Abstract
After the 2001 anthrax incidents, surface sampling techniques for biological agents were found to be inadequately validated, especially at low surface loadings. We aerosolized Bacillus anthracis Sterne spores within a chamber to achieve very low surface loading (ca. 3, 30, and 200 CFU per 100 cm2). Steel and carpet coupons seeded in the chamber were sampled with swab (103 cm2) or wipe or vacuum (929 cm2) surface sampling methods and analyzed at three laboratories. Agar settle plates (60 cm2) were the reference for determining recovery efficiency (RE). The minimum estimated surface concentrations to achieve a 95% response rate based on probit regression were 190, 15, and 44 CFU/100 cm2 for sampling steel surfaces and 40, 9.2, and 28 CFU/100 cm2 for sampling carpet surfaces with swab, wipe, and vacuum methods, respectively; however, these results should be cautiously interpreted because of high observed variability. Mean REs at the highest surface loading were 5.0%, 18%, and 3.7% on steel and 12%, 23%, and 4.7% on carpet for the swab, wipe, and vacuum methods, respectively. Precision (coefficient of variation) was poor at the lower surface concentrations but improved with increasing surface concentration. The best precision was obtained with wipe samples on carpet, achieving 38% at the highest surface concentration. The wipe sampling method detected B. anthracis at lower estimated surface concentrations and had higher RE and better precision than the other methods. These results may guide investigators to more meaningfully conduct environmental sampling, quantify contamination levels, and conduct risk assessment for humans.
Anthrax, the spectrum of diseases caused by infection with Bacillus anthracis, is not considered a communicable disease but is generally acquired via environmental exposures. Many anthrax cases through history have been the result of agricultural or industrial exposure to B. anthracis spores (33). The disease most often presents itself as a cutaneous infection; however, there are both gastrointestinal and inhalational forms of the disease. Inhalational anthrax is typically rapidly fatal, even with treatment. In general, inhalation exposures require specific conditions, such as poor ventilation and activities that disturb dust containing B. anthracis spores (13).
Because diagnosing anthrax in its early stages in human and animal hosts is difficult and B. anthracis spores are extremely stable in the environment, this microorganism has been investigated, developed, and deployed as a biological weapon throughout the 20th century. Use of this microorganism has seen varied success during World War I (9) and subsequently. It is generally accepted that there was an accidental release of B. anthracis spores from a weapons manufacturing or development facility in 1979 in Sverdlovsk, USSR (now Yekaterinaburg, Russia) (10, 26). In 1993, an attempt by a civilian group, Aum Shinrikyo, to use this microorganism to attack a civilian population in a Tokyo suburb did not result in any casualties (22, 28).
In 2001, envelopes containing a powder formulation of B. anthracis were mailed in the United States to several individuals. These letters were the presumed cause of 22 cases of clinical anthrax, 11 inhalational and 11 cutaneous, with 5 fatalities, all of whom suffered from inhalational disease (34). According to congressional testimony, the powdered spore suspension was “easily dispersed into the air” (29). Of the 11 individuals with inhalational disease, 2 had no history of handling mail or having any other direct contact with these threat letters (11, 21). Of the remaining nine individuals, eight were thought to have been exposed through handling or processing mail (20) but may never have picked up or directly handled the actual threat letters. Thus, some individuals who contracted inhalational disease may have been exposed to aerosols that were generated from residual spore material deposited on contaminated surfaces. This conclusion was borne out by a study conducted on the scene of one contamination incident, which demonstrated that spores could be reaerosolized from surfaces during simulated office activities—e.g., paper handling, foot traffic, moving containers—after a period of no entry and no ventilation for several days (38). McCleery et al. (25) found that reaerosolization of spores is possible in postal facilities.
In the mail-related instance of 2001, aerosol exposures occurred. Since spore-contaminated surfaces can become sources for aerosol generation, nonporous surfaces (walls, desks, lockers, etc.) were decontaminated to reduce risk while porous surfaces (draperies and sofas) were removed. To determine the efficacy of decontamination, contaminated buildings were first sampled for the presence of B. anthracis spores followed by treatment by a variety of techniques. Postdecontamination sampling was used to determine efficacy (37) and to assess the safety for reoccupancy.
The Government Accountability Office (GAO) reported that additional methodological validation of sampling collection and analytical methods should be conducted to enhance the interpretation of negative sampling results because initial samples from two postal facilities were negative, but later samples were positive (17). The GAO (17) report defined validation as “… a formal and independently administered empirical process. For validation, the overall performance characteristics of a given method must be certified as meeting the specified requirements for intended use and as conforming with applicable standards.” Currently, there is no preexisting standard for a presumable safe level of surface contamination with B. anthracis spores that may be assessed through sampling and analysis.
Development of independent standards for assessing the requirements for surface sampling methods requires an understanding of the rate at which spores leave surfaces to become entrained in aerosols, the potential for aerosol exposure by humans, and the infectivity of inhaled spores. Inhalation infectivity has been researched, but estimates of a lethal dose vary (14, 15). Bartrand et al. (5) conducted a risk analysis on the mortality of guinea pigs and rhesus monkeys exposed to B. anthracis spores and found a 50% lethal dose (LD50; i.e., the dose at which 50% of subjects die) of about 100,000 spores inhaled for 1-μm particles. Limitations of relating exposure to inhalation infectivity include quantification of the ability of spores to move from stasis on a surface to entrainment as an aerosol, quantification of exposures to the resultant aerosol, uptake by humans, room size and ventilation characteristics, and exposure time. Despite these limitations, it is necessary to standardize the performance of surface sampling methods.
Brown et al. evaluated wipe (6), swab (7), and vacuum (8) spore collection methods with B. atrophaeus. These studies have added significant information to the understanding of recovery efficiencies for these three sampling methods; however, sampling performance was not evaluated at very low spore surface loading concentrations. Sampling performance measures at very low surface loading of B. anthracis are needed to aid in the decision making for decontamination and other interventions (31, 38).
The goal of this study was to evaluate the current CDC environmental surface sampling methods for B. anthracis (12) as slightly modified based on subsequent CDC research (19, 30). We estimated B. anthracis Sterne sampling limit of detection (LOD), recovery efficiency (RE), and measurement precision for three sampling methods (swab, wipe, and vacuum) and two surfaces (steel and carpet) by allowing spores to settle from an aerosol in a controlled environment. In addition, we compared sample analyses performed at three laboratories to determine the level of interlaboratory variability.
MATERIALS AND METHODS
Spore preparation and settling chamber.
B. anthracis Sterne spores were prepared as follows. Ten-liter fermentation vessels were seeded (5% [vol/vol]) with overnight nutrient broth cultures of B. anthracis Sterne. Spores were grown in G medium, which consists of the following: yeast extract, 2.0 g liter−1; NH4SO4, 2.0 g liter−1; Dow antifoam 204, 0.3 ml liter−1; MgSO4·7H2O, 0.2 g liter−1; MnSO4·H2O, 0.038 g liter−1; ZnSO4·7H2O, 0.005 g liter−1; CuSO4·5H2O, 0.005 g liter−1; FeSO4·7H2O, 0.005 g liter−1; CaCl2·2H2O, 0.25 g liter−1; K2HPO4, 0.500 g liter−1; and glucose, 1.0 g liter−1. The pH was adjusted to 7.0 ± 0.1, and the glucose was added separately as a sterile solution after autoclaving.
The culture was incubated at 30°C in a 10-liter fermentation vessel with an agitation rate of 250 rpm and an aeration rate greater than 0.5 volume min−1. Sporulation was generally complete within 24 h. Spores were collected by simple centrifugation to remove spent media. The pelleted material was dried by a proprietary azeotropic method. Ten percent (by weight) of an amorphous silica-based flow enhancer was added to the dried spores. The dried material was milled using an exclusionary ball mill. In this process, the material passed through a series of stages separated by increasingly finer mesh screens. In each stage, 0.01-m-diameter steel balls forced the product through the screen separators. A pneumatic vibrator actuated the entire mill. The resulting spores were approximately 1.0 μm.
Two solutions were used for suspending spores: phosphate-buffered saline (PBS, Sigma Aldrich, St. Louis, MO) and Butterfield buffer with Tween 80 (BBT) (0.01%, pH 7.2; Becton Dickson Microbiology, Franklin Lakes, NJ). Plates of trypticase soy agar (TSA) with 5% sheep blood (TSAII, Becton Dickenson Microbiology, Franklin Lakes, NJ) were used by all labs to incubate samples from the surface sampling media (swab, wipe, and vacuum) at 35°C to 37°C for 16 h to 18 h before colonies were enumerated.
Plastic petri plates (60 cm2) (no. 35-1029; Falcon Products, San Jose, CA) filled to the rim with TSA (Acumedia; Neogen Corp., Lansing, MI) were used for reference samples. Filling to the rim reduced turbulence near the edge of the plates and produced more even particle deposits on the surface (4). In preliminary runs, Baron et al. (4) compared three processing techniques for settling plates and found “spreading” to have the highest recovery for comparison to surface sampling. Consequently, 100 μl of BBT was placed onto each agar plate, which was rotated on a turntable for 1 min while using a spreader to spread the spores. This technique was used to improve particle adhesion. Plates were incubated at 35°C to 37°C for 16 h to 18 h before colonies were enumerated. Agar plates were used as the reference to avoid particle loss that could occur with other processing techniques. Baron et al. (4) determined that the culturable fraction using the agar spreading technique was 0.16 (range, 0.098 to 0.23) for medium (20 CFU/plate) and high (160 CFU/plate) concentrations, while at the low (4.8 CFU/plate) concentration, the range was 0.066 to 0.31. The culturable fraction was the average concentration on the agar reference plates divided by particles in the 1.114- to 1.596-μm range (as measured with the Aerodynamic particle sizer [APS], model APS 3321; TSI, Inc., Shoreview, MN) for the volume of air above the plates.
A settling chamber (4) which was 1.22 m high with a cross section of 1.22 m by 2.44 m was constructed at Dugway Proving Ground with static-dissipative Plexiglas walls and an extruded-aluminum frame. Dry spore-containing particles were aerosolized into this settling chamber using an aerosol generation system and allowed to settle onto coupons. The aerosol generation system consisted of a small-scale powder disperser (model 433; TSI, Inc., Shoreview, MN), an impactor (model 266 Marple Impactor; Sierra Instruments, Carmel Valley, CA) to remove particles greater than 5 μm, and a mixing tunnel with a turbulence induction element propelled by nitrogen dilution gas with an ion air cannon static eliminator (Exair, Inc., Cincinnati, OH). Sampling locations within the chamber are indicated in Fig. 1. The chamber contained six sampling shelves (0.24 m above the bottom), machined on both sides to accommodate the different thicknesses of carpet or stainless steel sample coupons. The shelves could accommodate 30 sample coupons and 16 reference agar plates. Each sample location had a machined nonconductive Plexiglas cover with a tongue that fit into a matching groove on the shelf. The grooves were coated with silicone vacuum grease to reduce aerosol infiltration.
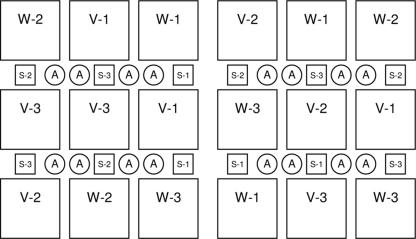
FIG. 1.
Layout of the chamber and an example of method and laboratory sample assignment. The large (929 cm2) and small (103 cm2) squares indicate the locations of the test coupons (stainless steel or carpet). The circles (60 cm2) indicate the reference agar plate (A) locations. For each chamber run, the method (S, swab; W, wipe, and V, vacuum) and laboratory (1, 2, and 3) were randomly assigned to each square test coupon as described in the text.
Between trials, all chamber surfaces were decontaminated with vaporous hydrogen peroxide (VHP) (model VHP1000; Steris Corp., Mentor, OH) by injection of VHP nominally at 1,000 ppm for 90 min. The VHP was out-gassed from the chamber surfaces by heating the chamber at approximately 43°C for about 3 days. This out-gassing procedure ensured that residual hydrogen peroxide levels did not interfere with subsequent spore recovery and is described in detail elsewhere (3). The sample covers and the inside surfaces of the steel and carpet sample holders were coated with aluminum tape (5-cm-wide heating system duct tape) to reduce sorption and release of the sterilization agent, namely, hydrogen peroxide (3).
Sampling coupons.
Test coupons included stainless steel and carpet squares. Small squares (103 cm2) were used for the swab method, and large squares (929 cm2) were used for wipe and vacuum methods. Swab test coupons were smaller because the smaller swab end makes it difficult and time-consuming to sample larger areas. Carpet coupons (style Browning 26; Shaw Industries, Dalton, GA) with a 0.6-cm tufted pile height were used a single time and then discarded. Stainless steel coupons (S-180 grade, T-304; Stewart Stainless Supply, Inc., Suwanee, GA) were washed with water and autoclaved between uses.
Chamber operation.
Separate experimental runs were performed with either the steel or carpet coupons placed in the sample holders. Covers were placed over the coupons and sealed with grease. The covers and other horizontal surfaces of the chamber, rubber gloves, and fan blades were coated with a light oil (WD-40, San Diego, CA) to reduce resuspension of particles as proposed by Turner and Hering (36). The chamber was sealed and purged for about 3 h with HEPA-filtered air. Aerosol concentration during the chamber runs was monitored in real time (averaging 5 min) with an APS. B. anthracis Sterne spores were aerosolized using the generation system. The relationship between aerosol particle count and the CFU count on exposed agar plates was determined from previous experiments as explained by Baron et al. (4). Purging of the chamber (as described above) followed for about 20 min to 45 min to reduce the aerosol concentration in the chamber. The concentration was further reduced by stirred settling while operating the four chamber fans alternately for 1 s each on a 4-min cycle. Stirred settling consists of providing limited air movement to improve mixing while maintaining very low air velocity at the sampling surface to reduce impaction and aerosol resuspension. Twenty minutes after active pumping, the exponential concentration decay monitored with the APS was modeled using an exponential decay equation (4, 18). This decay was used to forecast the time at which the chamber would reach the intended air concentration for uncovering sample surfaces to allow spores to be deposited. Once the forecast time was reached, chamber glove ports allowed access to open all sample covers and expose the test coupons and agar settle plates. During 10 h of stirred settling, 99% of the 1- to 2-μm particles were expected to settle onto the surfaces (4). After the 10-h settling period, all coupons and settle plates were covered and the remaining aerosol in the chamber was removed by evacuating the chamber using the vacuum pump for 1 h. After this final evacuation, the chamber door was opened and the agar settle plates were removed for incubation. With covers still in place over the test coupons, the horizontal surfaces within the chamber were wiped with sodium hypochlorite (1:10 dilution in Fox-Chlor household bleach; Superclean Brands, Inc., St. Paul, MN) and allowed to air dry with the chamber vacuum pump running for 30 min. After drying, the covers were removed one at a time and the coupons were sampled using the techniques indicated below. Then the chamber was sterilized as described above.
Comparison of sampling methods and laboratories.
Stainless steel and carpet coupons were evaluated independently by dispersion into the chamber of three challenge concentrations: 0.004, 0.018, and 0.168 particles per cm3, as measured by an APS. These air concentrations roughly corresponded to 3 CFU/100 cm2, 30 CFU/100 cm2, and 200 CFU/100 cm2, henceforth denoted as the low, medium, and high target concentrations, respectively. Three runs were conducted at each concentration using stainless steel coupons followed by three runs at each concentration using carpet coupons. The order of the target concentrations was randomly assigned within each surface material. These runs were used to compare the efficiencies of particle removal for the three sampling methods (swab, wipe, and vacuum) and the performance of three laboratories. Following dispersion, the test coupons were sampled using methods described below. Sixteen agar settle plates placed in the chamber during each run were used to estimate true spore surface loading without the added variability introduced by the sampling and processing methods. Thirty coupons were placed into the chamber for each run: nine large test coupons were sampled via the wipe method, nine large test coupons were sampled via the vacuum method, and 12 small test coupons (103 cm2) were sampled via the swab method. One-third of the samples were analyzed at each of three laboratories (labs 1, 2, and 3). Surfaces within the chamber were randomized for sampling method and laboratory (Fig. 1). Samples were shipped with ice packs by overnight delivery. All three laboratories coordinated the date to process the samples.
Swab, wipe, and vacuum sampling methods.
The same technician collected all samples applying the techniques described below. A firm uniform sample collection force was used for all surfaces. Gloves were worn during all sample collections and changed after every sample. All samples were placed in sample vials and sealed with Parafilm (Pechiney Plastic Packaging Company, Chicago, IL) before shipment. Three chamber blank samples of each type were collected directly outside the chamber door for each run by wetting the swab or wipe or placing the vacuum sock over the vacuum nozzle and then immediately placing the sample into the specimen tube for lab processing.
Swab samples were collected using foam critical swabs (catalog no. 10812-016; VWR International, Suwanee, GA), which previously were reported to have good recovery in work by the CDC (19, 30). Swabs were premoistened with 0.2 ml BBT. Each 103-cm2 surface was swabbed back and forth using several S strokes. The foam swabs were used to swab the surface in a horizontal direction and then the swab was turned to the other side and moved in a vertical direction across the surface. Swabs were placed in their prelabeled tubes after sampling.
Wipe samples were collected using Versalon all-purpose sponges (5 cm by 5 cm [catalog no. 8042]; Kendall Healthcare, Mansfield, MA) premoistened with 1.0 ml BBT. Each 929-cm2 surface was wiped back and forth with one sponge using vertical S strokes to cover the entire sample area. The sponge was then folded, and several horizontal S strokes were made over the same area with the other side of the wipe (12). When sampling was complete, the sponge was placed in a prelabeled, sterile Kendall screw-cap wide-mouth plastic specimen cup (VWR catalog no. 13915-774).
Vacuum filter samples were collected using vacuum socks (FAB-20-01-001A; Midwest Filtration, Inc., Fairfield, OH). The vacuum sock was inserted into the nozzle of the Omega HEPA abatement vacuum (Atrix Intl., Burnsville, MN) and held in place with a gloved hand. Each 929-cm2 surface was vacuumed by slowly pulling the nozzle (6 cm/s) across the surface with strokes 2.5 cm apart until the entire surface was vacuumed one time (12). Then a second pass was made in a perpendicular direction to the first. When the sampling was completed, the vacuum sock was removed from the vacuum nozzle and placed into a specimen cup, as described above. The vacuum nozzle exterior was wiped down with a bleach-dampened wipe (1:10 dilution of household bleach) between each vacuum sample.
Lab processing methods.
Each swab was placed into a tube containing 5 ml of BBT and vortexed for 2 min in 10-s bursts. The swab was removed, and the remaining eluent was vortexed and sonicated (40 kHz) for 30 s each. Three 1.5-ml aliquots of suspension were filtered onto 0.45-μm mixed cellulose ester filters (catalog no. 4800; Pall Corp., East Hills, NY). The filters were placed onto TSAII plates and incubated (as described above), and colonies were enumerated.
Fifty milliliters of BBT was added to each specimen cup containing wipe or vacuum sock samples. The vacuum sock samples were cut with sterile scissors vertically and horizontally, alternately submerging and cutting to wet the contents and reduce aerosolization. Each specimen cup was sealed with Parafilm, placed in a sealed biotransport box, and agitated for 30 min at 300 rpm. After agitation, 45 ml of the eluent was placed into a 50-ml tube and centrifuged at 3,500 × g for 15 min. The supernatant (42 ml) was discarded and the remaining 3 ml was vortexed and sonicated for 30 s each, with the cycle repeated two additional times. The resuspended eluent was filtered (in triplicate), placed onto TSAII plates, and incubated (as described above), and colonies were enumerated.
Sequential sampling passes.
Two additional runs evaluated collection efficiency using repeated sampling passes of the same surface (stainless steel and carpet) at the high target concentration. Each surface was sampled three consecutive times using new collection material. For each collection, the collection material was passed over the horizontal surfaces twice, with the second pass completed at a 90° angle to the first as described above. The spores remaining on the test coupons after sampling were removed by placing the surfaces into stomacher bags with BBT and processing them according to the stomacher (Seward model 3500; Seward, London, United Kingdom) instructions for 4 min on high (0.1 liter of BBT for small carpet samples and all steel samples, with 0.6 liter of BBT for large carpet samples). These wash samples were plated onto TSAII and incubated (as described above), and colonies were enumerated.
Statistical methods.
Statistical analyses were performed using SAS software (version 9.1; SAS Institute, Inc., Cary, NC). Numbers of B. anthracis Sterne CFU per sample were converted to an estimated surface concentration (CFU/100 cm2) using appropriate sampling fractions, volumes, and surface sampling areas.
LOD.
AOAC International (1) defines the LOD for qualitative methods as “one analyte particle in some undetermined upper limit of analytical sample size (conventionally 25 g).” The National Institute for Occupational Safety and Health defines the LOD for chemical sampling methods as 3 standard deviations above the mean of a blank instrument signal (23). These definitions, however, were not applicable to our experimental data, which consisted of, for each chamber run, an estimated surface concentration based on the agar reference plates and multiple samples (12 swab samples and 9 each of wipe and vacuum samples) that either detected B. anthracis or did not. We defined LOD for this study as the lowest surface concentration of B. anthracis Sterne for which the sampling method detected B. anthracis Sterne with a probability of 0.95 (LOD95) as estimated by probit regression (16, 35). Probit regression has been used in other settings (14) to determine “lethal dose” (or LD50) or “effective dose” (or 50% effective dose [ED50]). Probit analysis allows one to estimate the minimum concentration required to achieve a specified response rate. The probit regression model was
 |
where yij is the response (i.e., 0 = nondetection and 1 = detection) for the jth sample from the ith run, Ai is the mean agar concentration for the ith run, and Φ is the cumulative standard normal distribution function. Therefore, the estimated surface concentration to achieve a 95% response rate is given by
 |
where β̂0 and β̂1 are parameter estimates from the SAS PROBIT procedure. The Pearson chi-square test was used to assess model fit; for models with evidence of inadequate fit, we considered the use of generalized linear mixed models (SAS NLMIXED procedure) that included a random intercept term (2). All models assumed a natural response rate of zero, and confidence intervals (CIs) were calculated using Fieller's procedure (16). Initially, LODs were estimated using data from the 18 chamber runs. Because few negative results were observed, particularly for the wipe and vacuum sampling methods, two runs were added (one each for carpet and steel), using an even lower target concentration (i.e., <3 CFU/100 cm2), and the results of these runs were additionally used to estimate LODs for the wipe and vacuum sampling methods. Generally, a sample was defined to have detected B. anthracis Sterne if 1 or more CFU were observed; however, for wipe and vacuum sampling on steel, 3 or more CFU were required for a positive sample because 4 of 30 wipe and 8 of 30 vacuum chamber blanks from steel runs were positive for CFU. Twelve of the positive chamber blank samples had no more than 2 CFU on triplicate filters, and the highest sample resulted in only 5 CFU. For chamber runs involving carpet coupons and swab sampling on steel, no adjustment to LOD definition was made because few blanks were positive for CFU (1 of 27 swab samples on steel, 1 of 27 swab samples on carpet, 0 of 30 wipe samples on carpet, and 2 of 30 vacuum samples on carpet). All laboratory control samples were negative for CFU.
RE.
Sixteen agar plates were available as referents for each run. RE was computed based on these agar referents for each combination of surface material, target concentration, and sampling method as
 |
where nr was the number of chamber runs, ns was the number of collected samples, xij was the measured result from the jth sample from the ith run (i = 1 … nr, j = 1 … ns), and Ai was the mean of the agar results from run i.
Precision.
Precision, defined as the coefficient of variation (CV), was estimated using mixed-effects modeling (SAS MIXED procedure). Separate models were constructed for each combination of surface material, target concentration, and sampling method. All models specified the estimated surface concentration (CFU/100 cm2) as the dependent variable and included a random effect for chamber run resulting in between-run (σ2B) and within-run (σ2W) variance components. For the agar results, the estimated CV was
 |
where S2W was the estimated within-run variance and A was the estimated agar mean. For the swab, wipe, and vacuum methods, the models contained an additional random effect for laboratory so the within-run variance component was further partitioned into between-lab (σ2L) and within-lab (σ2W) variance components. For each sampling method, the estimated CV was
 |
where S2L was the estimated between-lab variance, S2W was the estimated within-lab variance, and M was the estimated sampling method mean. Initially, the side of the chamber (left and right) was considered an additional random effect (nested within chamber run) since samples were collected in two subrectangles within the chamber; however, the corresponding variance component was either zero or relatively small and the chamber side was not considered further.
Sampling method comparison.
The sampling methods were compared using mixed-effects modeling (SAS MIXED procedure). Separate models were constructed for each combination of surface material and target concentration. In these models, the dependent variable was the estimated surface concentration, run and laboratory were random effects, and sampling method and the mean agar concentration were fixed effects. Levels of the fixed effects were compared using the Tukey-Kramer adjustment for multiple comparisons. With the exception of a couple of outliers in the data, model residuals were approximately normally distributed.
RESULTS
LOD.
The wipe method detected B. anthracis Sterne at lower surface concentrations when sampling on stainless steel than the swab and vacuum sampling methods (Table 1). Wipe samples were estimated to detect B. anthracis Sterne on stainless steel surfaces with concentrations as low as 15 CFU/100 cm2 with a probability of 0.95 (95% CI, 7.6 to 84 CFU/100 cm2). Vacuum samples were estimated to detect stainless steel surface concentrations as low as 44 CFU/100 cm2 with a probability of 0.95 (95% CI, 24 to 140 CFU/100 cm2). Note that LOD estimates for wipe and vacuum on stainless steel required 3 or more CFU for a positive result because positive blank samples were observed for the wipe and vacuum methods during the stainless steel chamber runs. All other surface-method combinations required 1 or more CFU for a positive result. There was some evidence of lack of fit in the steel-swab model, likely due to results from a single run with a high surface loading but many negative results; consequently, the random-intercept probit model, which provided a significant improvement in model fit, was used to estimate the model parameters. To achieve a 95% detection rate using the swab sampling method on stainless steel, an estimated surface concentration of 190 CFU/100 cm2 is required (95% CI, 74 to 3,700 CFU/100 cm2).
TABLE 1.
Estimated LOD by surface material and sampling method
| Surface | Method | No. of runs | No. of samples | LODa
|
|||
|---|---|---|---|---|---|---|---|
| CFU/100 cm2
|
CFU/sampled areab
|
||||||
| LOD95 | 95% CI | LOD95 | 95% CI | ||||
| Steel | Swabc | 9 | 107 | 190 | 74-3,700 | 200 | 76-3,800 |
| Wiped | 10 | 90 | 15 | 7.6-84 | 140 | 71-780 | |
| Vacuumd | 10 | 90 | 44 | 24-140 | 410 | 230-1,300 | |
| Carpet | Swab | 9 | 108 | 40 | 16-560 | 41 | 17-580 |
| Wipe | 10 (9)e | 90 (81) | 9.2 (9.9) | 1.8-2.7 × 1031f (4.6-760) | 85 (92) | 17-2.5 × 1032f (42-7,100) | |
| Vacuum | 10 | 90 | 28 | 14-130 | 260 | 130-1,300 | |
The LOD, defined here as the lowest concentration that could be detected (i.e., positive for CFU) with LOD95, was estimated using probit regression (SAS PROBIT procedure), and 95% CIs were estimated using Fieller's procedure (15).
The sampled surface areas were approximately 103 cm2 for the swab method and 929 cm2 for the wipe and vacuum methods.
Steel-swab combination results exclude a single sample with contaminant overgrowth.
The steel-wipe and steel-vacuum combinations required 3 or more CFU for a positive result (see text for details); all other surface-method combinations required 1 or more CFU for a positive result.
The carpet-wipe combination CI was very wide, likely due to the results of a single run in which 100% of the wipe samples were positive in spite of the very low surface loading; results excluding this run are in parentheses.
The 95% CI for the carpet-wipe combination could not be computed due to constraints imposed by Fieller's method; results shown have 94% confidence rather than 95% confidence.
The wipe sampling method also detected B. anthracis Sterne on carpet at lower surface concentrations than the swab and vacuum sampling methods (Table 1). Wipe, vacuum, and swab samples were estimated to detect 1 or more CFU with a probability of 0.95 at surface concentrations of 9.2 CFU/100 cm2, 28 CFU/100 cm2, and 40 CFU/100 cm2, respectively. A 95% CI for the wipe method on carpet could not be computed due to constraints imposed by Fieller's method; consequently, a 94% CI was reported. The 94% CI for the wipe method on carpet was very wide, likely due to the results of a single run in which 100% of the wipe samples were positive in spite of the very low surface loading; the LOD95 estimate for wipe sampling on carpet excluding this run was 9.9 CFU/100 cm2 (95% CI, 4.6 to 760 CFU/100 cm2).
Since the sampled area was approximately nine times larger for the wipe and vacuum sampling methods compared to the swab method, LOD results are also provided in Table 1 in terms of CFU per sampled area. In terms of CFU/sampled area, the wipe method has the lowest LOD when sampling on stainless steel (140 CFU/sampled area), but the swab method has the lowest LOD when sampling on carpet (41 CFU/sampled area).
RE.
Target deposition was approximately 3, 30, and 200 CFU/100 cm2, for low, medium, and high, respectively; however, actual deposition varied (Table 2). The CV for the agar concentrations decreased from approximately 200% for the low target runs to approximately 19 to 26% for the high target runs, but the amount of variability expected relative to the Poisson distribution was always above 100% (Table 2). Mean RE was highest for the wipe sampling method compared to the swab and vacuum sampling methods, but variability was high, especially at the lowest target concentration (Table 2).
TABLE 2.
Mean, CV, and percentage of Poisson variability for agar reference plates and mean, median, and CV of RE by surface material, target concentration, and sampling method
| Surface | Targeta | Reference agarb
|
RE (%)c
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of samples | Mean (CFU/100 cm2) | CV (%) | % of Poisson variability | Sampling method | No. of samples | Mean | Median | CV (%) | ||
| Steel | Low (3 runs) | 48 | 8.3 | 230 | 510 | Swab | 36 | 3.4 | 0 | 550 |
| Wipe | 27 | 31 | 13 | 160 | ||||||
| Vacuum | 27 | 5.5 | 4.2 | 91 | ||||||
| Medium (3 runs) | 48 | 38 | 30 | 140 | Swab | 36 | 6.5 | 6.1 | 80 | |
| Wipe | 27 | 22 | 17 | 82 | ||||||
| Vacuum | 27 | 4.7 | 3.2 | 82 | ||||||
| High (3 runs) | 48 | 270 | 19 | 240 | Swab | 35 | 5.0 | 3.8 | 98 | |
| Wipe | 27 | 18 | 15 | 56 | ||||||
| Vacuum | 27 | 3.7 | 3.0 | 78 | ||||||
| Carpet | Low (2 runs) | 32 | 1.8 | 190 | 190 | Swab | 24 | 12 | 0 | 250 |
| Wipe | 18 | 120 | 4.5 | 220 | ||||||
| Vacuum | 18 | 6.3 | 2.1 | 130 | ||||||
| Medium (4 runs)d | 64 | 17 | 97 | 300 | Swab | 48 | 14 | 7.7 | 120 | |
| Wipe | 36 | 21 | 12 | 110 | ||||||
| Vacuum | 36 | 3.7 | 2.0 | 120 | ||||||
| High (3 runs) | 48 | 190 | 26 | 270 | Swab | 36 | 12 | 8.6 | 96 | |
| Wipe | 26 | 23 | 17 | 66 | ||||||
| Vacuum | 27 | 4.7 | 2.7 | 91 | ||||||
Target deposition densities were approximately 3, 30, and 200 CFU/100 cm2 for low, medium, and high, respectively.
The CV for agar results is 100% × the within-run standard deviation/agar mean; the percentage of Poisson variability is 100% × CV/Poisson CV, where Poisson CV = 100% × expected standard deviation/mean = 100% × (mean)1/2/mean.
RE (%) based on the reference agar is 100% × the mean (over all runs) of the mean (over all samples) of the ratio of the method result (based on a single sampling pass) to the mean agar result.
A single carpet run was intended to be low but was considered to be medium based on the agar results.
Precision.
Precision (i.e., within-run CV) of the sampling methods was poor (100 to 470%) at the low target concentration but improved with increasing surface concentration, with wipe samples on carpet achieving precision of about 40% at the highest target concentration (Table 3). Since agar precision represents deposition variability within the chamber, precision for the swab, wipe, and vacuum methods would not be expected to be better (i.e., lower CV) than the agar. Between-lab variability (CVL), always lower than within-lab variability (CVW), was higher at the lowest target concentrations and generally, but not always, lower for the wipe sampling method (Table 3).
TABLE 3.
Precision and mean estimated surface concentration by surface material, target concentration, and sampling method
| Surface | Targeta | Method | Precision CV(%)b
|
Concn (CFU/100 cm2)c
|
|||||
|---|---|---|---|---|---|---|---|---|---|
| CVR | CVL | CVW | CVmethod | No. | Mean | 95% CI | |||
| Steel | Low (3 runs) | Reference agar | 5.6 | 230 | 48 | 8.3 | 0-20 | ||
| Swab | 0 | 110 | 460 | 470 | 36 | 0.12 | 0-1.4 A | ||
| Wipe | 0 | 8.5 | 200 | 200 | 27 | 2.3 | 1.1-3.6 AC | ||
| Vacuum | 50 | 38 | 98 | 100 | 27 | 0.43 | 0-1.7 C | ||
| Medium (3 runs) | Reference agar | 19 | 30 | 48 | 38 | 19-57 | |||
| Swab | 27 | 0 | 82 | 82 | 36 | 2.5 | 0-6.5 A | ||
| Wipe | 28 | 27 | 76 | 80 | 27 | 8.4 | 5.0-12 AC | ||
| Vacuum | 0 | 18 | 82 | 84 | 27 | 1.8 | 0-5.2 C | ||
| High (3 runs) | Reference agar | 30 | 19 | 48 | 270 | 65-480 | |||
| Swab | 87 | 19 | 75 | 78 | 35 | 15 | 0.47-29 A | ||
| Wipe | 45 | 25 | 61 | 66 | 27 | 50 | 36-64 AC | ||
| Vacuum | 5.8 | 35 | 82 | 89 | 27 | 10 | 0-24 C | ||
| Carpet | Low (2 runs) | Reference agar | 34 | 190 | 32 | 1.8 | 0-11 | ||
| Swab | 0 | 85 | 220 | 230 | 24 | 0.18 | 0-1.1 A | ||
| Wipe | 0 | 26 | 180 | 180 | 18 | 1.7 | 0.80-2.7 AC | ||
| Vacuum | 0 | 0 | 170 | 170 | 18 | 0.11 | 0-1.1 C | ||
| Medium (4 runs)d | Reference agar | 0 | 97 | 64 | 17 | 10-23 | |||
| Swab | 98 | 0 | 73 | 73 | 48 | 2.3 | 0-5.7 B | ||
| Wipe | 52 | 9.3 | 100 | 100 | 36 | 3.4 | 0.14-6.8 C | ||
| Vacuum | 57 | 0 | 110 | 110 | 36 | 0.61 | 0-3.9 BC | ||
| High (3 runs) | Reference agar | 62 | 26 | 48 | 190 | 0-470 | |||
| Swab | 40 | 21 | 57 | 61 | 36 | 18 | 0-64 AB | ||
| Wipe | 47 | 8.6 | 37 | 38 | 26 | 35 | 0-77 AC | ||
| Vacuum | 37 | 30 | 44 | 53 | 27 | 6.2 | 0-48 BC | ||
Target deposition densities were approximately 3, 30, and 200 CFU/100 cm2 for low, medium, and high, respectively.
Precision (CV) was estimated using the MIXED procedure in SAS. The model for reference agar included a random effect for chamber run resulting in between-run (σ2B) and within-run (σ2W) variance components. Separate models for each of the sampling methods included random effects for chamber run and laboratory resulting in between-run (σ2B), between-lab (σ2L), and within-lab (σ2W) variance components. For each source of variation, CV = 100% × [(σ2source)½/Mean], so CVR is the between-run CV, CVL is the between-lab CV, and CVW is the within-run (agar) or within-lab (sampling methods) CV. For the sampling methods, CVmethod incorporates both between-lab and within-lab variability.
Means and 95% CIs were estimated using the MIXED procedure in SAS. The model for reference agar included a random effect for chamber run. The model for the sampling methods included random effects for chamber run and laboratory and fixed effects for mean agar and method. Means for sampling methods with the same letter are significantly different (Tukey-Kramer adjusted P value of <0.05).
A single carpet run was intended to be low but was considered to be medium based on the agar results.
Sampling method comparison.
The mean surface concentration based on the wipe sampling method was higher than the swab and vacuum sampling methods (Table 3). The difference was statistically significant for sampling on steel surfaces and for sampling on carpet at the low and high target concentrations (marginally significant for carpet at medium). In addition, at the medium and high target concentrations on carpet, the mean surface concentration based on the swab sampling method was significantly higher than that of the vacuum sampling method.
Sequential sampling passes.
Results for the sequential sample passes and wash solution from two additional runs at the high target concentration are shown in Table 4. The first sampling pass over steel coupons collected a majority (87, 95, and 88% for swab, wipe, and vacuum, respectively) of the recovered CFU from the sum of the three passes and the final wash sample. However, the first sampling pass over carpet coupons collected much lower percentages (8.9, 20, and 26% for swab, wipe, and vacuum, respectively), with the majority (86, 64, and 70% for swab, wipe, and vacuum, respectively) recovered in the wash solution.
TABLE 4.
Results of repeated sampling passes and final wash solution by surface material and sampling method
| Surface | Parameter | Result for:
|
|||||
|---|---|---|---|---|---|---|---|
| Swab
|
Wipe
|
Vacuum
|
|||||
| Mean | CV | Mean | CV | Mean | CV | ||
| Steel | No. of reference plates | 16 | 16 | 16 | |||
| Reference agar (CFU/100 cm2)a | NAd | 250 | 22 | NA | |||
| No. of samplesb | 8 | 9 | 5 | ||||
| 100% × P1/(P1 + P2 + P3 + W)c | 87 | 11 | 95 | 2.9 | 88 | 2.8 | |
| 100% × P2/(P1 + P2 + P3+ W) | 5.4 | 68 | 2.7 | 68 | 5.3 | 34 | |
| 100% × P3/(P1 + P2 + P3+ W) | 4.6 | 170 | 1.9 | 83 | 1.2 | 61 | |
| 100% × W/(P1 + P2 + P3+ W) | 2.7 | 130 | 0.3 | 110 | 5.4 | 31 | |
| 100% × (P1 + P2 + P3 + W)/A | NA | 20 | 48 | NA | |||
| Carpet | No. of reference plates | 12 | 12 | 12 | |||
| Reference agar (CFU/100 cm2) | 250 | 15 | 250 | 15 | 250 | 15 | |
| No. of samples | 8 | 6 | 6 | ||||
| 100% × P1/(P1 + P2 + P3 + W) | 8.9 | 37 | 20 | 15 | 26 | 64 | |
| 100% × P2/(P1 + P2 + P3 + W) | 2.9 | 61 | 9.4 | 10 | 2.7 | 61 | |
| 100% × P3/(P1 + P2 + P3 + W) | 2.7 | 33 | 6.6 | 28 | 1.4 | 130 | |
| 100% × W/(P1 + P2 + P3 + W) | 86 | 5.7 | 64 | 4.5 | 70 | 26 | |
| 100% × (P1 + P2+ P3 + W)/A | 112 | 19 | 63 | 9.6 | 13 | 66 | |
Reference agar samples for steel-swab and steel-vacuum combinations were not available for the repeated sampling pass experiment.
Steel-wipe combination results exclude a single sample because the sample was lost. Steel-vacuum combination results exclude a single sample because the tool to move the shelves was dropped, resulting in one of the samples not being opened prior to settling.
Pi is the result from sampling pass i (where i = 1, 2, or 3); W is the result from the final wash solution; and A is the mean agar result for the run.
NA, not applicable.
DISCUSSION
LOD.
Approximately 15% of the chamber blank samples were positive for CFU for the steel runs; therefore, some of the positive results observed at the low and very low target concentrations could have been due to sample contamination rather than recovery efficiency. Contamination was not likely to have occurred during the analytic process because all laboratory controls were negative. Since chamber blanks were collected outside the open door of the chamber at the time when the coupons were being sampled, some of our positive results may be due to contamination that occurred in the experimental setting. In addition, surface sample collection could have resulted in reaerosolization of spores inside the chamber (25, 38). In our study, many precautions were taken to reduce reaerosolization and contamination: light oil was sprayed over all horizontal surfaces, gloves, and fan blades to reduce reaerosolization; chamber air was pumped out after all surfaces were covered; and grease was placed on cover seals. Since slight contamination (∼2 CFU/sample) was observed for the wipe and vacuum samples during the steel runs, even with extreme precautions, we required samples to have 3 or more CFU to be considered positive when estimating the LOD for wipe and vacuum on steel.
Our estimated LODs can most readily be compared to LODs reported by Brown et al. (6-8), who aerosolized a spore mixture while measuring volumetric concentration and flushed the mixture to a dispersion chamber to allow the spores to settle; however, there are substantial methodological differences between the two studies. Brown et al. (6-8) used spores of B. atrophaeus, had surface loadings that were much higher (i.e., 100 to 100,000 CFU/cm2 or 10,000 to 10,000,000 CFU/100 cm2), and conducted only a single run for each sampling method at each of two surface concentrations, whereas we used B. anthracis Sterne, had much lower surface loadings (i.e., 2 to 300 CFU/100 cm2), and conducted three runs at each of three surface concentrations. In addition, Brown et al. calculated LODs based on their estimated RE and the requirement that the analytical method find at least one CFU/sample, whereas we used probit regression. When sampling steel surfaces with rayon swabs, Brown et al. (7) calculated an LOD of 25 CFU per 25-cm2 sampling area (or 100 CFU/100 cm2), whereas we estimated the LOD to be two times higher (190 CFU/100 cm2) for sampling steel surfaces with foam swabs. This difference could be due to lower recovery efficiencies at lower surface loadings, the method of estimating the LOD, or the type of swab used. Similarly, when sampling steel surfaces with a polyester-rayon blend gauze wipe, Brown et al. (6) calculated an LOD of 0.1 CFU/cm2 (or 10 CFU/100 cm2) based on a 1,000-cm2 sampling area, whereas we estimated the LOD to be 50% higher (15 CFU/100 cm2 based on a 929-cm2 sampling area). It is possible that these estimates of LOD are not functionally different, given the inherent variability. Finally, when sampling steel surfaces with the vacuum filter sock method, Brown et al. (8) calculated an LOD of 0.01 to 0.02 CFU/cm2 (or 1 to 2 CFU/100 cm2) based on a 10,000-cm2 vacuum sample area, whereas we estimated the LOD to be much higher (44 CFU/100 cm2 based on a 929-cm2 sampling area).
These LOD estimates should be cautiously interpreted for several reasons. First, the data are subject to small-sample-size limitations. The low number of chamber runs coupled with high variability resulted in very wide CIs. Second, the surface concentrations included in the runs may not have been ideal for each of the sampling methods. Ideally, surface concentrations producing detection probabilities ranging from 0 to 100% would have been included. Clearly, more runs were needed, especially at the lower concentrations. Finally, reaerosolization of spores during sampling was an issue during this project, especially at the lowest levels, which necessitated an alternative analysis for estimating LODs for wipe and vacuum on steel.
RE.
The wipe sampling method had higher recoveries on both steel and carpet surfaces compared to the swab and vacuum sampling methods. The influence of the positive chamber blanks on RE is minimal because the absolute number of CFU observed on the chamber blanks was 10 times lower than the surface samples, except in one instance (vacuum on steel at low concentration). For that particular instance, we reran the statistical analysis, excluding that run, and the estimated RE changed by less than 20% (5.5% to 4.9%). Sanderson et al. (31) found that vacuum samples were more likely to be positive for CFU during the 2001 post office study but sampled much larger areas when using the vacuum method compared to the wipe method. In this study, wipe and vacuum areas were equivalent. Intuitively, wiping tends to be a better removal technique for surface contamination compared to vacuuming because it physically rubs the surface. Recovery efficiencies of the swab and vacuum sampling methods were roughly equivalent. Sampling area should be considered when choosing between the swab and vacuum methods: e.g., swabs for smaller areas and vacuum for larger areas.
RE can most readily be compared to the findings of Brown et al. (6-8). Brown et al. observed that RE decreased with surface loading, but the decrease was neither large nor statistically significant. In our study, RE did not vary by surface loading. Table 2 shows higher mean RE for wipes at the lowest surface loading, but variability was very high and the median REs were more similar. Brown et al. (6) observed a mean RE of 31% at their lowest surface loading (100 to 1,000 CFU/cm2 or 10,000 to 100,000 CFU/100 cm2) for wipe sampling on stainless steel, whereas our study observed 18% mean RE at our highest surface loading of 270 CFU/100 cm2.
Brown et al. (7) observed a mean RE of 39.5% for swab sampling on stainless steel at their lowest surface loading compared to 5.0% at our highest surface loading. Our study used foam swabs, 0.2 ml of BBT to wet the swab, and 103-cm2 test coupons, whereas Brown et al. (7) used rayon swabs, 0.05 ml of sterile water to wet the swab, and 25-cm2 test coupons. These values are lower than Brown's RE, possibly because of the much lower surface loading.
Brown et al. (8) found 32% mean RE at their lowest surface loading for vacuum sampling on stainless steel. Our study found 3.7% mean RE at our highest surface loading. Both studies used the same vacuum sock. Vacuum sampling has the benefit of being able to cover areas much larger than the area (929 cm2) used in this study. The ability to sample larger areas may offset the lower RE.
Martin and Moore (24) used spores of Bacillus globigii to contaminate surfaces by an aerosol method and by application of droplets directly onto material. REs were similar for aerosol- and droplet-applied contamination, but higher variability was observed for aerosol contamination. Hodges et al. (19) and Rose et al. (30) both used direct application of contaminants in droplets to inoculate steel surfaces to determine recovery efficiencies of B. anthracis Sterne. Rose et al. (30) sampled stainless steel coupons using macrofoam swabs and found a mean RE of 44% when vortexing and 18% when sonicating the swabs during the analysis. In this study, we used macrofoam swabs to sample steel surfaces and used both vortexing and sonication, resulting in 5.0% RE. In the study by Rose et al. (30), the surface loading was approximately 3,900 CFU/cm2 (or 390,000 CFU/100 cm2), compared to a range of 8.3 to 270 CFU/100 cm2 in this study. Hodges et al. (19) used macrofoam swabs and found REs of 31.7% to 49.1%, with the higher RE at higher inoculation levels. These directly inoculated surfaces resulted in greater REs than that found in our study. Our lower RE could have been a result of the inoculation method or surface loading being 100 times lower in this study.
Precision.
Precision (as estimated by the CV) improved at the higher levels of surface loading and was generally better for sampling on carpet compared to steel. The wipe method provided the best precision at 66% for steel and 38% for carpet surfaces at the highest surface loading. Agar precision was poor at the lowest concentration but improved with higher surface concentration. Since agar CV represents the variability within the chamber, it represents a lower limit for precision of the sampling methods. Wipe sampling on carpet achieved precision close to agar precision; however, wipe sampling on steel was less precise than agar, especially at the higher concentrations. Under the conditions tested here, wipe samples would be the preferred method for delivering more precise estimates of contaminant surface loads.
When sampling on steel surfaces, repeated sampling passes showed that a majority (≥87%) of the spores were picked up in the first pass over the surface (Table 4). When sampling on carpet, a low percentage of spores (≤26%) were found on the first pass and a majority (≥64%) were found in the wash sample collected using a stomacher to remove spores from the sample coupons after the three sampling passes. The larger amount of spores found in the carpet wash samples could be due to the carpet being thicker than the steel, causing the stomacher paddles to have more contact with the carpet or the fact that removal of B. anthracis from stainless steel is difficult (27). Since a second or third pass did not result in many more CFU and the use of a stomacher wash is not practical in most environments, one sample pass was used in subsequent sample collections and is recommended for these surface sampling methods.
This study used very low surface loadings to estimate the LOD, RE, and precision. When sampling on steel or carpet surfaces, wipe sampling was shown to detect the presence of B. anthracis Sterne at lower concentrations (i.e., lower LOD95) and to have higher RE and better precision than swab and vacuum sampling. During the anthrax attacks of 2001, reliable methods were needed in which negative and low results could be quantified and interpreted to make decisions about reentry and to estimate risk. These results provide valuable information regarding the efficiency, level of detection, and precision of standard sampling methods for aerosolized B. anthracis Sterne spores. However, ventilation characteristics of the room, quantification of aerosolization from surfaces, and uptake by individuals would also be needed to quantify exposures to individuals based on these results. The RE or LOD95 values should not be used as definitive results. When using these data to perform risk assessments or for other reasons, precision and CIs should be taken into account. Although this study attempted to create conditions that were realistic and reproducible, it was conducted in a chamber with little interference from debris (dirt, fibers, and other particles) that might be found under field conditions. Field conditions are difficult to model in the laboratory, but debris will likely change the RE of these methods. The results do not account for variability of using multiple technicians to collect samples. These data may not be precisely representative of samples generated as the result of terrorist or occupational incidents with respect to the surface being sampled, the nonspore matrix, and many other significant factors.
These data document the overall performance characteristics and inherent variability of these methods. Conducting trials at very low surface concentration adds to the understanding and interpretation of these sampling method results when contamination is low or nonexistent. The LOD results will assist in determining the confidence that there is not contamination in a location, room, or building. These results can be used with models (32) that determine sampling strategies for quantifying B. anthracis contamination in a location, allowing decisions to be made on reentry.
Acknowledgments
We thank Teresa Schnorr, Wayne Sanderson, Max Kiefer, Matthew Gillen, Bruce Harper, Angelo Madonna, Greg Dahlstrom, Rich Haugland, Ken Martinez, Stanley A. Shulman, Jeff Neal, and Daryll Ward for assistance with this project.
The findings and conclusions in this presentation have not been formally disseminated by the National Institute for Occupational Safety and Health and should not be construed to represent any agency determination or policy.
Footnotes
Published ahead of print on 8 May 2009.
REFERENCES
- 1.AOAC International. 1999. Qualitative and Quantitative microbiology guidelines for methods validation. J. AOAC Int. 82:402-415. [Google Scholar]
- 2.Barchia, I. M., G. A. Herron, and A. R. Gilmour. 2003. Use of a generalized linear mixed model to reduce excessive heterogeneity in petroleum spray oil bioassay data. J. Econ. Entomol. 96:983-989. [DOI] [PubMed] [Google Scholar]
- 3.Baron, P. A., C. F. Estill, J. K. Beard, M. J. Hein, and L. Larsen. 2007. Bacterial endospore inactivation caused by outgassing of vapourous hydrogen peroxide from polymethyl methacrylate (Plexiglas). Lett. Appl. Microbiol. 45:485-490. [DOI] [PubMed] [Google Scholar]
- 4.Baron, P. A., C. F. Estill, G. J. Deye, M. J. Hein, J. K. Beard, L. D. Larsen, and G. E. Dahlstrom. 2008. Development of an aerosol system for uniformly depositing Bacillus anthracis spore particles on surfaces. Aerosol Sci. Technol. 42:159-172. [Google Scholar]
- 5.Bartrand, T. A., M. H. Weir, and C. N. Haas. 2008. Dose-response models for inhalation of Bacillus anthracis spores: interspecies comparisons. Risk Anal. 28:1115-1124. [DOI] [PubMed] [Google Scholar]
- 6.Brown, G. S., R. G. Betty, J. E. Brockmann, D. A. Lucero, C. A. Souza, K. S. Walsh, R. M. Boucher, M. Tezak, M. C. Wilson, and T. Rudolph. 2007. Evaluation of a wipe surface sample method for collection of Bacillus spores from nonporous surfaces Appl. Environ. Microbiol. 73:706-710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown, G. S., R. G. Betty, J. E. Brockmann, D. A. Lucero, C. A. Souza, K. S. Walsh, R. M. Boucher, M. S. Tezak, M. C. Wilson, T. Rudolph, H. D. A. Lindquist, and K. F. Martinez. 2007. Evaluation of rayon swab surface sample collection method for Bacillus spores from non-porous surfaces. J. Appl. Microbiol. 103:1074-1080. [DOI] [PubMed] [Google Scholar]
- 8.Brown, G. S., R. G. Betty, J. E. Brockmann, D. A. Lucero, C. A. Souza, K. S. Walsh, R. M. Boucher, M. S. Tezak, and M. C. Wilson. 2007. Evaluation of vacuum sock surface sample collection method for Bacillus spores from porous and non-porous surfaces. J. Environ. Monit. 9:666-671. [DOI] [PubMed] [Google Scholar]
- 9.Carus, W. S. 2001. German Secret Service, 1915-1917, p. 69-70. In Bioterrorism and biocrimes: the illicit use of biological agents since 1900. Center for Counterproliferation Research, National Defense University, Washington, DC.
- 10.Caudle, L. C., III. 1997. The biological warfare threat, p. 451-466. In F. R. Sidell, E. T. Takafuji, and D. R. Franz (ed.), Medical aspects of chemical and biological warfare. Office of the Surgeon General, Borden Institute, Walter Reed Army Medical Center, Washington, DC. http://www.bordeninstitute.army.mil/published_volumes/chemBio/Ch21.pdf.
- 11.Centers for Disease Control and Prevention. 2001. Investigation of bioterrorism-related anthrax—Connecticut, 2001. MMWR Morb. Mortal. Wkly. Rep. 50:1077-1079. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. 2002. Comprehensive procedures for collecting environmental samples for culturing Bacillus anthracis. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Atlanta, GA. http://www.bt.cdc.gov/agent/anthrax/environmental-sampling-apr2002.asp.
- 13.Centers for Disease Control and Prevention. 2006. Inhalation anthrax associated with dried animal hides—Pennsylvania and New York City, 2006. MMWR Morb. Mortal. Wkly. Rep. 55:280-282. [PubMed] [Google Scholar]
- 14.Cohen, M. L., and T. Whalen. 2007. Implications of low level human exposure to respirable B. anthracis. Appl. Biosafety 12:109-115. [Google Scholar]
- 15.Fennelly, K. P., A. L. Davidow, S. L. Miller, N. Connell, and J. J. Ellner. 2004. Airborne infection with Bacillus anthracis—from mills to mail. Emerg. Infect. Dis. 10:996-1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finney, D. J. 1971. Probit analysis, 3rd ed. Cambridge University Press, London, United Kingdom.
- 17.Government Accountability Office. 2005. Anthrax detection. Agencies need to validate sampling activities in order to increase confidence in negative results, p. 114. In Report to the Chairman, Subcommittee on National Security, Emerging Threats, and International Relations, House Committee on Government Reform, House of Representatives. GAO-05-251. Government Accountability Office, Washington, DC. http://www.gao.gov/new.items/d05251.pdf.
- 18.Hinds, W. C. 1999. Aerosol technology. J. Wiley and Sons, New York, NY.
- 19.Hodges, L. R., L. J. Rose, A. Peterson, J. Noble-Wang, and M. J. Arduino. 2006. Evaluation of a macrofoam swab protocol for the recovery of Bacillus anthracis spores from a steel surface. Appl. Environ. Microbiol. 72:4429-4430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jernigan, D. B., P. L. Raghunathan, B. P. Bell, R. Brechner, E. A. Bresnitz, J. C. Butler, M. Cetron, M. Cohen, T. Doyle, M. Fischer, C. Greene, K. S. Griffith, J. Guarner, J. L. Hadler, J. A. Hayslett, R. Meyer, L. R. Petersen, M. Phillips, R. Pinner, T. Popovic, C. P. Quinn, J. Reefhuis, D. Reissman, N. Rosenstein, A. Schuchat, W. Sheih, L. Siegal, D. L. Swerdlow, F. C. Tenover, M. Traeger, J. W. Ward, I. Weisfuse, S. Wiersma, K. Yeskey, S. Zaki, D. A. Ashford, B. A. Perkins, S. Ostroff, J. Hughes, D. Fleming, J. P. Koplan, J. L. Gerberding, and the National Anthrax Epidemiologic Investigation Team. 2002. Investigation of bioterrorism-related anthrax, United States, 2001: epidemiologic findings. Emerg. Infect. Dis. 8:1019-1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jernigan, J. A., D. S. Stephens, D. A. Ashford, C. Omenaca, M. S. Topeil, M. Galbraigh, M. Tapper, T. L. Fisk, S. Saki, T. Popovic, R. F. Meyer, C. P. Quinn, S. A. Harper, S. K. Fridkin, J. J. Sejvar, C. W. Shepard, M. McConnell, J. Guarner, W. Sheih, J. M. Malecki, J. L. Gerberding, J. M. Hughes, B. A. Perkins, and members of the Anthrax Bioterrorism Investigation Team. 2001. Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Emerg. Infect. Dis. 7:933-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keim, P., K. L. Smith, C. Keys, H. Takahashi, T. Kurata, and A. Kaufmann. 2001. Molecular investigation of the Aum Shinrikyo anthrax release in Kameido, Japan. J. Clin. Microbiol. 39:4566-4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kennedy, E. R., T. J. Fischbach, R. Song, P. M. Eller, and S. A. Shulman. 1995. Guidelines for air sampling and analytical method development and evaluation. NIOSH 95-117. National Institute of Occupational Safety and Health, Washington, DC.
- 24.Martin, D. D., and L. M. Moore. 2001. Technical report for the comparison of swab-sampling techniques for recovery of bacterial spores from three surfaces. West Desert Test Center document no. WDTC-TR-00-018, June 2001. U.S. Army Dugway Proving Ground, Dugway, UT.
- 25.McCleery, R. E., K. F. Martinez, G. A. Burr, and D. A. Mattorano. 2004. Health Hazard Evaluation Report 2002-0109-2927. Trenton Processing and Distribution Center, Trenton, NJ. Department of Health and Human Services, Washington, DC.
- 26.Meselson, M., J. Guillemin, M. Hugh-Jones, A. Langmuir, I. Popova, A. Shelokov, and O. Yampolskaya. 1994. The Sverdlovsk anthrax outbreak of 1979. Science 266:1202-1208. [DOI] [PubMed] [Google Scholar]
- 27.Noyce, J. O., H. Michels, and C. W. Keevil. 2006. Use of copper cast alloys to control Escherichia coli O157 cross-contamination during food processing. Appl. Environ. Microbiol. 72:4239-4244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Olson, K. B. 1999. Aum Shinrikyo: once and future threat? Emerg. Infect. Dis. 5:513-516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parker, J. S. 2001. Terrorism through the mail: protecting the postal workers and the public. Report submitted to the Committee on Governmental Affairs and the Subcommittee on International Security, Proliferation and Federal Service, October 31, 2001. http://hsgac.senate.gov/103101parker.htm.
- 30.Rose, L., B. Jensen, A. Peterson, S. N. Banerjee, and M. J. Arduino. 2004. Swab materials and Bacillus anthracis spore recovery from nonporous surfaces. Emerg. Infect. Dis. 10:1023-1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sanderson, W. T., R. R. Stoddard, A. S. Echt, C. A. Piacitelli, D. Kim, J. Horan, M. M. Davies, R. E. McCleery, P. Muller, T. M. Schnorr, E. M. Ward, and T. R. Hales. 2004. Bacillus anthracis contamination and inhalational anthrax in a mail processing and distribution center. J. Appl. Microbiol. 96:1048-1056. [DOI] [PubMed] [Google Scholar]
- 32.Sego, L. H., K. K. Anderson, B. D. Matzke, W. K. Sieber, S. A. Shulman, J. Bennett, M. Gillen, J. E. Wilson, and B. A. Pulsipher. 2007. An environmental sampling model for combining judgment and randomly placed samples. PNNL-16636. Pacific Northwest National Laboratory, Richland, WA.
- 33.Shafazand, S., R. Doyle, S. Ruoss, A. Weinacker, and T. A. Raffin. 1999. Inhalation anthrax epidemiology, diagnosis and management. Chest 116:1369-1376. [DOI] [PubMed] [Google Scholar]
- 34.Shieh, W., J. Guraner, C. Paddock, P. Greer, K. Tatti, M. Fischer, M. Layton, M. Philips, E. Bresnitz, C. P. Quinn, T. Popovic, B. A. Perkins, S. R. Zaki, and the Anthrax Bioterrorism Investigation Team. 2003. The critical role of pathology in the investigation of bioterrorism-related cutaneous anthrax. Am. J. Pathol. 163:1901-1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smieja, M., J. B. Mahony, C. H. Goldsmith, S. Chong, A. Petrich, and M. Chernesky. 2001. Replicate PCR testing and probit analysis for detection and quantitation of Chlamydia pneumoniae in clinical specimens. J. Clin. Microbiol. 39:1796-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Turner, J. R., and S. V. Hering. 1987. Greased and oiled substrates as bounce-free impaction surfaces. J. Aerosol Sci. 18:215-224. [Google Scholar]
- 37.U.S. Environmental Protection Agency. 2002. Federal on-scene coordinator's report for the Capitol Hill site, Washington, D.C. GS-10F-0076K. U.S. EPA Region 3, Philadelphia, PA.
- 38.Weis, C. P., A. J. Intrepido, A. K. Miller, P. G. Cowin, M. A. Durno, J. S. Gebhardt, and R. Bull. 2002. Secondary aerosolization of viable Bacillus anthracis spores in a contaminated U.S. Senate office. JAMA 288:2853-2858. [DOI] [PubMed] [Google Scholar]