Abstract
Multistep and single-step resistance selection studies were performed with razupenem, linezolid, and vancomycin against 10 methicillin (meticillin)-resistant and -susceptible Staphylococcus aureus strains. After 20 daily subcultures, razupenem yielded only clones with MICs of >4 μg/ml in one strain (8 μg/ml) whose parent's MIC was already 4 μg/ml. After 18 to 49 passages in 6/10 strains, razupenem MICs rose from 0.016 to 2 μg/ml (parents) to 0.125 to 8 μg/ml (with clones stable after 10 drug-free subcultures). Single-step mutant selection frequencies were similarly low for razupenem and comparators.
Staphylococcus aureus is becoming increasingly resistant to antibiotics. Additionally, the majority of methicillin (meticillin)-resistant S. aureus (MRSA) (and also some methicillin-susceptible [MSSA]) strains are resistant to all currently available quinolones (1). Heterogeneous vancomycin-intermediate S. aureus (hVISA) and vancomycin-intermediate S. aureus (VISA) strains (1, 5, 7, 8, 11, 12) are increasingly reported, and recently, nine vancomycin-resistant S. aureus (VRSA) strains have been described (1; M. Rybak, personal communication). Two recent papers emphasize the recent spread of VISA strains in Turkey (12) and France (7). Recently, Rybak et al. (11) have indicated, with macro Etest and population analysis testing, that the incidence of hVISA strains has increased over the past 22 years for an overall incidence of 2.2%. Yusof et al. (17) have recently described a double-sided vancomycin/teicoplanin macro Etest strip which accurately differentiates between hVISA and VISA strains. Utilization of this method will increase reports of the incidence of hVISA and VISA strains. As of this time, the pathogenicity of VRSA strains awaits confirmation.
The situation has become further complicated by the appearance and rapid spread, especially in the United States, of community-acquired MRSA strains, which are especially virulent possibly by virtue of the production of Panton-Valentine leukocidin (1). Although these strains are currently more drug susceptible than are hospital-acquired strains, this situation will not remain the same, and increased resistance will develop. Additionally, treatment of the community-acquired MRSA strains with glycopeptides will increase the selective pressure leading to nonsusceptibility to vancomycin and teicoplanin. There is therefore an urgent need for nonglycopeptide drugs with which to treat MRSA strains. Recently, we and others have also documented clinical development of daptomycin resistance after daptomycin therapy (8).
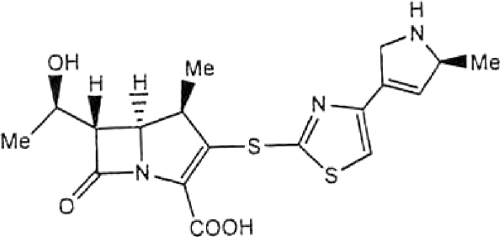
Razupenem (also formerly known as SM-216601, SMP-601, PZ-601, and PTZ601) (Fig. 1) is a new experimental broad-spectrum 2-(4-arylthiazol-2-ylthio)-1β-methylcarbapenem derivative with enhanced activity against gram-positive organisms, including staphylococci, enterococci, and MRSA (9, 10, 14, 15). This study examines the antistaphylococcal activity of razupenem compared to the activities of vancomycin and linezolid, by single- and multistep mutant selection analysis.
FIG. 1.
Chemical structure of razupenem.
Ten isolates were tested by multistep and single-step resistance selection analysis. These included eight MRSA strains, comprising two each of MSSA, MRSA, hVISA, VISA, and VRSA isolates. All organisms except VRSA 509 (Michigan) were recent isolates from patients at Hershey Medical Center. Razupenem powder was obtained from Protez Pharmaceuticals, Inc., Malvern, PA.
The CLSI standard macrodilution method was used for initial MICs (6). Serial passages were performed daily in Mueller-Hinton broth for each strain in subinhibitory concentrations of all antimicrobials. For each subsequent daily passage, an inoculum was taken from the tube 1 to 2 dilutions below the MIC that matched the turbidity of a growth control tube. This inoculum was used to determine the next MIC. Daily passages (minimum of 14) were performed until a significant increase in MIC (>4-fold) was obtained. Stability of the acquired resistance was determined by MIC determinations after 10 daily passages of the variant on blood agar without antibiotics (3, 4). A stable clone is defined as having an MIC after the drug-free passages within ±1 of the MIC before the drug-free passages. Only for razupenem clones were passages continued for the maximum of 50 days, regardless of MIC, as seen in Table 1. For multistep testing, confirmation of parent and resistant clones was done by pulsed-field gel electrophoresis (3, 4).
TABLE 1.
Results of S. aureus multistep resistance selection and daily MIC testing
| Strain | Antibiotic | Initial MIC (μg/ml) | Selected resistancea
|
Retest MIC after 10 antibiotic-free subcultures
|
MIC (μg/ml) at day:
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC (μg/ml) | Pass. | Razupenem | Linezolid | Vancomycin | 5 | 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | |||
| hVISA SA618 | Razupenem | 4 | 8 | 50 | 4 | 4 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | |||
| Linezolid | 4 | 16 | 50 | 4 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | 16 | ||||
| Vancomycin | 2 | 8 | 50 | 4 | 4 | 4 | 8 | 8 | 8 | 8 | 8 | 8 | 8 | ||||
| hVISA SA873 | Razupenem | 2 | 16 | 30 | 8 | 2 | 2 | 2 | 2 | 2 | 4 | 8 | 16 | 16b | 16 | 16 | 16 |
| Linezolid | 2 | 8 | 50 | 4 | 2 | 2 | 4 | 4 | 8 | 8 | 8 | 8 | 8 | ||||
| Vancomycin | 2 | 4 | 50 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 4 | 4 | ||||
| VISA SA555 | Razupenem | 0.5 | 4 | 27 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 4 | 4 | 4 | 8 | 16 |
| Linezolid | 2 | 4 | 50 | 2 | 2 | 2 | 2 | 4 | 4 | 4 | 4 | 4 | 4 | ||||
| Vancomycin | 8 | 8 | 50 | 8 | 8 | 8 | 8 | 8 | 16 | 32 | 32 | 32 | 8 | ||||
| VISA SA1287 | Razupenem | 0.06 | 0.5 | 18 | 0.25 | 8 | 1 | 0.25 | 0.25 | 0.25 | 0.5 | 0.5 | 2 | 2 | 2 | 2 | 4 |
| Linezolid | 4 | 16 | 50 | 8 | 8 | 8 | 8 | 8 | 16 | 16 | 16 | 16 | 16 | ||||
| Vancomycin | 4 | 8 | 50 | 4 | 4 | 8 | 4 | 4 | 4 | 4 | 4 | 8 | 8 | ||||
| MRSA SA525 | Razupenem | 1 | 16 | 28 | 8 | 4 | 2 | 2 | 4 | 4 | 4 | 4 | 16 | 16 | 16 | 32 | 32 |
| Linezolid | 4 | 16 | 50 | 4 | 4 | 16 | 16 | 16 | 16 | 16 | 16 | 16 | 16 | ||||
| Vancomycin | 2 | 8 | 50 | 2 | 4 | 4 | 8 | 4 | 4 | 8 | 16 | 8 | 8 | ||||
| MRSA SA547 | Razupenem | 0.5 | 4 | 23 | 2 | 4 | 2 | 0.5 | 1 | 2 | 4 | 4 | 8 | 16 | 16 | 16 | 16 |
| Linezolid | 4 | 32 | 48 | 0.125 | 32 | 2 | 4 | 4 | 8 | 8 | 16 | 16 | 16 | 16 | 32 | ||
| Vancomycin | 2 | 8 | 50 | 2 | 2 | 4 | 4 | 8 | 4 | 8 | 4 | 4 | 8 | ||||
| MSSA SA540 | Razupenem | 0.016 | 0.125 | 49 | 0.125 | 4 | 2 | 0.016 | 0.016 | 0.03 | 0.03 | 0.03 | 0.06 | 0.06 | 0.06 | 0.06 | 0.125 |
| Linezolid | 4 | 32 | 36 | 0.016 | 16 | 4 | 4 | 4 | 16 | 16 | 16 | 16 | 32 | ||||
| Vancomycin | 4 | 8 | 50 | 4 | 4 | 8 | 8 | 8 | 8 | 8 | 32 | 16 | 8 | ||||
| MSSA SA543 | Razupenem | 0.016 | 0.06 | 50 | 0.03 | 0.03 | 0.03 | 0.03 | 0.03 | 0.06 | 0.06 | 0.06 | 0.06 | 0.06 | |||
| Linezolid | 4 | 32 | 15 | 0.016 | 32 | 2 | 4 | 8 | 32 | ||||||||
| Vancomycin | 2 | 8 | 50 | 2 | 4 | 8 | 8 | 8 | 8 | 8 | 4 | 8 | 8 | ||||
| VRSA SA510 | Razupenem | 1 | 4 | 50 | 2 | 2 | 2 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | |||
| Linezolid | 4 | 16 | 50 | 2 | 4 | 4 | 8 | 8 | 8 | 8 | 8 | 8 | 16 | ||||
| Vancomycin | 64 | NT | NT | ||||||||||||||
| VRSA SA509 | Razupenem | 2 | 4 | 50 | 2 | 2 | 2 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | |||
| Linezolid | 2 | 16 | 28 | 1 | 32 | >64 | 2 | 4 | 4 | 8 | 16 | ||||||
| Vancomycin | >64 | NT | NT | ||||||||||||||
Pass., number of daily passages. Boldface text indicates stable clones defined to have an MIC after the drug-free passages within ±1 of the MIC before the drug-free passages. NT, not tested at MICs of ≥64 μg/ml.
Razupenem is the only drug for which passages were continued after the MIC was more than four times the initial MIC.
For single-step studies, very high inocula (1 × 1010 to 1 × 1011 CFU/ml) of the 10 isolates on cation-adjusted Mueller-Hinton plates were exposed to each drug at 2×, 4×, and 8× MIC. Each plate contained 20 ml medium and was inoculated with 50-μl aliquots of the above-mentioned high inocula. To ensure that colonies could be quantitated (0 to 300 colonies/plate), dilutions of the inoculum were also made, resulting in a minimum of three plates per drug concentration. The frequency of spontaneous mutations was calculated at each MIC multiple for each strain after incubation of plates for 48 h (4).
Results of the multistep resistance selection studies are presented in Table 1. As can be seen, parental MICs (μg/ml) were as follows: razupenem, 0.016 to 4; vancomycin, 2 to >64; linezolid, 2 to 4. Razupenem yielded no resistant clones (>4-fold increase) after 15 days (Table 1). After 20 daily subcultures, razupenem yielded only clones with MICs of >4 μg/ml (preliminary susceptibility breakpoint of ≤4 μg/ml obtained by population pharmacokinetics and Monte Carlo simulation [2]) in one strain (SA618; 8 μg/ml) (Table 1) whose parent's MIC was 4 μg/ml. This MIC remained stable throughout an additional 30 days (the maximum number of passages). After 18 to 49 days, in 6 of 10 strains, razupenem MICs rose from 0.016 to 2 μg/ml (parents) to 0.125 to 8 μg/ml (stable clones after 10 drug-free subcultures) (Table 1). Of these six resistant clones, two yielded razupenem MICs of >4 μg/ml. Linezolid yielded resistant clones after 15 to 48 days in 4 of 10 strains with MICs rising from 2 to 4 μg/ml (parents) to 16 to 32 μg/ml (stable clones) (Table 1). Vancomycin selected no resistant clones (>4-fold increase) in all eight strains tested (MICs of ≥64 μg/ml were not tested). MICs of vancomycin against the tested strains rose from 2 to 8 μg/ml (parents) to 4 to 8 μg/ml after 50 days (Table 1). No cross-resistance was found with any clone/antimicrobial combination (Table 1).
Results of the single-step resistance selection studies are presented in Table 2. Mutant selection frequencies for razupenem ranged from <4.0 × 10−11 to 6.0 × 10−6 at 2× MIC to <3.3 × 10−11 to 6.7 × 10−9 at 8× MIC. These frequencies were equivalent to those for the existing carbapenems (imipenem, meropenem) against Pseudomonas aeruginosa (13, 16). Comparator values were similar: vancomycin, <3.3 × 10−11 to >1.0 × 10−8 at 2× MIC to <3.3 × 10−11 to <5.0 × 10−10 at 8× MIC; and linezolid, <3.7 × 10−11 to <3.3 × 10−10 at 2× MIC to < 3.7 × 10−11 to <3.3 × 10−10 at 8× MIC.
TABLE 2.
Frequency of single-step mutations for S. aureus strains
| Strain | Selecting drug | Frequency ata:
|
||
|---|---|---|---|---|
| 2× MIC | 4× MIC | 8× MIC | ||
| hVISA SA618 | Razupenem | <4.2 × 10−11 | <4.2 × 10−11 | <4.2 × 10−11 |
| Linezolid | <5.3 × 10−11 | <5.3 × 10−11 | <5.3 × 10−11 | |
| Vancomycin | >1.0 × 10−8 | 1.0 × 10−8 | <5.0 × 10−10 | |
| hVISA SA873 | Razupenem | <1.9 × 10−10 | <1.9 × 10−10 | <1.9 × 10−10 |
| Linezolid | <1.9 × 10−10 | <1.9 × 10−10 | <1.9 × 10−10 | |
| Vancomycin | <1.3 × 10−10 | <1.3 × 10−10 | <1.3 × 10−10 | |
| VISA SA555 | Razupenem | 6.0 × 10−6 | 3.0 × 10−8 | <1.0 × 10−10 |
| Linezolid | <1.8 × 10−10 | <1.8 × 10−10 | <1.8 × 10−10 | |
| Vancomycin | <1.6 × 10−10 | <1.6 × 10−10 | <1.6 × 10−10 | |
| VISA SA1287 | Razupenem | 1.0 × 10−6 | 2.7 × 10−8 | 6.7 × 10−9 |
| Linezolid | <1.3 × 10−10 | <1.3 × 10−10 | <1.3 × 10−10 | |
| Vancomycin | <4.3 × 10−11 | <4.3 × 10−11 | <4.3 × 10−11 | |
| MRSA SA525 | Razupenem | 6.7 × 10−8 | <3.3 × 10−11 | <3.3 × 10−11 |
| Linezolid | <3.7 × 10−11 | <3.7 × 10−11 | <3.7 × 10−11 | |
| Vancomycin | <3.3 × 10−11 | <3.3 × 10−11 | <3.3 × 10−11 | |
| MRSA SA547 | Razupenem | 2.4 × 10−7 | <4.0 × 10−11 | <4.0 × 10−11 |
| Linezolid | <3.8 × 10−11 | <3.8 × 10−11 | <3.8 × 10−11 | |
| Vancomycin | <1.7 × 10−10 | <1.7 × 10−10 | <1.7 × 10−10 | |
| MSSA SA540 | Razupenem | <6.7 × 10−11 | <6.7 × 10−11 | <6.7 × 10−11 |
| Linezolid | <1.3 × 10−10 | <1.3 × 10−10 | <1.3 × 10−10 | |
| Vancomycin | <1.2 × 10−10 | <1.2 × 10−10 | <1.2 × 10−10 | |
| MSSA SA543 | Razupenem | <4.0 × 10−11 | <4.0 × 10−11 | <4.0 × 10−11 |
| Linezolid | <1.4 × 10−10 | <1.4 × 10−10 | <1.4 × 10−10 | |
| Vancomycin | <3.3 × 10−11 | <3.3 × 10−11 | <3.3 × 10−11 | |
| VRSA SA510 | Razupenem | 1.3 × 10−7 | 6.7 × 10−8 | <3.3 × 10−10 |
| Linezolid | <3.3 × 10−10 | <3.3 × 10−10 | <3.3 × 10−10 | |
| Vancomycin | NT | NT | NT | |
| VRSA SA509 | Razupenem | 1.9 × 10−8 | <5.9 × 10−11 | <5.9 × 10−11 |
| Linezolid | <1.4 × 10−10 | <1.4 × 10−10 | <1.4 × 10−10 | |
| Vancomycin | NT | NT | NT | |
NT, not tested at MICs of ≥64 μg/ml.
Previous reports of razupenem (also known previously as SM-216601, SMP-601, PZ-601, and PTZ601) have reported improved activity against staphylococci and Enterococcus faecium, with MICs against MRSA ranging from 0.06 to 2 μg/ml (MIC90, 2 μg/ml). The compound is also potent against streptococci, Haemophilus influenzae, Moraxella catarrhalis, and Enterobacteriaceae such as Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis (9, 14, 15). Razupenem is not compromised (like other β-lactams) by low temperature or high salt concentrations (10). Additionally, razupenem shows better pharmacokinetics in animals, suggesting a favorable pharmacokinetic profile in humans, with a longer half-life, than do available carbapenems (15). In a murine model of hematogenous bronchopneumonia caused by MRSA and VISA, treatment with razupenem (MICs of 2 μg/ml for test strains) resulted in a significant decrease in the number of viable bacteria, a higher survival rate, and less marked inflammatory changes in the group treated with razupenem than in the group treated with vancomycin (9).
The current study shows MICs against MRSA similar to those reported previously (9, 14, 15), and especially to those reported by Livermore and Warner (10) who obtained, irrespective of temperature and NaCl, razupenem MICs of 4 μg/ml in some strains. Our studies also indicate that razupenem has confirmed activity versus MRSA at a preliminary breakpoint of ≤4 μg/ml (2) and low rates of spontaneous mutations on single-step selection. Although razupenem had a low propensity to select for mutations after 20 daily subcultures, 6 of the 10 strains tested yielded clones with increased MICs, two with MICs above the preliminary susceptibility breakpoint of ≤4 μg/ml, at between 20 and 50 daily subcultures. The significance of these findings remains to be determined in the clinical setting.
Acknowledgments
This study was supported by a grant from Protez Pharmaceuticals, Inc., Malvern, PA.
Footnotes
Published ahead of print on 11 May 2009.
REFERENCES
- 1.Appelbaum, P. C. 2007. Reduced glycopeptide susceptibility in methicillin-resistant Staphylococcus aureus (MRSA). Int. J. Antimicrob. Agents 30:398-408. [DOI] [PubMed] [Google Scholar]
- 2.Bhavnani, S. M., O. O. Okusanya, J. P. Hammel, A. Forrest, G. L. Drusano, D. R. Andes, W. A. Craig, J. L Pace, C. L. Young, L. Xerri, and P. G. Ambrose. 2007. Population pharmacokinetic (PK) and Monte Carlo simulation (MCS) analyses to support phase 2/3 PZ-601 (SMP-601) dosing strategies for complicated skin and skin structure infections (cSSSI), abstr. A-40. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother.
- 3.Bogdanovich, T., C. Clark, K. Kosowska-Shick, B. DeWasse, P. McGhee, and P. C. Appelbaum. 2007. Antistaphylococcal activity of CG400549, a new experimental FabI inhibitor, compared with that of other agents. Antimicrob. Agents Chemother. 51:4191-4195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bogdanovich, T., D. Esel, L. M. Kelly, B. Bozdogan, K. Credito, G. Lin, K. Smith, L. M. Ednie, D. B. Hoellman, and P. C. Appelbaum. 2005. Antistaphylococcal activity of DX-619, a new des-F(6)-quinolone, compared to those of other agents. Antimicrob. Agents Chemother. 49:3325-3333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.City of New York Department of Health and Mental Hygiene. 2007. Alert #31: surveillance for vancomycin resistance in Staphylococcus aureus. City of New York Department of Health and Mental Hygiene, New York, NY.
- 6.Clinical and Laboratory Standards Institute. 2006. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A7, 7th ed. Clinical and Laboratory Standards Institute, Wayne, PA.
- 7.de Lassence, A., N. Hidri, J. F. Timsit, M. L. Joly-Guillou, G. Thiery, A. Boyer, P. Lable, A. Blivet, H. Kalinowski, Y. Martin, J. P. Lajonchere, and D. Dreyfuss. 2006. Control and outcome of a large outbreak of colonization and infection with glycopeptide-intermediate Staphylococcus aureus in an intensive care unit. Clin. Infect. Dis. 42:170-178. [DOI] [PubMed] [Google Scholar]
- 8.Julian, K., K. Kosowska-Shick, C. Whitener, M. Roos, H. Labischinski, A. Rubio, L. Parent, L. Ednie, L. Koeth, T. Bogdanovich, and P. C. Appelbaum. 2007. Characterization of daptomycin nonsusceptible vancomycin-intermediate Staphylococcus aureus in a patient with endocarditis. Antimicrob. Agents Chemother. 51:3445-3448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kihara, R., K. Yanagihara, Y. Morinaga, N. Araki, S. Nakamura, M. Seki, K. Izumikawa, H. Kakeya, Y. Yamamoto, K. Tsukamoto, S. Kamihara, and S. Kohno. 2008. Potency of SMP-601, a novel carbapenem, in hematogenous murine bronchopneumonia caused by methicillin-resistant and vancomycin-intermediate Staphylococcus aureus. Antimicrob. Agents Chemother. 52:2163-2168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Livermore, D. M., and M. Warner. 2009. Effects of low temperature and high salt on the activity of the novel carbapenem PZ-601 (SMP-601) against methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemother. 63:411-413. [DOI] [PubMed] [Google Scholar]
- 11.Rybak, M. J., S. N. Leonard, K. L. Rossi, C. M. Cheung, H. S. Sadar, and R. N. Jones. 2008. Characterization of vancomycin-heteroresistant Staphylococcus aureus from the metropolitan area of Detroit, Michigan, over a 22-year period (1986 to 2007). J. Clin. Microbiol. 46:2950-2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sancak, B., S. Ercis, D. Menemenlioglu, S. Colakoglu, and G. Hascelik. 2005. Methicillin-resistant Staphylococcus aureus heterogeneously resistant to vancomycin in a Turkish university hospital. J. Antimicrob. Chemother. 56:519-523. [DOI] [PubMed] [Google Scholar]
- 13.Sumita, Y., and M. Kukasawa. 1996. Meropenem resistance in Pseudomonas aeruginosa. Chemotherapy 42:47-56. [DOI] [PubMed] [Google Scholar]
- 14.Ueda, Y., M. Itoh, A. Sasaki, and M. Sunagawa. 2005. SM-216601, a novel parenteral 1beta-methylcarbapenem: structure-activity relationships of antibacterial activity and neurotoxicity in mice. J. Antibiot. (Tokyo) 58:118-140. [DOI] [PubMed] [Google Scholar]
- 15.Ueda, Y., K. Kanazawa, K. Eguchi, K. Takemoto, Y. Eriguchi, and M. Sunagawa. 2005. In vitro and in vivo antibacterial activities of SM-216601, a new broad-spectrum parenteral carbapenem. Antimicrob. Agents Chemother. 49:4185-4196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiedemann, B., and M. Zühlsdorf. 1989. Antibacterial properties of meropenem towards clinical isolates, β-lactamase producers and laboratory mutants. J. Antimicrob. Chemother. 24(Suppl. A):197-205. [DOI] [PubMed] [Google Scholar]
- 17.Yusof, A., A. Englehardt, A. Karlsson, L. Bylund, P. Vidh, K. Mills, M. Wootton, and T. R. Walsh. 2008. Evaluation of a new Etest vancomycin-teicoplanin strip for detection of glycopeptide-intermediate Staphylococcus aureus (GISA), in particular, heterogenous GISA. J. Clin. Microbiol. 46:3042-3047. [DOI] [PMC free article] [PubMed] [Google Scholar]