Abstract
The filoviruses Marburg virus and Ebola virus cause severe hemorrhagic fever with high mortality in humans and nonhuman primates. Among the most promising filovirus vaccines under development is a system based on recombinant vesicular stomatitis virus (VSV) that expresses a single filovirus glycoprotein (GP) in place of the VSV glycoprotein (G). Here, we performed a proof-of-concept study in order to determine the potential of having one single-injection vaccine capable of protecting nonhuman primates against Sudan ebolavirus (SEBOV), Zaire ebolavirus (ZEBOV), Cote d'Ivoire ebolavirus (CIEBOV), and Marburgvirus (MARV). In this study, 11 cynomolgus monkeys were vaccinated with a blended vaccine consisting of equal parts of the vaccine vectors VSVΔG/SEBOVGP, VSVΔG/ZEBOVGP, and VSVΔG/MARVGP. Four weeks later, three of these animals were challenged with MARV, three with CIEBOV, three with ZEBOV, and two with SEBOV. Three control animals were vaccinated with VSV vectors encoding a nonfilovirus GP and challenged with SEBOV, ZEBOV, and MARV, respectively, and five unvaccinated control animals were challenged with CIEBOV. Importantly, none of the macaques vaccinated with the blended vaccine succumbed to a filovirus challenge. As expected, an experimental control animal vaccinated with VSVΔG/ZEBOVGP and challenged with SEBOV succumbed, as did the positive controls challenged with SEBOV, ZEBOV, and MARV, respectively. All five control animals challenged with CIEBOV became severely ill, and three of the animals succumbed on days 12, 12, and 14, respectively. The two animals that survived CIEBOV infection were protected from subsequent challenge with either SEBOV or ZEBOV, suggesting that immunity to CIEBOV may be protective against other species of Ebola virus. In conclusion, we developed an immunization scheme based on a single-injection vaccine that protects nonhuman primates against lethal challenge with representative strains of all human pathogenic filovirus species.
Marburgvirus (MARV) and Ebolavirus (EBOV), the causative agents of Marburg and Ebola hemorrhagic fever (HF), respectively, represent the two genera that comprise the family Filoviridae (8, 24). The MARV genus contains a single species, Lake Victoria marburgvirus. The EBOV genus is divided into four distinct species: (i) Sudan ebolavirus (SEBOV), (ii) Zaire ebolavirus (ZEBOV), (iii) Cote d'Ivoire ebolavirus (CIEBOV), and (iv) Reston ebolavirus (REBOV). A putative fifth species of EBOV was associated with an outbreak in Uganda late in 2007 (33). MARV, ZEBOV, and SEBOV are important human pathogens, with case fatality rates frequently ranging between 70% and 90% for ZEBOV, around 50% for SEBOV, and up to 90% for MARV outbreaks depending on the strain of MARV (reviewed in reference 24). CIEBOV caused deaths in chimpanzees and a severe nonlethal human infection in a single case in the Republic of Cote d'Ivoire in 1994 (21). REBOV is highly lethal for macaques but is not thought to cause disease in humans, although the pathogenic potential of REBOV in humans remains unknown (24). An outbreak of REBOV in pigs was recently reported in the Philippines; however, it is unclear whether the disease observed in the pigs was caused by REBOV or other agents detected in the animals, including porcine reproductive and respiratory syndrome virus (5, 22).
While there are no FDA-approved vaccines or postexposure treatment modalities available for preventing or managing EBOV or MARV infections, there are at least five different vaccine systems that have shown promise in completely protecting nonhuman primates against EBOV, and four of these systems have also been shown to protect macaques against MARV HF (3, 6, 12, 18, 20, 28-31, 35). Several of these vaccine platforms require multiple injections to confer protective efficacy (3, 18, 30, 31, 35). However, for agents such as EBOV and MARV, which are indigenous to Africa and are also potential agents of bioterrorism, a single-injection vaccine is preferable. In the case of preventing natural infections, multiple-dose vaccines are both too costly and not practicable (logistics and compliance) in developing countries. In the case of a deliberate release of these agents, there would be little time for deployment of a vaccine that requires multiple injections. Thus, for most practical applications, a vaccine against the filoviruses necessitates a single immunization.
Of the prospective filovirus vaccines, only two systems, one based on a replication-defective adenovirus serotype 5 and the other based on the recombinant vesicular stomatitis virus (VSV), were shown to provide complete protection to nonhuman primates when administered as a single-injection vaccine (6, 12, 20, 28, 29). Most intriguingly, the VSV-based vaccine is the only vaccine which has shown utility when administered as a postexposure treatment against filovirus infections (7, 9, 15). Here, we evaluated the utility of combining our VSV-based EBOV and MARV vectors into a single-injection vaccine and determined the ability of this blended vaccine to protect nonhuman primates against three species of EBOV and MARV. Furthermore, we assessed the reusability of the VSV vectors in our macaque models of filovirus HF.
MATERIALS AND METHODS
Vaccine vectors and challenge virus.
The recombinant VSVs expressing the glycoprotein (GP) of ZEBOV (strain Mayinga) (VSVΔG/ZEBOVGP), the GP of SEBOV (strain Boniface) (VSVΔG/SEBOVGP), or the GP of MARV (strain Musoke) (VSVΔG/MARVGP) were generated using the infectious clone for the VSV Indiana serotype, as described recently (11, 15). CIEBOV was isolated from the human case from the Republic of Côte d'Ivoire in 1994 (21); SEBOV (strain Boniface) was isolated from a patient from the SEBOV outbreak in Sudan in 1976 (36); ZEBOV (strain Kikwit) was isolated from a patient from the ZEBOV outbreak in Kikwit, Democratic Republic of the Congo, in 1995 (19); and MARV (strain Musoke) was isolated from a human case in 1980 in Kenya (27).
Animal studies with single injection of a blended filovirus vaccine.
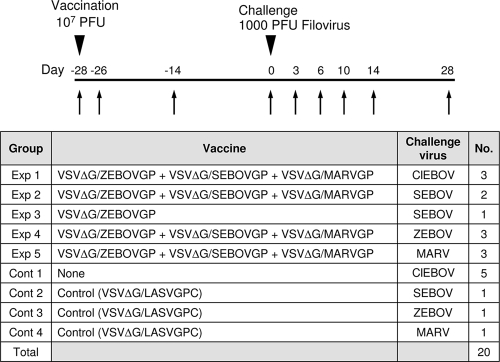
Twenty filovirus-naïve cynomolgus monkeys (Macaca fascicularis) were randomized into five experimental groups (experimental groups 1, 2, 3, 4, and 5), consisting of three monkeys per group (experimental groups 1, 4, and 5), two monkeys per group (experimental group 2), or one monkey per group (experimental group 3), and four control groups (control groups 1, 2, 3, and 4), consisting of five monkeys per group (control group 1) or one monkey per group (control groups 2, 3, and 4) (Fig. 1). Control group 1 included five animals, as there have been no studies to date to evaluate the pathogenic potential of CIEBOV in nonhuman primates, whereas control groups 2 to 4 consisted of one animal per group, as historical studies have shown that ZEBOV, SEBOV, and MARV are uniformly lethal in cynomolgus monkeys (6, 18, 20, 28-31, 35). Animals in four experimental groups (experimental groups 1, 2, 4, and 5) were vaccinated by intramuscular (i.m.) injection of ∼1 × 107 PFU of VSVΔG/SEBOVGP, 1 × 107 PFU of VSVΔG/ZEBOVGP, and 1 × 107 PFU of VSVΔG/MARVGP-Musoke (total dose of ∼3 × 107 PFU), while the single animal in experimental group 3 was vaccinated with 3 × 107 PFU of VSVΔG/ZEBOVGP only. The animals in control groups 2 to 4 were injected in parallel with an equivalent dose (∼3 × 107 PFU) of a VSV vector encoding a nonfilovirus GP (VSVΔG/LASVGPC [LASVGPC is a Lassa virus glycoprotein precursor]) (17), while the control animals in control group 1 were not vaccinated. The dose of ∼1 × 107 PFU of each vaccine component was chosen because it is comparable to that used in our previous preventive-vaccine studies with these vectors in nonhuman primates (6, 12, 14, 20). Four weeks after vaccination, all animals were exposed to infectious filoviruses via i.m. injection as follows: animals in experimental group 1 and control group 1 were exposed to 1,000 PFU of CIEBOV; animals in experimental groups 2 and 3 and control group 2 were exposed to 1,000 PFU of SEBOV; animals in experimental group 4 and control group 3 were exposed to 1,000 PFU of ZEBOV; and animals in experimental group 5 and control group 4 were exposed to 1,000 PFU of MARV.
FIG. 1.
Immunization and challenge of nonhuman primates. Flow chart (top) and table (bottom) of experimental design. Arrows indicate days of sampling. Cont, control group; Exp, experimental group; No., number of monkeys in group.
Animals were closely monitored for evidence of clinical illness (e.g., temperature, weight loss, changes in complete blood count, and blood chemistry) during both the vaccination and the filovirus challenge portion of the study. In addition, VSV and filovirus viremia were analyzed after vaccination and challenge, respectively. Animals were given physical exams and blood was collected on days 2, 14, and 28 after vaccination and on days 3, 6, 10, 14, and 28 after filovirus challenge (Fig. 1).
Animal studies with separate injections of filovirus vaccines.
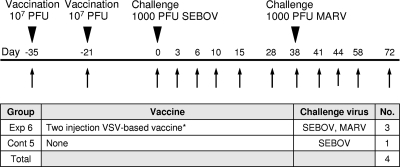
Four filovirus-naïve rhesus monkeys (Macaca mulatta) were randomized into an experimental group of three animals (experimental group 6) and a control group of one animal (control group 5) (Fig. 2). The three animals in the experimental group were vaccinated with ∼1 × 107 PFU of VSVΔG/SEBOVGP by i.m. injection. After 2 weeks, we vaccinated these animals with a blend of ∼1 × 107 PFU of VSVΔG/ZEBOVGP and 1 × 107 PFU of VSVΔG/MARVGP (Musoke strain). Three weeks after this second vaccination, all three animals and a single unvaccinated control animal were challenged by i.m. injection with 1,000 PFU of SEBOV. Surviving animals were back-challenged 38 days after the SEBOV challenge by i.m. injection with 1,000 PFU of MARV (strain Musoke). Animals were given physical exams and blood was collected at the time of vaccination and on days 3, 6, 10, 14 or 15, and 28 after filovirus challenge (Fig. 2).
FIG. 2.
Immunization, challenge, and rechallenge of nonhuman primates. Flow chart (top) and table (bottom) of experimental design. Arrows indicate days of sampling. *, the two-injection VSV-based vaccine consisted of a recombinant VSV-based SEBOV vaccine and subsequently a combination of a recombinant VSV-based ZEBOV vaccine and a VSV-based MARV vaccine, given as indicated. For definitions of abbreviations, see the legend for Fig. 1.
Animal studies performed in biosafety level 4 biocontainment facilities at USAMRIID were approved by the USAMRIID Laboratory Animal Use Committee. Animal research was conducted in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals and experiments involving animals and adhered to the principles stated in the Guide for the Care and Use of Laboratory Animals (21a). The facilities used are fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International. Animal studies performed in biosafety level 4 containment facilities at the Public Health Agency of Canada were performed under an approved animal use document according to the guidelines of the Canadian Council on Animal Care.
Hematology and serum biochemistry.
Total white blood cell counts, white blood cell differentials, red blood cell counts, platelet counts, hematocrit values, total hemoglobin concentrations, mean cell volumes, mean corpuscular volumes, and mean corpuscular hemoglobin concentrations were determined from blood samples collected in tubes containing EDTA by using a laser-based hematologic analyzer (Coulter Electronics, Hialeah, FL). Determination of the white blood cell differentials was performed manually with Wright-stained blood smears. Serum samples were tested for concentrations of albumin, amylase, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), glucose, cholesterol, total protein, total bilirubin (TBIL), blood urea nitrogen (BUN), and creatinine (CRE) by using a Piccolo point-of-care blood analyzer (Abaxis, Sunnyvale, CA).
Detection of VSV and filoviruses.
RNA was isolated from plasma and swabs using Tripure reagent (Invitrogen, Grand Island, NY). RNA was also isolated from peripheral blood mononuclear cells of animals challenged with CIEBOV, as this was the first evaluation of CIEBOV in nonhuman primates. Quantitative reverse transcriptase PCR (RT-PCR) assays were used for detection of RNA. VSV was detected using primers/probes targeting the nucleoprotein gene (nucleotide [nt] positions 1146 to 1201, GenBank accession no. AM690337). ZEBOV and CIEBOV were detected using primers/probes targeting the glycoprotein genes (for ZEBOV, nt positions 7720 to 7783, GenBank accession no. AF086833; for CIEBOV, nt positions 6962 to 7037, GenBank accession no. FJ217162). SEBOV and MARV RNAs were detected using primers/probes targeting the L genes (for SEBOV, nt positions 13465 to 13534, GenBank accession no. AY729654; for MARV, nt positions 13419 to 13483, GenBank accession no. AY358025). The limit of detection for these assays is 0.1 PFU/ml of plasma. Virus titration was performed by plaque assay with Vero E6 cells from all blood samples. Briefly, increasing 10-fold dilutions of the samples were adsorbed to Vero E6 monolayers in duplicate wells (0.2 ml per well); thus, the limit for detection was 25 PFU/ml.
Humoral immune response.
Immunoglobulin G (IgG) antibodies against CIEBOV, SEBOV, ZEBOV, or MARV were detected with an enzyme-linked immunosorbent assay (ELISA) using purified virus particles as an antigen source, as previously described (6, 12, 14, 20, 29).
RESULTS
Evaluation of a single-injection blended vaccine as a panfilovirus vaccine.
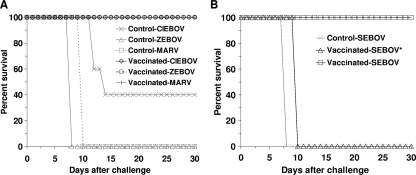
No animal showed any evidence of clinical illness as a result of vaccination (Table 1), and VSV RNA was detected only in the day 2 postimmunization sample from one animal (data not shown). None of the specifically vaccinated animals in experimental group 1, 4, or 5 showed any evidence of clinical illness after the filovirus challenge (Table 1), and all animals in these groups survived (Fig. 3). We were unable to detect filovirus viremia in any of these animals by plaque assay or PCR (Table 2). The single animal in experimental group 3 (subject 6) became clinically ill with symptoms consistent with SEBOV HF and succumbed to the SEBOV challenge on day 10 (Fig. 3). The two animals in experimental group 2 (subjects 4 and 5) developed mild clinical signs of illness by day 6, including fever, lymphopenia, and mild anorexia; however, both animals recovered quickly and appeared healthy by day 10. Surprisingly, we were unable to detect SEBOV viremia in either of these animals by plaque assay or PCR (Table 2).
TABLE 1.
Clinical findings for cynomolgus monkeys challenged with filoviruses
| Animal | Groupa | Vaccineb | Challenge virus | Symptoms observed between day 0 and day 28 after vaccine | Symptoms observed between day 1 and day 28 after filovirus challengee | Final outcome |
|---|---|---|---|---|---|---|
| Subject 1 | Exp 1 | VSV blend | CIEBOV | ⊘c | ⊘ | Survived |
| Subject 2 | Exp 1 | VSV blend | CIEBOV | ⊘ | ⊘ | Survived |
| Subject 3 | Exp 1 | VSV blend | CIEBOV | ⊘ | ⊘ | Survived |
| Control 1 | Cont 1 | None | CIEBOV | NAd | Mild rash (10-12), anorexia (10-12), depression (11, 12), lymphopenia (6, 10, 12), thrombocytopenia (10, 12), ALP→→→ (10), ALP→ (12), ALT→→→ (10, 12), AST→→→ (10, 12), BUN→→→ (12), CRE→ (12), GGT→→ (10),GGT→ (12), TBIL→ (12), UA→ (12) | Died on day 12 |
| Control 2 | Cont 1 | None | CIEBOV | NA | Anorexia (10, 11), thrombocytopenia (10), AST→→→ (10) | Survived |
| Control 3 | Cont 1 | None | CIEBOV | NA | Fever (6), moderate rash (10, 11), anorexia (10, 11), depression (10, 11), lymphopenia (6, 10), thrombocytopenia (6, 10), ALT→ (10), AST→→→(10) | Died on day 12 |
| Control 4 | Cont 1 | None | CIEBOV | NA | Anorexia (10-13), depression (12, 13), lymphopenia (6, 10), thrombocytopenia (6, 10), ALP→→ (10), ALT→ (10), AST→→→ (10), BUN→→ (10), CRE→ (10), GGT→→→ (10) | Died on day 14 |
| Control 5 | Cont 1 | None | CIEBOV | NA | Fever (6), mild rash (11-17), anorexia (9-17), depression (9-17), facial edema (11-17), lymphopenia (6, 10, 14), thrombocytopenia (10, 14), ALP→ (14), ALT→ (10), AST→→ (10), AST→→→ (14), BUN→ (10,14), GGT→ (10) | Survived |
| Subject 4 | Exp 2 | VSV blend | SEBOV | ⊘ | Fever (6), anorexia (8), depression (8), lymphopenia (6) | Survived |
| Subject 5 | Exp 2 | VSV blend | SEBOV | ⊘ | Fever (6), anorexia (8), depression (8), lymphopenia (6) | Survived |
| Subject 6 | Exp 3 | VSVΔG/ZEBOVGP | SEBOV | ⊘ | Anorexia (7-10), depression (7-10), mild rash (8, 9), moderate rash (10), epistaxis (8, 9), lymphopenia (6), thrombocytopenia (6), CRE→ (6) | Died on day 10 |
| Control 6 | Cont 2 | VSVΔG/LASVGPC | SEBOV | ⊘ | Anorexia (7, 8), depression (7, 8), severe rash (8), lymphopenia (6), thrombocytopenia (6), ALP→ (8), AST→→→ (6, 8), BUN→→→ (8) | Died on day 8 |
| Subject 7 | Exp 4 | VSV blend | ZEBOV | ⊘ | ⊘ | Survived |
| Subject 8 | Exp 4 | VSV blend | ZEBOV | ⊘ | ⊘ | Survived |
| Subject 9 | Exp 4 | VSV blend | ZEBOV | ⊘ | ⊘ | Survived |
| Control 7 | Cont 3 | VSVΔG/LASVGPC | ZEBOV | ⊘ | Moderate rash (6, 7), severe rash (8), anorexia (6-8), depression (6-8), lymphopenia (6), thrombocytopenia (6), ALP→ (6, 8), ALT→→→ (8), AST→→→ (6, 8), BUN→→→ (8), CRE→→→ (8), GGT→→→ (8), TBIL→→ (8) | Died on day 8 |
| Subject 10 | Exp 5 | VSV blend | MARV | ⊘ | ⊘ | Survived |
| Subject 11 | Exp 5 | VSV blend | MARV | ⊘ | ⊘ | Survived |
| Subject 12 | Exp 5 | VSV blend | MARV | ⊘ | ⊘ | Survived |
| Control 8 | Cont 4 | VSVΔG/LASVGPC | MARV | ⊘ | Mild rash (8), moderate rash (9, 10), anorexia (8-10), depression (8-10), lymphopenia (6), thrombocytopenia (6), ALP→→→ (10), ALT→→→ (10), AST→→→ (10), BUN→→→ (10), CRE→→→ (10), GGT→ (10), TBIL→→→ (10), GLU↓↓↓ (10), UA→→→ (10) | Died on day 10 |
Exp, experimental group; Cont, control group.
VSV blend, VSVΔG/ZEBOVGP plus VSVΔG/SEBOVGP plus VSVΔG/MARVGP.
⊘, no clinical symptoms.
NA, not applicable.
Days after filovirus challenge are shown in parentheses. A mild rash is defined as focal areas of petechiae covering less than 10% of the skin, a moderate rash is defined as areas of petechiae covering between 10% and 40% of the skin, and a severe rash is defined as areas of petechiae and/or echymosis covering more than 40% of the skin. Fever is defined as a temperature more than 2.5°F over baseline or at least 1.5°F over baseline and ≥103.5°F. Lymphopenia and thrombocytopenia are defined by a ≥35% drop in numbers of lymphocytes and platelets, respectively. UA, uric acid; GLU, glucose; →, 2- to 3-fold increase; →→, 4- to 5-fold increase; →→→, >5-fold increase; ↓↓↓, >5-fold decrease.
FIG. 3.
Kaplan-Meier survival curves for cynomolgus macaques vaccinated with a blended recombinant VSV vaccine and challenged with CIEBOV, ZEBOV, or MARV at day 28 after vaccination (A) or with a blended recombinant VSV vaccine or a monovalent ZEBOV vaccine (*) and challenged with SEBOV at day 28 after vaccination (B).
TABLE 2.
Viral load in cynomolgus monkeys after filovirus challenge
| Animal | Groupa | Vaccine | Challenge virus | Viral load (log10 PFU filovirus/ml plasma)b
|
|||||
|---|---|---|---|---|---|---|---|---|---|
| Plasma
|
PBMC
|
||||||||
| Day 6 | Day 0 | Day 14 | Day 6 | Day 10 | Day 14 | ||||
| Subject 1 | Exp 1 | Multivalent blend | CIEBOV | 0 (NT) | 0 (NT) | 0 (NT) | NT (−) | NT (−) | NT (−) |
| Subject 2 | Exp 1 | Multivalent blend | CIEBOV | 0 (NT) | 0 (NT) | 0 (NT) | NT (−) | NT (−) | NT (−) |
| Subject 3 | Exp 1 | Multivalent blend | CIEBOV | 0 (NT) | 0 (NT) | 0 (NT) | NT (−) | NT (−) | NT (−) |
| Control 1 | Cont 1 | None | CIEBOV | 5.17 (NT) | 4.84 (NT) | NT (+) | NT (+) | ||
| Control 2 | Cont 1 | None | CIEBOV | 2.44 (NT) | 2.35 (NT) | 0 (NT) | NT (−) | NT (+) | NT (+) |
| Control 3 | Cont 1 | None | CIEBOV | 4.51 (NT) | 5.70 (NT) | NT (+) | NT (+) | ||
| Control 4 | Cont 1 | None | CIEBOV | 2.44 (NT) | 6.63 (NT) | 5.63 (NT) | NT (+) | NT (+) | NT (+) |
| Control 5 | Cont 1 | None | CIEBOV | 5.18 (+) | 4.46 (+) | 2.35 (−) | NT (−) | NT (+) | NT (+) |
| Subject 4 | Exp 2 | Multivalent blend | SEBOV | 0 (−) | 0 (−) | 0 (−) | |||
| Subject 5 | Exp 2 | Multivalent blend | SEBOV | 0 (−) | 0 (−) | 0 (−) | |||
| Subject 6 | Exp 3 | VSVΔG/ZEBOVGP | SEBOV | 5.20 (+) | |||||
| Control 6 | Cont 2 | VSVΔG/LASVGPC | SEBOV | 6.17 (+) | |||||
| Subject 7 | Exp 4 | Multivalent blend | ZEBOV | 0 (−) | 0 (−) | 0 (−) | |||
| Subject 8 | Exp 4 | Multivalent blend | ZEBOV | 0 (−) | 0 (−) | 0 (−) | |||
| Subject 9 | Exp 4 | Multivalent blend | ZEBOV | 0 (−) | 0 (−) | 0 (−) | |||
| Control 7 | Cont 3 | VSVΔG/LASVGPC | ZEBOV | 5.83 (+) | |||||
| Subject 10 | Exp 5 | Multivalent blend | MARV | 0 (−) | 0 (−) | 0 (−) | |||
| Subject 11 | Exp 5 | Multivalent blend | MARV | 0 (−) | 0 (−) | 0 (−) | |||
| Subject 12 | Exp 5 | Multivalent blend | MARV | 0 (−) | 0 (−) | 0 (−) | |||
| Control 8 | Cont 4 | VSVΔG/LASVGPC | MARV | 5.93 (+) | 6.36 (+) | ||||
Exp, experimental group; Cont, control group.
Symbols in parentheses represent RT-PCR results. +, positive; −, negative; NT, not tested.
All control animals followed a typical filovirus disease course and developed macular rashes, lymphopenia, thrombocytopenia, and elevated levels of liver enzymes (Table 1). This included the five CIEBOV-infected macaques, of which three succumbed to death on day 12 (two animals) or day 14 (one animal) and two survived after a long convalescence (controls 2 and 5) (Table 1; Fig. 3). A detailed description of the pathology and pathogenesis of CIEBOV in cynomolgus monkeys will be reported separately. The remaining control animals in this study died on days 8 (SEBOV and ZEBOV) and 10 (MARV-Musoke strain) (Table 1; Fig. 3). Other than the control animals, the only animal in which we were able to detect the presence of circulating filovirus viremia was the single animal in experimental group 3 (subject 6) (Table 2). Unlike the other experimental-group animals in this study, which received the blended vaccine, this animal was vaccinated with the monovalent VSVΔG/ZEBOVGP vaccine and challenged with SEBOV to confirm that there is no cross-protection between ZEBOV and SEBOV.
Evaluation of humoral immune responses.
The antibody responses of the cynomolgus macaques immunized with the blended vector vaccine were evaluated after vaccination (day 14 and day 28) and after filovirus challenge (day 14 and day 28) by IgG ELISA. All of the animals developed modest IgG titers against SEBOV, ZEBOV, and MARV (range, 1:32 to 1:100) at the day of filovirus challenge (Table 3). Prechallenge titers were consistent with those from previous studies in which macaques were vaccinated with VSV vectors expressing a single filovirus GP (VSVΔG/ZEBOVGP or VSVΔG/MARVGP) (6, 12, 20). As noted in previous studies, IgG titers against filoviruses often increased after filovirus challenge (Table 3). We are uncertain as to whether this increase is a result of undetected virus replication at undetermined sites or whether the high dose of the challenge virus (1,000 PFU, approximately 30,000 virus particles) boosted the immune response.
TABLE 3.
Circulating levels of IgG against filoviruses in cynomolgus monkeys
| Animal | Groupa | Vaccine (challenge virus)b | IgG ELISA for: | Titer at time point after vaccination
|
||||
|---|---|---|---|---|---|---|---|---|
| Day 0 | Day 14 | Day 28 | Day 42 | Day 56 | ||||
| Subject 1 | Exp 1 | Multivalent blend (CIEBOV) | CIEBOV | 0 | 100 | 100 | 100 | 100 |
| SEBOV | 0 | 32 | 32 | 32 | 32 | |||
| ZEBOV | 0 | 100 | 100 | 100 | 100 | |||
| MARV | 0 | 100 | 100 | 100 | 100 | |||
| Subject 2 | Exp 1 | Multivalent blend (CIEBOV) | CIEBOV | 0 | 32 | 32 | 32 | 100 |
| SEBOV | 0 | 32 | 32 | 32 | 32 | |||
| ZEBOV | 0 | 32 | 32 | 32 | 32 | |||
| MARV | 0 | 32 | 32 | 32 | 32 | |||
| Subject 3 | Exp 1 | Multivalent blend (CIEBOV) | CIEBOV | 0 | 100 | 100 | 1,000 | 1,000 |
| SEBOV | 0 | 100 | 100 | 100 | 100 | |||
| ZEBOV | 0 | 32 | 32 | 100 | 100 | |||
| MARV | 0 | 320 | 320 | 320 | 320 | |||
| Control 2 | Cont 1 | None (CIEBOV) | CIEBOV | 0 | 0 | 0 | 100 | 320 |
| SEBOV | 0 | 0 | 0 | 32 | 32 | |||
| ZEBOV | 0 | 0 | 0 | 32 | 100 | |||
| MARV | 0 | 0 | 0 | 0 | 0 | |||
| Control 5 | Cont 1 | None (CIEBOV) | CIEBOV | 0 | 0 | 0 | 320 | 1,000 |
| SEBOV | 0 | 0 | 0 | 32 | 100 | |||
| ZEBOV | 0 | 0 | 0 | 100 | 1,000 | |||
| MARV | 0 | 0 | 0 | 32 | 0 | |||
| Subject 4 | Exp 2 | Multivalent blend (SEBOV) | SEBOV | 0 | 100 | 100 | 320 | 1,000 |
| ZEBOV | 0 | 32 | 32 | 100 | 1,000 | |||
| MARV | 0 | 100 | 100 | 100 | 100 | |||
| Subject 5 | Exp 2 | Multivalent blend (SEBOV) | SEBOV | 0 | 32 | 100 | 1,000 | 1,000 |
| ZEBOV | 0 | 32 | 32 | 100 | 1,000 | |||
| MARV | 0 | 100 | 100 | 100 | 100 | |||
| Subject 6 | Exp 3 | VSVΔG/ZEBOVGP (SEBOV) | SEBOV | 0 | 0 | 0 | ||
| ZEBOV | 0 | 32 | 32 | |||||
| MARV | 0 | 32 | 0 | |||||
| Control 6 | Cont 2 | VSVΔG/LASVGPC (SEBOV) | SEBOV | 0 | 32 | 0 | ||
| ZEBOV | 0 | 0 | 0 | |||||
| MARV | 0 | 32 | 0 | |||||
| Subject 7 | Exp 4 | Multivalent blend (ZEBOV) | SEBOV | 0 | 100 | 32 | 100 | 100 |
| ZEBOV | 0 | 32 | 32 | 1,000 | 1,000 | |||
| MARV | 0 | 32 | 32 | 100 | 100 | |||
| Subject 8 | Exp 4 | Multivalent blend (ZEBOV) | SEBOV | 0 | 32 | 32 | 100 | 100 |
| ZEBOV | 0 | 32 | 32 | 1,000 | 1,000 | |||
| MARV | 0 | 100 | 100 | 100 | 100 | |||
| Subject 9 | Exp 4 | Multivalent blend (ZEBOV) | SEBOV | 0 | 100 | 100 | 32 | 100 |
| ZEBOV | 0 | 32 | 32 | 32 | 320 | |||
| MARV | 0 | 32 | 100 | 100 | 100 | |||
| Control 7 | Cont 3 | VSVΔG/LASVGPC (ZEBOV) | SEBOV | 0 | 0 | 0 | ||
| ZEBOV | 0 | 32 | 0 | |||||
| MARV | 0 | 32 | 0 | |||||
| Subject 10 | Exp 5 | Multivalent blend (MARV) | SEBOV | 0 | 32 | 32 | 32 | 32 |
| ZEBOV | 0 | 100 | 32 | 100 | 320 | |||
| MARV | 0 | 100 | 100 | 100 | 100 | |||
| Subject 11 | Exp 5 | Multivalent blend (MARV) | SEBOV | 0 | 32 | 100 | 100 | 100 |
| ZEBOV | 0 | 32 | 32 | 320 | 320 | |||
| MARV | 0 | 100 | 100 | 320 | 320 | |||
| Subject 12 | Exp 5 | Multivalent blend (MARV) | SEBOV | 0 | 32 | 32 | 32 | 32 |
| ZEBOV | 0 | 32 | 32 | 320 | 320 | |||
| MARV | 0 | 100 | 100 | 1,000 | 3,200 | |||
| Control 8 | Cont 4 | VSVΔG/LASVGPC (MARV) | SEBOV | 0 | 0 | 0 | ||
| ZEBOV | 0 | 0 | 0 | |||||
| MARV | 0 | 32 | 0 | |||||
Exp, experimental group; Cont, control group.
The multivalent blend was a combination of a recombinant VSV-based SEBOV vaccine, a VSV-based ZEBOV vaccine, and a VSV-based MARV vaccine. Animals were challenged on day 28 with CIEBOV, SEBOV, ZEBOV, or MARV as indicated.
Back-challenge of control macaques that survived CIEBOV infection.
Previous studies have suggested that immunity to one species of EBOV does not confer protection against another species of EBOV. For example, macaques that are immune to SEBOV are not protected against challenge with ZEBOV, while macaques immune to ZEBOV are not protected against challenge with SEBOV (1, 20). In the current study, there were two macaques that survived CIEBOV challenge (controls 2 and 5) (Table 1; Fig. 3). One of the two cynomolgus monkeys that survived CIEBOV challenge was back-challenged by i.m. injection with 1,000 PFU of heterologous ZEBOV 131 days after initial CIEBOV exposure. Surprisingly, this animal did not become clinically ill or viremic and remained healthy. This animal was then challenged by i.m. injection with 1,000 PFU of heterologous SEBOV 38 days after the ZEBOV back-challenge. Again, this animal did not become clinically ill or viremic and remained healthy. The second control cynomolgus macaque that survived CIEBOV challenge was then back-challenged 43 days after the initial CIEBOV challenge by i.m. injection with 1,000 PFU of heterologous SEBOV. As with the previous back-challenge of an CIEBOV-immune macaque, we were surprised that this animal showed no evidence of clinical illness and did not become viremic. In summary, one CIEBOV-immune macaque survived back-challenge with heterologous ZEBOV and a second back-challenge with heterologous SEBOV, while a second CIEBOV-immune macaque survived back-challenge with heterologous SEBOV. A second back-challenge with ZEBOV was not performed on this animal, as the study protocol had expired.
Vaccination with VSVΔG/SEBOVGP followed by vaccination with VSVΔG/ZEBOVGP and VSVΔG/MARVGP.
It appeared that there may have been some weak interference between VSVΔG/SEBOVGP and the other VSV vectors in the single-vaccination, blended-vaccine study (Table 1, subjects 4 and 5). This may be due to the slower replication kinetics of VSVΔG/SEBOVGP than of VSVΔG/ZEBOVGP or VSVΔG/ MARVGP-Musoke (T. W. Geisbert and H. Feldmann, unpublished observation), or it may be a result of other causes, such as the affinity of the specific filovirus GPs for the antigen-presenting cells of the host. To begin to evaluate this finding, we next vaccinated three rhesus monkeys with ∼1 × 107 PFU of VSVΔG/SEBOVGP by i.m. injection. Rhesus monkeys were used because of availability and since the filovirus species and strains employed in this study cause uniform lethality in both macaque species (reviewed in reference 16). After 2 weeks, we vaccinated these animals with ∼1 × 107 PFU of VSVΔG/ZEBOVGP and 1 × 107 PFU of VSVΔG/MARVGP. Three weeks after this second vaccination, all three animals and a single control animal were challenged by i.m. injection with 1,000 PFU of SEBOV (Fig. 2). All three vaccinated animals showed no clinical evidence of SEBOV HF and remained healthy. In contrast, the control animal became severely ill and developed classic symptoms of SEBOV HF, including dehydration, anorexia, and the presence of a macular rash; this animal died on day 17. SEBOV was detected in plasma of this animal on days 6, 10, 14, and 17 by plaque assay and RT-PCR, while no evidence of SEBOV was detected in plasma of any of the three specifically vaccinated animals at any time point (data not shown). We next back-challenged the three surviving animals 38 days after the initial SEBOV challenge with 1,000 PFU of MARV-Musoke to determine whether the vaccine regimen employed in this study could confer protection against challenge with a different filovirus (Fig. 2). All three animals showed no clinical evidence of infection or viremia and survived the MARV back-challenge. As observed in the single-vaccine study (described above), all three vaccinated animals in this study developed modest IgG titers against SEBOV, ZEBOV, and/or MARV (range, 1:32 to 1:100) at the day of filovirus challenge (Table 4), with titers increasing after challenge. In summary, vaccination with VSVΔG/SEBOVGP followed 2 weeks later by vaccination with a mixture of VSVΔG/ZEBOVGP and VSVΔG/MARVGP conferred complete protection against both SEBOV and MARV-Musoke. This study also shows the reusability of these recombinant VSV vectors.
TABLE 4.
Circulating levels of IgG against filoviruses in rhesus monkeys
| Animal | Vaccine (challenge virus)a | IgG ELISA for: | Titer at time point after vaccination
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Day 0 | Day 14 | Day 35 | Day 50 | Day 63 | Day 73 | Day 87 | Day 101 | |||
| Subject 13 | Two-injection VSV-based vaccine | SEBOV | 0 | 100 | 100 | 3,200 | 3,200 | 3,200 | 3,200 | 3,200 |
| (SEBOV, MARV) | ZEBOV | 0 | 32 | 100 | 1,000 | 1,000 | 1,000 | 1,000 | 320 | |
| MARV | 0 | 32 | 32 | 32 | 32 | 32 | 1,000 | 1,000 | ||
| Subject 14 | Two-injection VSV-based vaccine | SEBOV | 0 | 100 | 320 | 3,200 | 3,200 | 1,000 | 1,000 | 3,200 |
| (SEBOV, MARV) | ZEBOV | 0 | 32 | 100 | 100 | 320 | 100 | 100 | 100 | |
| MARV | 0 | 0 | 320 | 320 | 100 | 100 | 3,200 | 1,000 | ||
| Subject 15 | Two-injection VSV-based vaccine | SEBOV | 0 | 100 | 320 | 320 | 320 | 100 | 100 | 100 |
| (SEBOV, MARV) | ZEBOV | 0 | 32 | 320 | 320 | 100 | 100 | 100 | 100 | |
| MARV | 0 | 32 | 320 | 320 | 100 | 100 | 3,200 | 3,200 | ||
| Control 5 | None (SEBOV) | SEBOV | 0 | 0 | 0 | 100 | ||||
| ZEBOV | 0 | 0 | 0 | 32 | ||||||
| MARV | 0 | 0 | 0 | 0 | ||||||
The two-injection VSV-based vaccine consisted of a recombinant VSV-based SEBOV vaccine given on day 0 and a combination of a recombinant VSV-based ZEBOV vaccine and a VSV-based MARV vaccine given on day 14. Animals were challenged on day 35 with SEBOV. Subjects 13 to 15 were back-challenged on day 73 with MARV.
DISCUSSION
This study demonstrates the feasibility of a single-injection panfilovirus vaccine and shows the potential to provide protection against multiple species and strains of filoviruses. In this study, cynomolgus macaques vaccinated with a single injection of a blended vaccine consisting of VSV vectors expressing the SEBOV GP, the ZEBOV GP, and the MARV (Musoke strain) GP were protected against four different filovirus species that have caused disease in humans: CIEBOV, SEBOV, ZEBOV, and MARV. Recently, a fifth putative species of EBOV was identified in Uganda (33). This species caused 37 deaths in 149 suspected cases (∼25% case fatality rate) and was reported to be most closely related to CIEBOV. As a combination of the SEBOV GP, the ZEBOV GP, and the MARV GP in our VSV vaccine resulted in the complete protection of nonhuman primates against CIEBOV in the current study, it seems reasonable to assume that this blended vaccination approach would also protect animals against the new EBOV species from Uganda. However, future studies will need to address protection against this newly identified EBOV. Regarding future development of filovirus vaccines, our finding that two control macaques that survived challenge with CIEBOV survived subsequent challenge with SEBOV and ZEBOV may have implications for vaccine design. It is possible that a filovirus vaccine expressing the CIEBOV GP may confer protection against all EBOV species. This would simplify production of a panfilovirus vaccine by reducing the number of necessary components from what appears to be three antigens (MARV GP, SEBOV GP, and ZEBOV GP) to two (MARV GP and CIEBOV GP).
Recently, a two-injection filovirus vaccine that is based on an adenovirus vector expressing multiple antigens from five different filoviruses (ZEBOV NP, ZEBOV GP, SEBOV GP, MARV Ci67 strain GP, MARV Ravn strain GP, MARV Musoke strain NP, MARV Musoke strain GP) was described (31). In this study, two groups of cynomolgus monkeys were given an initial i.m. injection of this vaccination and were then given a second injection of the vaccine 63 days later. The first group of vaccinated animals was challenged with the Musoke strain of MARV 42 days later and then back-challenged 72 days later with SEBOV. The second group of vaccinated animals was initially challenged with ZEBOV 43 days after the second vaccination and then back-challenged 69 days later with the Ci67 strain of MARV. All animals in these studies survived the initial filovirus challenge and a back-challenge with a different strain or species of filovirus. While these results show the potential of a multivalent filovirus vaccine, there are several concerns with the study and the adenovirus-based vaccine platform, including that (i) the vaccine as described requires two injections to elicit a protective response in nonhuman primates; (ii) a significant portion of the global population has preexisting antibodies against the adenovirus vector, which may affect efficacy (2, 23, 25) (in contrast, preexisting immunity against VSV in human populations is negligible [34]); (iii) this vaccine vector has performed poorly in recent highly publicized trials against human immunodeficiency virus in Africa (4, 26); and (iv) unfortunately, the two strains of MARV employed in this study (Musoke and Ci67) are remarkably similar in both sequence and disease course in nonhuman primates. There is no information on whether this vaccine would elicit a protective immune response against the seemingly most pathogenic Angola strain of MARV. As this strain has a much more rapid disease course in nonhuman primates than other MARV strains (13) and has been associated with higher mortality rates in humans than other MARV strains (32), it is unclear whether a replication-defective vaccine based on sequences of heterologous MARV strains would be able to protect against the Angola strain. We have recently shown that a single injection of our VSV-MARV vector expressing the GP of the Musoke strain can completely protect cynomolgus monkeys against challenge with either the Ravn strain or the Angola strain of MARV (6).
The main concern with the VSV vaccine vector is that replication-competent vectors may present more-significant safety challenges in humans, particularly those with altered immune status. In order to begin to address these concerns, we recently evaluated the safety of our replication-competent VSVΔG/ZEBOVGP vaccine in simian-human immunodeficiency virus-infected rhesus monkeys. We found that the vaccine caused no evidence of overt illness in any of these immunocompromised animals (14).
The serological response in almost all animals in the current study was weak to modest, a phenomenon that was described in our previous studies using the recombinant VSV vectors (6, 12, 20). Some of the control animals which were vaccinated with VSVΔG/LASVGPC showed low levels of anti-filovirus IgG (1:32) on day 14 after vaccination, which disappeared on day 28 and later (Table 3). This could be from cross-reactivity to cellular proteins due to antigen preparation in Vero cells but more likely represents a low affinity and a short-lived cross-reactivity to VSV or (less likely) to LASVGPC. VSV is a rhabdovirus and, as with filoviruses, a member of the order Mononegavirales. Some proteins of Mononegavirales (e.g., nucleoprotein and polymerase) are conserved, which could explain a certain cross-reactivity (10). Nevertheless, a transient titer of 1:32 most likely represents background reactivity rather than filovirus-specific IgG. The role of antibodies produced against vaccination with recombinant VSVs in protection against lethal filovirus challenge remains unclear. However, previous studies suggest a role for both cellular and humoral responses in protection (20).
In conclusion, the development of vaccines that require fewer injections and that can confer protection against multiple diseases or agents is highly desirable and will benefit first responders, family and household members, and laboratory workers. The results of the current study show that the use of replicating recombinant VSV-based vectors offers a promising approach to developing a single vaccine that can protect against all filovirus strains and species that cause disease in humans.
Acknowledgments
We thank John Crampton and Carlton Rice from USAMRIID for animal care. We thank Friederike Feldmann and Jason Gren from the National Microbiology Laboratory (NML) of the Public Health Agency of Canada (PHAC) for technical assistance. We are grateful to John Rose (Yale University) for kindly providing us with the VSV reverse-genetics system.
Work on filoviruses at USAMRIID was funded by the Defense Threat Reduction Agency (project number 04-4-7J-012). Work on filoviruses at the NML was supported by PHAC and through a grant awarded to H.F. from the Canadian Institutes of Health Research (MOP-39321).
Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by Boston University, the U.S. Army, the NIH, or PHAC.
Footnotes
Published ahead of print on 22 April 2009.
REFERENCES
- 1.Bowen, E. T., G. S. Platt, G. Lloyd, R. T. Raymond, and D. I. Simpson. 1980. A comparative study of strains of Ebola virus isolated from southern Sudan and northern Zaire in 1976. J. Med. Virol. 6129-138. [DOI] [PubMed] [Google Scholar]
- 2.Brandt, C. D., H. W. Kim, A. J. Vargosko, B. C. Jeffries, J. O. Arrobio, B. Rindge, R. H. Parrott, and R. M. Chanock. 1969. Infections in 18,000 infants and children in a controlled study of respiratory tract disease. I. Adenovirus pathogenicity in relation to serologic type and illness syndrome. Am. J. Epidemiol. 90484-500. [DOI] [PubMed] [Google Scholar]
- 3.Bukreyev, A., P. E. Rollin, M. K. Tate, L. Yang, S. R. Zaki, W. J. Shieh, B. R. Murphy, P. L. Collins, and A. Sanchez. 2007. Successful topical respiratory tract immunization of primates against Ebola virus. J. Virol. 816379-6388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen, J. 2007. AIDS research. Did Merck's failed HIV vaccine cause harm? Science 3181048-1049. [DOI] [PubMed] [Google Scholar]
- 5.Cyranoski, D. 2009. Ebola outbreak has experts rooting for answers. Nature 457364-365. [DOI] [PubMed] [Google Scholar]
- 6.Daddario-DiCaprio, K. M., T. W. Geisbert, J. B. Geisbert, U. Stroher, L. E. Hensley, A. Grolla, E. A. Fritz, F. Feldmann, H. Feldmann, and S. M. Jones. 2006. Cross-protection against Marburg virus strains using a live, attenuated recombinant vaccine. J. Virol. 809659-9666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daddario-DiCaprio, K. M., T. W. Geisbert, U. Stroher, J. B. Geisbert, A. Grolla, E. A. Fritz, L. Fernando, E. Kagan, P. B. Jahrling, L. E. Hensley, S. M. Jones, and H. Feldmann. 2006. Postexposure protection against Marburg haemorrhagic fever with recombinant vesicular stomatitis virus vectors in non-human primates: an efficacy assessment. Lancet 3671399-1404. [DOI] [PubMed] [Google Scholar]
- 8.Feldmann, H., T. W. Geisbert, P. B. Jahrling, H. D. Klenk, S. V. Netesov, C. J. Peters, A. Sanchez, R. Swanepoel, and V. E. Volchkov. 2004. Filoviridae, p. 645-653. In C. M. Fauquet, M. A. Mayo, J. Maniloff, U. Desselberger, and L. A. Ball (ed.), Virus taxonomy: eighth report of the international committee on taxonomy of viruses. Elsevier, London, United Kingdom.
- 9.Feldmann, H., S. M. Jones, K. M. Daddario-DiCaprio, J. B. Geisbert, U. Stroher, A. Grolla, M. Bray, E. A. Fritz, L. Fernando, F. Feldmann, L. E. Hensley, and T. W. Geisbert. 2007. Effective post-exposure treatment of Ebola infection. PLoS Pathog. 3e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feldmann, H., and H. D. Klenk. 1996. Marburg and Ebola viruses. Adv. Virus Res. 471-52. [DOI] [PubMed] [Google Scholar]
- 11.Garbutt, M., R. Liebscher, V. Wahl-Jensen, S. Jones, P. Moller, R. Wagner, V. Volchkov, H. D. Klenk, H. Feldmann, and U. Stroher. 2004. Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J. Virol. 785458-5465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geisbert, T. W., K. M. Daddario-DiCaprio, J. B. Geisbert, D. S. Reed, F. Feldmann, A. Grolla, U. Stroher, E. A. Fritz, L. E. Hensley, S. M. Jones, and H. Feldmann. 2008. Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine 266894-6900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geisbert, T. W., K. M. Daddario-DiCaprio, J. B. Geisbert, H. A. Young, P. Formenty, E. A. Fritz, T. Larsen, and L. E. Hensley. 2007. Marburg virus Angola infection of rhesus macaques: pathogenesis and treatment with recombinant nematode anticoagulant protein c2. J. Infect. Dis. 196(Suppl. 2)S372-S381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geisbert, T. W., K. M. Daddario-Dicaprio, M. G. Lewis, J. B. Geisbert, A. Grolla, A. Leung, J. Paragas, L. Matthias, M. A. Smith, S. M. Jones, L. E. Hensley, H. Feldmann, and P. B. Jahrling. 2008. Vesicular stomatitis virus-based Ebola vaccine is well-tolerated and protects immunocompromised nonhuman primates. PLoS Pathog. 4e1000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geisbert, T. W., K. M. Daddario-DiCaprio, K. Williams, J. B. Geisbert, A. Leung, F. Feldmann, L. E. Hensley, H. Feldmann, and S. M. Jones. 2008. Recombinant vesicular stomatitis virus vector mediates postexposure protection against Sudan Ebola hemorrhagic fever in nonhuman primates. J. Virol. 825664-5668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geisbert, T. W., P. B. Jahrling, T. Larsen, K. J. Davis, and L. E. Hensley. 2004. Filovirus pathogenesis in nonhuman primates, p. 203-238. In H.-D. Klenk and H. Feldmann (ed.), Ebola and Marburg viruses: molecular and cellullar biology. Horizon Bioscience, Norfolk, United Kingdom.
- 17.Geisbert, T. W., S. Jones, E. A. Fritz, A. C. Shurtleff, J. B. Geisbert, R. Liebscher, A. Grolla, U. Ströher, K. M. Daddario, M. C. Guttieri, B. R. Mothé, L. E. Hensley, P. B. Jahrling, and H. Feldmann. 2005. Development of a new rapid vaccine for the prevention of Lassa fever. PLoS Med. 2e183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hevey, M., D. Negley, P. Pushko, J. Smith, and A. Schmaljohn. 1998. Marburg virus vaccines based upon alphavirus replicons protect guinea pigs and nonhuman primates. Virology 25128-37. [DOI] [PubMed] [Google Scholar]
- 19.Jahrling, P. B., T. W. Geisbert, J. B. Geisbert, J. R. Swearengen, M. Bray, N. K. Jaax, J. W. Huggins, J. W. LeDuc, and C. J. Peters. 1999. Evaluation of immune globulin and recombinant interferon α-2b for treatment of experimental Ebola virus infections. J. Infect. Dis. 179(Suppl. 1)S224-S234. [DOI] [PubMed] [Google Scholar]
- 20.Jones, S. M., H. Feldmann, U. Stroher, J. B. Geisbert, L. Fernando, A. Grolla, H. D. Klenk, N. J. Sullivan, V. E. Volchkov, E. A. Fritz, K. M. Daddario, L. E. Hensley, P. B. Jahrling, and T. W. Geisbert. 2005. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat. Med. 11786-790. [DOI] [PubMed] [Google Scholar]
- 21.Le Guenno, B., P. Formenty, M. Wyers, P. Gounon, F. Walker, and C. Boesch. 1995. Isolation and partial characterisation of a new strain of Ebola virus. Lancet 3451271-1274. [DOI] [PubMed] [Google Scholar]
- 21a.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, DC.
- 22.Normile, D. 2009. Emerging infectious diseases. Scientists puzzle over Ebola-Reston virus in pigs. Science 323451. [DOI] [PubMed] [Google Scholar]
- 23.Piedra, P. A., G. A. Poveda, B. Ramsey, K. McCoy, and P. W. Hiatt. 1998. Incidence and prevalence of neutralizing antibodies to the common adenoviruses in children with cystic fibrosis: implication for gene therapy with adenovirus vectors. Pediatrics 1011013-1019. [DOI] [PubMed] [Google Scholar]
- 24.Sanchez, A., T. W. Geisbert, and H. Feldmann. 2006. Filoviridae: Marburg and Ebola viruses, p. 1409-1448. In D. M. Knipe, P. M. Howley, D. E. Griffin, et al. (ed.), Fields virology, 5th ed. Lippincott Williams & Wilkins, Philadelphia, PA.
- 25.Schulick, A. H., G. Vassalli, P. F. Dunn, G. Dong, J. J. Rade, C. Zamarron, and D. A. Dichek. 1997. Established immunity precludes adenovirus-mediated gene transfer in rat carotid arteries. Potential for immunosuppression and vector engineering to overcome barriers of immunity. J. Clin. Investig. 99209-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sekaly, R. P. 2008. The failed HIV Merck vaccine study: a step back or a launching point for future vaccine development? J. Exp. Med. 2057-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith, D. H., B. K. Johnson, M. Isaacson, R. Swanepoel, K. M. Johnson, M. Kiley, A. Bagshawe, T. Siongok, and W. K. Keruga. 1982. Marburg-virus disease in Kenya. Lancet i816-820. [DOI] [PubMed] [Google Scholar]
- 28.Sullivan, N. J., T. W. Geisbert, J. B. Geisbert, D. J. Shedlock, L. Xu, L. Lamoreaux, J. H. H. V. Custers, P. M. Popernack, Z.-Y. Yang, M. G. Pau, M. Roederer, R. A. Koup, J. Goudsmit, P. B. Jahrling, and G. J. Nabel. 2006. Immune protection of nonhuman primates against Ebola virus with single low-dose adenovirus vectors encoding modified GPs. PLoS Med. 3e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sullivan, N. J., T. W. Geisbert, J. B. Geisbert, L. Xu, Z. Y. Yang, M. Roederer, R. A. Koup, P. B. Jahrling, and G. J. Nabel. 2003. Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates. Nature 424681-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan, N. J., A. Sanchez, P. E. Rollin, Z. Y. Yang, and G. J. Nabel. 2000. Development of a preventive vaccine for Ebola virus infection in primates. Nature 408605-609. [DOI] [PubMed] [Google Scholar]
- 31.Swenson, D. L., D. Wang, M. Luo, K. L. Warfield, J. Woraratanadharm, D. H. Holman, J. Y. Dong, and W. D. Pratt. 2008. Complete protection of nonhuman primates against multistrain Ebola and Marburg virus infections. Clin. Vaccine Immunol. 15460-467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Towner, J. S., M. L. Khristova, T. K. Sealy, M. J. Vincent, B. R. Erickson, D. A. Bawiec, A. L. Hartman, J. A. Comer, S. R. Zaki, U. Ströher, F. Gomes da Silva, F. del Castillo, P. E. Rollin, T. G. Ksiazek, and S. T. Nichol. 2006. Marburgvirus genomics and association with a large hemorrhagic fever outbreak in Angola. J. Virol. 806497-6516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Towner, J. S., T. K. Sealy, M. L. Khristova, C. G. Albariño, S. Conlan, S. A. Reeder, P. L. Quan, W. I. Lipkin, R. Downing, J. W. Tappero, S. Okware, J. Lutwama, B. Bakamutumaho, J. Kayiwa, J. A. Comer, P. E. Rollin, T. G. Ksiazek, and S. T. Nichol. 2008. Newly discovered Ebola virus associated with hemorrhagic fever outbreak in Uganda. PLoS Pathog. 4e1000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wagner, R. R., and J. K. Rose. 1996. Rhabdoviridae: the viruses and their replication, p. 1121-1135. In D. M. Knipe and P. M. Howley (ed.), Fields virology. Lippincott Williams & Wilkins, Philadelphia, PA.
- 35.Warfield, K. L., D. L. Swenson, G. G. Olinger, W. V. Kalina, M. J. Aman, and S. Bavari. 2007. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J. Infect. Dis. 196(Suppl. 2)S430-S437. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. 1978. Ebola haemorrhagic fever in Sudan, 1976. Report of an international study team. Bull. W. H. O. 56247-270. [PMC free article] [PubMed] [Google Scholar]