Abstract
Objective
To analyse the effect of enrolment in the public health insurance scheme known as Seguro Popular [People’s Insurance] on access to health resources, treatment and blood glucose control among poor adults with diabetes in Mexico.
Methods
We analysed cross-sectional data from the 2006 National Health and Nutrition Survey and compared health care access and biological health outcomes, specifically glycosylated haemoglobin (HbA1c) levels, among adults with diabetes who were enrolled in the Seguro Popular (treatment group) and those who had no health insurance (control group). Standard propensity score matching was used to create a highly comparable control group.
Findings
Adults with diabetes who were enrolled in the Seguro Popular had significantly more access than comparable uninsured adults to some type of blood glucose control test (by a difference of 9.5 percentage points; 95% confidence interval, CI: 2.4–16.6) and to insulin injections (3.13 more per week; 95% CI: 0.04–6.22). Those with insurance were also significantly more likely to have appropriately-controlled blood glucose levels (HbA1c ≤ 7%) than their uninsured counterparts (by a difference of 5.6 percentage points; 95% CI: 0.9–10.3). Very poor glucose control (HbA1c > 12%) was found in a significantly smaller proportion of adults in the insured group than in the uninsured group (by a difference of 17.5 percentage points; 95% CI: 6.5–28.5).
Conclusion
The Seguro Popular appears to have improved access to health care and blood glucose control among poor adults with diabetes in Mexico, and it may have had a positive effect on the management of other chronic health conditions, but its long-term effects are yet to be demonstrated. Although the findings are most relevant to Mexico, they may also be applicable to other developing countries seeking to improve health-care coverage for the poor by expanding their public health insurance programmes.
Résumé
Objectif
Analyser l’effet de la couverture par le schéma d’assurance santé publique appelé Seguro Popular (Assurance du peuple) sur l’accès aux ressources de santé, au traitement et au contrôle de la glycémie pour les adultes pauvres et diabétiques du Mexique.
Méthodes
Nous avons analysé des données transversales provenant de l’Enquête nationale sur la santé et la nutrition de 2006 et comparé l’accès aux soins de santé et les résultats biologiques, notamment les taux d’hémoglobine glyquée (HbA1c), chez des adultes diabétiques bénéficiant de Seguro Popular (groupe traité) et chez des adultes diabétiques dépourvus d’assurance santé (groupe témoin). On a fait appel à l’appariement par scores de propension standard pour constituer un groupe témoin hautement comparable.
Résultats
Les adultes diabétiques bénéficiant de Seguro Popular disposaient d’un accès significativement plus important que les adultes comparables non assurés à certains types de contrôles de la glycémie (différence de 9,5 points de pourcentage ; intervalle de confiance à 95 %, IC : 2,4-16,6) et aux injections d’insuline (3,13 de plus par semaine ; IC à 95 % : 0,04-6,22). Les individus assurés avaient une probabilité significativement plus élevée de présenter une glycémie correctement contrôlée (HbA1c ≤ 7%) que leurs homologues non assurés (différence de 5,6 points de pourcentage ; IC à 95 % : 0,9-10,3). On a relevé une proportion significativement plus faible d’adultes présentant un contrôle de la glycémie très insatisfaisant (HbA1c > 12 %) dans le groupe assuré que dans le groupe non assuré (différence de 17,5 points de pourcentage ; IC à 95 % : 6,5-28,5).
Conclusion
L’assurance Seguro Popular semble avoir amélioré l’accès aux soins de santé et au contrôle de la glycémie pour les adultes pauvres et diabétiques du Mexique et pourrait avoir eu un effet positif sur la prise en charge d’autres maladies chroniques. Néanmoins, ses effets à long terme restent à démontrer. Si ces résultats concernent principalement le Mexique, ils peuvent aussi être applicables à d’autres pays en développement désireux d’améliorer la couverture des plus démunis par les soins de santé à travers l’élargissement de leurs programmes d’assurance santé publique.
Resumen
Objetivo
Analizar los efectos de la cobertura por el plan de seguro médico público conocido como Seguro Popular en el acceso a los recursos de salud y el tratamiento y control de la glucemia entre los adultos pobres con diabetes en México.
Métodos
Analizamos datos transversales de la Encuesta Nacional de Salud y Nutrición de 2006 a fin de comparar el acceso a la atención de salud y el valor de variables biológicas, concretamente de los niveles de glucohemoglobina (HbA1c), en adultos con diabetes beneficiarios del Seguro Popular (grupo de tratamiento) y en una población similar que carecía de seguro de enfermedad (grupo control). Se utilizó el método estándar de apareamiento según propensión para crear un grupo control altamente comparable.
Resultados
Los adultos con diabetes beneficiarios del Seguro Popular disfrutaron de un acceso significativamente mayor que los adultos no asegurados comparables a algún tipo de prueba de control de la glucemia (diferencia de 9,5 puntos porcentuales, con un intervalo de confianza, IC, del 95% de 2,4–16,6) y a inyecciones de insulina (3,13 más por semana; IC95%: 0,04–6,22). Los acogidos al seguro tenían también una mayor probabilidad de presentar una glucemia bien controlada (HbA1c ≤ 7%) que sus homólogos no asegurados (diferencia de 5,6 puntos porcentuales; IC95%: 0,9–10,3). En el grupo asegurado se observó que la proporción de adultos con un control muy deficiente de la glucosa (HbA1c > 12%) era significativamente inferior a la hallada en el grupo no asegurado (diferencia de 17,5 puntos porcentuales; IC95%: 6,5–28,5).
Conclusión
El Seguro Popular parece haber mejorado el acceso a la atención de salud y el control de la glucemia entre los adultos pobres con diabetes de México, y puede haber tenido un efecto positivo en el tratamiento de otras dolencias crónicas, pero quedan por demostrar sus efectos a largo plazo. Aunque los resultados son de especial interés para México, posiblemente pueden aplicarse también a otros países en desarrollo que aspiran a mejorar la cobertura de atención sanitaria de la población pobre ampliando sus programas de seguro médico público.
ملخص
الهدف
تحليل أثر إدراج نظام التأمين الصحي العمومي المعروف باسم «التأمين الشعبي» على الوصول إلى الموارد الصحية ومعالجة وضبط سكر الدم بين البالغين الفقراء من السكريين في المكسيك.
الطريقة
حلل الباحثون معطيات المقطع العرضي للمسح الوطني للصحة والتغذية 2006 وقارنوا عملية الوصول للرعاية الصحية والحصائل الصحية البيولوجية، ولاسيما مستويات الهيموغلوبين الغليكوزي HbAc1 لدى البالغين السكريين المدرجين ضمن نظام “التأمين الشعبي” (مجموعة المعالجة) وبين غير المدرجين ضمن ذلك النظام (مجموعة الشواهد). واستخدموا حرزاً معيارياً للمواءمة لإنشاء مجموعة شواهد قابلة للمقارنة بدرجة عالية.
الموجودات
يتمتع البالغون السكريون المدرجون ضمن نظام “التأمين الشعبي” بوصول لبعض أنماط اختبارات ضبط سكر الدم أكثر مما يتمتع به غير المدرجين بالنظام (والفرق يصل إلى 9.5 بالمئة من النقاط بمجال ثقة 95%: 2.4 – 16.6) ولحقن الإنسولين (3.13 أكثر لكل أسبوع بمجال ثقة 95%: 0.04 – 6.22). ويغلب أن تكون مستويات ضبط الغلوكوز الظاهرية (مستوى HbAc1 يعادل أو يقل عن 7%)، أكثر لدى المتمتعين بالتأمين مما لدى أقرانهم من غير المتمتعين بالتأمين (بفارق 5.6 من النقاط المئوية، بمجال موثوقية 95%: 0.9 – 10.3). ووجدت مستويات الضبط السئ جدا لغلوكوز الدم (HbAc1 أكثر من 12%) بنسبة أقل كثيرا لدى مجموعة البالغين المتمتعين بالتأمين، مما لدى مجموعة غير المتمتعين بالتأمين (بفارق 17.5 من النقاط المئوية وبمجال موثوقية 9.5% : 6.5 – 28.5).
الاستنتاج
لقد حسن نظام التأمين الشعبي من إمكانية الوصول للرعاية الصحية وضبط غلوكوز الدم بين البالغين الفقراء السكريين في المكسيك، وقد يكون له تأثير إيجابي على تدبير الحالات الصحية المزمنة الأخرى، إلا أن تأثيراته البعيدة الأمد لم تتضح بعد. ورغم أن الموجودات ذات علاقة أكثر بالمكسيك، فإنها قد تنطبق على البلدان النامية الأخرى التي تبحث عن تحسين التغطية بالرعاية الصحية للفقراء من خلال توسيع برامج التأمين الصحي العمومي فيها.
Introduction
Lack of health insurance can deprive the poor of access to services or put them at risk of financial hardship. To protect the poor against excessive health expenditures, many countries have implemented mechanisms such as community-based health insurance,1,2 national health insurance3–6 and targeted public health insurance.7,8
Mexico has multiple health insurance providers. The Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado [State Employee’s Social Security and Social Services Institute, ISSSTE] provides coverage for government employees and the Instituto Mexicano del Seguro Social [Mexican Social Security Institute, IMSS] covers for private-sector employees. By 2001, however, nearly half of the Mexican working-age population had no health insurance.9 The Seguro Popular [People’s Insurance], launched that year, represented a major effort to protect the working-age population against steep health-care costs. Enrolment in the Seguro Popular is not dependent on health status or pre-existing illness, there is no co-payment in accordance with the type of health care received, and family contributions are determined solely by ability to pay.10 Medical interventions are offered mainly through the public health network.
The Seguro Popular, which covers health care for many diseases, including cancer, asthma, anaemia, pneumonia and diabetes,11 was implemented gradually between 2001 and 2005, but only in communities with health units having accreditation, that is, the proven capacity – medical resources, personnel and infrastructure, etc. – to provide the health interventions covered by the Seguro Popular. Thus, during the implementation phase, people chose to enrol based largely on programme availability at the regional level, and this, in turn, was determined by health infrastructure capacity.
Background
According to WHO estimates, by 2030, approximately 366 million adults will have diabetes (type 2 in over 90% of the cases), and 75% of these adults will be living in developing countries.12 In Mexico, type 2 diabetes is the leading cause of death among adults, according to the 2007 National Death Registry.13 Data from the 2005–2006 cross-sectional Encuesta Nacional de Salud y Nutrición [National Health and Nutrition Survey, ENSANUT] showed that 7.1% of adults reported having been diagnosed with type 2 diabetes by a physician.14 Test results based on fasting blood serum samples collected for the ENSANUT suggest that a large number of Mexican adults have undiagnosed diabetes and that the estimated overall prevalence of diabetes is about 14%. (S Villalpando, personal communication).
Diabetes requires life-long treatment and periodic clinical follow-up. Health care is needed on a regular basis to attain good control of blood glucose levels, blood pressure, blood lipids and body weight; to reduce or delay the onset of complications, and to delay or prevent death from the disease. Periodic health-care visits (three to four per year, according to Mexican and international guidelines) should include laboratory testing to assess the need for more aggressive therapy.15,16
Lifestyle intervention, including a healthy diet and physical activity, is the first line of treatment for diabetes, but the American Diabetes Association and the European Association for the Study of Diabetes17 recommend aggressive treatment of the disease, including early initiation of insulin therapy. Diabetes management also involves close monitoring for chronic complications affecting the kidneys, eyes or feet.15,16
In Mexico, the total annual cost of managing diabetes and its complications in 2000 was estimated at over 15 billion United States dollars (US$), of which approximately US$ 765 million represented direct medication costs.18 In that same year, an estimated 44% of adults who had been previously diagnosed with diabetes in Mexico reported having no health insurance.19 Diabetic patients who lack health insurance are less likely to adhere to medical care.20 The Seguro Popular was intended to improve the treatment options and laboratory tests available to Mexicans with diabetes, as well as to ensure their access to appropriate medication.
Previous empirical research suggests that people who are Seguro Popular beneficiaries have better access to health care than those who are not. Bleich et al.21 found that hypertensive adults enrolled in the Seguro Popular were more likely to be treated for high blood pressure and to attain good control. Sosa-Rubí et al.22 found that pregnant women enrolled in the Seguro Popular were more likely to receive formal obstetric care.
This paper examines the effect of Seguro Popular enrolment on access to health care, specifically health resources (medical visits, laboratory tests and use of medication, including insulin injections), and on blood glucose control (as measured by glycosylated haemoglobin, HbA1c, the gold standard for blood glucose control surveillance).15,16 An HbA1c test is required at least twice a year for diabetes patients with stable blood glucose and at least four times a year for patients without stable blood glucose or for those who have just begun or changed therapy.16 To reduce confounding in the observational data analysed, we used propensity score matching to estimate the average treatment effect, with “treatment” defined as enrolment in the Seguro Popular.
Our working hypothesis was that enrolment in the Seguro Popular improves access to treatment and health outcomes among patients with diabetes. This hypothesis is consistent with the stated goal of the Seguro Popular: to improve access to qualified and specialized health services among poor and uninsured Mexicans.
Methods
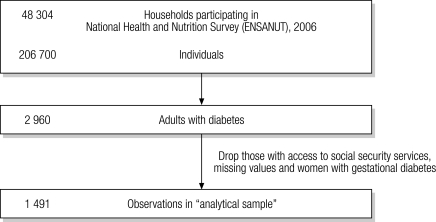
From the 2005–2006 ENSANUT we obtained data on treatment, medical care and biological outcomes in diabetes patients.14 The ENSANUT is a nationally representative survey that in 2005–2006 had a sample of 48 304 households and 206 700 individuals. We selected a subsample of 2960 adults with diabetes (i.e. adults who had been diagnosed with diabetes by a physician or who reported being under treatment for diabetes). After we excluded pregnant women with hyperglycaemia (assumed to have gestational diabetes), adults with access to social security services, and responses with missing data, our final sample for analysis included 1491 adults (Fig. 1).
Fig. 1.
Selection of participants: a flow diagram
Adults (aged 20–80 years) provided the following information: number of visits to physicians for diabetes control; frequency and type of treatment (diet, alternative medicines or standard drug therapy, such as insulin and oral hypoglycaemic agents); and access to laboratory tests, including testing frequency. In addition, a random subsample of patients (n = 1115) was selected for HbA1c testing.
Variables
We analysed access outcomes and biological outcomes. The first included access to laboratory tests; four or more yearly visits to a physician for diabetes control; treatment with any drug, including insulin; number of weekly insulin injections (if on insulin); and number of blood glucose control tests per month.
Biological outcomes were based on blood glucose control, as determined by HbA1c levels. We constructed two indicators of glucose control on the basis of recommended levels of HbA1c. Patients were initially categorized as having “appropriate glucose control” (HbA1c ≤ 7%) or “poor glucose control” (HbA1c > 7%) and were then further classified in accordance with the more extreme values: “very poor glucose control” (HbA1c > 12%) or “appropriate and poor glucose control” (HbA1c ≤ 12%). Patients in the “very poor glucose control” category were those having the poorest outcomes and the highest risk of premature death and complications.23
For analysis, health insurance status, as reported by surveyed individuals, was the exposure variable. We compared individuals enrolled in the Seguro Popular (“treatment” category) with individuals who reported having no insurance (control category).
We assessed characteristics of the individual, the household and the state as treatment predictors: for the individual, age, sex, education and ethnicity; for the household, family assets (as a proxy for family wealth) and rural or urban residential area; for the state, the general region of the country (north, east central, west central and south–southeast). We also considered potential confounders (e.g. using body mass index, BMI, as a proxy for lifestyle) and time since diabetes was diagnosed.
Finally, data from Mexico’s 2005 Registro Nacional de Infraestructura en Salud [National Registry of Health Infrastructure] was added to determine whether the availability of health professionals (i.e. the numbers of physicians and nurses) and health units per 1000 population modified the treatment effect.24 To estimate the number of physicians, nurses and health units per 1000 population, we used 2005 census data for municipalities generated by Mexico’s National Geographical Institute.25
Statistical methods
Because enrolment in the Seguro Popular is voluntary, health insurance status is not randomly allocated and the data may be subject to self-selection bias. To reduce this bias, we used standard propensity score matching. We first constructed a propensity score that estimated the probability of enrolment in the Seguro Popular given a set of predictors, and we then created a control group (uninsured) and a treatment group (insured) having similar propensity scores. We used a logistic regression model to estimate the conditional probability of Seguro Popular enrolment, given a set of covariates (X). Nearest neighbour matching allowed us to match insured and uninsured individuals with similar propensity scores.26,27
If outcomes are assumed to be independent of programme participation after controlling for propensity score, the average treatment effect is:
| ATT = E [E [Y1| SPi = 1, p(Xi)] – E [Y0| SPi = 0, p(Xi)]] |
where SPi = 1 if the individual is enrolled in the Seguro Popular and SPi = 0 if not; and where the expectations [E] are conditional on treatment status, as represented by the vertical bar. ATT is the difference between the mean outcomes for those treated (Y1) and for those untreated (Y0), after controlling for observed variables with the propensity score p(Xi).
To ensure comparability, we tested the balancing property: pre-treatment covariates did not differ statistically between Seguro Popular enrolees and people without health insurance. 28 We followed the algorithm suggested by Dehejia and Wahba29,30 to find the best model specification. The method involved the use of different specifications until we obtained a balanced distribution of the following covariates: sex, age, family asset index, residence area, residence region, ethnicity, education and marital status. Furthermore, we estimated the percentage bias reduction by calculating the difference in absolute bias between treated and control groups as a percentage of the square root of the average of the sample variances.31
We performed sensitivity analysis to test the association of HbA1c results with the potential lifestyle confounders (using BMI as a proxy for lifestyle) and the time since diabetes was first diagnosed. We also checked the independent effect of Seguro Popular enrolment and of health professional availability on the coverage of diabetes treatment and control. This involved estimating a multivariate model using matched data for two outcomes: regular use of any blood glucose control test and proportion of patients with “very poor glucose control”. We adjusted the multivariate model with clustering for the potential effect modifier of health professional availability, as determined by the number of physicians, nurses and health units in a given location compared with the median for the entire municipality.
Results
Table 1 presents the sociodemographic characteristics of the uninsured population and of the population enrolled in the Seguro Popular. The table shows both raw (unmatched) and matched means. In the unmatched sample, adults enrolled in the Seguro Popular had less formal education and fewer family assets but were more likely to be female and married and to live in rural areas and in Mexico’s West central and South–southeast regions, than uninsured adults. In the matched samples, the differences between Seguro Popular enrolees and uninsured individuals (i.e. the bias)31 were considerably smaller for most of the variables. The t test for some predictors still showed statistical significance for the entire sample; however, for the propensity score estimation, the t test showed statistically insignificant differences for the covariables at each of the seven propensity score blocks (results not shown).
Table 1. Sociodemographic characteristics of adults with diabetes enrolled in the Seguro Popular and of uninsured adults, Mexico, 2006.
| Unmatched samples |
Matched samples |
Percentage reduction in bias | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Seguro Popularan = 430 | Uninsuredan = 1061 | t-test P‑value | Seguro Popularan = 425 | Uninsuredan = 1029 | t-test P‑value | |||||||||
| Individual characteristic | ||||||||||||||
| Sex | ||||||||||||||
| Maleb | 30.9 | 40.1 | ||||||||||||
| Female | 69.1 | 59.9 | 0.001 | 68.9 | 69.9 | 0.115 | 89.1 | |||||||
| Age, in years | ||||||||||||||
| 20–39 | 17.5 | 16.3 | 0.558 | 17.2 | 15.1 | 0.709 | –69.0 | |||||||
| 40–59 | 50.0 | 48.2 | 0.518 | 50.12 | 55.3 | 0.002 | –179 | |||||||
| 60–79 | 29.4 | 31.8 | 0.378 | 29.7 | 26.6 | 0.109 | –30.7 | |||||||
| ≥ 80b | 3.0 | 3.9 | ||||||||||||
| Marital status | ||||||||||||||
| Married | 73.1 | 64.8 | 0.002 | 72.9 | 80.2 | 0.000 | 12.5 | |||||||
| Unmarriedb | 26.7 | 35.3 | ||||||||||||
| Education | ||||||||||||||
| Noneb | 21.4 | 21.6 | ||||||||||||
| Primary | 66.8 | 57.7 | 0.001 | 66.8 | 64.2 | 0.018 | 72.5 | |||||||
| Secondary | 8.7 | 12.6 | 0.032 | 8.7 | 8.5 | 0.166 | 94.0 | |||||||
| High school/college | 2.8 | 8.4 | 0.000 | 2.8 | 3.0 | 0.000 | 95.8 | |||||||
| Ethnicity (self-identified) | ||||||||||||||
| Indigenous | 23.8 | 23.3 | 0.830 | 24.1 | 26.8 | 0.016 | –442 | |||||||
| Not indigenousb | 76.3 | 76.7 | ||||||||||||
| Family assets | ||||||||||||||
| Mean (asset index)c | –0.504 | –0.235 | 0.000 | –0.495 | –0.433 | 0.000 | 76.9 | |||||||
| Regional characteristic | ||||||||||||||
| Area of residence | ||||||||||||||
| Metropolitan | 20.9 | 42.0 | 0.000 | 20.9 | 22.1 | 0.000 | 94.5 | |||||||
| Urban | 39.9 | 32.3 | 0.005 | 40.0 | 37.6 | 0.049 | 69.4 | |||||||
| Ruralb | 39.4 | 25.8 | ||||||||||||
| Region of residence | ||||||||||||||
| North | 16.4 | 19.7 | 0.136 | 16.5 | 13.4 | 0.001 | 8.4 | |||||||
| East central | 15.7 | 26.9 | 0.000 | 15.8 | 15.1 | 0.002 | 93.7 | |||||||
| West central | 39.6 | 26.3 | 0.000 | 39.5 | 39.8 | 0.000 | 98.3 | |||||||
| South–southeastb | 27.9 | 26.9 | ||||||||||||
a Values are percentages, unless otherwise noted; percentages may not add up to 100% due to rounding error. b Omitted (reference) category. Table reports nearest neighbour matching with common support. The t test for each covariable may show statistical significance for the variable evaluated for the entire sample; however, for the propensity score, t tests for insignificant differences were conducted at each propensity score block (results not shown). The percentage of bias reduction reports reduction in absolute bias between the treatment category (Seguro Popular enrollees) and the control category (the uninsured) as a percentage of the square root of the average of the sample variances in the treated and non-treated groups.31 c The asset index is based upon household infrastructure, building materials, and ownership of certain durable assets, as a proxy for household’s wealth. It may be negative because it is constructed with principal components analysis. A more negative index indicates lower household wealth. Estimations based on data from the 2006 Encuesta Nacional de Salud y Nutrición.14
Table 2 shows the logistic regression model for propensity scores. In the model, females and married people were more likely to be enrolled in the Seguro Popular, as were adults with diabetes who had fewer assets or who lived in rural areas or in the west central region.
Table 2. Logistic modela of the propensity score to estimate the effect of Seguro Popular enrolment on diabetes treatment and control in Mexico, 2006 (n = 1479).
| Variable | Probability of enrolment in the Seguro Popular |
||||
|---|---|---|---|---|---|
| Coefficient | Z-value | P-value | |||
| Individual characteristic | |||||
| Sex | |||||
| Female | 0.43 | 3.27 | 0.001 | ||
| Age, in years | |||||
| 20–39 | 0.44 | 1.16 | 0.246 | ||
| 40–59 | 0.28 | 0.78 | 0.434 | ||
| 60–79 | 0.11 | 0.3 | 0.763 | ||
| Marital status | |||||
| Married | 0.43 | 3.06 | 0.002 | ||
| Education | |||||
| Primary school | 0.18 | 1.15 | 0.249 | ||
| Secondary school | –0.20 | –0.77 | 0.444 | ||
| High school/university | –0.61 | –1.67 | 0.094 | ||
| Ethnicity | |||||
| Indigenous | –0.13 | –0.88 | 0.381 | ||
| Household characteristic | |||||
| Family assets | –0.26 | –3.41 | 0.001 | ||
| Regional characteristic | |||||
| Area of residence | |||||
| Metropolitan | –0.03 | –0.18 | 0.860 | ||
| Urban | –0.80 | –4.77 | 0.000 | ||
| Region of residence | |||||
| North | 0.23 | 1.19 | 0.233 | ||
| East-central | –0.43 | –2.39 | 0.017 | ||
| West-central | 0.48 | 3.1 | 0.002 | ||
a Log-likelihood ratio test, χ² (degrees of freedom): 139.15 (15); probability > χ² = 0.000.
Table 3 presents differences in health outcomes between individuals with and without insurance. Those enrolled in the Seguro Popular reported, on average, greater access to blood glucose control tests of any type (including urine and capillary blood reactive strips) and more blood glucose control tests per month. After propensity matching, these differences became significant. The proportion of adults with diabetes who were under insulin treatment was similar between groups, and matched differences were not significant. However, among adults who used insulin, those enrolled in the Seguro Popular received, on average, 3.13 more insulin injections per week than those without insurance. Uninsured insulin users received a median of seven insulin injections per week (probably one injection per day), while insured insulin users received a median of 14 insulin injections per week (probably two injections per day). In addition, those enrolled in the Seguro Popular had more blood glucose tests per month and a greater likelihood of having visited a physician four times or more per year.
Table 3. Average effect of enrolment in the Seguro Popular in terms of diabetes treatment and control, Mexico, 2006a.
| Outcome variable | Mean |
Unmatched |
Matched |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Seguro Popular | Uninsured | Unmatched differenceb | t-value | P-value | Matched ATTc (95% CI) | t-value | P-value | ||||||||
| Health care access outcome | |||||||||||||||
| Regular use of any blood glucose control testd | 0.809 | 0.754 | 0.055 | 2.300 | *** | 0.095 (0.020‑0.161) | 2.626 | *** | |||||||
| No. of insulin users | 0.0415 | 0.0479 | –0.0064 | –0.504 | NS | 0.001 (–0.032–0.034) | 0.066 | NS | |||||||
| No. of insulin shots per week among insulin users | 12.6 | 8.99 | 3.600 | 2.922 | *** | 3.133 (0.04–6.22) | 1.988 | ** | |||||||
| No. of blood sugar control tests per month | 1.02 | 0.87 | 0.144 | 0.825 | NS | 0.142 (0.024–0.260) | 2.371 | *** | |||||||
| Four or more physician visits per year | 0.918 | 0.811 | 0.107 | 4.795 | *** | 0.093 (0.032–0.154) | 3.019 | *** | |||||||
| Biological outcome | |||||||||||||||
| Proportion of diabetics with appropriate glucose controle | 0.089 | 0.074 | 0.015 | 0.624 | NS | 0.056 (0.009–0.103) | 2.316 | *** | |||||||
| Proportion of diabetics with very poor glucose controlf | 0.367 | 0.462 | –0.095 | –2.122 | *** | –0.175 (–0.285–0.065) | –3.159 | *** | |||||||
**P < 0.05; ***P < 0.01, using t tests, of mean differences between treatment and control (unmatched and matched) groups. ATT, average treatment effect on the treated; CI, confidence interval; NS, not significant. a The data are not weighted. b This is the raw difference between unmatched samples, or the difference between the mean observed in Seguro Popular enrollees and the mean observed in the uninsured population. c The ATT is based on the differences in mean outcome for propensity-score-matched individuals using nearest neighbour matching. d Tests may include urine or capillary blood reactive strips, blood glucose, or glycosylated haemoglobin (HbA1c). e Appropriate glucose control (HbA1c ≤ 7%) compared with poor glucose control (HbA1c > 7%). f Very poor glucose control (HbA1c > 12%) compared with normal and poor glucose control (HbA1c ≤ 12%).
Finally, Seguro Popular enrolees had appropriate glucose control, based on HbA1c levels, in greater proportion than uninsured patients (8.9% versus 7.4%, respectively). Conversely, uninsured patients had very poor glucose control in greater proportion than Seguro Popular enrolees (46.2% versus 36.7%, respectively). On the basis of propensity score matching, the average treatment effect was an increase of 5.6 percentage points in those with appropriate control and a decrease of 17.5 percentage points in those with very poor glucose control. These differences are of obvious clinical importance.
In sensitivity analyses, we examined whether the number of physicians, nurses or health units per 1000 population altered the model in terms of the regular use of some type of blood glucose control test. After adjustment for Seguro Popular enrolment, no odds ratio (OR) showed statistical significance. However, the interaction term that showed a greater availability of physicians among Seguro Popular enrolees was significant and positive. People insured through the Seguro Popular and who lived in municipalities with an above-median number of physicians per 1000 population had considerably higher odds of regularly using any glucose control test (OR: 15.85; z-statistic: 2.62).
We then analysed the interaction between the number of physicians, nurses and health units per 1000 population and the “very poor glucose control” indicator. Municipalities with more health units per 1000 population had a greater likelihood of being the place of residence of those with “very poor glucose control” (OR: 3.17; z‑statistic: 2.08). Similarly, Seguro Popular enrolees and people living in areas with more nurses per 1000 population had a greater likelihood of not having “very poor glucose control” (OR: 4.59; z-statistic: 1.75).
Sensitivity analyses showed that the association between potential confounders (BMI as proxy for lifestyle and time since diabetes first diagnosed) and health-care outcomes was not significant. Such confounders were significantly associated with the biological outcomes but did not substantially modify the results presented already. The additional covariates showed no significance in the propensity score model.
Discussion
The findings of this study suggest that the Seguro Popular has improved both access to health services and biological health outcomes among adults with diabetes. Over the past 20 years, various countries in Latin America – Argentina, Brazil, Chile and Colombia – have implemented health insurance reform to improve the coverage of marginalized groups.32 The current study demonstrates the success of an insurance programme targeted to the poor in Mexico. Its results may be relevant for other populations living in a similar socioeconomic setting and may help to shape programmes for improving access to health services and health status among the poor.
Although adults with diabetes who were Seguro Popular enrolees had better access to health care and better blood glucose level control, the effect of enrolment on biological outcomes was modest: a large proportion of both the insured and uninsured remained in the “very poor glucose control” category. It is too early to determine whether the Seguro Popular will reduce premature deaths from the chronic complications of diabetes, but continued emphasis on quality of care and treatment will be necessary to meet this long-term goal.
Limitations
This study has limitations. It is cross-sectional, hence it captures only a single point in time. Responses to questions about the past are subject to recall bias. Furthermore, self-reported outcomes, such as the number of visits to a physician, are subject to reporting bias. The biological tests performed provide more objective measures. Although we controlled for many variables that influence insurance choice (including age, sex, marital status and residential region), other factors (e.g. genetic or environmental) could also make an individual more prone to diabetes and less likely to enrol in the Seguro Popular. We also assumed (as is common in studies with propensity score matching) that unobservable components could be ignored.
Health insurance for the poor is a relatively new concept and its effect has not been widely evaluated yet. The results provided here are among the very few based on an assessment of individual health status indicators. As the Seguro Popular programme is quite new, these are early results; effects over the longer term should be the subject of future research. ■
Acknowledgements
We thank Heleen Vermandere for her research assistance and the two anonymous reviewers for their helpful comments and constructive suggestions.
Footnotes
Funding: This work was initially carried out within the context of Mexico’s National Institute of Public Health’s evaluation of the Seguro Popular commissioned by the Health Ministry of Mexico (SSA).
Competing interests: None declared.
References
- 1.Ranson MK. Reduction of catastrophic health care expenditures by a community-based health insurance scheme in Gujarat, India: current experiences and challenges. Bull World Health Organ. 2002;80:613–21. [PMC free article] [PubMed] [Google Scholar]
- 2.Wang H, Yip W, Zhang L, Wang L, Hsiao W. Community-based health insurance in poor rural China: the distribution of net benefits. Health Policy Plan. 2005;20:366–74. doi: 10.1093/heapol/czi045. [DOI] [PubMed] [Google Scholar]
- 3.Chu TB, Liu TC, Chen CS, Tsai YW, Chiu WT. Household out-of-pocket medical expenditures and national health insurance in Taiwan: income and regional inequality. BMC Health Serv Res. 2005;5:60. doi: 10.1186/1472-6963-5-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Obermann K, Jowett MR, Alcantara MO, Banzon EP, Bodart C. Social health insurance in a developing country: the case of the Philippines. Soc Sci Med. 2006;62:3177–85. doi: 10.1016/j.socscimed.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 5.Wagstaff A, van Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993-1998. Health Econ. 2003;12:921–34. doi: 10.1002/hec.776. [DOI] [PubMed] [Google Scholar]
- 6.Limwattananon S, Tangcharoensathien V, Prakongsai P. Catastrophic and poverty impacts of health payments: results from national household surveys in Thailand. Bull World Health Organ. 2007;85:600–6. doi: 10.2471/BLT.06.033720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagstaff A, Lindelowb M, Jun G, Ling X, Juncheng Q. Extending health insurance to the rural population: an impact evaluation of China’ s new cooperative medical scheme (The World Bank Policy Research Working Paper Series 4150). Washington, DC: The World Bank; 2007. [DOI] [PubMed]
- 8.Frenk J, González-Pier E, Gómez-Dantés O, Lezana MA, Knaul FM. Comprehensive reform to improve health system performance in Mexico. Lancet. 2006;368:1524–34. doi: 10.1016/S0140-6736(06)69564-0. [DOI] [PubMed] [Google Scholar]
- 9.Gakidou E, Lozano R, González-Pier E, Abbott-Klafter J, Barofsky JT, Bryson-Cahn C, et al. Assessing the effect of the 2001-06 Mexican health reform: an interim report card. Lancet. 2006;368:1920–35. doi: 10.1016/S0140-6736(06)69568-8. [DOI] [PubMed] [Google Scholar]
- 10.Frenk J, Sepúlveda J, Gómez-Dantés O, Knaul F. Evidence-based health policy: three generations of reform in Mexico. Lancet. 2003;362:1667–71. doi: 10.1016/S0140-6736(03)14803-9. [DOI] [PubMed] [Google Scholar]
- 11.Popular S. Secretaría de Salud [Internet]. Mexico City: SSA. Catálogo universal de servicios de salud 2008. Available from: http://www.seguro-popular.salud.gob.mx/images/contenidos/Normateca/Spss/causes_2009.pdf [accessed on 16 June 2009].
- 12.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 13.Sistema Nacional de Información en Salud. Secretaría de Salud [Internet]. Mexico City: SSA; National Death Registry 2007. Available from: http://sinais.salud.gob.mx/descargas/xls/diezprincausasmort2007_CNEGySR.xls [accessed on 7 April 2009].
- 14.Olaiz-Fernández G, Rivera-Dommarco J, Shamah-Levy T, Rojas R, Villalpando-Hernández S, Hernández-Avila M, et al. Encuesta Nacional de Salud y Nutrición 2006. Cuernavaca, Mexico: Instituto Nacional de Salud Pública; 2006. [Google Scholar]
- 15.Mexico, Secretaría de Salud. Modificación de la norma oficial mexicana NOM-015-SSAA2-1994 para la prevención, tratamiento y control de la diabetes mellitus en la atención primaria Mexico City: SS; 2001.
- 16.American Diabetes Association Standards of medical care in diabetes – 2007. Diabetes Care. 2007;30(Suppl 1):S4–41. doi: 10.2337/dc07-S004. [DOI] [PubMed] [Google Scholar]
- 17.Nathan DM, Buse JB, Davidson MB, Heine RJ, Holman RR, Sherwin R, et al. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy; a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006;29:1963–72. doi: 10.2337/dc06-9912. [DOI] [PubMed] [Google Scholar]
- 18.Barcelo A, Aedo C, Rajpathak S, Robles S. The cost of diabetes in Latin America and the Caribbean. Bull World Health Organ. 2003;81:19–27. [PMC free article] [PubMed] [Google Scholar]
- 19.Olaiz-Fernández G, Rojas R, Aguilar-Salinas CA, Rauda J, Villalpando S. Diabetes mellitus en adultos mexicanos: Resultados de la Encuesta Nacional de Salud 2000. Salud Publica Mex. 2007;49(S3):s331–7. [Google Scholar]
- 20.Lerman-Garber I. La atención del paciente más allá del primer nivel de atención. Salud Publica Mex. 2007;49:99–103. [Google Scholar]
- 21.Bleich SN, Cutler DM, Adams AS, Lozano R, Murray CJ. Impact of insurance and supply of health professionals on coverage of treatment for hypertension in Mexico: population based study. BMJ. 2007;335:875. doi: 10.1136/bmj.39350.617616.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sosa-Rubi SG, Galarraga O, Harris JE. Heterogeneous impact of the “Seguro Popular” program on the utilization of obstetrical services in Mexico, 2001. A multinomial probit model with a discrete endogenous variable. J Health Econ. 2009;28:20–34. doi: 10.1016/j.jhealeco.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–12. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mexico, Secretaría de Salud. Subsistema de Información de Equipamiento, Recursos Humanos e Infraestructura para la Atención de la Salud (SINERHIAS) Mexico City: SSA; 2005.
- 25.Instituto Nacional de Estadística. Geografía e Informática. Conteo de población y vivienda 2005 Mexico, DF: INEGI; 2005. [Google Scholar]
- 26.Becker S, Ichino A. The estimation of average treatment effects based on propensity scores. Stata J. 2002;2:358–77. [Google Scholar]
- 27.Leuven E, Sianesi B. Psmatch2: Stata module to perform full Mahalanobis and propensity score matching, common support graphing, and covariate imbalance testing, 2003 [Internet site]. Available from: http://ideas.repec.org/c/boc/bocode/s432001.html [accessed on 7 April 2009].
- 28.Rosenbaum P, Rubin D. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. doi: 10.1093/biomet/70.1.41. [DOI] [Google Scholar]
- 29.Dehejia RH, Wahba S. Propensity score-matching methods for nonexperimental causal studies. Rev Econ Stat. 2002;84:151–61. doi: 10.1162/003465302317331982. [DOI] [Google Scholar]
- 30.Dehejia RH, Wahba S. Causal effects in nonexperimental studies: re-evaluating the evaluation of training programs. J Am Stat Assoc. 1999;94:1053–62. doi: 10.2307/2669919. [DOI] [Google Scholar]
- 31.Rosenbaum P, Rubin D. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33–8. doi: 10.2307/2683903. [DOI] [Google Scholar]
- 32.Jack W. Public intervention in health insurance markets: theory and four examples from Latin America. World Bank Res Obs. 2002;17:67–88. doi: 10.1093/wbro/17.1.67. [DOI] [Google Scholar]