Abstract
Although the nature and scope of addictive disease are commonly reported in the lay press, the problem of physician addiction has largely escaped the public's attention. This is not due to physician immunity from the problem, because physicians have been shown to have addiction at a rate similar to or higher than that of the general population. Additionally, physicians' addictive disease (when compared with the general public) is typically advanced before identification and intervention. This delay in diagnosis relates to physicians' tendency to protect their workplace performance and image well beyond the time when their life outside of work has deteriorated and become chaotic. We provide an overview of the scope and risks of physician addiction, the challenges of recognition and intervention, the treatment of the addicted physician, the ethical and legal implications of an addicted physician returning to the workplace, and their monitored aftercare. It is critical that written policies for dealing with workplace addiction are in place at every employment venue and that they are followed to minimize risk of an adverse medical or legal outcome and to provide appropriate care to the addicted physician.
Approximately 10% to 12% of physicians will develop a substance use disorder during their careers, a rate similar to or exceeding that of the general population.1,2 Although physicians' elevated social status brings many tangible and intangible rewards, it also has an isolating effect when they are confronted with a disease such as addiction, which has a social stigma. This isolation can lead to disastrous consequences, both in delaying the recognition of and in intervening in the disease process, as well as in the attendant risk of death by inadvertent overdose or suicide.3
Further causes for delay in diagnosis include fear on the part of the physician that disclosure of an addictive illness might cause loss not only of prestige but also of his or her license to practice medicine and thus livelihood. Additionally, a physician's family members and coworkers will often participate in a “conspiracy of silence” in an effort to protect the family or practice workers from economic ruin by the loss of the physician's job and income.
McLellan et al2 conducted a 5-year longitudinal cohort study of 904 physicians, 87% of whom were male, who were enrolled in 16 state physician health programs (PHPs). Alcohol was the primary drug of abuse in 50.3%, opioids in 35.9%, stimulants in 7.9%, and other substances in 5.9%; 50% reported abuse of multiple substances, 13.9% a history of intravenous drug use, and 17% previous treatment for addiction. The authors found that certain specialties, such as anesthesiology, emergency medicine, and psychiatry, appeared to be overrepresented in these programs relative to their numerical representation in the national physician pool. Indeed, other investigators have suggested that these specialties seem to have a disproportionate propensity toward addiction.4,5 Contributing factors may include stresses of the work, ready access to narcotics and other psychotropic drugs in the workplace, and perhaps a selection bias in the type of physicians who seek these specialties.6
Physicians in different specialties tend to abuse different classes of drugs. For example, although alcohol is the drug of choice for most physicians with addiction, only about 10% of anesthesiologists enter treatment for alcohol addiction. Instead, the vast majority of addicted anesthesiologists are addicted to potent intravenous opioids such as fentanyl and sufentanil. Often, addicted physicians divert these drugs from the workplace, indeed from their individual patients, and losing their job would cut their lifeline to their drug of abuse. Thus, they preserve their work performance above all other aspects of their life, and by the time a physician's addictive illness becomes apparent in the workplace, the rest of his or her social, family, and personal life is in shambles.7
For editorial comment, see page 576
For a colleague who suspects addiction in a peer, the challenges of conclusively identifying and intervening can be daunting and include everything from a concern of “What right do I have to tell them how to live their life?” to a fear of retaliatory litigation. Additionally, the medical licensing boards in many states have included the risk of sanctions if a physician becomes aware of an addictive disease in a colleague and fails to intervene or notify the board or the state's PHP. This aspect will be covered more fully in a later section.
WHAT IF PHYSICIAN ADDICTION IS SUSPECTED?
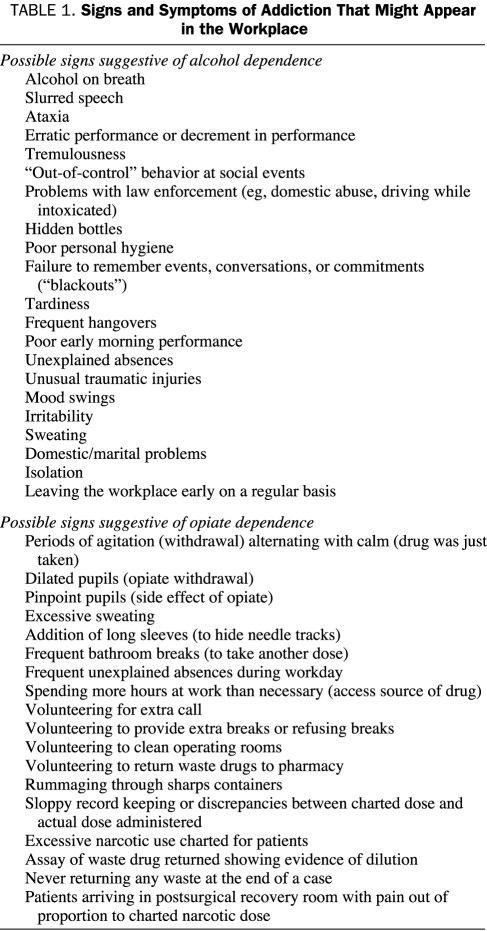
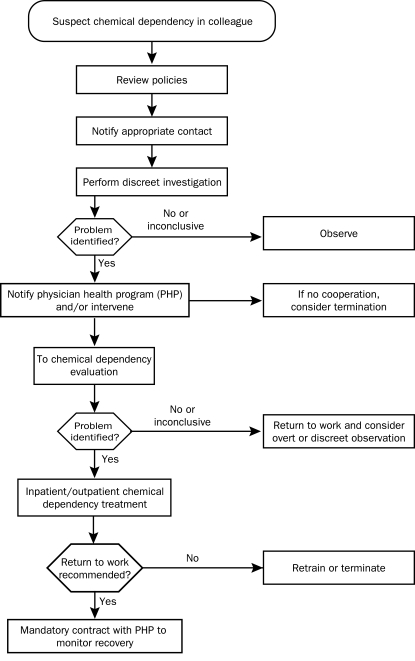
The signs and symptoms of addictive illness range from very subtle to extremely overt (Table 1). Although they might be as obvious as intoxication on duty, with the stereotypical signs of ataxia and dysarthria, the findings in general are far more subtle. Particularly with opioid addiction, the addicted physician may continue to function at a high level, and his or her colleagues have only a hint of a problem because of behavior changes. Although protecting the safety of our (and the addicted physician's) patients is of the utmost importance, the addicted physician who engages in parenteral opioid use has a very real risk of serious morbidity (eg, anoxic brain injury from inadvertent overdose) and death. Thus, rapid confirmation and intervention are necessary if physician addiction is suspected. Unfortunately, decisions must often be made in the face of inconclusive evidence of physician addiction or diversion of drugs for self-use. If an evaluation is delayed until evidence of physician addiction or diversion of drugs is secured “beyond a reasonable doubt,” the risk of a tragic outcome increases. As any intervention that requires an evaluation for chemical dependency does not consist of accusing the individual of a crime—reasonable suspicion of an addictive illness is sufficient.8 In the Figure, we provide a generalized (and greatly oversimplified because it is impossible to include the myriad ways these situations might unfold) approach to a prototypic investigation, intervention, and follow-up of a physician suspected of substance abuse; however, it is essential that each health care organization, regardless of its size, has written policies in place specific to the state laws. Because laws for dealing with these issues vary from state to state, the admittedly simplistic algorithm in the Figure is not sufficiently specific to substitute for a formal written policy for all health care organizations. If organizations fail to formalize in writing their policies, they are at subsequent risk of adverse medical or legal outcomes.
TABLE 1.
Signs and Symptoms of Addiction That Might Appear in the Workplace
FIGURE.
Generalized approach to a prototypic investigation, intervention, and follow-up of a physician suspected of abusing substances.
WHAT DOES INTERVENTION INVOLVE?
Although intervention can have different meanings in different contexts, we define it as the initial confrontation with the suspected addict in an effort to coerce the individual to submit to a formal chemical dependency evaluation by experts. An intervention is one of life's most stressful events, for both the suspected addict and those intervening. It is not to be undertaken casually; rather, it requires preparation and logistical support.9 Above all, the person intervening should never simply approach the suspected addict one-on-one and ask if he or she is addicted or diverting drugs or suggest that he or she stop using or diverting drugs. This strategy is not only pointless as denial is the hallmark of addictive illness, it is also potentially dangerous because the threat to the physician's status, autonomy, security, and financial stability may drive him or her to an act of desperation such as suicide.3
In the setting of suspected acute intoxication in a physician who provides patient care or who might be reasonably expected to provide care in the near future (eg, while being “on-call” for emergency care), immediate removal from the practice setting is essential. In such cases, an intervention will include accompanying the suspected addicted physician to an established health care environment, such as the employee health clinic or emergency department, where immediate drug testing can be undertaken. If testing confirms acute intoxication, this portion of the intervention (ie, documentation of substance abuse) is now complete. Care of the physician who abuses drugs now involves taking him or her to a facility that has the means to evaluate for addiction. Faithful adherence to preexisting institutional policies is important. In a less urgent situation in which addiction is suspected in the absence of workplace intoxication, it is critical that before intervention there is a plan for a chain-of-custody transfer of the suspected addict to the area where he or she will be evaluated, whether that is an employee health clinic, a state PHP, or directly to a chemical dependency expert. Most state PHPs will provide invaluable assistance with either conducting an effective intervention or providing a recommendation for referral to a third-party specializing in interventions.10 Although it is beyond the scope of this article to provide a detailed manual on how best to perform a safe and effective intervention, in the past 20 years, theories of the timing of intervention have evolved from waiting until the addict has reached “rock bottom,” ie, the point of absolute despair and having lost everything meaningful in his or her life, to a model in which an intervention occurs earlier in the disease process. Using this confrontational approach, the addict is faced by a roomful of family members, coworkers, supervisors, etc, who offer specific evidence of the addictive behavior they have witnessed in an effort to rapidly break down the tendency of the addict to deny a problem. The addict is then immediately transferred to a chemical dependency treatment facility for detoxification, evaluation, and treatment. After any intervention, the addicted physician must never be simply sent home with instructions to check in for an evaluation at some later date because the risk of suicide is far too great (M.D.S., oral communication, March 4, 2009). The evaluation phase may last from several hours to several days and is often an inpatient process.
One frustration in the aftermath of such an intervention is that, due to confidentiality concerns, once the suspected addict is in evaluation or chemical dependency treatment, there is very little transfer of information back to the workplace regarding the accuracy of the diagnosis in question or a possible timetable for return to practice. This can prove problematic for those trying to fill the manpower gap left by the physician's absence from the workplace. Additionally, the medical evaluation of the physician can be inconclusive. In such cases, we recommend continued discreet observation of the physician for further worrisome behavior because even experts can be fooled by a well-crafted denial.
WHAT IS CHEMICAL DEPENDENCY “TREATMENT”?
Evaluation of physicians with substance abuse disorders is difficult and requires a multidisciplinary team with experience working with this population.11 The intellect that physicians rely on to learn their craft allows them to develop exceptional rationalization, denial, and resistance techniques. Thus, recognition of their disease is difficult.12 During the initial evaluation, most physicians will deny having a problem. Although a detailed substance use history is essential to the diagnosis, it can be remarkably difficult to obtain. Therefore, collateral information from friends, family, coworkers, and pharmacies is required to gather documentation to support the diagnostic evaluation, and the evaluating program will typically require signed releases from the physician undergoing evaluation to obtain this vital information. The substance use evaluation seeks to determine whether addiction indeed exists and the extent of the problem. Both a complete medical history and a physical examination are necessary because addicted individuals have often neglected their health. A family evaluation gathers information about the individual's functioning and determines how the family has been affected. Co-occurring psychiatric illness (called a dual-diagnosis, ie, substance use disorder combined with a major depressive disorder, bipolar affective disorder, or anxiety or panic disorder) is common in the addicted physician and can undermine recovery from addiction13; thus, psychiatric and psychological evaluations are needed. Cognitive screening is required to rule out substantial impairment, which can be further assessed by complete neurocognitive testing. Substantial cognitive and memory impairments are often seen in the setting of alcohol and methamphetamine dependence.
After a diagnosis of addiction has been established, treatment should be initiated at a program that specializes in the care of addicted physicians. Detoxification is frequently needed to prevent withdrawal symptoms and to provide a safe transition to a drug-free state. The patient will be assigned to an addiction counselor and a physician. Most treatment-program curricula include individual and group psychotherapy, education about addiction, and the opportunity for fellowship to reestablish positive relationships with peers.14 The primary focus of most treatment programs is complete abstinence from drugs and alcohol and is based around a 12-step program, as originally crafted for the Alcoholics Anonymous model. McLellan et al2 found that 95% of physicians underwent treatment on the basis of this model, with 78% entering a residential treatment program for a mean of 72 days (range, 30-90 days) and 22% entering directly into outpatient treatment. Addiction treatment is designed to help individuals recognize the extent that addiction has controlled their behavior and altered their lives. Initial treatment efforts help addicts break through denial, recognize those aspects of their lives that need attention and healing, and come to accept that they have a life- and career-threatening disease. An effort is made to provide them with the skills and resources needed to stay abstinent and address their other problems, which range from marital and family issues to loss of job or professional license.
Addiction treatment programs specializing in the care of physicians offer specific therapeutic modalities targeted at physicians. Group therapy for physicians, consisting of meetings with multiple addicted-physician peers, is a primary feature of these programs. These groups provide the opportunity for physicians to recognize their own maladaptive behaviors reflected in their peers and to discuss those issues unique to the health care workplace. This includes discussion of access to addicting medications, licensure, shame and guilt, return-to-work issues, and dealing with patients. This type of therapy requires a staff familiar with physicians and their work environment. A medical practice assessment is used to identify risks and problems in the workplace and to establish a treatment plan supportive of abstinence. Such plans include recommendations for mutual help meetings (Alcoholics Anonymous, Narcotics Anonymous), therapy, monitoring, and workplace limitations.11 The treatment plans attempt to align the patients' goals with those of their employers, the state PHP, and other interested parties (eg, the Drug Enforcement Administration). Additionally, it is beneficial for those leaving treatment to connect with physicians already in recovery from addiction and to establish a recovering peer group in their local community.
SHOULD THE ADDICTED PHYSICIAN RETURN TO PRACTICE?
Physicians have remarkable abstinence rates after completing an addiction/rehabilitation program compared with the general population. Abstinence rates are between 74% and 90%, similar to another professional group with higher than average success rates, airline pilots.15-17
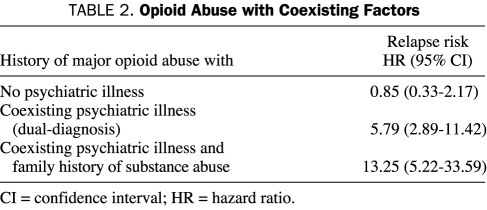
These high rates could be due to motivation to maintain licensure and to continue professional practice, as well as the extensive treatment and long-term monitoring that are required. However, there is also a disturbing rate of recidivism for addicted physicians. The Washington State PHP reviewed its experience with health care professionals during a 10-year period and found that 25% had at least 1 relapse and noted apparent contributing or confounding factors.13 Relapse risk was increased by a family history of a substance use disorder and by a coexisting psychiatric illness (dual-diagnosis). Indeed, in the setting of opioid addiction, a coexisting psychiatric illness or a positive family history of addiction resulted in a significantly increased risk of relapse. The 3 factors, when combined in a single individual, resulted in a 13-fold increase in risk of relapse (Table 2). Menk et al18 found that even 1 relapse can be catastrophic in the setting of addiction to potent opioids such as fentanyl, because 16% of the relapsed anesthesia residents were found dead before anyone suspected a relapse. Thus, addiction treatment and monitoring programs must account for these factors when treatment plans are being developed and when physicians are being counseled about returning to practice.
TABLE 2.
Opioid Abuse with Coexisting Factors
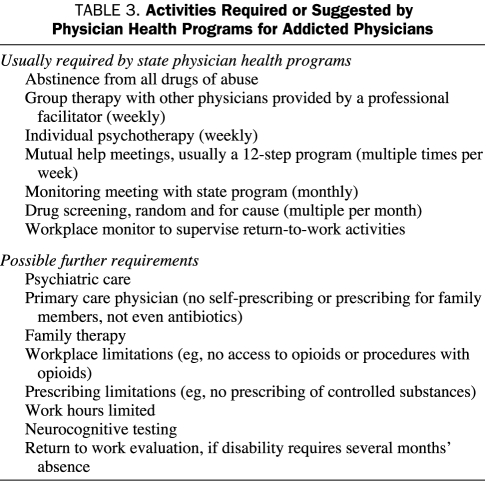
Society and the individual's investment in physician training, as well as the high abstinence rates for addicted physicians who complete an appropriate treatment program, support a rehabilitation model, not a punitive stance. Shore19 revealed a high suicide rate associated with a punitive model in contrast to high recovery rates associated with a good monitoring system. Many physicians can successfully return to practice with a solid addiction recovery program and monitoring systems in place. Any physician returning to practice should engage in his or her state's PHP, and in general such participation is mandatory. These programs are usually led by physician advocates, and they provide resources for individual and group therapy, psychiatric care, mutual help meetings, body fluid monitoring for drugs of abuse, and workplace education and monitoring. Usually, PHPs require contracts with the physician that document expected activities and require compliance with the activities (Table 3) most likely to ensure abstinence and successful return to practice. Failure to comply with the program required by the PHP will result in reporting to the state's medical licensing board, at which point there will typically be a disciplinary action taken with the possibility of public disclosure, sanctions up to and including license suspension, or, in extreme cases, revocation. The PHP will generally manage the logistics of obtaining and monitoring required drug screens, both random and for cause. Such testing both promotes abstinence and establishes a record of abstinence, although limits of such testing exist that can lead to both false-positive and false-negative test results. Often, limitations on physician prescribing are put in place to include opioids or other potentially addicting medications. Return to a group practice setting with the provision of on-site supervision by peers is considered optimal but typically is not mandatory (M.D.S., e-mail communication, March 30, 2009).
TABLE 3.
Activities Required or Suggested by Physician Health Programs for Addicted Physicians
Anesthesiologists represent a special case, in that access to and use of highly addictive drugs are common in anesthesia practice. Furthermore, anesthesiologists who are addicted to anesthetic agents or anesthetic supplements (eg, opioids, propofol, volatile anesthetic agents) have a uniquely high relapse rate associated with an unacceptable risk of morbidity and mortality.18 As such, it is often preferable to limit the future professional activities of these once-addicted anesthesiologists to nonclinical roles such as research, teaching, and administration or to direct them to a new practice specialty. Indeed, this high relapse rate in anesthesiologists, coupled with the substantial risk that the initial manifestation of relapse will be death, has led 2 of the authors (K.H.B. and M.D.S.) to suggest in a recent editorial that anesthesia caregivers who become addicted to anesthetic agents should not be allowed to return to the operating room environment.20
LEGAL ASPECTS
The legal aspects of addressing physician addiction can be thorny and complex. The first legal and ethical obligation of a clinic or hospital after discovery that a staff physician has an addiction is to safeguard patients by removing the physician from practice and counseling the physician to take a leave of absence for treatment. State laws vary on drug testing of employees.21 Some states disallow drug and alcohol testing unless the employer has a written drug and alcohol testing policy in place that meets certain legal requirements. Some state laws restrict random testing and limit grounds for testing based on “reasonable suspicion.”
State medical licensing boards typically require physicians to self-report and to report on other physicians who are unable to practice medicine safely because of drug or alcohol use.22 Most states have a bypass mechanism that allows foregoing of a report to the state licensing board and instead allows a report to the state's PHP to satisfy this requirement.23 However, these bypass programs may have eligibility requirements that exclude certain physicians from participating and require a report to the medical board. Typical exclusions are for physicians who are already under licensing board discipline, those who previously have been terminated from a professional rehabilitation program, those who have diverted controlled substances for other than self-administration, or those whose continued practice of medicine would create a serious risk of harm to the public.24 As long as the reported physician complies with the practice limitations and continuing care requirements of the rehabilitation program and abides by the requirements of the PHP, the physician engaged in a bypass program typically can avoid formal, public reprimand or disciplinary action by the licensing board. However, in California, such a bypass rehabilitation program has come under public attack for permitting impaired physicians to continue to practice and for not being effective in adequately protecting patients from substandard care.25
Federal laws, such as the Americans with Disabilities Act,26 and state civil rights laws27 generally protect physicians actively engaged in chemical dependency treatment programs as well as recovering addicts. These laws generally require “reasonable accommodation” for the recovering alcoholic and drug addict, such as a modified work schedule. (However, the Americans with Disabilities Act specifically excludes as a covered disability “psychoactive substance abuse disorders resulting from current illegal use of drugs.” 28) Furthermore, federal and state laws mandate job protection, typically up to 12 weeks, during a medical leave for addiction treatment.29
When a physician returns to work after addiction treatment, employers and hospitals generally can impose restrictions on employment, as described in the previous section. Clinics and hospitals should spell out for the returning physician the consequences of a relapse or failure to comply with any of the return-to-work conditions.
Is an impaired or recovering physician required to disclose this status to patients as part of informed consent? State courts are split on this issue. For example, in 2000 the Georgia Supreme Court ruled that no cause of action existed against a physician for his failure to disclose his drug (cocaine) use to his patient before a surgical procedure and that this failure did not void the patient's informed consent to the procedure.30 In contrast, a Louisiana appellate court ruled in 1991 that a surgeon's failure to disclose his alcohol abuse voided the patient's consent to a lumbar spine procedure.31 The court reasoned that the alcohol abuse created a material risk relating to the physician's ability to perform the surgery, and if the physician had disclosed this information, the patient could have opted for another type of treatment.
CONCLUSION
Addictive disease is relatively common in the general population and in the physician population. Prompt recognition of addictive disease in a physician is difficult and yet critical because delay could result in morbidity or mortality not only in the addicted physician but also in his or her patients. It is vital that written policies and procedures are in place to assist in these highly emotionally charged situations, because they will promote a consistent and effective approach to promoting early recognition of a substance abuse problem, an effective intervention, and effective treatment and aftercare. Such policies can help prevent disastrous medical and legal outcomes for the affected physician, for his or her colleagues or employer, and for the physician's patients. Each state's PHP can serve as a valuable source of information and assistance and should be contacted when an optimal course of action is unclear. Many physicians can achieve long-term recovery and sobriety with appropriate treatment, aftercare, and monitoring, although certain specialties, such as anesthesiology, present unique challenges and concerns. Given the potential harm that might befall both the addicted physician and patients, it is essential that family, friends, colleagues, and employers not “turn a blind eye” to a physician in whom addiction is suspected. Effective, and often life-saving, evaluation and treatment are available and must be sought for the benefit of all.
REFERENCES
- 1.Hughes PH, Brandenburg N, Baldwin DC, Jr, et al. Prevalence of substance use among US physicians [published correction appears in JAMA. 1992;268(18):2518] JAMA 1992;267(17):2333-2339 [PubMed] [Google Scholar]
- 2.McLellan AT, Skipper GS, Campbell M, DuPont RL. Five year outcomes in a cohort study of physicians treated for substance use disorders in the United States. BMJ 2008;337:a2038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Myers MF, Gabbard GO. The Physician as Patient: A Clinical Handbook for Mental Health Professionals Washington, DC: American Psychiatric Publishing; 2008. [DOI] [PubMed] [Google Scholar]
- 4.Silverstein JH, Silva DA, Iberti TJ. Opioid addiction in anesthesiology [published correction appears in Anesthesiology. 1993;79(5):1160] Anesthesiology 1993;79(2):354-375 [DOI] [PubMed] [Google Scholar]
- 5.Hughes PH, Baldwin DC, Jr, Sheehan DV, Conard S, Storr CL. Resident physician substance use, by specialty. Am J Psychiatry 1992;149(10):1348-1354 [DOI] [PubMed] [Google Scholar]
- 6.Gallegos KV, Browne CH, Veit FW, Talbott GD. Addiction in anesthesiologists: drug access and patterns of substance abuse. QRB Qual Rev Bull. 1988;14(4):116-122 [DOI] [PubMed] [Google Scholar]
- 7.Talbott GD, Gallegos KV, Wilson PO, Porter TL. The Medical Association of Georgia's Impaired Physicians Program. Review of the first 1000 physicians: analysis of specialty. JAMA 1987;257(21):2927-2930 [PubMed] [Google Scholar]
- 8.Holmes L. http://www.house.leg.state.mn.us/hrd/pubs/dgaltest.pdf. Information Brief: Minnesota House of Representatives, Research Department. Workplace drug and alcohol testing. Accessed May 4, 2009.
- 9.Coombs RH. Drug-Impaired Professionals Cambridge, MA: Harvard University Press; 1997. [Google Scholar]
- 10. http://www.fsphp.org. Federation of State Physician Health Programs Web site. Accessed May 4, 2009.
- 11.Graham AW, Schultz TK, Mayo-Smith MF, Ries RK, Wilford BB. Principles of Addiction Medicine 3rd ed.Chevy Chase, MD: American Society of Addiction Medicine; 2007. [Google Scholar]
- 12.Gastfriend DR. Physician substance abuse and recovery: what does it mean for physicians—and everyone else [editorial]? JAMA 2005;293(12):1513-1515 [DOI] [PubMed] [Google Scholar]
- 13.Domino KB, Hornbein TF, Polissar NL, et al. Risk factors for relapse in health care professionals with substance use disorders. JAMA 2005;293(12):1453-1460 [DOI] [PubMed] [Google Scholar]
- 14.Talbott GD, Wright C. Chemical dependency in health care professionals. Occup Med. 1987;2(3):581-591 [PubMed] [Google Scholar]
- 15.Skutar C. Physicians Recovery Network targets attitudes about impairment. Mich Med. 1990;89(12):30-32 [PubMed] [Google Scholar]
- 16.Kliner DJ, Spicer J, Barnett P. Treatment outcome of alcoholic physicians. J Stud Alcohol 1980;41(11):1217-1220 [DOI] [PubMed] [Google Scholar]
- 17.Gallegos KV, Norton M. Characterization of Georgia's Impaired Physicians Program treatment population: data and statistics. J Med Assoc Ga 1984;73(11):755-758 [PubMed] [Google Scholar]
- 18.Menk EJ, Baumgarten RK, Kingsley CP, Culling RD, Middaugh R. Success of reentry into anesthesiology training programs by residents with a history of substance abuse. JAMA 1990;263(22):3060-3062 [PubMed] [Google Scholar]
- 19.Shore JH. The Oregon experience with impaired physicians on probation: an eight-year follow-up. JAMA 1987;257(21):2931-2934 [PubMed] [Google Scholar]
- 20.Berge KH, Seppala MD, Lanier WL. The anesthesiology community's approach to opioid- and anesthetic-abusing personnel: time to change course. Anesthesiology 2008;109(5):762-764 [DOI] [PubMed] [Google Scholar]
- 21.State and territory laws http://www.dol.gov/asp/programs/drugs/said/StateLaws.asp. US Department of Labor Web site. Accessed May 5, 2009.
- 22. http://www.fsmb.org/directory_smb.html. Federation of State Medical Boards Web site. Accessed May 5, 2009.
- 23. http://webrh12.revisor.leg.state.mn.us/statutes/?id=181. 2008 Minnesota statutes. Minnesota Office of the Revisor of Statutes Web site. Accessed May 5, 2009.
- 24. http://www.hpsp.state.mn.us/ State of Minnesota Health Professionals Service Program Web site. Accessed May 5, 2009.
- 25. http://www.msnbc.msn.com/id/22314486/from/ET2007. Addicted doctors still practice while in rehab: confidential programs criticized after reports of botched operations. MSNBC Web site. Accessed May 5, 2009.
- 26. http://www.law.cornell.edu/uscode/html/uscode46/usc_sec_46_00012101----000-.html. U. S. code collection: definitions. Cornell University Law School Web site. Accessed May 5, 2009.
- 27. http://www.law.cornell.edu/wex/index.php/Disability_law. Disability law: an overview. Cornell University Law School Web site. Accessed May 5, 2009.
- 28. http://www4.law.cornell.edu/uscode/ U. S. code collection: contents and context. Cornell University Law School Web site. Accessed May 5, 2009.
- 29. http://www.dol.gov/dol/topic/benefits-leave/index.htm. Leave benefits. US Department of Labor Web site. Accessed May 5, 2009.
- 30. http://biotech.law.lsu.edu/cases/consent/albany_urology_clinic.htm. Albany Urology Clinic PC. v. Cleveland: 272 Ga. 296, 528 S.E.2d 777 (Ga. 2000) Accessed May 5, 2009.
- 31. http://www.lawandbioethics.com/demo/Main/LegalResources/C5/Hidding.htm. Hidding v. Williams (578 So. 2d 1192) 1991. Accessed May 5, 2009.