Abstract
Scapula taping is a commonly used adjunctive treatment for shoulder impingement pathology. However, this intervention has not previously been subject to formal investigation. A pilot single-blind randomized controlled trial was conducted to evaluate facilitatory taping as an adjunct to routine physiotherapy management. Twenty-two subjects with unilateral shoulder impingement symptoms were randomized into a taping with routine physiotherapy or a routine physiotherapy only group. The intervention group had scapula taping applied three times per week for the first two weeks of their treatment. All subjects were assessed at baseline, then at 2 and 6 weeks after the commencement of treatment. Pain and functional ability were assessed using the Shoulder Pain and Disability Index, range of shoulder elevation, and self-reported pain on elevation. At 2 weeks, the taping group demonstrated a strong trend toward reduced pain both on self-reported activity (SPADI pain subscale mean for taping 27.0 versus 41.5 for control) and pain during measured abduction (mean VAS 22.8 for taped, 46.8 for control), statistical power being limited by small sample size. No similar trend was evident in the SPADI disability subscale. The magnitude of the differences was reduced at 6-week follow-up. This study provides preliminary evidence for a short-term role for scapula taping as an adjunct to routine physiotherapy in the management of shoulder impingement symptoms but also highlights the need for consideration on a case basis relating to risk factors for skin reaction.
KEYWORDS: Adhesive Tape, Rehabilitation, Shoulder Impingement Syndrome
Perceived abnormalities in scapula position and control during static and dynamic activities have been implicated with sub-acromial impingement. Sub-acromial impingement is one of the most frequently reported shoulder conditions presenting for treatment1–3 and is associated with a reduction of the subacromial region and intrusion on the soft tissues located within this space4. This has been reported to relate to extrinsic factors such as abnormal glenohumeral kinematics or scapula positioning during movement4. Normal and abnormal neuromuscular control of the scapula has been extensively studied using electromagnetic, topographic, magnetic resonance, and digital image processing devices1,5–8. A consistent association has been described between inadequate motor control of the scapula and patients with shoulder impingement symptoms1,5. Whether altered movement control is a primary cause or a consequence of sub-acromial impingement remains a point of conjecture; however, both clearly remain associated, and treatment directed at the neuromuscular sub-systems continues to be a popular choice in the management of this disorder9,10.
Movement dysfunctions of the scapula have been described in various forms; the most common are referred to as winging and pseudo-winging. Inadequacies in motor control during scapula rotation have also been associated with impingement syndrome. Normal and abnormal motion of the scapula was summarized by Michener et al4 with respect to shoulder impingement syndrome to include upward-downwards rotation (antero-posterior axis), external-internal rotation (superior-inferior axis), and anterior-posterior tilting (medial-lateral axis). The abnormal pattern of scapula winging involves excessive internal rotation and to a lesser extent anterior tilting of the scapula7. Pseudo-winging involves excessive anterior tilting and a lesser degree of internal scapula rotation. The third common scapula movement dysfunction involves a lack of upward rotation of the glenoid during elevation of the humerus or insufficient control of downward rotation of the glenoid during lowering of the arm. Scapula position in a clinical setting is usually determined by skin surface palpation11, providing an estimate of movement dysfunction and indicating subsequent management strategies.
The management of shoulder impingement pathology should address the primary underlying causative factors12. This typically includes addressing posture and neuromuscular control via specific exercise4,9,10,13–15 and facilitatory taping15,16. Soft tissue massage, joint mobilizations, and passive stretches are also commonly used treatment choices that have been reported to assist recovery in people suffering from impingement symptoms17–19.
One method believed to assist exercise therapy for shoulder pathology is facilitatory scapular taping. This is despite limited evidence to support such a treatment intervention. The original support for scapula taping in the literature lies only with single case reports in which taping was one component of treatment provided15,19. Over the past decade, varying studies have attempted to understand the influence of taping by determining the impact of this intervention on shoulders without pathology20–22. These studies have shown that taping does not clearly influence motor neuron pool excitability, electromyographic muscle activity, or joint repositioning in normal shoulders. While these studies have been unable to demonstrate how taping may influence motor control within rehabilitation, these do not provide evidence that taping does not assist clients suffering impingement symptoms or other shoulder pathology. An electromyographic study on symptomatic shoulder impingement subjects found scapula taping to significantly reduce upper trapezius fiber muscle activity but not alter lower fibers of trapezius or serratus anterior muscle activity23. The benefit of such an intervention and its electromyographic effect on the recovery of those clients suffering impingement symptoms remains unknown.
To date, no research has been conducted to determine clinical effects of taping in subjects with sub-acromial impingement symptoms. It remains unclear as to whether this intervention is efficacious and if it is, what dosage parameters are required to ensure an effective adjunctive treatment. Therefore, the purpose of this pilot study was to investigate the short-term effect of taping on people presenting with sub-acromial impingement symptoms.
Methods
Subjects
All participants in this study were referred for outpatient physiotherapy treatment at the Royal Newcastle Hospital, a teaching hospital in regional New South Wales, Australia. Referral was accepted from either the patient's general practitioner or from an orthopedic surgeon. Written informed consent was obtained from all participants prior to enrollment in the trial. The study was approved by the Hunter Area Research Ethics Committee.
People aged between 18 and 70 years experiencing unilateral shoulder pain of more than six-week duration were considered for inclusion. Each participant's pain was reproduced using the shoulder impingement test described by Hawkins and Kennedy24 to meet the inclusion criteria. Participants were required to have effective written and verbal competence in the English language.
Potential participants were excluded if cervical spine involvement in the disorder could be demonstrated. This was defined by active neck movement reproducing pain in the shoulder region. A presence of a glenohumeral joint adhesive capsulitis as identified by a loss of passive shoulder motion into external rotation25 also led to exclusion from the study. Other exclusion criteria used in this study were a history of previous shoulder surgery, physiotherapy treatment for this disorder in the past four weeks, steroid injection into or around the shoulder in the past two months, demonstrable neurological deficits, poor or fragile skin condition, and a report of past skin reaction associated with the use of adhesive tape.
Design
A randomized, single-blind clinical trial design was used. Prior to commencing the study, a randomization list was created using a random number table. Eligible patients were enrolled and allocated a study number. All participants were then assessed by a blinded research assistant using standard physiotherapy measures and they completed a Shoulder Pain and Disability Index questionnaire (SPADI)26. Group allocation (taping or not taped) was then made using sequentially numbered sealed opaque envelopes.
Intervention
All participants received routine physiotherapy treatment as indicated in an individual assessment of their condition by their treating physiotherapist. In addition to routine care, the intervention group received scapular taping applied three times per week for the first two weeks of their treatment. Each taping was removed after two days in situ. Education sessions were provided to treating physiotherapists to attain agreement on range of acceptable treatment options, including soft tissue massage and joint mobilization techniques, exercise (scapula and rotator cuff stabilization, stretches, and general strengthening). No taping was applied to either group between the 2- and 6-week measures.
The method of scapula taping was based on the common dysfunctions of winging, pseudo-winging, and excess downward rotation. The taping consisted of two straps: the first strap anchored over the anterior deltoid muscle and extended posteriorly along the line of the spine of the scapula, terminating in the midline; the second strap anchored anteriorly over the coracoid process and extended posteriorly and inferomedially over the scapula in imitation of the line of pull of the lower trapezius (Figure 1). Skin preparation included the use of a protective barrier wipe beneath the adhesive tape to assist in maintaining skin integrity. An initial tape layer comprised a 50mm hypoallergenic polyacrylate adhesive non-woven bandage over which was laid a 38mm premium non-elastic zinc oxide adhesive tape. Taping was standardized through education of physiotherapists involved in the study.
FIGURE 1.

Method of scapula taping.
Measures
Measurement occurred prior to randomization at baseline and then at 2 weeks and 6 weeks following the commencement of treatment. All data were collected by an assessor blinded to the patients' group allocation.
The primary outcome measure used for the study was the SPADI questionnaire26. This self-administered questionnaire yields a continuous measure between 0 and 100 on 13 items measuring shoulder pain and functional status. These are used to produce two subscale scores for pain (5 items) and disability (8 items), and a total score. This instrument has previously been demonstrated to be valid and reliable in detecting changes in patient clinical status26–28.
Shoulder range of movement into flexion and abduction was evaluated using a digital inclinometer using the standardized approach described and assessed for both inter- and intra-rater reliability by Green et al29. A visual analogue scale (VAS) pain score was recorded for each of these active movements. Assessors remained blinded to group allocation at all times. In addition, demographic and background factors were recorded including age, gender, dominant hand, side of symptoms, and duration of symptoms.
Statistical Analysis
Measurements of all outcomes were examined for normality, and taping and control groups compared by the non-parametric Wilcoxon rank-sum test. This occurred using measurements from baseline, 2 weeks, and 6 weeks following the commencement of treatment. A p-value of less than 0.05 was considered to be statistically significant. All analyses were performed using STATA version 8.1.
Results
Twenty-two people were recruited into this pilot study; 10 were allocated to the taping with normal treatment group and 12 to the normal treatment alone control group. The characteristics of the participants are given in Table 1. At baseline, the control group had a significantly lower median age and a greater number of male participants than the taped group.
TABLE 1.
Characteristics of study sample
| Taping with routine physiotherapy (n=10) Median (interquartile range) | Routine physiotherapy only (n=12) Median (interquartile range) | ||
|---|---|---|---|
| Gender | Male | 3 | 7 |
| Female | 7 | 5 | |
| Age (years) | 62 (51–67) | 54.5 (45.5–62.5) | |
| Handedness | |||
| Left | 1 | 1 | |
| Right | 9 | 11 | |
| Side of symptoms | |||
| Left | 2 | 5 | |
| Right | 7 | 7 | |
| Duration of symptoms (weeks) | 16 (7–26) | 17 (12–65) | |
n = number of subjects
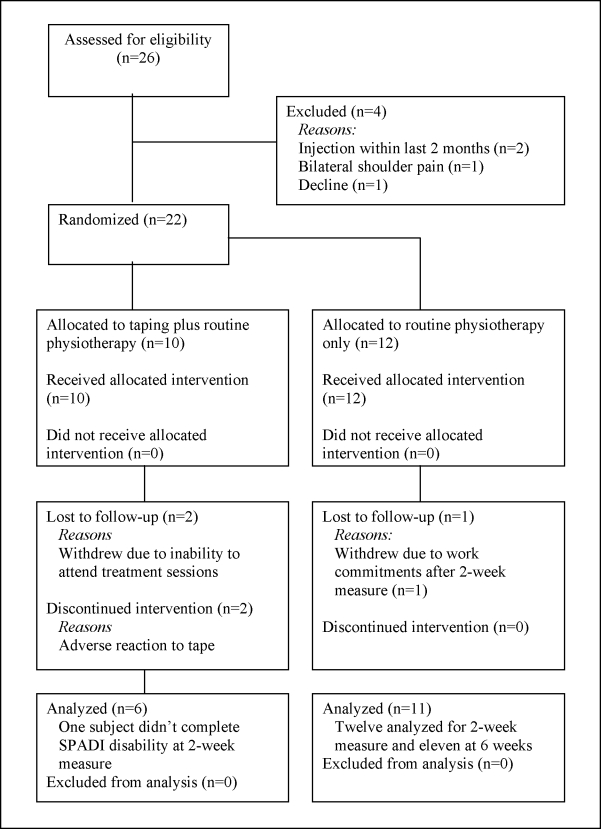
Details of inclusion into the study through final data analysis have been provided in Figure 2. The analysis of data at each measurement stage is provided in Table 2.
FIGURE 2.
Flow diagram of participant inclusion
TABLE 2.
Shoulder Pain and Disability Index and impairment measures
| Taping with routine physiotherapy Median (interquartile range) | Routine physiotherapy only Median (interquartile range) | P value for difference between groups | |
|---|---|---|---|
| Baseline | n = 10 | n = 12 | |
| SPADI Total | 47.7 (39.4–62.8) | 54.4 (27.2–65.1) | 0.90 |
| SPADI Pain | 54.6 (43.6–69.1) | 60.0 (32.7–67.3) | 0.74 |
| SPADI Disability | 36.9 (23.4–60.2) | 50.0 (21.6–63.6) | 0.67 |
| Flexion (degrees) | 131 (124–138) | 126.5 (98.5–140) | 0.45 |
| Flexion VAS (mm) | 25 (11–46) | 32 (14–58.5) | 0.69 |
| Abduction (degrees) | 85.5 (76–124) | 86.5 (62.5–120) | 0.58 |
| Abduction VAS (mm) | 53 (37–63) | 56.5 (14.5–66.5) | 0.95 |
| 2 weeks | n = 6 | n = 12 | |
| SPADI Total | 18.4 (16.0–31.1) n = 5 | 41.5 (12.6–54.3) | 0.60 |
| SPADI Pain | 20.9 (16.4–32.7) | 40.9 (15.4–64.6) | 0.28 |
| SPADI Disability | 20.5 (10.2–29.6) n = 5 | 42.6 (4.6–55.1) | 0.92 |
| Flexion (degrees) | 129 (122–134) | 129 (118–147) | 0.96 |
| Flexion VAS (mm) | 15.5 (5–24) | 38.5 (4.5–51.5) | 0.45 |
| Abduction (degrees) | 122.5 (113–134) | 120 (72–144) | 0.93 |
| Abduction VAS (mm) | 16.5 (5–36) | 56 (32.5–67) | 0.09 |
| 6 weeks | n = 6 | n = 11 | |
| SPADI Total | 13.1 (2.1–33.6) | 19.7 (0–59) | 0.76 |
| SPADI Pain | 18.2 (1.8–25.5) | 20 (0–60) | 0.76 |
| SPADI Disability | 8.5 (1.1–27.3) | 12.5 (0–51.1) | 0.72 |
| Flexion (degrees) | 143.5 (130–152) | 150 (136–155) | 0.96 |
| Flexion VAS (mm) | 13.5 (5–32) | 6 (4–26) | 0.76 |
| Abduction (degrees) | 129 (116–136) | 127 (77–147) | 0.84 |
| Abduction VAS (mm) | 9 (5–14) | 10 (2–66) | 0.45 |
SPADI = Sholder Pain and Disability Index; n = number of subjects
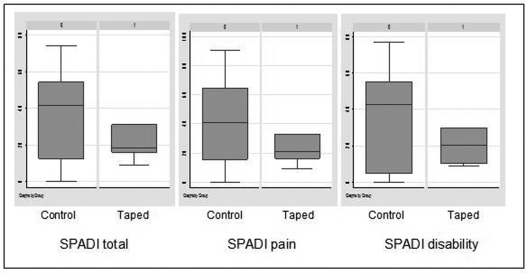
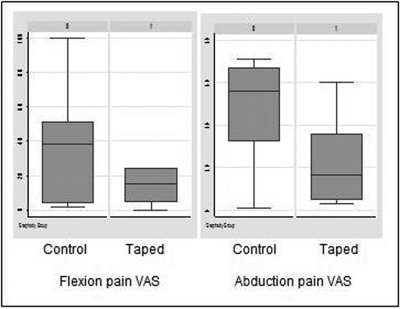
Two weeks following the commencement of treatment, there was a strong trend toward greater self-reported improvement in the taped group. Although not reaching statistical significance, all 3 median subscale scores on the SPADI questionnaire (total, pain, and disability) were markedly lower for the taped group than the normal physiotherapy only group (Figure 3). Similarly, self-reported pain on measured active movements using the visual analogue scale was comparatively much lower in the taped group (Figure 4). Impairment measures themselves showed no difference in range between groups in spite of the changes in self-report measures. At the 6-week follow-up, between-group differences were minimal in regard to either self-report measures or range of movement indicating that these results were not sustained over time.
FIGURE 3.
Comparison of Shoulder Pain and Disability Index scores at 2-week follow-up
FIGURE 4.
Comparison of pain visual analogue scores at two weeks
Discussion
Imbalances in some baseline characteristics such as age and gender between groups were evident despite the rigor of the randomization process. This is indicative of the pilot nature of this data and the consequent small sample size. Thus, the findings should be considered as hypothesis-generating rather than conclusive.
Our results suggest that there may be a potential role for scapular taping as an adjunct to usual physiotherapy treatment in the management of people with impingement symptoms of the shoulder. This benefit appears in the form of a “window” that provides a period of relative pain control occurring early in the treatment process. This is apparent in the analysis at 2 weeks following the commencement of treatment where a marked between-group difference existed on the SPADI pain subscale and on VAS pain scores associated with active flexion and abduction of the shoulder. The implication of this finding is that the reduction in pain as a product of scapular taping may permit the more effective delivery of manual techniques and exercise-based interventions targeting the shoulder dysfunction. The application of such techniques in the presence of pain is less effective and less tolerated by patients.
This finding is supported by the published case studies of both Host16 and Schmitt and Snyder-Mackler15 and the clinical observations reported by Mottram9, where the application of tape resulted in a reduction of painful symptoms reported by their respective patients. This occurs despite the differences in the methods of tape application between each of these studies and our own study.
However, differences between the groups at the 6-week follow-up do not illustrate a sustained effect from the taping intervention with no clinically significant difference detectable in self-reported pain scores either on the SPADI questionnaire or VAS of active planar movements at that point. This suggests that any benefits are short-lived and the decision to use facilitatory taping in the clinic should be aimed at specific short-term targets in the rehabilitation process. This aspect reflects the findings of Alexander et al20, who noted that the electromyography changes observed with taping were not sustained following the removal of tape.
One potential limitation of the study relates to the use of the sole impingement test described by Hawkins and Kennedy24 for inclusion in the study. More recently available evidence suggests a combination of Hawkins and Kennedy, painful arc sign, and infraspinatus muscle test might provide greater probability of detecting impingement symptoms30.
Of particular concern in this pilot study was the differential rate of drop-out between the two treatment groups raising questions of acceptability, dosage, and skin reaction in taping of this type. In all, 4 people out of 10 in the taping group either withdrew or were withdrawn from the study by the researchers compared to one withdrawal in the treatment-only group. One reason for the loss of the taped participants was the occurrence of mild skin reactions to the taping. As detailed earlier, the researchers attempted to minimize the risk of skin reaction through a multi-step approach to the application of the tape including the use of barrier wipes to provide a protective coating for the skin and the application of hypoallergenic woven tape beneath the rigid strapping tape. The consequent high rate of skin reaction was unexpected given clinical experience and raises issues of whether taping for extended periods over a two-week period is acceptable to patients with shoulder impingement disorders and whether the short-term benefit derived from its use is justifiable given the risks of reaction and complication due to adverse skin responses.
One possible reason for the high rate of skin reaction could be related to the age of the group enrolled in the study. The mean age of participants was 57.9 years, which may make them more prone to fragile skin and skin reactions as a result of removal and reapplication than a younger age group. The dosage of taping applied was equivalent in terms of duration of application to that described by Host16 in her case study of a 40 year-old male in which no adverse effects were reported. However, the 33 year-old subject described in the case study of Schmitt and Snyder-Mackler15 experienced skin reaction to the prolonged use of tape, causing the technique to be discontinued in that case. Further trials with larger sample sizes would allow for identification of subgroups that may benefit from taping without an elevated risk of skin reaction.
One further limitation arose as a consequence of the differential rate of loss to follow-up. Ideally, this pilot study should have been analyzed using an “intention to treat” analysis whereby all participants' data would be included in the final analysis. This is achieved by carrying forward the last observation from withdrawn participants into analysis of subsequent measurement31. However, due to the timeframes used in this study, this meant carrying forward pre-treatment data. As only 6 people from the taping group were available at the 2-week follow-up, almost half of the data analyzed would relate to the pre-treatment status of this group. This in itself would lead to the introduction of considerable bias into the analysis since both groups received active physiotherapy treatment and both groups demonstrated measurable clinical improvements as a result. The loss to follow-up in this pilot study is in itself informative, and the inclusion of this proportion of baseline data in follow-up analysis would only result in a further reduction of power in detecting treatment effects due to taping.
Conclusion
The results of this pilot study suggest a short-term role for scapula taping as an adjunctive treatment in the management of shoulder impingement problems. Taping appears to provide a reduction in pain experienced when assessed by both self-reported measures of function and on active movements. This benefit occurs only while the taping is continued and is not maintained on follow-up. The benefits need to be considered against the risk of adverse skin reaction to taping in each patient.
Acknowledgement
The authors would like to thank the Division of Allied Health, Hunter Area Health Service, Australia, for its financial support of this pilot study.
Footnotes
This study was supported by a research grant from the Division of Allied Health, Hunter Area Health Service, New South Wales, Australia.
REFERENCES
- 1.Lukasiewicz A, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574–586. doi: 10.2519/jospt.1999.29.10.574. [DOI] [PubMed] [Google Scholar]
- 2.van der Windt DA, Koes BW, Boeke AJ, Deville W, de Jong BA, Bouter LM. Shoulder disorders in general practice: Prognostic indicators of outcome. Br J General Practice. 1996;46:519–523. [PMC free article] [PubMed] [Google Scholar]
- 3.Vecchio P, Kavanagh R, Hazleman BL, King RH. Shoulder pain in a community-based rheumatology clinic. Br J Rheumatol. 1995;34:440–442. doi: 10.1093/rheumatology/34.5.440. [DOI] [PubMed] [Google Scholar]
- 4.Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech. 2003;18:369–379. doi: 10.1016/s0268-0033(03)00047-0. [DOI] [PubMed] [Google Scholar]
- 5.Ludewig P, Cook T. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 6.Ryan S, Magarey M, Jones M. "ree-dimensional analysis of scapula position. Proceedings of Manipulative Physiotherapists Association of Australia Tenth Biennial Conference 1997; 175–176.
- 7.Warner JP, Miceli LJ, Arslanian LE, Kennedy J, Kennedy R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. Clin Orthop Relat Res. 1992;285:191–199. [PubMed] [Google Scholar]
- 8.Heiko G, Stammberger T, Bonel H, et al. Magnetic-based motion analysis of the shoulder during elevation. Clin Orthop Relat Res. 2000;370:154–163. doi: 10.1097/00003086-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Mottram SL. Dynamic stability of the scapula. Man Ther. 1997;2:123–131. doi: 10.1054/math.1997.0292. [DOI] [PubMed] [Google Scholar]
- 10.Hess SA. Functional stability of the shoulder joint. Man Ther. 2000;5:63–71. doi: 10.1054/math.2000.0241. [DOI] [PubMed] [Google Scholar]
- 11.Lewis J, Green A, Reichard Z, Wright C. Scapular position: The validity of skin surface palpation. Man Ther. 2002;7:26–30. doi: 10.1054/math.2001.0405. [DOI] [PubMed] [Google Scholar]
- 12.Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain (Review) The Cochrane Database Syst Rev. 2003;2:CDOO4258. doi: 10.1002/14651858.CD004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jonsson P, Wahlstrom P, Ohberg L, Alfredson H. Eccentric training in chronic painful impingement syndrome of the shoulder: Results of a pilot study. Knee Surg Sports Traumatol Arthrosc. 2006;14:76–81. doi: 10.1007/s00167-004-0611-8. [DOI] [PubMed] [Google Scholar]
- 14.Haahr JP, Andersen JH. Exercises may be as efficient as subacromial decompression inpatients with subacromial stage II impingement: 4–8 years' follow-up in a prospective, randomized study. Scand J Rheumatol. 2006;35:224–228. doi: 10.1080/03009740600556167. [DOI] [PubMed] [Google Scholar]
- 15.Schmitt L, Snyder-Mackler L. Role of scapula stabilizers in etiology and treatment of impingement syndrome. J Orthop Sports Phys Ther. 1999;29:331–338. doi: 10.2519/jospt.1999.29.1.31. [DOI] [PubMed] [Google Scholar]
- 16.Host H. Scapula taping in the treatment of anterior shoulder impingement. Phys Ther. 1995;75:803–812. doi: 10.1093/ptj/75.9.803. [DOI] [PubMed] [Google Scholar]
- 17.van den Dolder PA, Roberts DL. A trial into the effectiveness of soft tissue massage in the treatment of shoulder pain. Aust J Physiother. 2003;49:183–188. doi: 10.1016/s0004-9514(14)60238-5. [DOI] [PubMed] [Google Scholar]
- 18.Conroy DE, Hayes KW. The effect of joint mobilization as a component of comprehensive treatment for primary shoulder impingement syndrome. J Orthop Sports Phys Ther. 1998;28:3–14. doi: 10.2519/jospt.1998.28.1.3. [DOI] [PubMed] [Google Scholar]
- 19.Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther. 2000;30:126–137. doi: 10.2519/jospt.2000.30.3.126. [DOI] [PubMed] [Google Scholar]
- 20.Alexander CM, Stynes S, Thomas A, Lewis J, Harrison PJ. Does tape facilitate or inhibit the lower fibres of trapezius? Man Ther. 2003;8:37–41. doi: 10.1054/math.2002.0485. [DOI] [PubMed] [Google Scholar]
- 21.Cools AM, Witvrouw EE, Danneels LA, Cambier DC. Does taping influence electromyographic muscle activity in the scapular rotators in healthy subjects? Man Ther. 2002;7:154–162. doi: 10.1054/math.2002.0464. [DOI] [PubMed] [Google Scholar]
- 22.Zanella PW, Willey SM, Seibel SL, Hughes CJ. The effect of scapular taping on shoulder joint repositioning. J Sport Rehabil. 2001;10:113–123. [Google Scholar]
- 23.Smith MJ, Sparkes V. The immediate effect of scapular taping on surface electromyographic activity of the scapular rotators in swimmers with subacromial impingement symptoms. Phys Ther Sport. 2006;7:171. [Google Scholar]
- 24.Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med. 1980;8:151–158. doi: 10.1177/036354658000800302. [DOI] [PubMed] [Google Scholar]
- 25.Mitsch J, Casey J, McKinnis R, Kegerreis S, Stikeleather J. Investigation of a consistent pattern of motion restriction in patients with adhesive capsulitis. J Man Manip Ther. 2004;12:153–159. [Google Scholar]
- 26.Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res. 1991;4:143–149. [PubMed] [Google Scholar]
- 27.Heald SL, Riddle DL, Lamb RL. The shoulder pain and disability index: The construct validity and responsiveness of a region-specific disability measure. Phys Ther. 1997;77:1079–1089. doi: 10.1093/ptj/77.10.1079. [DOI] [PubMed] [Google Scholar]
- 28.Williams JW, Holleman DR, Jr, Simel DL. Measuring shoulder function with the shoulder pain and disability index. J Rheumatol. 1995;22:727–732. [PubMed] [Google Scholar]
- 29.Green S, Buchbinder R, Forbes A, Bellamy N. A standardized protocol for measurement of movement of the shoulder using the Plurimeter-V inclinometer and assessment of its intrarater and interrater reliability. Arthritis Care Res. 1998;11:43–52. doi: 10.1002/art.1790110108. [DOI] [PubMed] [Google Scholar]
- 30.Bin Park H, Yokota A, Gill H, Rassi G, McFarland E. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Jt Surg Am. 2005;87A:1446–1455. doi: 10.2106/JBJS.D.02335. [DOI] [PubMed] [Google Scholar]
- 31.Shao J, Zhong B. Last observation carryforward and last observation analysis. Statist Med. 2003;22:2429–2441. doi: 10.1002/sim.1519. [DOI] [PubMed] [Google Scholar]