Abstract
Background
As life expectancies rise and the number of persons over age 75 in the population increases, the proper treatment of elderly cardiac patients is becoming a matter of ever greater medical and political importance.
Methods
In collaboration with the German Federal Quality Assurance Office (Bundesgeschäftsstelle Qualitätssicherung, BQS), the authors analyzed the risk profiles of elderly patients by means of data sets from all cardiac surgical centers in Germany for the year 2007. The results regarding risk distribution and the morbidity and lethality statistics for isolated coronary surgery were derived from the complete, nationwide BQS data pool, containing information on a total of 47,881 operations. Data on quality of life and long-term survival were obtained from a selective literature search using Medline.
Results
Compared to patients under age 65, those over age 75 have significantly more prognosis-determining comorbidities and risk factors. Accordingly, complication rates and lethality are higher in the latter age group (for example, there is a 4.3-fold relative risk elevation for renal dysfunction, a 3.0-fold elevation for neurological complications, and 3.7-fold elevation for in-hospital lethality). The patient’s chronological age is a risk factor for lethality and morbidity after coronary surgical procedures.
Conclusions
The lethality risk of a bypass operation can be predicted very accurately with the aid of modern scoring systems. Successful cardiac surgical procedures can return the patient to a normal life expectancy and quality of life for his or her age group.
Keywords: demographic trends, life expectancy, coronary heart disease, cardiac surgery, health economics
Demographic change presents great challenges to medicine. Especially heart disease has become more common as people live longer. In addition to other age related physiological changes to the coronary vasculature, calcium concentrations increase between the 40th and 70th year of life by a factor of 500 (1). As a result, the incidence of symptomatic coronary heart disease (CHD), myocardial infarction (MI), and sudden cardiac death increases. With a higher life expectancy and an ever increasing number of persons older than 75 in the total population, adequate healthcare provision for elderly persons with heart disease presents not only a medical challenge but is also of great health political importance. The associated questions relating to health economics, resource provision, and medical ethics make high demands on the competence of medical professionals as well as those who carry the political responsibility.
This review article provides an overview of the extent to which risk is increased in heart surgery in elderly people. The authors present original data from Germany, which they analyzed in collaboration with the German Federal Office for Quality Assurance (Bundesgeschäftsstelle Qualitätssicherung, BQS). From the BQS’s complete data set on isolated coronary surgery for the year 2007, the risk distribution and morbidity and mortality statistics were analyzed with regard to age related problems. Participation in quality assurance is compulsory for all German hospitals for cardiac surgery, so that the real situation is reflected in the data. Further, the authors conducted a selective literature search for original articles in Medline, using the search terms "octogenarians" AND "quality of life" AND "cardiac surgery" AND "long term survival". The articles had to give results for postoperative survival and quality of life. In conclusion, an outlook is given of recent developments in cardiac surgery, which may lead to further risk reduction in the treatment of elderly patients.
Age and mortality trends
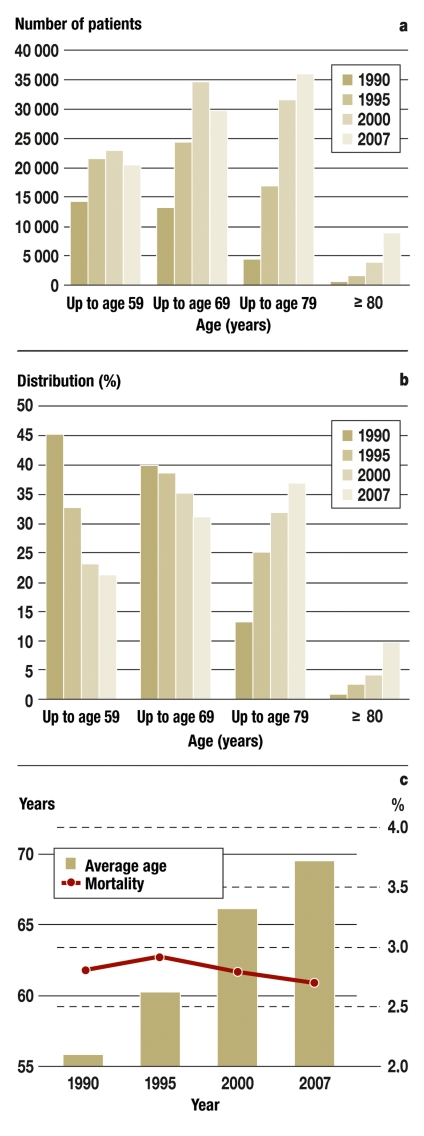
Until the late 1980s, cardiac surgery was mainly restricted to patients younger than 65, but the proportion of older patients has risen steadily in the following years (Figure 1). In Germany, the average age of cardiac surgical patients increased from 1990 to 2007 from 55.8 years to 68.8 years; the proportion of patients older than 80 is 9.8% (2).
Figure 1. Age distribution in cardiac surgery in adults from 1990 to 2007.
a) Absolute numbers in age groups: 20–59 years, 60–69 years, 70–79 years, 80 years and older. The age group of the 70- to 79-year-olds increased 7-fold over the time period, and that of people older than 80, 24-fold.
b) Proportional distribution in the respective age group. The age group of 70- to 79-year-olds was the largest cohort in 2007.
c) Increase in average age of all operated patients with isolated bypass operations from 1990 to 2007. 1990: n=23 733; 1995: n=51 698; 2000: n=61 997; 2007: n=49 788; Mortality: 1990=2.8%, 1995=2.9%, 2000=2.8%, 2007=2.7%. Source: German Society for Thoracic and Cardiovascular Surgery
Many studies have shown a correlation between age and morbidity and mortality risk (3). When comparing 60 year olds with 80 year olds, the effect of age on surgical mortality is lowest for isolated aortic valve replacement, whereas the risk is 3.7-fold increased for isolated bypass grafting (in-hospital mortality <65 years = 1.5%; >74 years = 5.6%).
Especially the combination of bypass operation and mitral valve replacement seems to be associated with a high mortality risk in older patients (19.6%) (4). The methods used in surgery, anesthesia, and intensive care have been refined in recent years to the point where, in spite of more heart operations in older patients, the surgical mortality of bypass operations was kept constant, at 2.9% in 1990 and 2.7% in 2007 (Figure 1c).
Comorbidities and risk factors
An open questions concerns the disease independent influence of the biological aging process and therefore the cellular and tissue aging process on the operative risk. Thus far, a physiological paremeter that characterizes the biological age related changes is lacking. Chronological age is therefore the only measurable variable that may be used as a parameter, which can be assigned to the patient’s aging process. On the basis of existing data, it can be assumed that chronological age is a risk factor for morbidity and mortality after cardiac surgery. Compared with an age <65 years, the odds ratio for the mortality risk is 1.7 for 65- to 74-year-olds, 3.18 for 75- to 84-year-olds, and 5.85 for people older than 85 years. Notably, the individual biological age may deviate from the chronological age and is modified to a hitherto unknown degree by comorbidities (diabetes mellitus, renal failure), health oriented behaviors, and genetic predisposition (5). In general, the number of comorbidities that determine the prognosis increases with chronological age (Table 1). An operative risk that is already raised due to age is further raised due to comorbidities. As can be seen in Table 1, almost all relevant risk factors are represented in the older group to a significantly higher degree than in the younger group. By identifying risk factors and quantifying their importance in recent years, scoring systems have been developed for cardiac surgery that enable a preoperative assessment of the mortality risk. The scoring system KCH score 2.0 was most recently standardized for German data by the BQS for 2007 (6). It has a high predictive value for operations in Germany, whereas older scoring systems, such as the EURO score, possibly substantially overestimate the probability of death. The relevance of risk factors according to the KCH score is shown in Table 1 as odds ratios in the second column. If younger (<65 years) and older (75–84 years) patients have comparable risks with regard to the risk factors listed in Table 1 then the likelihood of dying is increased 3.18-fold for older patients. The odds ratio for patients older than 85 is thus 5.85 (Box).
Table 1. Risk factors and comorbidities of young and elderly patients (2007).
| Risk factor | Odds ratio according to KCH score | Regression coefficient according to KCH score | Prevalence of risk factor in the age group 20–64 years (n = 15 794) | Prevalence of risk factor in the age group ≥ 75 years (n = 11 427) | Comparison of prevalence in the age groups |
| Left ventricular ejection fraction (LVEF) <30% | 2.78 | 1.024 | 8.50% | 8.00% | n/s |
| Critical preoperative condition | 2.43 | 0.889 | 9.7% | 11.0% | p < 0.001 |
| Heart failure NYHA IV | 2.32 | 0.842 | 10.3% | 11.7% | p < 0.001 |
| Renal failure | 2.18 | 0.780 | 2.8% | 4.6% | p < 0.001 |
| Reoperations on heart/aorta | 1.97 | 0.677 | 3.8% | 5.2% | p < 0.001 |
| Emergency | 1.93 | 0.658 | 12.0% | 13.8% | p < 0.001 |
| Other cardiac arrhythmias | 1.93 | 0.655 | 1.2% | 3.4% | p < 0.001 |
| BMI <20 | 1.72 | 0.541 | 1.2% | 1.6% | p < 0.05 |
| Pulmonary hypertension | 1.69 | 0.525 | 1.7% | 3.7% | p < 0.001 |
| LVEF 30–50% | 1.59 | 0.466 | 27.9% | 33.0% | p < 0.001 |
| Arterial vascular disorders | 1.59 | 0.461 | 16.5% | 25.4% | p < 0.001 |
| Other pulmonary disorders | 1.57 | 0.454 | 2.2% | 2.6% | p < 0.05 |
| Heart failure NYHA III | 1.48 | 0.389 | 44.3% | 51.1% | p < 0.001 |
| Female sex | 1.31 | 0.269 | 15.1% | 32.8% | p < 0.001 |
| Pulmonary disorder: COPD | 1.30 | 0.261 | 8.2% | 11.7% | p < 0.001 |
| Heart rhythm: atrial fibrillation | 1.30 | 0.259 | 2.0% | 9.1% | p < 0.001 |
| Troponin positive | 1.26 | 0.235 | 13.9% | 15.6% | p < 0.001 |
| Myocardial infarction <21 days earlier | 1.24 | 0.215 | 20.1% | 23.6% | p < 0.001 |
| Diabetes mellitus (insulin) | 1.22 | 0.201 | 12.4% | 13.1% | n/s |
LVEF, left ventricular ejection fraction; BMI, body mass index; n/s, non-significant Source: Bundesgeschäftsstelle für Qualitätssicherung (BQS, German Federal Quality Assurance Office), 2008
Box. Determining the age dependent mortality risk with the KCH score (version 2.0) of the German Federal Quality Assurance Office (example).
If a younger (64) female patient and an older one (79) have comparable risks (being female, NYHA III, pulmonary hypertension, LVEF 30–50%, atrial fibrillation, arterial vascular disease), then, according to the KCH score, the expected in-hospital mortality for the younger patient is 2.4% to 3.9% and for the older patient, 9.9% to 15.3%. The age related difference is about 3-fold.
Alexander et al. reach the same conclusions in the hitherto largest field study, which included 67 764 patients (4743 older than 80 years) (4). The authors found that hospital mortality in older patients without important comorbidities was 3.8 times that of the younger patient group. In patients with severe comorbidities the importance of age disappears. In these, the mortality risk was mainly determined by the number and severity of the comorbidities.
Some retrospective analyses gave little importance to the factor age and concluded that higher mortality in older patients was caused by their risk factors, for example, renal failure (4, 5, 7). In spite of the heterogeneous study situation between large field studies on the one hand and a few single-center retrospective analyses on the other, the variable "chronological age" is included in all scoring systems as an independent risk factor. This is also taken into consideration in the (older) EURO score, which allocates risk points for every five years after the 55th year of life (8, 9).
A special situation is emergency surgery in cardiogenic shock after myocardial infarction, which has a particularly poor prognosis at an old age. Metha et al. have reported mortality rates of 31.9% in the age group >80 years (10).
Postoperative complications
In the BQS data for 2007, the complication rate after cardiac surgical procedures in patients older than 75 is notably higher than in younger patients (table 2). This particularly concerns severe complications such as renal failure (0.9% vs 3.9%, p<0.001), stroke (0.6% vs 1.8%, p<0.001), and respiratory complications (3.0% vs 7.1%, p<0.001). Correspondingly, extended periods on the ventilator (7.4% vs 16.0%), stays in intensive care ≥ 4 days (18.8% vs 33.8%), and the need for dialysis (0.8% vs 2.8%) are much more common.
Table 2. Frequency of postoperative complications in young versus elderly patients.
| Postoperative complication | Age 20–64 years (n = 15 794) | Age ≥ 75 years (n = 11 427) | p-value | Relative risk increase |
| Impaired retention | 0.9% | 3.9% | p < 0.001 | 4.3 |
| Dialysis | 0.8% | 2.8% | p < 0.001 | 3.5 |
| Neurological complications | 0.6% | 1.8% | p < 0.001 | 3.0 |
| Reintubation | 3.0% | 7.1% | p < 0.001 | 2.4 |
| Postoperative ventilation >24 h | 7.4% | 16.0% | p < 0.001 | 2.2 |
| Stay in intensive care ≥ 4 days | 18.8% | 33.8% | p < 0.001 | 1.8 |
| Donor blood | 39.0% | 63.0% | p < 0.001 | 1.6 |
| In-hospital mortality | 1.5% | 5.6% | p < 0.001 | 3.7 |
Bundesgeschäftsstelle für Qualitätssicherung (BQS, German Federal Quality Assurance Office), 2008
In the registry study by Alexander et al., severe complications such as renal failure, stroke, and cardiac pump failure were also 4 times higher in patients over age 80 years compared to those under age 65 years (4).
Life expectancy
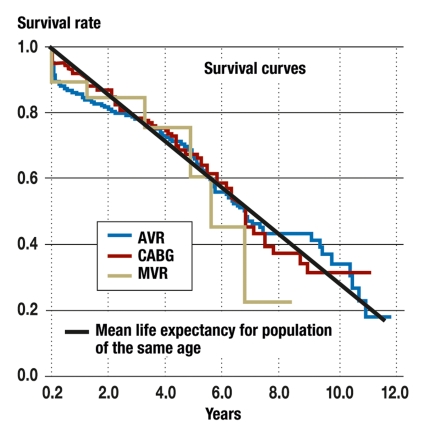
The determining factors for the long term prognosis are the number and severity of comorbidities. Extrapolated to the total population, even elderly patients can regain their normal life expectancy after successful surgery. This is particularly so for patients whose left ventricular function was maintained (11, 12).
Isolated bypass surgery and isolated aortic valve replacement have an excellent long term survival prognosis, whereas patients have a comparatively lower survival interval after mitral valve operations. The genesis of the mitral valve disease is the decisive factor. Myxomatous degeneration with intact left ventricular function has a high survival rate, whereas ischemic mitral insufficiency that is accompanied by reduced left ventricular function is associated with a notably lower survival rate (13).
Further to the risk factor "reduced cardiac function," high grade renal impairment severely limits long term survival after cardiac surgery.
The advantage of revascularization therapy
A prospective randomized study that investigates medical or interventional therapy compared with surgical revascularization in older patients has thus far not been conducted. Two studies, however, have given an indication that invasive revascularization therapy is more beneficial. A retrospective analysis of 6000 patients (APPROACH study) and the prospectively randomized TIME study, which included 300 patients, investigated optimal medical therapy with invasive revalcularization in older patients with symptomatic angina pectoris. The data from the APPROACH study show advantages of invasive revascularization even in older patients (percutaneous coronary intervention [PCI] or bypass surgery [CABG]) compared with medical treatment. In the group of patients older than 80, the survival rater after 4 years was 77.4% in the revascularization group and 60.3% in the medical treatment group. Interestingly, the gain from invasive revascularization was greater at a higher age than in patients younger than 70. The number needed to treat (NNT) to prevent one death for invasive revascularization compared with medical treatment was 33.1 in patients younger than 70 in the PCI group and 23.4 in the CABG group; in patients older than 80, the NNT for the PCI group was 8.9 and for the CABG group, 5.9. The authors concluded that "age alone should not be a deterrent to performing invasive revascularization" (14).
The results of the randomized TIME study also underline the importance of invasive revascularization in symptomatic patients. The necessity of repeated hospitalization was significantly lower after revascularization, even though long term survival and quality of life after 4.2 years did not differ in the intention-to-treat analysis. It should be mentioned, however, that in the long term, 46% of patients from the conservative arm did have invasive revascularization and survived significantly longer because of it (15). Revascularization in symptomatic patients should be attempted with an appropriate procedure in older patients while taking into consideration the risk constellation. This is laid down in the national disease management guideline on coronary artery disease (16).
Aortic valve replacement in elderly patients
Varadarajan et al., in a retrospective cohort study, showed that even in patients older than 80 who have severe aortic stenosis, surgery can increase life expectancy substantially (17). The patients’ chronological age alone should not be an exclusion criterion for aortic valve replacement.
For very old patients with a high operative risk, valve replacement through a transapical access without use of the heart-lung machine seems to be a good treatment alternative. Current results from experienced centers indicate that good functional results can be achieved while the complication rate remains acceptable (18).
Quality of life after cardiac surgery
Whether a particular therapy finds acceptance depends on whether patients can expect a good quality of life after the treatment. This is especially the case for very invasive procedures in elderly patients. In recent years, an increasing number of scientific studies have focused on the aspects of quality of life after cardiac surgical procedures. Quality of life includes the patient’s return to their familiar environment and regaining autonomy. Yager and Robinson, in an editorial in the American Heart Journal, comment on a retrospective analysis by Rady and colleagues and pose critical questions about preoperative risk communication. Rady et al., in their original article—suitably entitled: Cardiac surgery for octogenarians: is it an informed decision?—reported about a high proportion of patients who had to be admitted to nursing care after their operation, at least temporarily (19). Even though this is confirmed by a minority of studies, one has to assume that elderly patients are at risk of losing their autonomy and familiar environment after the operation. This raises the following important questions:
Can the quality of life and the prognosis be substantially improved by cardiac surgery?
Are patients in a position to make an informed decision in favor of or against the procedure after the physician has explained possible benefits and risks in a balanced manner when providing information?
Clinicians need to define the indication with the patient in mind—beyond the principal need for surgery—by taking into consideration further biological, psychological, and emotional factors, so as to advise patients on their individual case. Apart from the personal experience of the experienced surgeon, no further objective criteria are available. At this point, further, joint research with geriatricians might define parameters that make it easier to assess the individual potential and thus create the conditions to achieve yet better results in elderly patients.
In spite of the caution with which the results of the retrospective APPROACH study should be interpreted, it can be stated that surgical revascularization treatment in patients older than 80 achieved excellent quality of life and, in particular, a high degree of satisfaction, even 3 years on (20).
Huber et al. analyzed the postoperative quality of life in 136 patients with a mean age of 82 years (Figure 2). A significant reduction in cardiac symptoms in 93% of patients, no complaints in the preceding 4 weeks in 90%, and satisfaction with treatment in 94% all speak in favor of the surgical intervention (12).
Figure 2.
Long term survival after cardiac surgical procedures in elderly patients compared with normal life expectancy in Germany. The figure was modified from Schmidtler et al. (Thorac and Cardiovasc Surg 2008; 56: 14–19), and data from the Federal Statistical Office were added. AVR=aortic valve replacement, CABG=coronary artery bypass grafting; MVR=mitral valve replacement
Outlook
Studies thus far have shown that elderly patients can be operated on with an acceptable mortality risk. However, comparative studies are needed that take into account the specific risks in elderly patients (for example, stroke) and compare less invasive surgical procedures, such as surgery without heart-lung machine (OPCAB, off-pump coronary artery bypass surgery) (21, 22), with conventional procedures. Retrospective analyses have shown an advantage of off-pump surgery in elderly patients (23). It seems plausible that in patients at high risk, operating without the invasive heart-lung machine and the trauma of clamping the (atherosclerosed) ascending aorta, might lower the rate of postoperative complications (24). The authors are looking forward to the results from the new GOPCABE study, which is ongoing and compares in a randomized design revascularization without heart-lung machine with the conventional technique in elderly patients.
If the operative risk is very high, hybrid revascularization should be considered. In patients with coronary heart disease, the anterior interventricular ramus is grafted with the left internal thoracic artery in a minimally invasive procedure, and in a second step, stents are implanted into further stenosed vessels. Randomized comparative data on this technique are thus far lacking. Interestingly, elderly patients benefit from grafting the anterior interventricular ramus with the internal thoracic artery with regard to their survival prognosis (25).
Future studies should aim to find the optimum therapy for elderly patients. To this end, it seems necessary to identify from the multitude of biological, psychological, and emotional factors the ones that substantially influence the postoperative result. The care of elderly cardiac surgical patients can be improved only through the interplay of anesthesia, cardiology, geriatrics, and cardiac surgery. Adapting the treatment to the individual patient is crucial. Generally it has to be said that the medical and financial costs of cardiac surgery in older patients are much higher than in younger ones. The political and ethical decision to guarantee all social strata medically indicated and necessary treatments from the resources of the social insurance systems therefore implies the coverage of any such costs.
Key messages.
The number of cardiac surgery patients older than 70 years has increased 7-fold in the past 17 years, and that of patients older than 80 years, 24-fold.
The increased morbidity and mortality after cardiac surgical procedures in elderly patients is due to biological aging processes, but also to the higher prevalence of comorbidities.
Even in patients older than 75 years, normal life expectancy can be restored by an operation.
Postoperative quality of life and the satisfaction with the surgical treatment is good, even in elderly patients.
Less invasive surgical techniques offer a therapeutic option for high risk patients.
Acknowledgments
Translated from the original German by Dr Birte Twisselmann.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Dakik HA, Skouri HN, Mehio-Sibai A, et al. Prevalence of coronary artery calcium among asymptomatic men and women in a developing country: comparison with the USA data. Atherosclerosis. 2005;183:141–145. doi: 10.1016/j.atherosclerosis.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 2.Bruckenberger E. 20 Herzbericht 2007. http://www.bruckenberger.de.
- 3.Trummer G, Beyersdorf F. Heart surgery in the elderly. Dtsch Med Wochenschr. 2005;130:731–734. doi: 10.1055/s-2005-865088. [DOI] [PubMed] [Google Scholar]
- 4.Alexander KP, Anstrom KJ, Muhlbaier LH, et al. Outcomes of cardiac surgery in patients > or = 80 years: results from the National Cardiovascular Network. J Am Coll Cardiol. 2000;35:731–738. doi: 10.1016/s0735-1097(99)00606-3. [DOI] [PubMed] [Google Scholar]
- 5.Baskett R, Buth K, Ghali W, et al. Outcomes in octogenarians undergoing coronary artery bypass grafting. Cmaj. 2005;172:1183–1186. doi: 10.1503/cmaj.1041342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.BQS, Bundesgeschäftsstelle Qualitätssicherung gGmbH 2008. Risikoadjustierung der In-Hospital-Letalität mit dem logistischen KCH-SCORE 2.0. http://www.bqs-outcome.de/2007/ergebnisse/leistungsbereiche/koronarchirurgie/buaw/risikoadjustierung.
- 7.Stoica S, Cafferty F, Kitcat J, et al. Octogenarians undergoing cardiac surgery outlive their peers—a case for early referral. Heart. 2006;92(4):503–506. doi: 10.1136/hrt.2005.064451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson WM, Smith JM, Woods SE, Hendy MP, Hiratzka LF. Cardiac surgery in octogenarians: does age alone influence outcomes? Arch Surg. 2005;140:1089–1093. doi: 10.1001/archsurg.140.11.1089. [DOI] [PubMed] [Google Scholar]
- 9.Roques F, Nashef SA, Michel P, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19 030 patients. Eur J Cardiothorac Surg. 1999;15:816–822. doi: 10.1016/s1010-7940(99)00106-2. discussion 22-3. [DOI] [PubMed] [Google Scholar]
- 10.Mehta RH, Eagle KA, Coombs LP, et al. Influence of age on outcomes in patients undergoing mitral valve replacement. Ann Thorac Surg. 2002;74:1459–1467. doi: 10.1016/s0003-4975(02)03928-0. [DOI] [PubMed] [Google Scholar]
- 11.Schmidtler FW, Tischler I, Lieber M, et al. Cardiac surgery for octogenarians - a suitable procedure? Twelve-year operative and post-hospital mortality in 641 patients over 80 years of age. Thorac Cardiovasc Surg. 2008;56:14–19. doi: 10.1055/s-2007-965642. [DOI] [PubMed] [Google Scholar]
- 12.Huber CH, Goeber V, Berdat P, Carrel T, Eckstein F. Benefits of cardiac surgery in octogenarians—a postoperative quality of life assessment. Eur J Cardiothorac Surg. 2007;31:1099–1105. doi: 10.1016/j.ejcts.2007.01.055. [DOI] [PubMed] [Google Scholar]
- 13.DiGregorio V, Zehr KJ, Orszulak TA, et al. Results of mitral surgery in octogenarians with isolated nonrheumatic mitral regurgitation. Ann Thorac Surg. 2004;78:807–813. doi: 10.1016/j.athoracsur.2004.03.041. discussion 13-4. [DOI] [PubMed] [Google Scholar]
- 14.Pfisterer M. Long-term outcome in elderly patients with chronic angina managed invasively versus by optimized medical therapy: four-year follow-up of the randomized Trial of Invasive versus Medical therapy in Elderly patients (TIME) Circulation. 2004;110:1213–1218. doi: 10.1161/01.CIR.0000140983.69571.BA. [DOI] [PubMed] [Google Scholar]
- 15.Graham MM, Ghali WA, Faris PD, Galbraith PD, Norris CM, Knudtson ML. Survival after coronary revascularization in the elderly. Circulation. 2002;105:2378–2384. doi: 10.1161/01.cir.0000016640.99114.3d. [DOI] [PubMed] [Google Scholar]
- 16.Ollenschläger G, Lelgemann M, Kopp I. The German Program for Disease Management Guidelines: CHD Guideline 2006. Med Klin. 2006;101:993–998. doi: 10.1007/s00063-006-1130-9. [DOI] [PubMed] [Google Scholar]
- 17.Varadarajan P, Kapoor N, Bansal RC, Pai RG. Survival in elderly patients with severe aortic stenosis is dramatically improved by aortic valve replacement: results from a cohort of 277 patients aged > or = 80 years. Eur J Cardiothorac Surg. 2006;30:722–727. doi: 10.1016/j.ejcts.2006.07.028. [DOI] [PubMed] [Google Scholar]
- 18.Walther T, Simon P, Dewey T, et al. Transapical minimally invasive aortic valve implantation: multicenter experience. Circulation. 2007;116(11 Suppl):240–245. doi: 10.1161/CIRCULATIONAHA.106.677237. [DOI] [PubMed] [Google Scholar]
- 19.Yager JE, Peterson ED. Cardiac surgery in octogenarians: have we gone too far … or not far enough? Am Heart J. 2004;147:187–189. doi: 10.1016/j.ahj.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Graham MM, Norris CM, Galbraith PD, Knudtson ML, Ghali WA. Quality of life after coronary revascularization in the elderly. Eur Heart J. 2006;27:1690–1698. doi: 10.1093/eurheartj/ehl038. [DOI] [PubMed] [Google Scholar]
- 21.Hake U, Dahm M, Böning A, Massoudy P, Schmitz C, Tzanova I. Koronaroperationen ohne Herz-Lungen-Maschine. Dtsch Arztebl. 2007;104(30):2127–2132. [Google Scholar]
- 22.Klotz S, Scheld H. Moderne Verfahren in der operativen Myokardrevaskularisierung. Dtsch Arztebl. 2007;104(48):3334–3339. [Google Scholar]
- 23.Demaria RG, Carrier M, Fortier S, et al. Reduced mortality and strokes with off-pump coronary artery bypass grafting surgery in octogenarians. Circulation. 2002;106(12 Suppl 1):5–10. [PubMed] [Google Scholar]
- 24.Bolotin G, Shapira Y, Gotler Y, et al. The potential advantage of „no-touch“ aortic technique in off-pump complete arterial revascularization. Int J Cardiol. 2007;114:11–15. doi: 10.1016/j.ijcard.2005.11.107. [DOI] [PubMed] [Google Scholar]
- 25.Moon MR, Sundt TM, Pasque MK, Barner HB, Gay WA, Jr, Damiano RJ., Jr Influence of internal mammary artery grafting and completeness of revascularization on long-term outcome in octogenarians. Ann Thorac Surg. 2001;72:2003–2007. doi: 10.1016/s0003-4975(01)03144-7. [DOI] [PubMed] [Google Scholar]