Abstract
Commonly studied physical functions include activities such as walking and climbing stairs. Despite the acknowledged role of environmental factors and behavioral strategies to compensate for reduced performance capacity or environmental barriers in characterizing physical functioning, most assessments do not take these factors into account. This article presents a new conceptual model for assessment of relevant physical functioning while accounting for habitual environmental factors and compensation strategies.
Limitations in physical functioning are important to consider because of their widespread prevalence and their link to: (1) decreased quality of life, (2) increased risk of disability, falls and fractures, and depression, and (3) increased health care costs.1–7 With the rising prevalence of physical limitations and attendant social, physical, and financial costs, it is increasingly relevant to examine the adequacy and completeness of our conceptualization of such limitations. It also is valuable to determine whether physical functioning assessments are adequate in identifying pertinent contributors to physical functioning capacity as well as performance ability.
Recognizing the environment in which initiation and progression of physical functioning limitations occur is essential in understanding these limitations. The World Health Organization (WHO) acknowledges the centrality of the environment when it defines activity limitations as “problems in activity that occur as a result of an interaction between a health condition and the context in which the person exists.”8,9 This environmental context can range from exposures such as air pollution and general neighborhood conditions10,11 to more immediate environmental factors such as inadequate lighting or icy sidewalks, which can facilitate or hinder physical functioning.
The degree to which individuals can and do deal with diminished abilities and environmental challenges determines how well they will function in their real-life setting.9–12 Common compensation and coping strategies, for example, include modifying the way an activity is performed, recruiting external supports such as an assistive device or another person, and avoidance.13–17
Many assessments of functioning do not capture the broad dynamic of personal, social, environmental, and compensatory strategies in physical functioning performance.8,12,18–21 Various conceptual models depicting interactions between the environment and physical functioning tend to be focused on interventions at the individual level (eg, clinically oriented models guiding assessment and treatment of patients)22,23 or are public health-oriented models aimed at intervening at the community level (eg, improving access for people with disabilities).24 Conceptual models describing aging-related physical functioning difficulties tend to focus on development of these limitations1 and are not readily translated to the assessment realm.
The purpose of this article is to present a new conceptual model—Physical Functioning Assessment in Your Environment (PF-E)—for the assessment of physical functioning status. In the model, physical functioning is conceptualized as being supported by physical abilities such as walking, reaching, vision, and hearing, as well as by those in the cognitive domain such as spatial orientation, short-term memory, intelligible speech, and alertness.2 The model also addresses habitual environmental factors and compensation and coping strategies.
The conceptual model draws upon constructs identified in the 2001 International Classification of Functioning, Disability and Health (ICF)8,25 and the ideas and research of Fried,13,14 Agree,18 Kielhofner,22 Lawton,26–28 and others.15–17,29 The development of this conceptual model is motivated by the escalating prevalence of limited physical functioning, the desire to broaden the focus of current conceptualizations of physical functioning used in clinical treatment paradigms; the limited incorporation of cognitive aspects in characterizing physical functioning, lack of assessments incorporating the breadth of personal and community factors that impinge upon living with physical functioning limitations, and failure to include assessment of potentially modifiable community-level factors.
Prevalence of Limited Physical Functioning Difficulties
Limitations in physical functioning are fairly common among middle-aged and older Americans. Among those 60 to 69 years of age, 21% reported difficulty or inability to walk 0.4 km (0.25 mile),7 and this proportion increased to 30% and 49% in the 70- to 79-year-old and ≥80-year-old age groups, respectively. In a population-based survey of Americans over 65 years of age, 12% had difficulty hearing normal conversation, and 11% had difficulty seeing words or letters in newsprint.30 Among those 45 to 64 years of age, 16% were limited in their ability to engage in work, school, play, or other activities for health reasons.31
The ICF: A Broad Framework of Health and Human Functioning
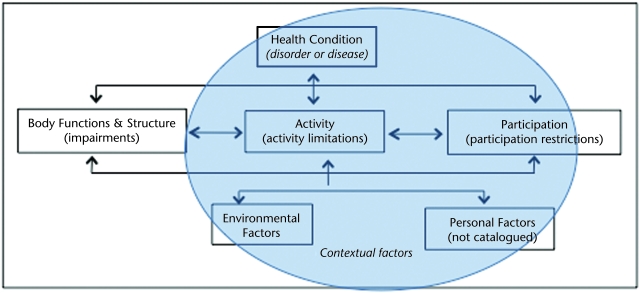
The WHO's ICF8 represents a detailed examination of both environmental factors and individual-level factors as they relate to health and human functioning. Although this classification system is not specifically focused on physical functioning assessment, it does provide a framework upon which conceptual models can be developed. The classification system addresses the biological, psychological, social, and environmental components of disability (schematic shown in Fig. 1; accompanying definitions shown in the Table). In the ICF context, a health condition includes diseases, disorders, injury, or trauma; aging; and congenital anomalies that interrelate with 3 functioning components: (1) body functions and body structures, (2) activities, and (3) participation. Figure 1 shows the interplay of these functioning components with contextual aspects, including environmental and personal factors.
Figure 1.
International Classification of Functioning, Disability and Health model of disability. Reprinted with permission of the World Health Organization from: International Classification of Functioning, Disability and Health: Short Version. Geneva, Switzerland: World Health Organization; 2001:26.
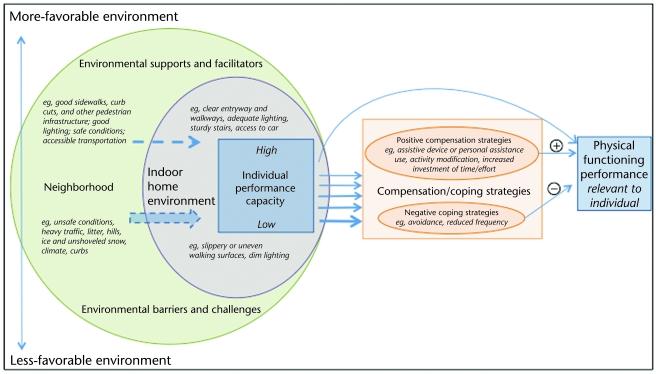
Table.
Terms and Definitions Used in the 2001 International Classification of Functioning, Disability and Health8
The ICF broadly characterizes environmental factors, considering products and technology, the natural environment and human-made changes to the environment, social support and relationships, attitudes, and the availability of services, systems, and policies. Although this WHO-endorsed classification incorporates a broad set of environmental components, it recognizes, but does not classify, personal factors, such as age and sex, which are acknowledged as integral to functioning, disability, and health.8,25
The ICF characterizes disability as a problem in 1 of the 3 functioning components after contextual factors are considered. Deficits in body structure or function are identified as impairments, difficulties with tasks or actions are labeled activity limitations, and problems with social participation are termed participation restrictions. Impairments, activity limitations, and participation restrictions are considered disabilities (ie, if the interaction between a person's health condition and the contextual influences surrounding that person results in less than a full range of functioning, that person is considered disabled).
The ICF provides 2 important qualifiers to describe severity of activity limitations: the performance qualifier, which describes what an individual does in his or her current environment, and the capacity qualifier, meant to represent the environmentally adjusted ability of the individual. Whereas the former qualifier describes the features of an individual's environment, the latter qualifier describes an individual's ability to execute a task or an action in a standard or uniform environment. Thus, the discrepancy between capacity and performance in the ICF classification provides a useful guide as to what can be done to enhance the individual's environment to aid in improving functioning and is highly consistent with use in developing policies. Given the breadth of possibilities afforded by the ICF, it is useful to consider this framework as a point of reference when evaluating existing models.
Physical Functioning and the Environment: Models and Assessments Focused on the Individual
Contribution of Conceptual Model Incorporating the Home Environment and Physical Functioning
Seminal work that conceptualized the role of an individual's home environment in physical functioning performance was published by Lewin32 in his person-environment (PE) fit and Life Space models. Person-environment fit describes the level of accommodation provided by a person's environment for performance of activities. The PE fit model has 2 interactive components: the person component and the environment component. The person component is defined as a set of competencies, including biological health, sensory and motor skills, and cognitive function, and the environment component is defined in terms of demands. Demands are expressed as environmental “press” (ie, the strength with which the environment demands a response from the person).
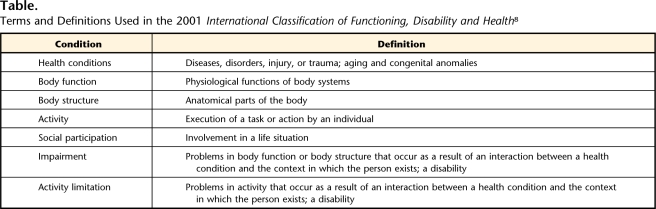
The concept of PE fit is represented in Figure 2, showing Lawton's press-competence model,28 wherein an individual with a given competence interacts with an environmental situation having a given “press” or demand. The central line, labeled “adaptation level,” represents a theoretical level where the environmental press level matches the competence of the person. In terms of physical functioning, physical barriers in the environment are not necessarily problems per se. Instead, the magnitude of problems differs for different people, depending on each person's competence level.28 If environmental press is too strong or too weak relative to the level of competence, negative affect and maladaptive behavior will occur. In a related concept, the environmental docility hypothesis, Lawton and Simon26 postulated that individuals with lower competence are more sensitive than those with higher competence to the demands of their environment. This phenomenon is portrayed in Figure 2 by the relatively narrow bands of maximum comfort and performance associated with low competence compared with the wider bands associated with high competence. Home and neighborhood environments, therefore, become critically important for individuals with less physical and cognitive capacity.33
Figure 2.
Lawton's press-competence model. Reprinted with permission of the American Psychological Association from: Lawton MP, Nahemow L. Ecology and the aging process. In: Eisdorfer C, Lawton MP, eds. The Psychology of Adult Development and Aging. Washington, DC: American Psychological Association; 1973. Copyright 1973 by the American Psychological Association.
Lawton's ecological model was developed to explain the interaction between an individual and his or her home environment; however, the model's focus is on the home environment, and the context of outdoor public space is very different in terms of the ideal level of press. Whereas the home environment optimally will be adapted to an individual with a specific competence level (expected to decline with age), public space serves the entire community and a wide range of competence levels. Therefore, in extending this concept to the public health realm, the ideal amount of press would be different than that for an individual's home environment.
Clinically Oriented Conceptual Models and Assessments
Many physical functioning conceptual models acknowledge environmental factors, but the majority of these models were developed to guide the assessment and treatment of clinical endpoints. Such models offer a comprehensive portrayal of the individual's process of adaptation to shifting environmental demands or an altered “performance capacity” (eg, diminished physical or cognitive ability),22,34 and related assessments reflect these considerations. Outcomes typically included in such assessments are improvement of physical capacity, behavior modification to compensate for lower capacity or a more demanding environment, modification of expectations and goals, and modification of the home environment. For example, both the Canadian Occupational Performance Measure, based on the Canadian Model of Occupation Performance,34 and the Occupational Performance History Interview II,22 rooted in the Model of Human Occupation, are specifically intended for use as initial assessments on which occupational therapy goals and treatment are developed.
Thus, although environmental, compensation, and coping factors are incorporated into these assessments, they are ultimately aimed at changing individual behaviors and environments. Furthermore, these and other assessments such as the Craig Handicap Assessment and Reporting Technique (CHART35) are intended for use in people with existing physical functioning deficits. This setting is different from public health and prevention-oriented models and assessments, most of which are intended for use in the general population with a wide range of limitations and a range of developmental stages. Thus, although clinically oriented conceptual models offer insight into the individual realm, they do not address opportunities to measure and change community-level factors.
Physical Functioning and the Environment: Models and Assessments Focused on Community-Level Factors
Although social, political, and public health conceptual models offer insight into the interaction between individual and community-level factors as they relate to aging, physical functioning, and disability,36 they tend to focus on broad dynamics of the system and environmental factors rather than physical functioning performance in the context of these environmental factors. The “universal design” movement,24 for example, promotes support of cognition, vision, hearing and speech, body function, and mobility through incorporation of community-level features usable by everyone. Although the individual is recognized as a key element in the dynamic, the focal point is the environment. Questionnaires such as the Craig Hospital Inventory of Environmental Factors,37 the Facilitators And Barriers Survey of environmental influences on participation among people with lower limb Mobility impairments and limitations (FABS/M),38 and the Community Health Environment Checklist39 assess environmental barriers and absence of supports in physical functioning, participation, and life satisfaction, but they do not measure an individual's physical functioning performance. In sum, although many conceptual models and assessments of physical functioning acknowledge both capacity and environment, they tend to be aimed at either individual-level or community-level factors.
Physical Functioning Assessment: Need for Improvement
Recently, some authors14,15,40–44 have argued that traditional assessments of physical function do not adequately capture “real-life” functioning performance. If the interplay among an individual's performance capacity, his or her habitual indoor and outdoor environments, and his or her compensatory and coping strategies are not characterized, an incomplete picture of physical functioning performance results.45–49 Furthermore, no conceptual model is identified in the description of many physical functioning assessments.
Failure of existing assessments to specify the context in which respondents should report their functioning level limits the ability to fully capture and interpret such functional measures. For example, a different set of strategies is needed to negotiate life in a city high-rise apartment with an elevator versus a suburban 2-story house with a basement. Furthermore, when an assessment does not instruct respondents to report ability in performing tasks in a standard way (termed “capacity” by the ICF) or as usual performance, it is not possible to know how to correctly interpret the resulting data.
Agree18 contended that the dynamic between the use of assistive technology and the amount of functional disability in the absence of modifications or adjustments is an important area of assessment. Agree defined residual disability as the degree of disablement that remains after personal care or assistive technology has ameliorated some part of the total underlying need. She pointed out that with the use of equipment or human help, some individuals may report no problems at all—and, as such, this construct is an important, albeit underassessed, component when considering limitations in physical functioning. This important dynamic is identifiable in a cross-sectional assessment conducted in a nationally representative sample by the National Center for Health Statistics.50 In that study, 10.1% of the participants aged 45 to 64 years and 5.7% of those aged ≥65 years reported long-term use of an assistive technology, yet considered themselves as having no limitations. Thus, these individuals forestalled classifying themselves as having activity limitations through compensation strategies that modified their environments.
Use of compensatory and coping strategies is common among people with reduced performance capacity. In a study of 248 older adults with osteoarthritis, only 3 respondents reported no adaptations in performing activities related to personal care, mobility, and household tasks, and they valued activities such as socializing, physical activities, and traveling.20 Thus, failure to capture such strategies when characterizing physical functioning performance precludes a comprehensive portrayal of an individual's real-life performance. Furthermore, although research suggests that compensatory strategies reduce difficulty in performing physical functions,14,50 human help frequently is used as an endpoint to represent “poor functioning.”51 Although the assumption that human help is utilized in the most severe limitations in physical functioning, Hoenig and colleagues’15 research suggests that the choice of compensation strategy is determined, in part, by logistical factors rather than by severity. Individuals living with another person were more likely to use human help than to use of an assistive device.
Research on strategies to compensate for increased environmental press among individuals with high performance capacity is not well addressed in the physical functioning literature. Weiss et al defined a compensatory strategy as “a way of achieving a result that is adopted frequently in the face of physical impairment or limitation and under usual conditions.”29(p1217) In Hoenig and colleagues’ 2006 study,15 those individuals with the best physical performance did not use compensatory strategies, but the context of the study was indoor mobility and, therefore, presumably less demanding than outdoor mobility. Weiss et al also pointed out that, under demanding environmental conditions, even the healthiest person would “appreciate a cane.” Barriers to neighborhood walking in the general population have been characterized extensively in the physical activity literature as lack of perceived personal safety, open space, and connected street networks, as well as high traffic volumes, among other features.52,53
A New Conceptual Model Describing Assessment of Physical Functioning Performance
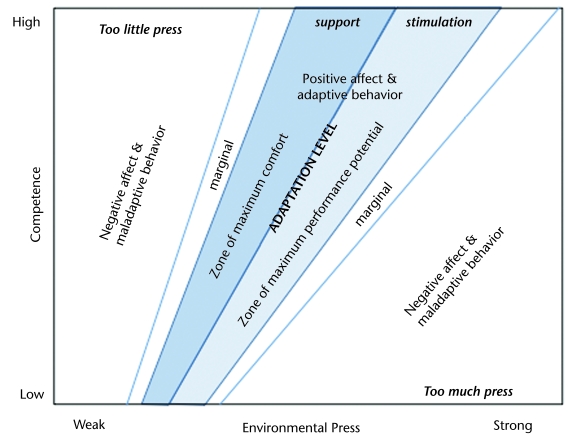
The PF-E conceptual model (Fig. 3) was developed to address the need for physical functioning assessments that reflect performance capacity, environmental factors, and coping and compensation strategies. This conceptual model is intended to serve as a guide for developing new and extending existing perceived and performance-based physical functioning assessments targeted toward middle-aged and older people living in urban and suburban areas. The model also highlights the opportunity to separately characterize home and neighborhood environments to identify possible areas of environmental improvement.
Figure 3.
The Physical Functioning Assessment in Your Environment (PF-E) conceptual model, integrating the indoor and outdoor environments, compensation strategies, and physical functioning performance.
Functions described by the PF-E conceptual model include those that support mobility in a broad sense, such as walking, climbing stairs, reaching, standing, seeing and reading, hearing, spatial orientation, and transportation, among others. The individual is represented in the box labeled “individual performance capacity” in Figure 3. A range of performance capacity levels is shown, from “high” at the top of the box to “low” in the bottom part of the box. This range of capacities can be thought of as differences among people or differences within an individual over time as they experience decline in functioning capacity.
Within each unique environment, barriers and supports are present. Although neighborhood barriers and supports to physical functioning are unique for each community assessed, home supports and barriers will be unique to individuals (unless they are living in an institutional setting). Thus, it is clear that habitual existence in public and private environments collectively characterizes an individual's unique environment. More-favorable environments are represented in the upper part of Figure 3, whereas less-favorable environments are shown at the bottom of the figure.
Environmental press is shown in Figure 3 with arrows pointing from the neighborhood, through the indoor environment toward the individual's performance capacity. The thick arrow portrays the larger influence of environmental press on those individuals with lower performance capacity; a thinner arrow shows that environmental press has little impact on those individuals with high performance capacity. These arrows are dashed to distinguish them from the arrows to their right depicting the immediate process of physical functioning performance.
The compensation strategies represented in this model are considered “performance qualifiers” within the ICF. Compensation strategies are used by individuals with a performance capacity in the range below “high” and by individuals who live in a less-favorable environment (those with greater press). Differences in use of compensation strategies are represented in Figure 3 by thicker arrows near the bottom of the individual performance capacity box, indicating more compensation, and by thinner arrows near the middle of the box, representing less reliance on these strategies. The illustration shows that individuals with a high level of performance capacity living in a favorable environment do not use compensation strategies for physical functioning performance.
Positive compensation strategies (eg, use of a hearing aid) enhance a person's performance capacity and improve physical functioning performance. Use of human help also is considered a compensation strategy, and this assistance may come from a family member, friend, or paid helper. Examples of human help include direct assistance, such as receiving help climbing stairs, traveling to a destination, or the performance of a task such as grocery shopping. Whereas the act of modifying the existing environment or moving to a new environment is considered compensation, once that transition has occurred, the new or modified environment simply becomes part of the habitual environment.
In sum, integration of an individual's unique environment, as well as compensation and coping strategies, into assessment of physical functioning performance is a key aspect of the model because such factors likely influence performance of an activity. The model is inclusive of a range of physical and cognitive functions but is meant to target assessment of functions relevant to an individual's life. The model is intended for use in developing assessments for clinical settings, as well as the public health and policy realms. Characterization of the neighborhood environment draws attention to relevant community-level factors that may be changed through legislation.
Rationale for Development of the PF-E Model
The PF-E conceptual model was created to motivate the development of physical functioning assessments that include a range of individual and community-level factors that affect performance. Although this model builds upon and extends existing seminal conceptualizations, it also differs from them in key ways.
The model presented here has drawn upon the ICF's conceptualization of capacity and performance. In Figure 1, a shaded circle has been drawn around the area of focus for the PF-E model, which includes some aspects of ICF chapters on products and technology, the natural environment and human-made changes to environment, and support and relationships. These aspects are included because they are modifiable and may directly influence an individual's capacity for physical functioning.
Although the ICF does not propose a specific conceptualization of physical functioning per se, the PF-E model highlights physical functioning within the context of relevant home and community environmental factors. For example, in Figure 1, both use of a cane for walking and an environmental barrier such as low light would be classified into the “environmental factors” box (although they are classified into separate ICF chapters), whereas they are portrayed separately in Figure 3. Delineation of such factors allows conceptualization of interplay between the individual and different facets of the environment. In addition, the PF-E differs from the ICF in that not all of the compensation strategies proposed in the PF-E are classified in the ICF. For example, modifying the way an activity is performed to make it easier is not included in the ICF.
The PF-E model incorporates ideas from Lawton26–28; however, the public health approach presented here differs from his individually tailored approach to person-environment fit. Whereas Lawton's research focused heavily on the home environment, the PF-E model incorporates the home and neighborhood environments. This is relevant because identifying the ideal amount of environmental press will be necessarily be different in someone's home versus in the community.
Summary and Future Research Needs
There is a need to improve understanding of physical functioning within an individual's unique habitual environment.25,54 Capturing this information as early as midlife, when age-related physical functioning problems often develop,55 is valuable in characterizing decline in functioning across time. The proposed model is meant to guide assessment of a wide range of physical functioning tasks in middle-aged and older suburban and urban dwellers. This could include assessment of a group with diverse performance levels or of individuals with varying performance levels across time.
The PF-E model is preliminary and, as such, will require empirical testing and conceptual refinement. It is presented as a comprehensive, but not all-encompassing, approach to assessment. For example, the environments considered do not necessarily include the workplace environment. This is a limitation of the model, because people habitually travel outside the realm presented. Future versions of the PF-E model may include a broader environment.
The specification of the neighborhood environment as unique is important because it allows for identification of a community's supports and barriers to physical functioning. Although these differences could include nonmodifiable factors such as presence of hills, other identified barriers such as lack of pedestrian crosswalks could be improved through legislation. Thus, application of the model in assessing functioning within communities could help to improve functioning at the community level. Although efforts to make cities accessible for people with overt disabilities have been visible, making communities friendlier to people with milder physical functioning problems has not been widespread. Our emphasis on compensation strategies also is valuable beyond quantifying physical functioning performance because key compensation behaviors, once identified, can be modified. Additionally, intervention with an appropriate assistive device may improve physical functioning performance.
Development of physical functioning assessments based on the PF-E model has the potential to add real-life depth to these assessments. Furthermore, gathering information on communities and individuals using a well-conceptualized and integrated model can eventually stimulate researchers and policy makers to make changes that would reduce demands on people with functional limitations and increase support for promoting community-level physical functioning.
Dr Tomey provided concept/idea/project design. Both authors provided writing. Dr Sowers provided consultation (including review of manuscript before submission).
Dr Tomey and Dr Sowers are funded, in part, with support from the National Institutes of Health, Department of Health and Human Services, through the National Institute on Aging (grants AG17104 and AG29835).
References
- 1.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. [DOI] [PubMed] [Google Scholar]
- 2.Royall DR, Lauterbach EC, Kaufer D, et al; Committee on Research of the American Neuropsychiatric Association. The cognitive correlates of functional status: a review from the Committee on Research of the American Neuropsychiatric Association. J Neuropsychiatry Clin Neurosci. 2007;19:249–265. [DOI] [PubMed] [Google Scholar]
- 3.Wolinsky FD, Miller DK, Andresen EM, et al. Effect of subclinical status in functional limitation and disability on adverse health outcomes 3 years later. J Gerontol A Biol Sci Med Sci. 2007;62:101–106. [DOI] [PubMed] [Google Scholar]
- 4.Stevens JA, Olson S. Reducing falls and resulting hip fractures among older women. MMWR Recomm Rep. 2000;49(RR-2):3–12. [PubMed] [Google Scholar]
- 5.Schieman S, Plickert G. Functional limitations and changes in levels of depression among older adults: a multiple-hierarchy stratification perspective. J Gerontol B Psychol Sci Soc Sci. 2007;62:S36–S42. [DOI] [PubMed] [Google Scholar]
- 6.Fried TR, Bradley EH, Williams C, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161:2602–2607. [DOI] [PubMed] [Google Scholar]
- 7.Ervin RB. Prevalence of functional limitations among adults 60 years of age and over: United States, 1999–2002. Adv Data. 2006;375:1–7. [PubMed] [Google Scholar]
- 8.International Classification of Functioning, Disability and Health. Available at: http://www.who.int/classifications/icf/site/index.cfm. Accessed May 2, 2008.
- 9.Jette AM. Toward a common language for function, disability, and health. Phys Ther. 2006;86:726–734. [PubMed] [Google Scholar]
- 10.Schootman M, Andresen EM, Wolinsky FD, et al. Neighborhood conditions and risk of incident lower-body functional limitations among middle-aged African Americans. Am J Epidemiol. 2006;163:450–458. [DOI] [PubMed] [Google Scholar]
- 11.Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. Am J Epidemiol. 2002;155:507–515. [DOI] [PubMed] [Google Scholar]
- 12.Dixon RA, Bäckman L. Concepts of compensation: integrated, differentiated and Janus-faced. In: Dixon RA, Bäckman L, eds. Compensating for Psychological Deficits and Declines: Managing Losses and Promoting Gains. Mahwah, NJ: Erlbaum; 1995:3–19.
- 13.Fried LP, Bandeen-Roche K, Williamson JD, et al. Functional decline in older adults: expanding methods of ascertainment. J Gerontol A Biol Sci Med Sci. 1996;51:M206–M214. [DOI] [PubMed] [Google Scholar]
- 14.Fried LP, Young Y, Rubin G, Bandeen-Roche K; WHAS II Collaborative Research Group. Self-reported preclinical disability identifies older women with early declines in performance and early disease. J Clin Epidemiol. 2001;54:889–901. [DOI] [PubMed] [Google Scholar]
- 15.Hoenig H, Ganesh SP, Taylor DH Jr, et al. Lower extremity physical performance and use of compensatory strategies for mobility. J Am Geriatr Soc. 2006;54:262–269. [DOI] [PubMed] [Google Scholar]
- 16.West SK, Munoz B, Rubin GS, et al. Compensatory strategy use identifies risk of incident disability for the visually impaired. Arch Ophthalmol. 2005;123:1242–1247. [DOI] [PubMed] [Google Scholar]
- 17.Baltes PB, Baltes MM, eds. Successful Aging: Perspectives From the Behavioral Sciences. New York, NY: Cambridge University Press; 1990.
- 18.Agree EM. The influence of personal care and assistive devices on the measurement of disability. Soc Sci Med. 1999;48:427–443. [DOI] [PubMed] [Google Scholar]
- 19.Keysor J, Jette AM, Haley SM. Development of the Home and Community Environment (HACE) instrument. J Rehabil Med. 2005;37:37–44. [DOI] [PubMed] [Google Scholar]
- 20.Gignac MA, Cott C, Badley EM. Adaptation to disability: applying selective optimization with compensation to the behaviors of older adults with osteoarthritis. Psychol Aging. 2002;17:520–524. [PubMed] [Google Scholar]
- 21.Bucks RS, Ashworth DL, Wilcock GK, Siegfried K. Assessment of activities of daily living in dementia: development of the Bristol Activities of Daily Living Scale. Age Ageing. 1996;25:113–120. [DOI] [PubMed] [Google Scholar]
- 22.Kielhofner G, Burke JP, Igi CH. A model of human occupation, part 4: assessment and intervention. Am J Occup Ther. 1980;34:777–788. [DOI] [PubMed] [Google Scholar]
- 23.Townsend E, ed. Enabling Occupation: An Occupational Therapy Perspective. Ottawa, Ontario, Canada: Canadian Association of Occupational Therapists Publications ACE; 2002.
- 24.Story MF, Mueller JL, Mace RL. The Universal Design File: Designing for People of All Ages and Abilities. Rev ed. Raleigh, NC: Center for Universal Design, North Carolina State University; 1998.
- 25.Schneidert M, Hurst R, Miller J, Ustün B. The role of environment in the International Classification of Functioning, Disability and Health (ICF). Disabil Rehabil. 2003;25:588–595. [DOI] [PubMed] [Google Scholar]
- 26.Lawton MP, Simon B. The ecology of social relationships in housing for the elderly. Gerontologist. 1968;8:108–115. [DOI] [PubMed] [Google Scholar]
- 27.Lawton MP. Three functions of the residential environment. In: Pastalan LA, Cowart ME, eds. Lifestyles and Housing of Older Adults: The Florida Experience. Binghamtom, NY: Haworth Press Inc; Journal of Housing for the Elderly. 1989:35–50.
- 28.Lawton MP. Competence, environmental press, and the adaptation of older people. In: Lawton MP, Windley PG, Byerts TO, eds. Aging and the Environment. New York, NY: Springer; 1982:33–59.
- 29.Weiss CO, Hoenig HM, Fried LP. Compensatory strategies used by older adults facing mobility disability. Arch Phys Med Rehabil. 2007;88:1217–1220. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Prevalence of disabilities and associated health conditions among adults—United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50:120–125. [PubMed] [Google Scholar]
- 31.Adams PF, Wilson Lucas J, Barnes PM. Summary health statistics for U.S. population: National Health Interview Survey, 2006. National Center for Health Statistics. Vital Health Stat. 2008:10(236). [PubMed]
- 32.Lewin K. Field Theory in Social Science. New York, NY: Harper & Brothers; 1951.
- 33.Oswald F, Hieber A, Wahl H, Mollenkopf H. Ageing and person: environment fit in different urban neighbourhoods. Eur J Ageing. 2005;2:88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carswell A, McColl MA, Baptiste S, et al. The Canadian Occupational Performance Measure: a research and clinical literature review. Can J Occup Ther. 2004;71:210–222. [DOI] [PubMed] [Google Scholar]
- 35.Whiteneck G, Brooks CA, Charlifue S, et al. Guide for use of the CHART: Craig Handicap Assessment and Reporting Technique. Available at: http://www.craighospital.org/research/CHART%20Manual.pdf. Accessed May 2, 2009.
- 36.Putnam M. Linking aging theory and disability models: increasing the potential to explore aging with physical impairment. Gerontologist. 2002;42:799–806. [DOI] [PubMed] [Google Scholar]
- 37.Whiteneck G, Meade MA, Dijkers M, et al. Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch Phys Med Rehabil. 2004;85:1793–1803. [DOI] [PubMed] [Google Scholar]
- 38.Gray DB, Hollingsworth HH, Stark S, Morgan KA. A subjective measure of environmental facilitators and barriers to participation for people with mobility limitations. Disabil Rehabil. 2008;30:434–457. [DOI] [PubMed] [Google Scholar]
- 39.Stark S, Hollingsworth HH, Morgan KA, Gray DB. Development of a measure of receptivity of the physical environment. Disabil Rehabil. 2007;29:123–137. [DOI] [PubMed] [Google Scholar]
- 40.Peel C, Sawyer Baker P, Roth DL, et al. Assessing mobility in older adults: the UAB Study of Aging Life-Space Assessment. Phys Ther. 2005;85:1008–1119. [PubMed] [Google Scholar]
- 41.Patla AE, Shumway-Cook A. Dimensions of mobility: defining the complexity and difficulty associated with community mobility. J Aging Phys Act. 1999;7:7–19. [Google Scholar]
- 42.Shumway-Cook A, Patla AE, Stewart A, et al. Environmental demands associated with community mobility in older adults with and without mobility disabilities. Phys Ther. 2002;82:670–681. [PubMed] [Google Scholar]
- 43.Bandinelli S, Pozzi M, Lauretani F, et al. Adding challenge to performance-based tests of walking: the Walking InCHIANTI Toolkit (WIT). Am J Phys Med Rehabil. 2006;85:986–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iwarsson S, Wahl HW, Nygren C, et al. Importance of the home environment for healthy aging: conceptual and methodological background of the European ENABLE-AGE Project. Gerontologist. 2007;47:78–84. [DOI] [PubMed] [Google Scholar]
- 45.McHorney CA, Kosinski M, Ware JE Jr. Comparisons of the costs and quality of norms for the SF-36 health survey collected by mail versus telephone interview: results from a national survey. Med Care. 1994;32:551–567. [DOI] [PubMed] [Google Scholar]
- 46.Coyne KS, Margolis MK, Gilchrist KA, et al. Evaluating effects of method of administration on walking impairment questionnaire. J Vasc Surg. 2003;38:296–304. [DOI] [PubMed] [Google Scholar]
- 47.Kelly-Hayes M, Jette AM, Wolf PA, et al. Functional limitations and disability among elders in the Framingham Study. Am J Public Health. 1992;82:841–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Survey of Income and Program Participation (SIPP) 2004 panel questionnaire functional limitations and disability section. Available at: http://www.bls.census.gov/sipp/top_mod/2004/quests/2004w5tm.pdf. Accessed May 6, 2008.
- 49.Haywood KL, Garratt AM, Fitzpatrick R. Older people specific health status and quality of life: a structured review of self-assessed instruments. J Eval Clin Pract. 2005;11:315–327. [DOI] [PubMed] [Google Scholar]
- 50.Madans J, Rasch B, Altman B. Exploring the impact of assistive device use on disability measurement. Available at: www.cdc.gov/nchs/ppt/citygroup/madans_rasch_altman.ppt. Accessed May 14, 2008.
- 51.Boggatz T, Dijkstra A, Lohrmann C, Dassen T. The meaning of care dependency as shared by care givers and care recipients: a concept analysis. J Adv Nurs. 2007;60:561–569. [DOI] [PubMed] [Google Scholar]
- 52.Sallis JF, Cervero RB, Ascher W, et al. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297–322. [DOI] [PubMed] [Google Scholar]
- 53.Trayers T, Lawlor DA. Bridging the gap in health inequalities with the help of health trainers: a realistic task in hostile environments? A short report for debate. J Public Health (Oxf). 2007;29:218–221. [DOI] [PubMed] [Google Scholar]
- 54.Pollard B, Johnston M. The assessment of disability associated with osteoarthritis. Curr Opin Rheumatol. 2006;18:531–536. [DOI] [PubMed] [Google Scholar]
- 55.Pope SK, Sowers MF, Welch GW, Albrecht G. Functional limitations in women at midlife: the role of health conditions, behavioral and environmental factors. Women's Health Issues. 2001;11:494–502. [DOI] [PubMed] [Google Scholar]