Abstract
Objective
This study was undertaken to document current practice patterns for the surgical treatment of endometrial cancer in Korea.
Methods
Questionnaires were distributed to 131 Korean gynecologic oncologists, all members of the Korean Gynecologic Oncology Group. Questions addressed extent of hysterectomy procedure, pelvic (PEN) or paraaortic (PAN) lymph node dissection, ovarian preservation, and omentectomy.
Results
Completed questionnaires were returned by 64.1% (84/131) of the oncologists at 50 institutes. Extrafascial hysterectomy (EH) was used by 32% of respondents and modified radical hysterectomy (MRH) or radical hysterectomy (RH) by 17%. Hysterectomy procedures were selectively employed based on tumor-related factors by 51% of the respondents. Laparoscopic hysterectomy was routinely utilized by 49% and was more commonly used by younger surgeons with 10 years of experience or less. PEN dissection was routinely utilized by 67% and was used selectively based on tumor-related factors by 33%. PAN dissection/biopsy was used either routinely (43%) or selectively based on tumor-related factors (43%). PAN dissection/biopsy had never been employed by 12% of the respondents. Sixty-nine percent of respondents stated that grossly normal looking ovaries can be preserved during surgery in young aged patients with early stage disease, and 29% stated that bilateral oophorectomy should be performed irrespective of age or stage. Omentectomy was routinely performed by 11% of respondents, and was selectively performed when extrauterine spread was present by 41%.
Conclusion
Surgical procedures for the treatment of endometrial cancer are still not standardized among Korean gynecologic surgeons. Clinical trials to determine the benefits of the different surgical procedures should be developed.
Keywords: Practice pattern, Endometrial cancer
INTRODUCTION
The surgical treatment of endometrial cancer has two major purposes, i.e., to completely remove the tumor burden and to obtain histopathologic information to determine stage and decide on future treatment strategies. According to the National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines, when disease is confined to the uterus, total hysterectomy, bilateral salpingo-oophorectomy, and pelvic/paraaortic lymph node dissection should be considered; omentectomy is also recommended in patients with suspected extra-uterine disease. Furthermore, in patients with suspected cervical stromal involvement, radical hysterectomy (RH) is recommended.1 However, the procedures and extent of surgery used in patients with endometrial cancer vary considerably. In terms of lymphadenectomy, extensive paraaortic lymph node dissection is recommended by some investigators, but concern about post-operative morbidity and/or lack of surgical skill may steer the inexperienced surgeon away from extensive surgery. On the other hand, no reliable diagnostic tool is available to predict the status of cervical stromal invasion, and thus, some surgeons tend to perform routine extensive type II or III hysterectomies.
Thus, the different surgical treatments utilized by surgeons are likely to influence the results of multicenter clinical trials on endometrial cancer patients, and may reduce the qualities of such studies. For this reason, the Korean Gynecologic Oncology Group surveyed its members to determine actual practice patterns for the surgical treatment of endometrial cancer.
MATERIALS AND METHODS
A survey regarding actual surgical procedures undertaken for endometrial cancer was distributed to 131 members of the Korean Gynecologic Oncology Group. The questionnaire addressed the following; mean number of patients treated per year, surgical experience, the extent of standard hysterectomy procedures, use of laparoscopic surgery, criteria for pelvic/paraaortic lymph node dissection or biopsy, and whether ovarian preservation or omentectomy was performed. Pelvic lymph node dissection (PEN) was defined as bilateral removal of all nodal tissue and the skeletonization of all vessels from the mid portion of the common iliac artery to the circumflex iliac vein, and laterally, from the mid portion of the psoas muscle to the ureter medially, including the hypogastric artery and vein and from the obturator fossa anterior to the obturator nerve. Paraaortic lymph node dissection (PAN) was defined as the removal of nodal tissue over the distal vena cava from the level of the inferior mesenteric artery to the mid right common iliac artery and/or up to the renal artery. If the number of removed lymph nodes exceeded 4, we defined the procedure as 'dissection', and if below 4 as biopsy or sampling. All replies were returned by FAX or mail, and all respondents replied in name.
RESULTS
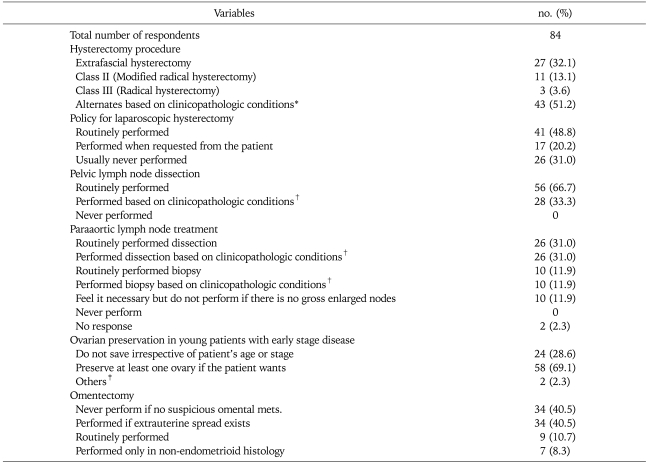
A total of 84 surveys were returned from 50 different institutes. Table 1 summarizes the routinely performed hysterectomy procedure, and indications for Class II/III hysterectomy, PEN, PAN, ovarian preservation, and omentectomy.
Table 1.
Surgical procedures for endometrial cancer
*Suspicious of cervical invasion by MRI or endocervical curettage, non-endometrioid histology, deep myometrial invasion, †Evidence of paraaortic node swelling, evidence of pelvic node invasion, non-endometrioid type, evidence of cervical involvement, deep myometrial invasion, Grade 2 or 3, ‡Consider preservation after confirming tumor free by frozen biopsy
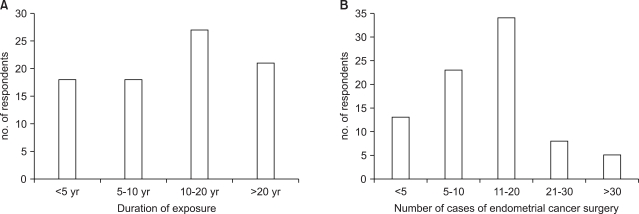
1. Surgical expertness of respondents
All respondents were gynecologic oncologists attached to a university hospital or a specialized cancer hospital. The number of operations per respondent for endometrial cancer was usually in the range 11 to 20 per annum (40%), and the mean period of exposure to endometrial cancer surgery was 10 to 20 years (32%) (Fig. 1).
Fig. 1.
Experiences of respondents; (A) Duration of exposure to endometrial cancer surgery, (B) Number of cases of endometrial cancer surgery treated per respondent.
2. The extent of standard hysterectomy procedures
Twenty-seven (32%) respondents performed only extrafascial hysterectomy (EH), 11 (13%) performed modified radical hysterectomy (MRH)2 as a routine procedure for the treatment of endometrial cancer patients. Three respondents (4%) routinely performed RH, and 43 (51%) performed different procedures based on specific tumor related clinicopathologic conditions. Indications for performing RH were suspected cervical stromal involvement by MRI or endocervical curettage, deep myometrial invasion (21/77, 27%), or a non-endometrioid histology (18/77, 23%).
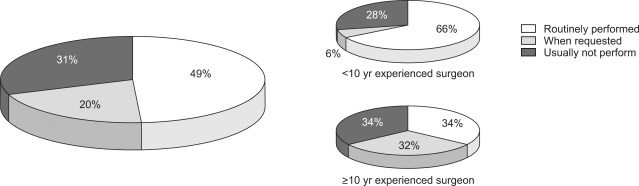
3. Use of laparoscopic surgery
Forty-one respondents (49%) preferred laparoscopic surgery as a routine procedure in patients with a tumor confined to the uterus, 17 (20%) considered laparoscopic surgery when required by patients, and 26 (31%) had never used laparoscopic surgery. After subdividing respondents according to surgical experience, surgeons with more than 10 years of experience of endometrial cancer surgery (when laparoscopic surgery was not popular) were found to use laparoscopic surgery routinely in only 34% of operations. On the other hand, surgeons with less than 10 years of experience used laparoscopic surgery routinely in 68% of operations (Fig. 2).
Fig. 2.
Use of laparoscopic hysterectomy for the treatment of endometrial cancer.
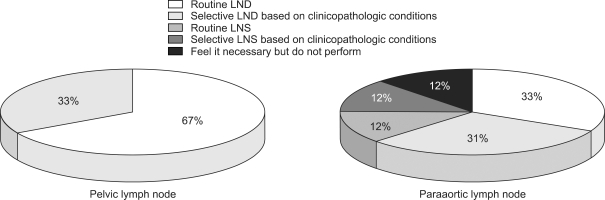
4. Pelvic lymph node dissection
The majority of respondents were in favor of performing PEN, and 67% stated that they always perform PEN without exception, irrespective of stage or tumor grade.
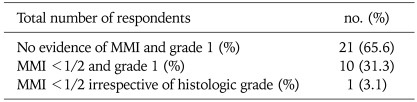
On the other hand, 33% stated that they do not perform PEN in selected patients with low risk of lymph node metastasis. Among responders who stated they can omit PEN, 66% thought that pelvic lymphadenectomy can be omitted in clinical stage Ia only, 31% thought that pelvic lymphadenectomy can be omitted in patients with well differentiated tumors invading less than half of the myometrium by preoperative MRI evaluation, and a small minority (3%) considered that pelvic lymphadenectomy can be omitted in patients with tumors invading less than half of the myometrium, irrespective of differentiation (Table 2).
Table 2.
Clinicopathologic conditions not requiring pelvic lymph node dissection (N=32)
MMI: myometrial invasion
5. Paraaortic lymph node dissection
Of the 84 respondents, 72 (86%) performed PAN dissection or biopsy; 26 (31%) routinely performed PAN dissection irrespective of tumor stage, 26 (31%) selectively performed PAN dissection in patients with poor prognostic risk factors, 10 (12%) routinely performed PAN biopsy irrespective of tumor stage, and 10 (12%) selectively performed PAN biopsy based on tumor related factors.
Ten respondents (12%) replied, although they felt that PAN dissection is necessary, that they never undertook a procedure to determine paraaortic node status if they do not find any palpable enlarged nodes intraoperatively (Fig. 3). The criteria used to indicate PAN dissection by 35 respondents who said they performed PAN dissection or biopsy in selective cases were; preoperatively suspected or intraoperatively palpable PAN, a positive common iliac node by frozen section biopsy, a non-endometrioid histology, suspected cervical stromal invasion, >1/2 myometrial invasion, and a histologic grade 3 tumor (the frequencies of using these criteria were in the named order).
Fig. 3.
Lymph node dissection policies during endometrial cancer surgery.
LND: lymph node dissection, LNS: lymph node sampling
6. Preservation of ovaries in young patients
We asked the respondents the following question, after describing the following scenario. A 30-year-old woman with one daughter, who had not decided to curtail childbearing, is diagnosed as having a well differentiated endometrioid type adenocarcinoma by endometrial curettage, and myometrial invasion not exceeding half the thickness of the muscular wall by MRI.
Q: Would you preserve her ovaries during hysterectomy?
Thirty-five (42%) respondents said they would perform bilateral oophorectomy, 40 (48%) responded that they would preserve one or both ovaries, and the remaining 9 (11%) said that they would consider ovarian preservation when strongly requested to do so, but only after cautioning the patient about the possibility of occult metastasis.
To a question concerning current policy regarding ovarian preservation in young endometrial cancer patients, 29% of respondents said that they would always perform bilateral salpingooophoretomy irrespective of clinical stage or patient age, whereas 69% responded that they would save one or both ovaries if the patient concerned strongly requested that the ovaries be saved and there was no gross intraoperative evidence of disease spread to the adnexa. The remaining respondents replied that they would decide on ovary preservation after verifying frozen section results after bilateral ovarian wedge resection. In summary, patients' wishes to save their ovaries mainly influenced decisions concerning preservation.
7. Omentectomy
When asked whether physicians perform omentectomy or not during surgery, 11% responded they always perform omentectomy regardless of stage, 41% responded that they do not perform omentectomy if there is no evidence of omental metastasis, and 41% responded that they perform omentectomy if extrauterine tumor spread is detected even with a grossly tumor-free omentum. The remaining 7% said they perform omentectomy when the histologic subtype is non-endometrioid.
DISCUSSION
Surgery has been the treatment of choice for endometrial cancer since the FIGO surgical staging system was adopted in 1988. However, the treatment guidelines issued by the NCCN were essentially based on clinical stage, and thus, although these guidelines have been adopted as a standard for some time, surgical procedures have not been standardized among Korean gynecologic oncologists.1 This variety of standard surgical procedures for endometrial cancer is not unique to Korea. In Japan, Watanabe et al. investigated the status of endometrial carcinoma surgical procedures by surveying members of the Japan Gynecologic Oncology Group (JGOG). Based on 139 responses, total abdominal hysterectomy (TAH) was found to be employed routinely by 30% of respondents and Piver class II by 30%. The remaining 1/3 selected TAH, Class II hysterectomy, or RH based on tumor related factors. Furthermore, RH was not used in 70% of institutions, and was performed in the remaining 30% based on tumor related factors. Also, it was found out that the range of conducting hysterectomy differed by the characteristics of the operating institutions. In cancer specialty hospitals, the rate of conducting simple hysterectomy based on the principles of endometrial cancer treatment was high and the rate of radical hysterectomy was relatively lower compared that of university hospitals and other general hospital.3 Also, the results of a similar survey in the North American region showed that only 54.2% of the institutions always practiced pelvic lymphadenectomy when practicing endometrial cancer surgery, while approximately 30% of them did not practice class II or III type hysterectomy even in the presence of any risk factor.4 When comparing the results of this study to such data with regard to hysterectomy, the operating frequency of class II hysterectomy seems to be higher compared to the Western results while being somewhat similar with the results of neighboring Japan; but the rate of changing operation scope depending on clinical conditions such as risk factors of cervical invasion is higher among Korean surgeons.
The current NCCN Clinical Practice Guideline recommends practicing radical hysterectomy only when cervical infiltration is suspected on MRI or when confirmed by cervical biopsy. However, as can be seen in the survey results from Korea and Japan, many clinicians practice hysterectomy more extensively even when cervical involvement is not suspected prior to surgery. This is probably due to the fact that cervical infiltration cannot be totally ruled out by pre-operation evaluations since present imaging diagnosis, including MRI, does not attain enough sensitivity to predict whether cervical involvement has occurred before surgery, as stated by the above guidelines. In fact, the author and colleagues (unpublished data) conducted a retrospective analysis on 85 cases of endometrial cancer, which were histologically identified to feature infiltration, over the last 10 years and showed that a MRI sensitivity of 44.7%, and this figure was 53.3% when limited to stromal invasion, suggesting that about half of cervix infiltrations are incidentally detected by post-operation histological exam. Therefore, inaccuracy of such pre-operation prediction, as seen in the results of this investigation, might represent one of the major reasons why clinicians commonly practice extensive hysterectomy.
Practicing pelvic lymphadenectomy in endometrial cancer treatment is an area in which a consensus is established among clinicians in general; nevertheless, about 1/3 of the responders omitted lymphadenectomy in patients that presumably feature a very small possibility of lymph node metastasis. As of yet, no results from a large-case randomized study addressing the efficacy of paraaortic lymphadenectomy in endometrial cancer is available, and small-scale studies on this issue provide inconsistent results regarding improved survival rate of patients,5-8 and the largest difference in opinions was shown among the responders regarding this issue. In addition, a large number of responders recognized the need for paraaortic lymphadenectomy but did not actually practice it due to lack of surgical skills. Looking into the survey results in other countries regarding lymphadenectomy, physicians in Japan generally practices pelvic lymphadenectomy in 97.8% of cases regardless of clinical prognostic factors, which was in drastic contrast with that of Korea.3 Meanwhile, the investigation by an Italian group in 2001 of 276 respondents showed that paraaortic lymphadenectomy was not practiced at all, and only about 31% practiced pelvic lymphadenectomy.9
In the operative treatment principle of endometrial cancer, bilateral adnexectomy along with hysterectomy is stated as a standard procedure. Unlike cervical cancer whose prognosis is not affected by oophorectomy, or ovarian cancer which, in the early stages, allows retention of the opposite ovary to retain fertility, the principle of bilateral adnexectomy in endometrial cancer is being applied without regard to age or prognostic factors. However, quite a large number of clinicians were found to actually practice ovary preservation in early stage endometrial cancer and this issue was included in this survey in order to figure out the status quo. In a survey in which an example was provided regarding a case of a 30 years old woman with clinical stage Ib, the ratio of respondents who chose to excise both ovaries according to the principle with no regard to the age and stage, and that of those who responded to retain one or more ovaries turned out to be similar. The author and colleagues recently reported that the possibility of micro metastatic cancer in an ovary which appeared macroscopically normal was less than 1% in patients whose extrauterine metastasis was not confirmed during surgery, which based on retrospective analysis of 260 endometrial patients, and it was also reported that there were zero cases of recurrence after 76-months' follow-up of 35 cases of early endometrial cancer patients with ovary retention.10
The significance of this survey is that it demonstrated the presence of a certain discrepancy between the clinical guidelines for certain diseases that we have been accepting as basic treatment, and the actual practice adopted by clinicians, an example of which is endometrial cancer in the field of gynecologic cancer. Quite a large proportion of former treatment principles have not changed for a long time despite the publication of a large number of studies due to the difficulty to secure the basics through a large-scale phase III study that affect the current treatment guideline. As a result, the actual practice, in many occasions, is performed as a modified form from the existing principle depending on the judgment of each physician, based on the results of small-scale studies, and surgical treatment of endometrial cancer is a representative case in which a large diversity is observed, even among gynecologic oncologists in actual practice.
This investigation was conducted without full verification of the reliability and validity of its survey items and the respondents represented a partial sample of the population of the entire gynecologic oncologists, and therefore, this study is limited in reflecting the actual practice. Nevertheless, this study has significance as a reference material for recognizing the fact that some difference exists in the practice by physicians with regard to surgical treatment of endometrial cancer, and that it is required to minimize such difference in order to conduct multicenter clinical studies more efficiently in the future.
Footnotes
This study was supported by a grant of the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (0412-CR01-0704-0001).
References
- 1.National Comprehensive Cancer Network. Fort Washington: National Comprehensive Cancer Network; c2009. [cited 2009 April 22]. NCCN Clinical Practice Guidelines in Oncology [Internet] Available from: http://www.nccn.org. [Google Scholar]
- 2.Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstet Gynecol. 1974;44:265–272. [PubMed] [Google Scholar]
- 3.Watanabe Y, Aoki D, Kitagawa R, Takeuchi S, Sagae S, Sakuragi N, et al. Status of surgical treatment procedures for endometrial cancer in Japan: results of a Japanese Gynecologic Oncology Group survey. Gynecol Oncol. 2007;105:325–328. doi: 10.1016/j.ygyno.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 4.Maggino T, Romagnolo C, Landoni F, Sartori E, Zola P, Gadducci A. An analysis of approaches to the management of endometrial cancer in North America: a CTF study. Gynecol Oncol. 1998;68:274–279. doi: 10.1006/gyno.1998.4951. [DOI] [PubMed] [Google Scholar]
- 5.Yaegashi N, Ito K, Niikura H. Lymphadenectomy for endometrial cancer: is paraaortic lymphadenectomy necessary? Int J Clin Oncol. 2007;12:176–180. doi: 10.1007/s10147-006-0621-2. [DOI] [PubMed] [Google Scholar]
- 6.Mariani A, Keeney GL, Aletti G, Webb MJ, Haddock MG, Podratz KC. Endometrial carcinoma: paraaortic dissemination. Gynecol Oncol. 2004;92:833–838. doi: 10.1016/j.ygyno.2003.11.032. [DOI] [PubMed] [Google Scholar]
- 7.Ozsoy M, Dilek S, Ozsoy D. Pelvic and paraaortic lymph node metastasis in clinical stage I endometrial adenocarcinoma: an analysis of 58 consecutive cases. Eur J Gynaecol Oncol. 2003;24:398–400. [PubMed] [Google Scholar]
- 8.Yenen MC, Dilek S, Dede M, Goktolga U, Deveci MS, Aydogu T. Pelvic-paraaortic lymphadenectomy in clinical Stage I endometrial adenocarcinoma: a multicenter study. Eur J Gynaecol Oncol. 2003;24:327–329. [PubMed] [Google Scholar]
- 9.Amadori A, Bucchi L, Gori G, Falcini F, Saragoni L, Amadori D. Frequency and determinants of lymphadenectomy in endometrial carcinoma: a population-based study from northern Italy. Ann Surg Oncol. 2001;8:723–728. doi: 10.1007/s10434-001-0723-z. [DOI] [PubMed] [Google Scholar]
- 10.Lee TS, Jung JY, Kim JW, Park NH, Song YS, Kang SB, et al. Feasibility of ovarian preservation in patients with early stage endometrial carcinoma. Gynecol Oncol. 2007;104:52–57. doi: 10.1016/j.ygyno.2006.07.003. [DOI] [PubMed] [Google Scholar]