucoma |
| Diabetic Retinopathy |
| What does a comprehensive eye exam involve |
| Parts of the eye your doctor may discuss with you |
| What does “dilated” mean; why is it important to have your eyes dilated |
| The difference between a comprehensive eye exam and a vision screening |
| Why it’s important to get a comprehensive eye exam every year |
| Being InCHARGE of solving common challenges |
| How to find an eye doctor |
| What is an ophthalmologist; optometrist; optician |
| Resource list for eye doctors in your area. |
| Making and keeping the appointment |
| How to find transportation to the eye doctor |
| Transportation services in your area if you don’t drive or family/friend can’t take you |
| Covering the cost of your comprehensive eye exam |
| Medicare and Medicaid: What do they cover |
| If you don’t have health insurance: a resource list for eye care services |
| Communicating with your doctor |
| Your rights as a patient |
| Being a good listener |
| If you have questions, ask them. |
| Before the doctor leaves the room … |
| Building trusting relationship with your doctor |
| Being InCHARGE of your eye care future |
| Setting a goal to have a dilated comprehensive eye exam every year |
| Be InCHARGE; Steps 1, 2, and 3 |
| Making the commitment to your eye health |
Three months after the InCHARGE presentation, an interviewer telephoned attendees in order to repeat the 7-item questionnaire administered before the class. Additional questions were also asked about whether the person sought a comprehensive eye exam in the three-months since the class, whether the exam was worthwhile, whether they used the resource book sent home, what they learned from the class, and what were their eye care plans for the next two years.
Results
Eighty-five older African Americans attended one of the presentations. Group size at the five senior centers where InCHARGE was held varied from 9 to 24 attendees (mean 17). The average age was 77 years old (SD 9) and ranged from 52-100 years old. When asked when was the last time they visited an eye doctor for an eye exam, 56% of attendees reported that it was within the last year, and 31% reported within 1 to 2 years. Twelve percent reported their last visit to the eye doctor was more than 2 years ago and 1% reported never having been to an eye doctor. Participants’ self-rating of their eyesight was 5% reporting excellent, 32% very good, 46% good, 12% fair, and 5% poor.
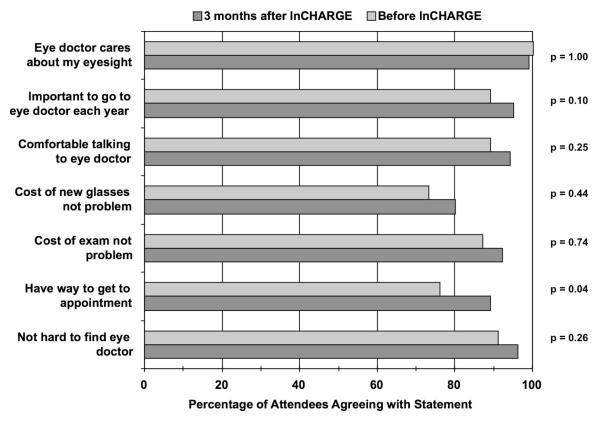
All 85 attendees provided responses on the pre-event questionnaire. At the three-month telephone follow-up, 71 participated; the remaining 14 did not participate because they declined to participate (8), had no memory of attending the class (1) or could not be contacted by telephone (2 with no answer after 10 call-attempts, 3 invalid phone numbers). Figure 1 displays the results from the 7-item questionnaire on attitudes and beliefs about eye care, before and three-months after InCHARGE. Before the presentation, the vast majority of attendees displayed positive attitudes about going to the eye doctor annually (89%), communicating with the eye doctor (89%), finding an eye doctor (91%) and covering the cost (87%) and acknowledged that the eye doctor cares about their eyesight (100%). Percentages were lower for items addressing they had a way to get to the appointment (76%) and the cost of eyeglasses was not a problem (73%). Three months following InCHARGE, the percentage of attendees expressing positive attitudes about eye care increased, even for those positive responses that were at high rates to begin with before InCHARGE. However, only one of these increases was statistically significant, the percentage of those who said they had a way to the eye appointment (p=0.04)
Figure 1.
Percentage of attendees agreeing with statements about eye care before and three months after participating in InCHARGE.
With respect to eye care utilization in the three months following InCHARGE, 72% (51 of 71) of those interviewed indicated that they either had a comprehensive eye exam by an ophthalmologist or optometrist since InCHARGE (40), or had made an appointment for one (11). All 40 of those persons who had undergone a comprehensive exam since InCHARGE reported it worthwhile. Sixty-four percent reported receiving a new prescription for eyeglasses during the exam, although less than half (44%) who received a prescription reported getting it filled. Of those who did not undergo an exam or did not set up an appointment after InCHARGE (n = 20), their reasons for not doing so were that they saw no reason to go for a comprehensive eye exam (8), they had not gotten around to it yet (7), or they went to the eye doctor shortly before the InCHARGE class (5).
Table 2 lists how participants responded to the question “What was the most important thing you learned from the InCHARGE class?” Responses fell into 7 categories, with 75% of respondents (55 of 71) identifying messages presented at the class. In order from most to least frequent message conveyed, these were the importance of getting an eye exam, obtaining information on common eye conditions, that the eye exam should occur every year, importance of that exam being a dilated exam, establishing good communication with the doctor, and other. Twenty-five percent of respondents (18 of 71) were unable to identify what they learned, even though they attended the class.
Table 2.
At follow-up, how participants responded to the question “What was the most important thing you learned from the InCHARGE class? (N=71)
| Categories of Response and Examples | Frequency of Category |
|---|---|
| Importance of getting eye examination | 17 |
| “It’s important to have your eyes checked” | |
| “It’s important to get an eye exam” | |
| Obtained information on eye care and common eye conditions in older adults | 13 |
| “I learned a lot about cataract and glaucoma” | |
| “To take good care of your eyes” | |
| Importance of getting eye examination every year | 10 |
| “Get eyes checked yearly to prevent something being wrong with eyes” | |
| “Learned how important it is to see an eye doctor every year” | |
| Importance of getting eyes dilated during exam | 5 |
| “Make sure you get your eyes dilated when you go” | |
| “It is important to get your eyes dilated” | |
| Establishing good communication with eye doctor | 4 |
| “Be frank with your doctor; express how your eyes feel” | |
| “Be comfortable with doctor; ask the doctor questions” | |
| Other | 4 |
| “I can use the discount coupon for eyeglasses at the optical shop” | |
| “Keep your glasses clean” | |
| Don’t know | 18 |
| “I can’t remember” |
Table 3 lists how participants responded to the question “What plans do you have for your eye care in the next two years?” Responses were grouped into two categories, those that were consistent with the main messages of the InCHARGE curriculum, and those that were inconsistent. Results were that 87% of respondents (62 of 71) identified plans for the future consistent with InCHARGE’s key messages, with most centering on a plan for routine eye care by an eye specialist. The remaining 13% (9 of 71) did not provide a response in line with InCHARGE’s key message of preventive routine eye care.
Table 3.
At follow-up, how participants responded to the question “What plans do you have for your eye care in the next two years?” (N=71)
| Categories of Response and Examples | Frequency of Category |
|---|---|
| Responses consistent with InCHARGE | 62 |
| “To get my eyes checked once each year” | |
| “To keep getting my eyes checked” | |
| “Follow-up on appointments” | |
| “To continue to see my doctor and use my eye drops” | |
| “To keep my appointment and keep a watch on my cataracts” | |
| “Because of severe vision loss, hoping not to go completely blind so I will keep my appointments” |
|
| “Have my eyes checked at least yearly and more often if necessary” | |
| “Continue to see my ophthalmologist” | |
| “See my optometrist as often as needed” | |
| Responses inconsistent with InCHARGE | 9 |
| “Will go to doctor only if my eyes worry me” | |
| “No plans; if anything goes wrong, I will go to the doctor then” | |
| “Not certain” | |
| “Just hope my eyes are good” | |
| “Don’t have plans” |
Discussion
These results suggest that, even before an eye health education class, older African Americans living in the urban south who attend senior centers had generally positive attitudes about seeking eye care, consistent with previous focus groups.16 Over 85% of those surveyed stated they agreed it was important to seek annual care from an eye doctor, felt comfortable talking to the doctor, and could find and cover the cost of an eye doctor appointment. On the other hand, there was less affirmation they could find transportation to the appointment. Previous research has suggested that finding transportation to healthcare appointments remains a challenge for older adults because driving cessation is more common among the elderly,36, 37 and even for those who do drive, driving exposure is often limited to highly familiar routes close to home.38, 39 The cost of eyeglasses was a concern for about ¼ of those surveyed. Medicare does not cover the cost of spectacle frames or lenses, except following cataract surgery, and thus for many older adults, eyeglasses are an out-of-pocket expense.
Positive attitudes about seeking eye care, finding and communicating with an eye doctor, and covering the appointment’s cost were pervasive in the sample, creating a ceiling effect at baseline. Thus, an increase in the percentage of participants expressing positive attitudes in these areas following InCHARGE could not be observed. However, our post-InCHARGE survey revealed the program had a positive impact on attitudes about transportation problems in that there was an increase in the percentage of attendees at the three-month follow-up who indicated that they could find a way to the appointment. This suggests InCHARGE successfully conveyed strategies for reducing transportation barriers (e.g., asking family/friends for ride, using community transportation services).
Before InCHARGE, about half of attendees (56%) reported having an eye examination by an eye doctor in the previous year. Although our sample size is small, this eye care utilization rate for older African Americans is similar to those reported for larger sample studies that also used self-report methods.12, 13 Given the higher rate of vision impairment among older African Americans as compared to other segments of the population, that half of older African American may not be receiving annual eye care is cause for concern. An important question is to what extent self-reported eye care utilization rates by older African Americans reflect actual use, but there are no studies that have addressed this issue. Many studies have examined the relationship between self-reported health care utilization (not just eye care) and actual utilization, largely in older adult populations, finding that self-report data have highly variable accuracy.40 This body of work has not focused on utilization by older African Americans.
Three-months following InCHARGE, ¾ of attendees reported they received an exam since InCHARGE or had one scheduled for the near future. These results suggest InCHARGE may have been effective in influencing behavior to seek comprehensive eye care. However, given that previous research suggests uncertainty about the accuracy of self-reported health care utilization, further research is advisable to confirm that medical records verify these self-reported visits to the eye care specialist.
In response to the question about what they learned from InCHARGE, the vast majority stated one of the curriculum’s key messages about the routine use of comprehensive eye care or strategies for removing barriers to care. When asked about plans for the future and eye care, most acknowledged they would seek care on a routine basis. These responses are encouraging since they were spontaneously generated answers, rather than choosing among multiple-choice options.
This study suggests that the InCHARGE curriculum conveys and reinforces information about the preventive importance of routine comprehensive eye care to older African Americans and may influence their seeking of eye care. This study was conducted in metropolitan Montgomery, Alabama. The older African Americans from this region who attended displayed generally positive attitudes about eye care even before participating in InCHARGE, and thus were near ceiling on some outcomes of interest. Thus they may not have been the ideal population for testing the responsiveness of InCHARGE. Our next step is to explore InCHARGE’s responsiveness among older African Americans in rural counties, where vision impairment rates are even further exacerbated and perceived barriers to care are more numerous.
Acknowledgments
This research was funded by the National Institutes of Health grant R21-EY14071, EyeSight Foundation of Alabama, Pfizer, Research to Prevent Blindness Inc., and the Alfreda J. Schueler Trust.
References
- 1.Sommer A, Tielsch JM, Katz J, et al. Racial differences in the cause-specific prevalence of blindness in east Baltimore. New Engl J Med. 1991;325:1412–1417. doi: 10.1056/NEJM199111143252004. [DOI] [PubMed] [Google Scholar]
- 2.West SK, Munoz B, Schein OD, et al. Racial differences in lens opacities: The Salisbury eye evaluation (SEE) project. Am J Epidemiol. 1998;148:1033–1039. doi: 10.1093/oxfordjournals.aje.a009579. [DOI] [PubMed] [Google Scholar]
- 3.Tielsch JM, Sommer A, Katz J, et al. Racial variations in the prevalence of primary open-angle glaucoma. JAMA. 1991;266:369–374. [PubMed] [Google Scholar]
- 4.The Diabetes Control and Complication Trial Research Group Lifetime benefits and costs of intensive therapy as practiced in the diabetes control and complications trial. JAMA. 1996;276:1409–1415. [PubMed] [Google Scholar]
- 5.Tielsch JM, Sommer A, Will J, et al. Blindness and visual impairment in an American urban population: The Baltimore eye survey. Arch Ophthalmol. 1990;108:286–290. doi: 10.1001/archopht.1990.01070040138048. [DOI] [PubMed] [Google Scholar]
- 6.Johnson CA, Keltner JL, Cello KE, et al. Baseline visual field characteristics in the ocular hypertension treatment study. Ophthalmology. 2002;109:432–437. doi: 10.1016/s0161-6420(01)00948-4. [DOI] [PubMed] [Google Scholar]
- 7.Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol. 2003;121:48–56. doi: 10.1001/archopht.121.1.48. [DOI] [PubMed] [Google Scholar]
- 8.Javitt JC, Brenner MH, Curbow B, et al. Outcomes of cataract surgery: Improvement in visual acuity and subjective visual function after surgery in the first, second, and both eyes. Arch Ophthalmol. 1993;111:686–691. doi: 10.1001/archopht.1993.01090050120041. [DOI] [PubMed] [Google Scholar]
- 9.Coleman AL, Yu F, Keeler E, et al. Treatment of uncorrected refractive error improves vision-specific quality of life. J Am Geriatr Soc. 2006;54:883–90. doi: 10.1111/j.1532-5415.2006.00817.x. [DOI] [PubMed] [Google Scholar]
- 10.Owsley C, McGwin G, Jr, Scilley K, et al. Effect of refractive error correction on health-related quality of life and depression in older nursing home residents. Arch Ophthalmol. 2007;125:1471–1477. doi: 10.1001/archopht.125.11.1471. [DOI] [PubMed] [Google Scholar]
- 11.Wang F, Javitt JC. Eye care for elderly Americans with diabetes mellitus: Failure to meet current guidelines. Ophthalmology. 1996;103:1744–1750. doi: 10.1016/s0161-6420(96)30432-6. [DOI] [PubMed] [Google Scholar]
- 12.Orr P, Barron Y, Schein OD, et al. Eye care utilization by older Americans: The SEE project. Ophthalmology. 1999;106:904–909. doi: 10.1016/s0161-6420(99)00508-4. [DOI] [PubMed] [Google Scholar]
- 13.Bazargan M, Baker RS, Bazargan S. Correlates of recency of eye examination among elderly African-Americans. Ophthalmic Epidemiol. 1998;5:91–100. doi: 10.1076/opep.5.2.91.1577. [DOI] [PubMed] [Google Scholar]
- 14.The Bausch and Lomb InVision Institute . National Study on Vision Care and Correction. Rochester, New York: 1990. [Google Scholar]
- 15.Walker EA, Basch CE, Howard CJ, et al. Incentives and barriers to retinopathy screening among African-Americans with diabetes. J Diabetes Complications. 1997;11:298–306. doi: 10.1016/s1056-8727(96)00121-3. [DOI] [PubMed] [Google Scholar]
- 16.Owsley C, McGwin G, Jr, Scilley K, et al. Perceived barriers to care and attitudes about vision and eye care: Focus groups with older African Americans and eye care providers. Invest Ophthalmol Vis Sci. 2006;47:2797–2802. doi: 10.1167/iovs.06-0107. [DOI] [PubMed] [Google Scholar]
- 17.Ellish N, Royak-Schaler R, Passmore S, et al. Knowledge, attitudes, and beliefs about dilated eye examinations among African-Americans. Invest Ophthalmol Vis Sci. 2007;48:1989–1994. doi: 10.1167/iovs.06-0934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tielsch JM, Sommer A, Katz J, et al. Socioeconomic status and visual impairment among urban Americans. Arch Ophthalmol. 1991;109:637–641. doi: 10.1001/archopht.1991.01080050051027. [DOI] [PubMed] [Google Scholar]
- 19.Watson MR, Horowitz AM, Garcia I, et al. A community participatory oral health promotion program in an inner-city Latino community. J Public Health Dent. 2001;61:34–41. doi: 10.1111/j.1752-7325.2001.tb03353.x. [DOI] [PubMed] [Google Scholar]
- 20.Walker EA, Wylie-Rosett J, Samoon G, et al. Program development to prevent complications of diabetes: Assessment of barriers in an urban clinic. Diabetes Care. 1995;18:1291–1293. doi: 10.2337/diacare.18.9.1291. [DOI] [PubMed] [Google Scholar]
- 21.Fox SA, Stein JA, Sockloskie RJ, et al. Targeted mailed materials and the Medicare beneficiary: Increasing mammogram screening among the elderly. Am J Public Health. 2001;91:55–61. doi: 10.2105/ajph.91.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Javitt JC. Preventing blindness in Americans: The need for eye health education. Surv Ophthalmol. 1995;40:41–44. doi: 10.1016/s0039-6257(95)80045-x. [DOI] [PubMed] [Google Scholar]
- 23.Kupfer C. Public health ophthalmology. Br J Ophthalmol. 1987;71:116–117. doi: 10.1136/bjo.71.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones KD, Newcomb RD. Vision health education: An idea whose time has come. J Am Optom Assoc. 1979;50:1089–1092. [PubMed] [Google Scholar]
- 25.Basch CE, Walker EA, Howard CJ, et al. The effect of health education on the rate of ophthalmic examinations among African Americans with diabetes mellitus. Am J Public Health. 1999;89:1878–1782. doi: 10.2105/ajph.89.12.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schoenfeld ER, Greene JM, Wu SY, et al. Recruiting participants for community-based research: The Diabetic retinopathy awareness program. Ann Epidemiol. 2000;10:432–440. doi: 10.1016/s1047-2797(00)00067-3. [DOI] [PubMed] [Google Scholar]
- 27.Lee PP, Linton KL, Ober RR, et al. The efficacy of a multimedia educational campaign to increase the use of eye care services. Ophthalmology. 1994;101:1465–1469. doi: 10.1016/s0161-6420(94)31151-1. [DOI] [PubMed] [Google Scholar]
- 28.National Eye Institute. National Eye Health Education Program (NEHEP) National Institutes of Health; 2007. http://www.nei.nih.gov/nehep. [Google Scholar]
- 29.Quigley HA, Park CK, Tracey PA, et al. Community screening for eye disease by laypersons: The Hoffberger program. Am J Ophthalmol. 2002;133:386–392. doi: 10.1016/s0002-9394(01)01380-0. [DOI] [PubMed] [Google Scholar]
- 30.Anderson RM, Wolf FM, Musch DC, et al. Conducting community-based, culturally specific, eye disease screening clinics for urban African Americans with diabetes. Ethn Dis. 2002;12:404–410. [PubMed] [Google Scholar]
- 31.National Cancer Institute . Making Health Communication Programs Work. National Institutes of Health; 2002. [Google Scholar]
- 32.Green LW, Ottoson JM. Community and Population Health. 8th ed McGraw-Hill; New York: 1999. [Google Scholar]
- 33.Rosenstock IM. The health belief model: Explaining health behavior through expectancies. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Heath Education: Theory, Research, and Practice. Jossey-Bass; San Francisco: 1990. pp. 39–62. [Google Scholar]
- 34.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 35.Airhihenbuwa CO, Lowe AG. Improving the health status of African Americans: Empowerment as health education intervention. In: Livingston IL, editor. Handbook of Black American Health: The Mosaic of Conditions, Issues, Policies, and Prospects. Greenwood Press; Westport CT: 1994. pp. 387–398. [Google Scholar]
- 36.Marottoli RA, de Leon CFM, Glass TA, et al. Consequences of driving cessation: Decreased out-of-home activity levels. J Gerontol: Soc Sci. 2000;55B:S334–S340. doi: 10.1093/geronb/55.6.s334. [DOI] [PubMed] [Google Scholar]
- 37.Fonda SJ, Wallace RB, Herzog AR. Changes in driving patterns and worsening depressive symptoms among older adults. J Gerontol: Soc Sci. 2001;56B:S343–S351. doi: 10.1093/geronb/56.6.s343. [DOI] [PubMed] [Google Scholar]
- 38.Ball K, Owsley C, Stalvey B, et al. Driving avoidance and functional impairment in older drivers. Accid Anal Prev. 1998;30:313–322. doi: 10.1016/s0001-4575(97)00102-4. [DOI] [PubMed] [Google Scholar]
- 39.Hu PS, Young JR. 1995 Nationwide Personal Transportation Survey. U.S. Department of Transportation, Federal Highway Administration; Washington, DC: 1999. Summary of Trends. [Google Scholar]
- 40.Bhandari A, Wagner T. Self-reported utilization of health care services: Improving measurement and accuracy. Medical Care Res Rev. 2006;63:217–235. doi: 10.1177/1077558705285298. [DOI] [PubMed] [Google Scholar]