Abstract
Breath tests using 13C-substrates have been proposed for the measurement of gastric emptying (GE). The mathematical analysis of the breath 13CO2 excretion that most accurately predicts GE t1/2 from simultaneous scintigraphy is unresolved.
Aim
To compare 5 mathematical methods to estimate GE t½ by breath test (BT) with t½ from simultaneous scintigraphy.
Methods
Data acquired from a dual-labeled solid-liquid meal containing 99mTc sulfur colloid and 13C-Spirulina platensis from 57 healthy volunteers were used to compare 4 mathematical methods reported in the literature (Ghoos method; generalized linear regression [Viramontes]; linear regression [Szarka]; Wagner-Nelson method) and the total cumulative breath 13CO2 excretion with ≥ 12 breath samples collected over at least 4 hours. The concordance correlation coefficient (CCC) for the t½ results obtained with each method using breath test data was compared with the results obtained with scintigraphy.
Results
The linear regression and generalized linear regression methods used 5 samples at 45, 90, 120, 150 and 180 minutes. All methods, except for the Wagner-Nelson method, resulted in mean GE t½ that approximated t½ obtained with scintigraphy. The highest CCC was observed with the linear regression method. Simple cumulative excretion of breath 13CO2 provides a better CCC than the Ghoos method.
Conclusion
The linear regression and generalized linear regression methods (which also require relatively few breath samples) provide the most accurate analyses of breath 13CO2 excretion in stable isotope GEBT.
Keywords: scintigraphy, spirulina
INTRODUCTION
Scintigraphy is the accepted gold standard for measurement of gastric emptying of solids and, worldwide, it is the most commonly used method; consensus protocols for measurement of gastric emptying have been recently published (1). However, scintigraphy is not generally available, and involves radiation exposure, precluding use in pregnant patients and healthy children. Thus, breath tests using 13C-substrates (13C-octanoic acid breath test, 13C-OABT, or the edible 13C-enriched blue-green alga, Spirulina platensis) have been proposed for the measurement of gastric emptying. These substrates are rapidly absorbed in the proximal small intestine, metabolized in the liver with the production of 13CO2 which is exhaled rapidly with low interindividual variability (2). Thus, 13CO2 exhalation reflects gastric emptying of nutrients (2).
Several of the breath test methods, using different mathematical models to analyze the breath test, have been compared to results obtained with simultaneous scintigraphy (2–7). The optimal mathematical analysis for the interpretation of these breath test metrics is still unclear. Ghoos et al. developed the original nonlinear regression or Ghoos model (2). In prior studies from our laboratory, we had noted that the results using this model differed significantly from the results obtained by simultaneous scintigraphy, and that the accuracy of the test could not be enhanced by increasing the duration of breath collection (3). In other studies, we noted that breath 13CO2 excretion continued to increase after the radioisotope had been shown to have emptied from the stomach during simultaneous scintigraphy (4,5). By way of contrast, the analysis proposed by Ghoos et al. (2) requires a steady state in 13CO2 excretion to have been achieved by the end of the breath collection. Our experience was that the parameter m, which reflects this portion of the breath 13CO2 excretion curve, was not constant, and in several instances exceeded 100% of the given dose (4,5). This overestimation of the parameter m led to erratic performance of the mathematical model relative to the gold standard.
Therefore, an alternative approach was developed in which the analysis was based on a minimum number of breath samples at pre-specified times during the 3 hour postprandial period to mathematically predict the gastric emptying Tlag and T1/2 measured by simultaneous scintigraphy (4,5). Other mathematical methods have also been proposed in the literature.
The aim of the current study was to compare 5 mathematical methods to estimate gastric emptying results, and to compare the results with those obtained with simultaneous scintigraphy. In order to evaluate the performance of the mathematical models in a broad range of gastric emptying rates, we used pharmacological approaches to accelerate or retard gastric emptying.
METHODS
Study Design
This is a single cohort study of data obtained in 57 healthy volunteers. Scintigraphic and breath test data using a dual-labeled, solid-liquid meal of egg whites, whole wheat bread and skimmed milk containing 99mTc sulfur colloid and 13C-Spirulina platensis were used to compare 4 mathematical methods reported in the literature and a fifth approach based on the cumulative excretion of 13CO2 over 4 hours. Details of participants and methods are published elsewhere (6).
Subjects and Conduct of Gastric Emptying Tests
The healthy volunteers (26 males), aged 18–56 years (mean 34, SD 9.7 years), and body mass index median 24.9 kg/ m2 (range 18.7±41.9), were recruited by public advertisement. Written informed consent was obtained before participation in the protocol, which was approved by the Institutional Review Board and the Radiation Control Committee of the Mayo Clinic. 13CO2 breath test was conducted using 13C–S. platensis, an edible blue-green alga that contains 50±60% protein, 30% starch, and 10% lipid. When metabolized, the proteins, carbohydrates and lipids of the S. platensis give rise to respiratory CO2 that is enriched in 13C. The test meal consisted of eggs dosed with 200 mg of 13C–S. platensis (AB Diagnostics, Inc., Houston, TX, USA) and 0.5 mCi 99mTc-sulphur colloid. The egg whites were mixed with 0.5 mCi 99m Tc-sulfur colloid.
After an overnight fast, anterior and posterior scintiscans were obtained using a large field of view camera with the patient standing. Imaging began at the start of the test meal, and scans were obtained every 15 minutes for the first 2 hours and every 30 minutes for the next 3 hours (total 5 hours). End-tidal breath samples were obtained before the meal and at the same times as the Ghoos camera images. 13CO2 breath content was determined in a centralized laboratory by isotope ratio mass spectrometry (8,9).
Scintigraphic gastric emptying was summarized using a power exponential model (10). propt = [exp −(κt) β] where propt is the proportion remaining in the stomach at time t. The index κ represents the instantaneous slope of the curve; β is an index for the shape of the curve (β = 1 implies a simple exponential emptying model as occurs with liquid emptying). The parameters κ and β were estimated using the nonlinear least squares (NLIN) procedure in the SAS software package (11). The gastric half-emptying times (t1/2) were derived after estimating κ and β for each subject, and solving the following equation for tp =(1/κ) * [Log((1/p))] (1/β) , where p=0.5.
The 13C enrichment determined by isotope ratio mass spectrometry was expressed as the delta per mL difference between the 13CO2/12CO2 ratio of the sample and the standard. To calculate the quantity of 13C appearing in breath per unit time, delta over baseline (DOB) was used: 13Cµmol/L/min= DOB X 0:0112372 X CO2 production, where 0.0112372 is the isotopic abundance of the limestone standard, Pee Dee Belemnite, and CO2 production was corrected for age, sex, height and weight using the algorithms of Schofield et al. (12).
Atropine and Erythromycin Dosing to Mimic Delayed and Accelerated Gastric Emptying
Subjects were randomized to a total dose of intravenous atropine (0.01 or 0.02 mg/kg) or intravenous erythromycin (2.0 or 3.0 mg/kg), or no treatment, and the bolus was given immediately prior to meal ingestion, and infusion continued over 50 minutes as previously described (6). These infusions provided gastric emptying rates to simulate a spectrum from dumping syndrome to severe gastroparesis. As published previously (6), there were no age, height, weight, BMI (by ANOVA) or gender (by χ2) differences among the erythromycin (n=10), control (n=33), and atropine (n=14) groups.
Mathematical Methods Used for Analysis of Breath 13CO2 Excretion Curves
Five different methods were investigated to compare their ability to provide estimates of t1/2 obtained by simultaneous scintigraphy:
A. Ghoos method
(2) used all breath samples collected over a 4-hour time period. In this method the parameters a, b, and c in the nonlinear model:
are first estimated for each subject using a nonlinear least squares algorithm (PROC NLIN in he SAS ® package). The area under the predicted breath test concentration curve [i.e., the predicted values of 13CO2 (t) vs. time using the estimated parameter values for a, b, and c) for each subject was then computed via numerical integration (in the current study, the gamma function in SAS ® was used). Then these computed areas were “adjusted” by regressing the scintigraphic t½ values on these areas to obtain the following estimate of t½:
B. Total cumulative breath 13CO2 excretion
(which used at least 12 breath samples collected over at least 4 hours). The rationale for including this additional analysis is based on the observation that the cumulative maximum 13CO2 excretion represents an objective parameter that is collected according to the test protocol and is not mathematically derived. The cumulative breath test values were then used to predict the scintigraphic t ½ values using a simple exponential model (scintigraphic t ½ = η*exp(−θ*Cumulative BT value). The estimated coefficients in this model were, η =290.4 , and θ=0.0204.
C. Wagner-Nelson method
(13) used all breath samples collected over a 4-hour period. The Wagner-Nelson equation is:
where F(t) is a fractional dose of the 13C label emptied,
The fractional dose curve [F(t) vs. t ] for each subject is then treated as a “emptying curve” and t½ estimates obtained via, for example, linear interpolation.
D. Generalized linear regression method [Viramontes (6)]
used only 5 breath samples at 45, 90, 120, 150 and 180 minutes. In this method, the gastric emptying t½ is estimated directly as t½ = 1/LP1/2, where LP1/2 (the “linear predictor”) is given by
E. Linear regression method [Szarka (7)]
which used the same 5 breath samples at 45, 90, 120, 150 and 180 minutes. In this method, the 13CO2 values are used to compute estimates of the GE proportions at times t=15 to 240 minutes. The following formula summarizes the linear regression models and the coefficients are given in Table I.
For example, for t=30 minutes, the estimated GE proportion is obtained by multiplying the values for gender (0=Females,1=Males), BMI, and the 13CO2 values by their respective coefficients: 0.00980, −0.00655 , −0.02590 , −0.17187, 0.15184, −0.06426, and 0.03375 from Table I (30 min) and adding in the corresponding intercept term for 30 minutes to get an estimated GE proportion at 30 minutes. Doing this for each time point yields an estimated gastric emptying curve. The gastric emptying t½ values are then estimated via linear interpolation from the above computed GE proportions at the time points around propt=0.5.
Table I. Linear Regression Model (Szarka method) Coefficients for Estimating Gastric Emptying Proportions Obtained via Scintigraphy Using Individual Breath 13CO2 Excretion Data.
| GE propt at t=(min) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Intercept | Gender | BMI | B45(t) | B90(t) | B120(t) | B150(t) | B180(t) | |
| 15 | 1.09476 | –0.01908 | –0.00415 | –0.00320 | –0.11959 | 0.11568 | –0.02513 | –0.00296 |
| 30 | 1.12249 | 0.00980 | –0.00655 | –0.02590 | –0.17187 | 0.15184 | –0.06426 | 0.03375 |
| 45 | 1.11271 | 0.01303 | –0.00687 | 0.01437 | –0.22596 | 0.16223 | –0.08794 | 0.05765 |
| 60 | 1.04898 | 0.02113 | –0.00538 | 0.05942 | –0.25427 | 0.14985 | –0.10530 | 0.07821 |
| 75 | 1.07397 | 0.02773 | –0.00537 | 0.15000 | –0.30612 | 0.15117 | –0.12109 | 0.07300 |
| 90 | 1.06163 | 0.02812 | –0.00467 | 0.17145 | –0.29358 | 0.13126 | –0.14364 | 0.07598 |
| 105 | 1.09566 | 0.01673 | –0.00611 | 0.19115 | –0.21736 | 0.03825 | –0.12854 | 0.06893 |
| 120 | 1.09889 | 0.00833 | –0.00595 | 0.17042 | –0.17673 | 0.03345 | –0.15714 | 0.06451 |
| 150 | 1.05673 | –0.00527 | –0.00596 | 0.15955 | –0.10749 | 0.03581 | –0.18595 | 0.03408 |
| 180 | 1.07560 | 0.00231 | –0.00886 | 0.10135 | –0.03675 | 0.00027 | –0.13224 | –0.02133 |
| 210 | 0.90088 | 0.00457 | –0.00698 | 0.06637 | –0.02634 | 0.02323 | –0.12215 | –0.03186 |
| 240 | 0.71615 | –0.00362 | –0.00487 | 0.06655 | –0.02279 | 0.00428 | –0.08159 | –0.03467 |
Statistical Analysis
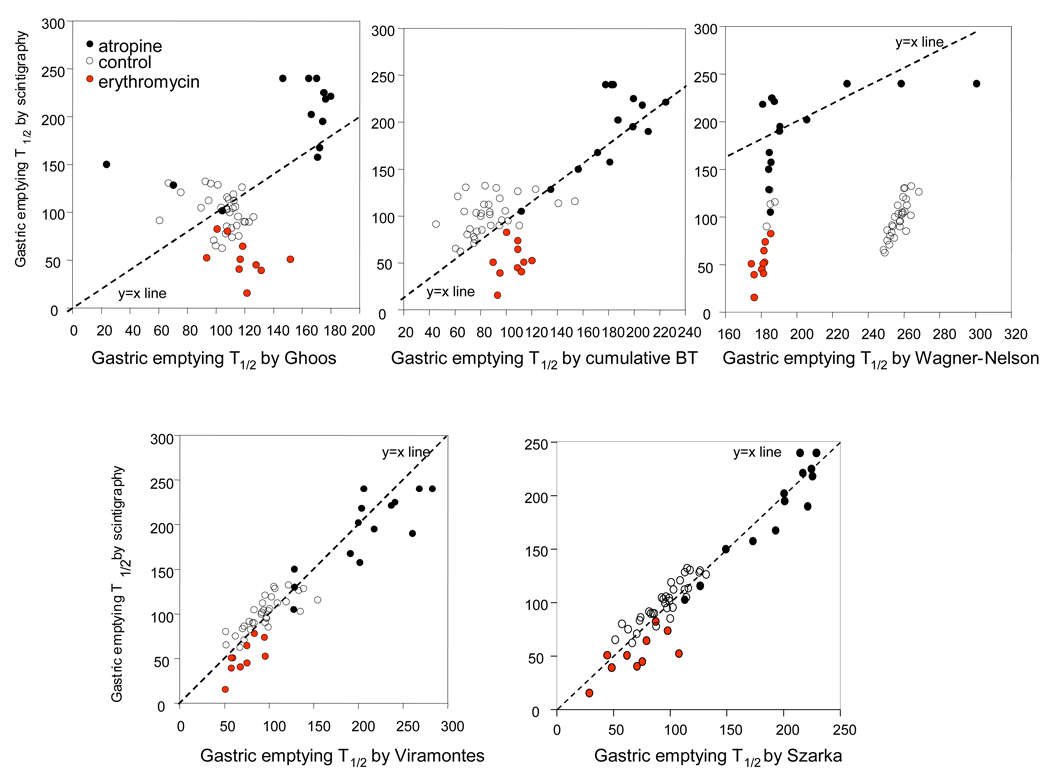
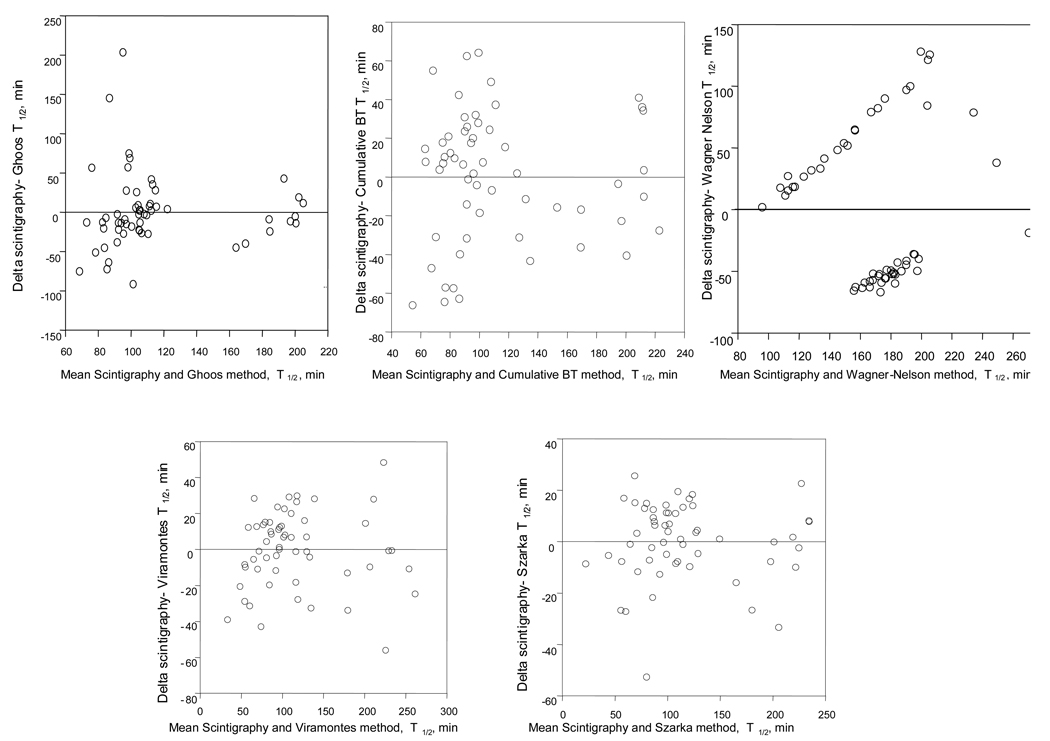
The concordance correlation coefficient [CCC (14)] for the t½ results obtained with each method using breath test data were compared with the t½ results obtained with simultaneous scintigraphy. Scatter plots of the t½ values by scintigraphy (Y-axis) versus the various breath test method estimates of t½ (X axis) were made including the Y=X line to illustrate agreement for each method relative to the gold standard scintigraphic gastric emptying results. In addition, Bland-Altman plots are provided to compare the residuals to the average of the combination of methods for scintigraphy and each mathematical method using breath CO2 excretion.
RESULTS
Gastric Emptying
As previously published (6), the pharmacological modulation resulted in the expected prolongation of gastric emptying with atropine (207.9 ± 72.6 min [SD]), and acceleration with erythromycin (50.2 ± 18.1 min), both significantly different from control (100.7 ± 20.2 min).
Table II shows t½ results obtained by each method as well as the difference in estimated t½ relative to the gold standard scintigraphy. All methods, except for the Wagner-Nelson method, resulted in mean gastric emptying t½ values that approximated the data obtained with scintigraphy. Note however that, although the mean difference for several methods, is close to zero (other than the Wagner Nelson method, which shows several points falling far from the line of identity, as evident in Figure 1), there is a large standard deviation of the difference for the Ghoos model and cumulative excretion methods. The smaller standard deviation typically indicates that there are fewer poorly fitted observations (the gold standard scintigraphy t½ values) with the linear regression (Szarka) and generalized linear regression (Viramontes) methods.
Table II. Comparison of t½ Results by Scintigraphy and Mathematical Models Using Breath Test Data.
t½ results (Mean ± SD, min and [range]) obtained by each method and difference in estimated t½ (mean ± SD and [range]) relative to the gold standard, scintigraphy
| Method | Scinti- graphy |
Ghoos | Cum.13CO2 excretion |
Wagner -Nelson |
Viramontes | Szarka |
|---|---|---|---|---|---|---|
| T½ | 114 ± 55 (16 to 240)† | 117 ± 31 (24 to 179) | 113 ±46 (45 to 225) | 225 ± 38 (175 to 301) | 118 ±60 (51 to 282) | 115 ±53 (29 to 229) |
| Δ t½ vs. scintigraphy | -------------- | −4 ± 47 (−106 to 126) | 1 ± 35 (−78 to 62) | −112 ±65 (−187 to 39) | −4 ±22 (−71 to 34) | −1 ±15 (−55 to 26) |
| CCC | -------------- | 0.43 | 0.77 | 0.01 | 0.93 | 0.96 |
Three subjects had censored t½ values (i.e., t½ > 240 minutes)
Cum=cumulative; Δ=delta; CCC= concordance correlation coefficient
Figure 1.
Scatter plots for each mathematical model used for breath test relative to scintigraphic gastric emptying t1/2 measured simultaneously. Data are separated for the participants receiving atropine, erythromycin and controls. Note i.v. atropine retarded and i.v. erythromycin accelerated gastric emptying relative to controls as shown by the data corresponding to the Y axis. Note also that the data with breath test analyzed by Viramontes and Szarka models most closely approximate the y=x line and are clustered according to gastric emptying category.
The scatter plots in Figure 1 illustrate the agreement for each mathematical model based on breath test values relative to the gold standard, scintigraphy. Points closer to the Y=X line indicate better agreement. Each data point in each plot represents the result for one individual participant, and the difference from the Y=X line reflects the discordance from the gold standard. The Bland-Altman plots in Figure 2 show the residuals or differences between the respective breath test and scintigraphic t1/2 data in relation to the average of the values by scintigraphy and the specific mathematical analysis. Note that the scatter of the residuals around the zero line (identity) is smallest for the Szarka and Viramontes methods.
Figure 2.
Bland Altman for each mathematical model used for breath test relative to scintigraphic gastric emptying t1/2 measured simultaneously.
Correlation between Mathematical Analysis Methods
The highest concordance correlation coefficient was observed with the linear regression [Szarka] method (Table II). The simple cumulative excretion of breath 13CO2 method provided a better concordance correlation coefficient than the Ghoos method.
DISCUSSION
In this technical evaluation of the mathematical models to estimate gastric emptying t1/2 relative to the simultaneous measurements using scintigraphy, the linear regression [Szarka] and generalized linear regression [Viramontes] methods appear to provide the best analyses of breath 13CO2 excretion in stable isotope gastric emptying breath tests. This study is the largest assessment of the different models in which the calculated gastric emptying parameters were observed with the same meal by simultaneous measurements with scintigraphy and breath test. Moreover, the database was selected to ensure that there was a broad spectrum of gastric emptying rates: accelerated normal or delayed. Therefore, the conclusions from our analysis are generalizable.
Whether the breath test is used for diagnostic purposes or to assess the effect of medication, it is critically important that the test is accurate. In this study, the different models have been applied to data obtained using the same meal, and the average t1/2 estimates are close to the scintigraphic data and therefore realistic. This contrasts with some data in the literature which provide unrealistic estimates of t lag and t1/2, when using the Ghoos model method. For example, in a study using a dually radiolabeled muffin, the mean t lag measured by scintigraphy was 42 ± 19 minutes, whereas the mean t lag obtained using the 13C-octanoic acid breath test (OBT) was 121 ± 25 minutes and the overall mean t1/2 as measured by scintigraphy was 104 ± 24 minutes (mean ± SD) whereas, the mean t1/2 by OBT was 212 ± 52 minutes (15).
The cumulative excretion model has the advantage that it uses the actual data collected during the study without the use of any weighting factors; it is therefore potentially more useful in laboratories that have not developed analysis by comparison with simultaneous scintigraphy. However, it does require collection of breath samples over 3–4 hours, and its correlation with scintigraphy does not reach the level observed with the Szarka and Viramontes models which require a small number of breath samples, and are therefore more cost-effective. Thus, one advantage of the linear regression [Szarka] and generalized linear regression [Viramontes] methods is that they require a smaller number of breath samples, typically 5, to obtain the estimates of gastric emptying; this also reduces the cost of the test since it reduces the number of breath samples requiring collection, containers, mailing to a central laboratory and analysis. The linear regression [Szarka] models is also versatile and can be converted to estimate the proportion remaining in the stomach at defined times (e.g. at 1, 2 and 4 hours after meal ingestion).
We conclude that, since the linear regression [Szarka] and generalized linear regression [Viramontes] methods require relatively few (e.g. 5) breath samples and the analysis provides the closest agreement with t½ results based on scintigraphy, these methods provide the best analyses of breath 13CO2 excretion in stable isotope gastric emptying breath tests. The data (coefficients) provided in table I provide the reader with the opportunity to use the linear regression [Szarka] method to estimate a gastric emptying curve from measured breath 13CO2 excretion. From these estimated GE proportions, an estimated t½ value could be obtained. Measurement of the percent retention at specified time points is of interest, and it may reflect gastric emptying rates more accurately than gastric emptying t½ if the latter analysis is limited to a few scans at defined times, such as 1, 2 and 4 hours. However, it is worth noting that, in this study, gastric emptying was measured by means of scans obtained every 15 minutes for the first 2 hours and every 30 minutes for the next 3 hours (total 5 hours). Moreover, other relevant summaries of a gastric emptying curve (e.g., a gastric emptying lag time, proportion remaining at 3-hours) can easily be calculated from the estimated GE proportions with the information available. Finally, studies in patients with gastroparesis (rather than pharmacologically-induced gastric emptying delay) would be of interest to confirm the conclusions on the optimal pharmacological models used with the breath test. This has been performed with the Szarka model (7) which included approximately 43% of patients with delayed gastric emptying.
Acknowledgments
Dr. Camilleri is funded in part by grants RO1 DK 67071 and K24 DK 02638 from National Institutes of Health. We thank Mrs. Cindy Stanislav for excellent secretarial assistance. An abstract of the study was presented at the American College of Gastroenterology Annual Meeting, October 2008.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Contributor Information
Suwebatu T. Odunsi, Clinical Enteric Neuroscience Translational and Epidemiological Research (CENTER), Mayo Clinic, Rochester, Minnesota
Michael Camilleri, Clinical Enteric Neuroscience Translational and Epidemiological Research (CENTER), Mayo Clinic, Rochester, Minnesota
Lawrence A. Szarka, Clinical Enteric Neuroscience Translational and Epidemiological Research (CENTER), Mayo Clinic, Rochester, Minnesota
Alan R. Zinsmeister, Department of Health Sciences Research, Division of Biostatistics, Mayo Clinic, Rochester, Minnesota
REFERENCES
- 1.Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, McCallum RW, Nowak T, Nusynowitz ML, Parkman HP, Shreve P, Szarka LA, Snape WJ, Jr, Ziessman HA. Consensus recommendations for gastric emptying scintigraphy. A Joint Report of the Society of Nuclear Medicine and the American Neurogastroenterology and Motility Society. Am J Gastroenterology. 2008;103:753–763. doi: 10.1111/j.1572-0241.2007.01636.x. [DOI] [PubMed] [Google Scholar]
- 2.Ghoos YF, Maes BD, Geypens BJ, Mys G, Hiele MI, Rutgeerts PJ, Vantrappen G. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology. 1994;104:1640–1647. doi: 10.1016/0016-5085(93)90640-x. [DOI] [PubMed] [Google Scholar]
- 3.Choi M-G, Camilleri M, Burton DD, Zinsmeister AR, Forstrom LA, Nair KS. 13C-octanoic acid breath test for gastric emptying of solids: accuracy, reproducibility and comparison with scintigraphy. Gastroenterology. 1997;112:1155–1162. doi: 10.1016/s0016-5085(97)70126-4. [DOI] [PubMed] [Google Scholar]
- 4.Lee JS, Camilleri M, Zinsmeister AR, Burton DD, Kost LJ, Klein PD. A valid, accurate, office based non-radioactive test for gastric emptying of solids. Gut. 2000;46:768–773. doi: 10.1136/gut.46.6.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee J-S, Camilleri M, Zinsmeister AR, Burton DD, Choi M-G, Nair KS, Verlinden M. Toward office-based measurement of gastric emptying in symptomatic diabetics using [13C]octanoic acid breath test. Am J Gastroenterol. 2000;95:2751–2761. doi: 10.1111/j.1572-0241.2000.03183.x. [DOI] [PubMed] [Google Scholar]
- 6.Viramontes BE, Kim D-Y, Camilleri M, Lee JS, Stephens D, Burton DD, Thomforde GM, Klein PD, Zinsmeister AR. Validation of a stable isotope gastric emptying test for normal, accelerated or delayed gastric emptying. Neurogastroenterol Motil. 2001;13:567–574. doi: 10.1046/j.1365-2982.2001.00288.x. [DOI] [PubMed] [Google Scholar]
- 7.Szarka LA, Camilleri M, Vella A, Burton D, Baxter K, Simonson J, Zinsmeister AR. A stable isotope breath test with a standard meal for abnormal gastric emptying of solids in the clinic and in research. Clin Gastroenterol Hepatol. 2008;6:635–643. doi: 10.1016/j.cgh.2008.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klein PD. Clinical applications of 13CO2 measurements. Federation Proc. 1982;41:2698–2701. [PubMed] [Google Scholar]
- 9.Schoeller DA, Schneider JF, Solomons NW, Watkins JB, Klein PD. Clinical diagnosis with the stable isotope 13C in CO2 breath tests: methodology and fundamental considerations. J Lab Clin Med. 1977;90:412–421. [PubMed] [Google Scholar]
- 10.Elashoff JD, Reedy TJ, Meyer JH. Analysis of gastric emptying data. Gastroenterology. 1982;83:1306–1312. [PubMed] [Google Scholar]
- 11.SAS Institute Inc. SAS/STAT Users Guide, Version 6. 4th edn. Vol. 2. Cary, NC: SAS Institute; 1989. pp. 1135–1194. [Google Scholar]
- 12.Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39:541. [PubMed] [Google Scholar]
- 13.Sanaka M, Urita Y, Sugimoto M, Yamamoto T, Kuyama Y. Comparison between gastric scintigraphy and the [13C]-acetate breath test with Wagner-Nelson analysis in humans. Clin Exp Pharmacol Physiol. 2006;33:1239–1243. doi: 10.1111/j.1440-1681.2006.04516.x. [DOI] [PubMed] [Google Scholar]
- 14.Carrasco JL, Jover L. Estimating the generalized concordance correlation coefficient through variance components. Biometrics. 2003;59:849–858. doi: 10.1111/j.0006-341x.2003.00099.x. [DOI] [PubMed] [Google Scholar]
- 15.Chey WD, Shapiro B, Zawadski A, Goodman K. Gastric emptying characteristics of a novel (13)C-octanoate-labeled muffin meal. J Clin Gastroenterol. 2001;32:394–399. doi: 10.1097/00004836-200105000-00007. [DOI] [PubMed] [Google Scholar]