Abstract
Spinal histoplasmosis is a rare disease condition that must be differentiated from other common inflammatory lesions of the spine such as tuberculosis. A case is presented of a pathologically proven African spinal hisptoplasmosis in a 39-year old female.
Paraplegia and fever were the patient clinical fingings. Cervical plain radiography demonstrated a lytic destructive process of the lower cervical spine with radiographic signs similar to tuberculosis. The surgical management and chemotherapy of histoplasmosis are breifly discussed.
Keywords: African histoplasmosis, spine, radiology, histopathology
Introduction
Although African histoplasmosis has a predilection for bones, spinal involvement is rare1. Only a few cases are reported in the recent literature. This report is presented because of the rare localisation of the disease and the similar radiological signs to tuberculous spondylitis.
Case Report
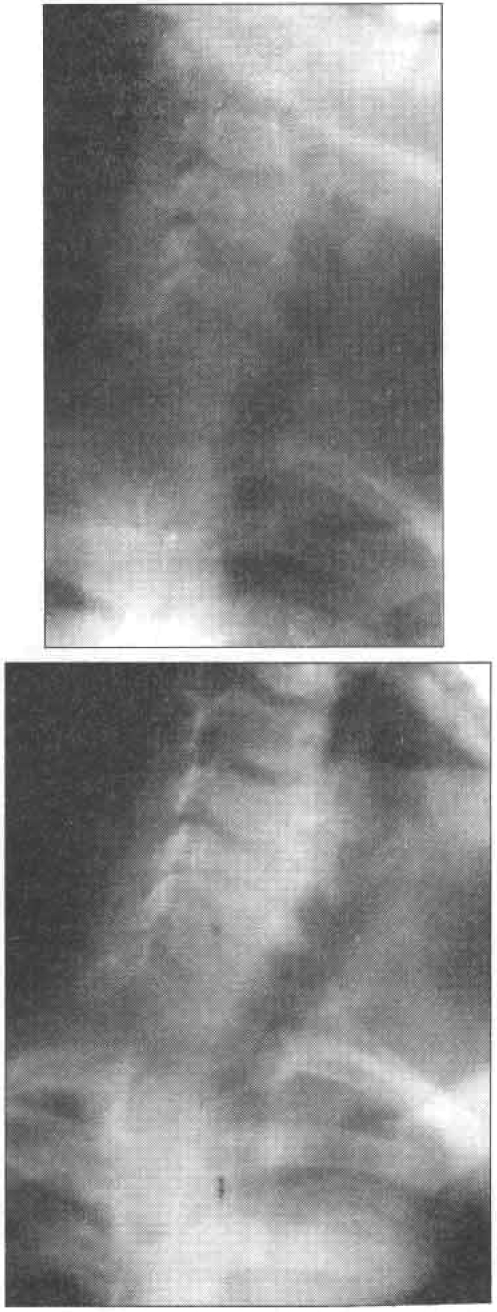
A 39-year old female of unknown HIV-Sero status was admitted to Mulago Hospital as a referral from an up country hospital with a 5 month-history of weight loss, fluctuating fever, weakness of the lower limbs and backache. The painful swelling at the back of the neck and paraplegia were of recent occurrence of 1 - month and 2 weeks duration respectively. The initial plain cervical radiographs (Fig. 1 and 2) revealed a destructive osteolytic process involving the vertebral bodies and posterior elements of C4–C6 with marked reduction in height of the respective intervetebral disc spaces. A tentative diagnosis of tuberculosis spondylitis was made while under attention of the referring clinician. Because of scarcity of laboratory facilities in that centre, the patient was on tuberculosis trial treatment. During the 2-weeks when the patient was on treatment, her condition deteriorated and she was referred. On clinical evaluation, she was noted to be sick looking with extensive oral thrush and fungal paronychial. The significant findings were in he neuro-musco-skeletal system. In addition to the cervical swelling, increased tone, hyperreflema and sustained ankle clonus were noted. The sensory level was at T1/T2.
Figures 1 & 2 Destructive lytic process involving the vertebral bodies and posterior elements and intervening discs at C4–C6
In view of the clinical and radiological findings, the orthopaedic surgeon opted for surgical management. Using a dorsal approach, a large purulent fluid collection with yellow granules was drained. The cervical vertebrae C4–C6 were noted to be loose.
The bone specimen and purulent fluid collection were sent for histopathological analysis. Histo pathologically Histoplasma dubious was isolated from the former and coliforms pseudomonas from the latter. The patient was treated with rifampicin and Ketoconazole according to culture and sensitivity results. She was discharged in brace and wheel chair.
Discussion
Histoplasmosis is a fungal infection caused by H. capsulatum and H. Duboissi. The former is common in N. America especially along the Mississippi valley and the latter in equatorial Africa2.
Generally, fungal infection of bone is rare in the temperate climate but relatively common in the tropics especially among people with a primitive life style2. H. Duboissi bas more predilection for bone than H. caspsulatum and commonly affects the ribs and skull but the spine and long bone are rarely involves. 1,2 recent medical literature indicates a close relationship of histopasmosis and acquired immune deficiency syndrome (AIDS) 1,3–6. Unfortunately the immune status of the patient presented is not known. However, the clinical features are suggestive of compromised immunity. Bone histoplasmosis commonly lead to osteolytic lessions1. The skull and spine infections may not be associated with new bone information simulating tuberculosis and osteoltic metastases as in the patient presented 2. Typically well defined and avoid. However in advanced stage, the lesions commonly provoke a periosteal reaction.
Osteolytic metastases were unlikely in the presented case because of the reduction in height of the intervetebral disc spaces. Tuberculosis spondylitis was a possibility though the location is relatively rare. Spinal lesions are reporteed to respond well to antifungal therapy1, 7. In the case presented, the patient improved on antibiotics and antifungals together with open drainage of purulent collection. Unfortunately, the patient was lost to follow up. From this report it can be concluded that spinal African histoplasmosis should be included into the differential diagnosis of osteolytic spinal lesions especially in immune deficient patients.
References
- 1.Geffray L, veyssier P, Cevallos R, Beadud B. African histoplasmosis: clinical and therapeutic aspects relation to AIDS. Apropos of 4 cases, including a case with HIV-1 HLTV-1 co-infection. Ann-Med-Intene-Paris. 1994;145(6):424–427. [PubMed] [Google Scholar]
- 2.Terence PJ, Jeremy PRJ. In: Bone and joint infection Diagnostic Radiology: A text book of medical imaging. Grainger RG, Allison DJ, editors. 1997. pp. 1871–1873. [Google Scholar]
- 3.Chandenier J, Goma D, Moyen G, Samba LMC. African histoplasmosis due to Histoplasma capsulatum:var dubiossi relationship with AIDS in recent Congolese cases. Sante. 1995;5(4):227–234. [PubMed] [Google Scholar]
- 4.Manfred IR, Mazzoni A, Nanett A, Chiodo F. Histoplasmosis capsulati and luboissi in Europe: the impact of HIV pandemic, travel and immigration. Eur - J-Epidemiol. 1994;10(6):675–678. doi: 10.1007/BF01719280. [DOI] [PubMed] [Google Scholar]
- 5.Bone and joint sites of African histoplasmosis (Histoplasms duboissi): A case and review of the literature. Rev-Rhum-Ed-Fr. 1994;61(11):829–838. [PubMed] [Google Scholar]
- 6.Munis A, Habte GE. Disseminated histoplasmosis in a patient from a non endemic area who has acquired immunodeficiency syndrome. South-Med-J. 1995;88(6) doi: 10.1097/00007611-199506000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Kelly DR, Smith CDJ, Quietness MP. Successful medical treatment of a spinal Histoplasma. J Neuromaging. 1994;4(4):237–239. doi: 10.1111/jon199444237. [DOI] [PubMed] [Google Scholar]