Abstract
The prevalence and clinical correlates of substance use disorders (SUDs) were examined in a clinical sample of Obsessive Compulsive Disorder (OCD). As part of their intake interview into an observational study of the course of OCD, 323 participants completed a battery of standardized measures. Twenty-seven percent of the sample met lifetime criteria for a SUD. 70% of participants with comorbid SUDs reported that OCD preceded SUD onset by at least one year. Younger age at OCD onset and presence of Borderline Personality Disorder (BPD) were each associated with increased risk of alcohol use disorders but only BPD was associated with increased risk of drug use disorders. SUDs affect more than one-quarter of individuals who seek treatment for OCD. Individuals with a juvenile-onset of OCD or comorbid BPD may be especially vulnerable to SUDs. Further research is needed to identify risk factors for SUDs and to better understand their impact on OCD course.
Keywords: Obsessive Compulsive Disorder, Substance Use Disorders, comorbidity
Obsessive-compulsive disorder (OCD) is an often disabling anxiety disorder characterized by intrusive thoughts and/or repetitive behaviors. Despite reports of high comorbidity rates of anxiety disorders with substance use disorders (SUDs), surprisingly little is known about OCD and SUD comorbidity (Kessler et al., 2005; Kushner, Abrams, & Borchardt, 2000; Merikangas et al., 1998; Regier et al., 1990). To our knowledge, only a few studies have reported OCD-SUD comorbidity rates in individuals receiving treatment for SUD (Eisen & Rasmussen, 1989; Fals-Stewart & Angarano, 1994; Riemann, McNally, & Cox, 1992) or individuals receiving treatment for OCD (Denys, Tenney, van Megen, de Geus, & Westenberg, 2004; Diniz et al., 2004; Rasmussen & Eisen, 1998; Yaryura-Tobias et al., 2000). However, no studies have examined the clinical correlates of SUDs in a representative, clinical sample of OCD. Identifying characteristics of individuals with comorbid OCD-SUD will enhance our understanding of the relationship of these two disorders and may lead to improving available treatment interventions.
Comorbidity rates of OCD and SUDs vary depending on the sampling method. Elevated comorbidity rates have been reported in the general population as well as in substance use treatment samples. Data derived from the Epidemiological Catchment Area (ECA) estimate that 24% of individuals with OCD meet lifetime criteria for an alcohol use disorder, 18% meet lifetime criteria for a drug use disorder (Karno, Golding, Sorenson, & Burnam, 1988) and individuals with OCD are at increased risk for substance use dependence (Regier et al., 1990). OCD prevalence rates among individuals receiving treatment for a substance use disorder range from 6% to 12% (Eisen & Rasmussen, 1989; Riemann et al., 1992), two to six times higher than those found in the general population. However, lifetime SUD rates in individuals treated at OCD specialty clinics, range from 10% to 16% (Diniz et al., 2004; Rasmussen & Eisen, 1998; Yaryura-Tobias et al., 2000), which are slightly lower or comparable to SUD prevalence in the general population (Kessler et al., 2005; Robins et al., 1984). One possible explanation for the discrepant rates may be that individuals with SUDs are more likely to be referred to specialized substance use programs rather than anxiety specialty clinics.
Etiological models of comorbidity have focused on causal explanations (i.e. having one disorder increases risk for the other disorder) or explanations based on a “shared etiology” (individuals with both disorders share a common risk factor). In a review of studies examining alcohol use disorders and anxiety disorders, Kushner and colleagues (Kushner et al., 2000) concluded that anxiety disorders and alcohol use disorders appear to influence each other. That is, having either an anxiety disorder or an SUD may increase vulnerability of developing the other disorder, as well as contribute to the persistence of anxiety and/or SUD symptoms. Understanding comorbidity appears especially relevant to OCD, as there is evidence that taking certain substances (e.g. cocaine or methamphetamine) may exacerbate OCD symptoms, while others (e.g. opiates) may potentially alleviate OCD symptoms (Koizumi, 1985; Koran et al., 2005; Satel & McDougle, 1991).
The primary aim of this study was to identify demographic and clinical correlates of SUDs in individuals with a primary DSM-IV diagnosis of OCD. Unlike previous studies that have recruited from a single site (either an OCD specialty clinic or a SUD treatment setting), participants were systematically recruited from multiple treatment sites including an OCD specialty clinic, two general psychiatric outpatient groups, and an inpatient psychiatric hospital with both mental health and substance use specialty programs. Based on findings from previous reports that comorbid SUDs are associated with greater levels of psychopathology (Cassidy, Ahearn, & Carroll, 2001; Diniz et al., 2004; Drake, Bartels, Teague, Noordsy, & Clark, 1993; Hasin et al., 1996; Keel et al., 2003; Mueser et al., 1990; Tohen et al., 1992), we hypothesized that individuals with OCD+SUD would also report more severe OCD symptoms, increased rates of comorbidity and poorer psychosocial functioning. Based on clinical experience, we also hypothesized that individuals with OCD+SUD would be more likely to report that onset of OCD symptoms preceded the onset of an SUD. A secondary aim was to explore potential risk factors for developing an SUD among individuals with OCD.
Methods
Participants
Participants were 323 adults (over the age of 18), enrolled in the Brown Longitudinal OCD Study (BLOCS), an observational follow-up study of the course of OCD. Data reported in this paper were collected from consecutive adult participants who completed intake interviews between June 2001 and December 2005. Study inclusion criteria were: primary DSM-IV diagnosis of OCD (i.e., OCD was the disorder that the participant identified as causing the most problems lifetime), at least 6 years of age, and treatment-seeking for OCD within the past five years. The only exclusion criterion was the presence of an organic mental disorder. A more detailed description of the sample characteristics, subject recruitment and study procedures is available elsewhere (Pinto, Mancebo, Eisen, Pagano, & Rasmussen, 2006).
The majority of the sample (95%) was Caucasian and 55% was female. Fewer than half (44%) were married and the average age of adult participants was 40.1 years (SD = 12.8, range = 19-75). Fifty-eight percent of participants were currently employed and 45% had achieved a bachelor's degree or higher. Demographic and clinical characteristics of this sample are consistent with those of samples in previous studies of OCD phenomenology, including the DSM-IV field trial (Eisen et al., 1999; Foa et al., 1995; Rasmussen & Tsuang, 1986). Specifically, mean age at intake, slightly higher percentage of women, low rates of racial/ethnic minorities, and OCD symptom severity scores are all comparable to those reported in the DSM-IV field trial (Foa et al., 1995).
Procedures
Participants were recruited from multiple psychiatric treatment settings including consecutive admissions to an outpatient OCD specialty clinic, inpatient units of a private, psychiatric hospital, a community mental health center, two general psychiatric outpatient clinics and the private practices of three experts in cognitive-behavior therapy for OCD. The Butler Hospital and Brown University Institutional Review Boards approved the study. Patients were interviewed in person by trained research assistants after providing written informed consent to participate in annual interviews. Subjects were paid $25 for participating in the intake interview.
The data presented here were collected as part of the intake interview which consisted of standardized semi-structured interviews, rater-administered assessments, and self-report questionnaires. Interviewer training consisted of a rigorous training program described in detail elsewhere (Pinto et al., 2006) and all interviewers demonstrated a high degree of interrater reliability with both clinicians and senior raters (intraclass correlation coefficiencets > .85 for YBOCS total score and SCID diagnoses). Interviewers completed detailed, written narrative summaries of each case which were reviewed by a senior staff member and a clinical psychologist with expertise in OCD. In addition, each case was presented at a weekly staff meeting attended by a psychiatrist and two psychologists with expertise in OCD (M.C.M, J.L.E. and A.P).
Measures
The Butler Hospital OCD Database, a semi-structured rater administered questionnaire, was used to collect detailed information on demographic characteristics, clinical features of OCD, and previous treatments.
Comorbidity was assessed using the Structured Clinical Interview for DSM-IV Axis I Disorders - Patient version (SCID-P) and the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) (First, Gibbon, Spitzer, Williams, & Benjamin, 1997; First, Spitzer, Gibbon, & Williams, 1996). Age of onset was ascertained using the SCID-P and was defined as the age when symptoms first met DSM-IV criteria for the disorder. Substance Use Disorders included Alcohol Abuse or Dependence and Drug Abuse or Dependence (not including nicotine).
Current symptom severity (past week) was assessed using four rater-administered scales and one self-report questionnaire. OCD symptom severity was assessed by the Yale-Brown Obsessive Compulsive Scale (Y-BOCS), a 10-item scale with established reliability and validity (Goodman, Price, Rasmussen, Mazure, Delgado et al., 1989; Goodman, Price, Rasmussen, Mazure, Fleischman et al., 1989). Insight regarding OCD symptoms was evaluated using the Brown Assessment of Beliefs Scale (BABS), a 6-item scale (Eisen et al., 1998). The 25-item Modified Hamilton Rating Scale for Depression (MHRSD), a modified version of the widely accepted Hamilton Rating Scale for Depression (HRSD), was used to assess severity of depressive symptoms (Hamilton, 1960; Miller, Bishop, Norman, & Maddever, 1985). The validity of the MHRSD has been established by comparing it to the original HRSD (Miller et al., 1985). The Global Assessment of Functioning Scale (GAF) was used to assess global severity of psychopathology and impairment in functioning (American Psychiatric Association, 2000). Quality of life was assessed using the general subscale of the Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q), a reliable and valid self-report measure (Endicott, Nee, Harrison, & Blumenthal, 1993). Higher scores on the symptom severity measures (YBOCS, BABS, MHRSD) indicate more severe symptoms and lower scores on the GAF and Q-LES-Q indicate poorer quality of life and functioning.
Statistical Analyses
Statistical analyses were performed using SPSS 14.0 for Windows. Means, standard deviations, frequencies, and percentages were calculated. Chi-square and t-test analyses were used to compare demographic and clinical characteristics of individuals with SUDs (OCD+SUD) to those without SUDs. We also examined differences in characteristics of participants who reported OCD onset prior to SUD onset (n=61) and those of individuals who reported that OCD onset occurred in the same year or at least one year after SUD onset (n=26). All tests were two-tailed with an α level of .01 to account for multiple comparisons.
We conducted logistic regression analyses to identify potential predictors of Substance Use Disorders. Because different types of substances may be linked to OCD in different ways, we ran two separate regression models using lifetime history of any alcohol use disorder (n=77) or drug disorder (n=46) as the outcome variable. Because we were interested in identifying variables that theoretically preceded SUD onset, we excluded current symptom severity items and disorders with an onset following SUD onset and limited analyses only to individuals who reported that SUD onset occured in the same year or at least one year following OCD onset.
Results
Prevalence of Substance Use Disorders
As shown in Table 1, 27% (n=87) of the sample met lifetime DSM-IV criteria for a substance use disorder: 12% met criteria for an alcohol use disorder only (abuse or dependence), 11% met criteria for both an alcohol and a drug use disorder, and 3% met criteria for drug use disorder only. Nearly twice as many individuals met criteria for dependence than abuse. The most commonly abused substances were alcohol, cannabis, and cocaine. Seventeen (5%) participants met current (past month) criteria for a substance use disorder.
Table 1.
Lifetime and Current Comorbidity of Substance Use Disorders among Individuals with OCD (N=323)
| Lifetime N (%) | Current N (%) | |||||
|---|---|---|---|---|---|---|
| Total2 | Abuse | Dependence | Total2 | Abuse | Dependence | |
| Any Substance Use Disorder1 | 87 (26.9) | 36 (11.1) | 65 (20.1) | 17 (5.3) | 3 (1.0) | 14 (4.3) |
| Alcohol Use Disorder | 77 (23.8) | 24 (7.4) | 53 (16.4) | 13 (4.0) | 3 (1.0) | 10 (3.2) |
| Drug Use Disorder | 46 (14.2) | 16 (4.9) | 30 (9.28) | 4 (1.2) | 1 (<1.0) | 1 (<1.0) |
| Cannabis | 17 (5.3) | 9 (2.8) | 8 (2.5) | 3 (1.0) | 1 (<1.0) | 2 (1.0) |
| Cocaine | 12 (3.7) | 2 (1.0) | 10 (3.1) | 2 (1.0) | 0 (0.0) | 2 (1.0) |
| Opioid | 5 (1.5) | 0 (0.0) | 5 (1.5) | 4 (1.2) | 0 (0.0) | 4 (4.2) |
| Sedatives/anxiolytics | 3 (1.0) | 3 (1.0) | 0 (0.0) | 2 (1.0) | 0 (0.0) | 2 (1.0) |
| Polydrug | 6 (1.9) | 2 (1.0) | 4 (1.2) | 1 (<1.0) | 0 (0.0) | 1 (<1.0) |
| Other drug3 | 2 (1.0) | 0 (0.0) | 2 (1.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Diagnoses based on the Structured Clinical Interview for DSM-IV-Patient version. Nicotine and caffeine use were not assessed.
Total number meeting criteria for any substance use disorders does not add up to a sum of abuse and dependence because some participants met criteria for both alcohol and drug use disorders.
Other drugs included stimulants and hallucinogens.
Characteristics of Individuals with SUDs
Demographic and clinical characteristics of participants with OCD+SUD and those without SUD are listed in Table 2. Significantly fewer participants with OCD+SUD than those without SUD had completed a college degree. All other demographic and clinical characteristics were similar between the two groups. Regarding symptom severity at time of assessment, participants with OCD+SUD presented with more severe OCD symptoms, poorer insight regarding OCD, poorer quality of life and greater impairment in overall psychosocial functioning than participants without SUD.
Table 2.
Demographic and Clinical Correlates of OCD Participants with and without a Lifetime Substance Use Disorder (SUD)
| SUD present (N=87) | SUD absent (N=236) | Statistic | df | p-value | |
|---|---|---|---|---|---|
| Age, yrs, Mean (SD), | 37.3 (11.5) | 40.5 (13.4) | 0.963t | 182.10 | .337 |
| Range | 19-61 | 19-75 | |||
| Gender, Male, n (%) | 49 (56.3) | 98(41.5) | 5.612c | 1 | .018 |
| Race/Ethnicity, n (%) | |||||
| Caucasian | 86 (98.8) | 229 (97.0) | * | .679 | |
| Not Hispanic/Latino | 87 (100) | 227 (96.2) | * | .114 | |
| Marital Status, n (%) | |||||
| Never married | 34 (39.1) | 82 (34.7) | 1.801c | 2 | .406 |
| Currently married | 36 (41.4) | 117 (49.6) | |||
| Widow/separated/divorced | 17 (19.5) | 37 (15.7) | |||
| Education, college degree, n (%) | 38 (43.7) | 145 (61.4) | 18.167c | 1 | .004 |
| Unemployed, n (%) | 43 (49.4) | 93 (39.4) | 2.617c | 1 | .106 |
| Age at OCD onset1, Mean (SD) | 17.71 (9.2) | 18.79 (10.0) | 0.880t | 319 | .380 |
| Range | 5-55 | 4-62 | |||
| Age of minor OCD Symptoms1, | |||||
| Mean (SD) | 11.86 (7.1) | 12.23 (8.3) | 0.379t | 160.06 | .705 |
| Range | 3-35 | 4-60 | |||
| Latency to treatment for OCD, yrs | |||||
| Mean (SD) | 11.27 (10.28) | 11.75 (11.71) | 0.336t | 315 | .737 |
| OCD Course (retrospective), n (%) | |||||
| Episodic | 7 (8.0) | 19 (8.1) | * | .020 | |
| Waxing and Waning | 17 (19.5) | 54 (22.9) | |||
| Continuous | 56 (64.4) | 159 (67.4) | |||
| Deteriorating | 6 (6.9) | 2 (0.01) | |||
| Sudden onset of OCD symptoms | 14 (16.3) | 42 (17.8) | .101c | 1 | .751 |
| Current Symptom Severity, Mean (SD) | |||||
| Y-BOCS total score (0-40) | 22.75 (8.9) | 19.75 (8.1) | -2.87t | 321 | .004 |
| BABS total score (0-24) | 8.12 (5.3) | 5.82 (4.8) | -3.58t | 298 | <.001 |
| Q-LES-Q general score (14-70) | 54.11 (18.5) | 63.25 (16.8) | 3.77t | 266 | <.001 |
| GAF (0-100) | 48.20 (12.6) | 53.22 (11.5) | 3.39t | 321 | .001 |
| Comorbid Axis I disorder2 (other than OCD or SUD) | 79 (90.8) | 203 (87.3) | 0.757 | .384 | |
| Any mood disorder | 73 (83.9) | 167 (70.8) | 5.753 | .016 | |
| Major Depressive Disorder | 67 (77.0) | 149 (63.1) | 5.525 | .019 | |
| Any psychotic disorder | 3 (3.4) | 2 (0.8) | * | .123 | |
| Any anxiety disorder (not OCD) | 52 (59.8) | 130 (55.1) | 0.567 | .451 | |
| Any eating disorder | 4 (4.6) | 18 (7.6) | 0.919 | .338 | |
| Any somatoform disorder | 14 (16.1) | 14 (5.9) | 8.287 | .004 | |
| Body Dysmorphic Disorder | 12 (13.8) | 11 (4.7) | 8.022 | .005 | |
| Any impulse disorder | 16 (18.4) | 38 (16.1) | 0.239 | .625 | |
| Any tic disorder | 15 (17.2) | 34 (14.4) | 0.397 | .529 | |
| ADHD | 15 (18.3) | 19 (8.2) | 6.41 | .011 | |
| Comorbid Axis II disorder2 (PD) | 47 (54.0) | 82 (34.7) | 10.44 | .001 | |
| Avoidant PD | 17 (20.0) | 32 (13.9) | 1.79 | .181 | |
| Obsessive Compulsive PD | 32 (37.6) | 52 (22.5) | 7.29 | .007 | |
| Borderline PD | 15 (17.6) | 6 (2.6) | 22.69 | <.001 | |
For Statistic column: t=t-test; c=chi-square;
=Fischer's exact
Age of onset was missing for participants who could not reliably estimate the age of onset of OCD or did not recall minor symptoms prior to onset of clinical symptoms.
Abbreviations: YBOCS = Yale-Brown Obsessive Compulsive Scale; BABS=Brown Assessment of Beliefs Scale; QLESQ=Quality of Life and Enjoyment Survey Questionnaire; GAF = Global Assessment of Functioning
Diagnoses based on the Structured Clinical Interview for DSM-IV-Patient version (SCID-P) and Structured Clinical Interview for DSM-IV -Axis II (SCID-II).
Table 3 shows lifetime functional impairment variables of individuals with and without SUDs. Those with OCD+SUD were more likely to be receiving disability benefits than participants without SUD. In addition, lifetime SUD was associated with a history of being housebound due to OCD symptoms and psychiatric hospitalizations. Although history of suicidal ideation due to OCD was similar among the two groups, those with OCD+SUD were more likely to report suicide attempts than participants without SUD. Both groups reported similar levels of impairment in occupational and social functioning during the worst period of OCD symptoms.
Table 3.
Lifetime Functional Impairment in Participants with and without lifetime Substance Use Disorder (SUD)
| Variable | SUD present (n=87) | SUD absent (n=236) | Statistic1 | p-value |
|---|---|---|---|---|
| Receiving disability payments, n (%) | 27 (31.0) | 36 (15.3) | 10.08c | .001 |
| Disability primarily due to OCD, n (%) | 21 (24.1) | 27 (11.4) | 8.10c | .004 |
| Functional impairment due to OCD: | ||||
| occupational functioning2 , Mean (SD) | 3.0 (0.9) | 2.8 (0.8) | -1.73t | .084 |
| social functioning2, Mean (SD) | 2.7 (0.8) | 2.5 (0.9) | -1.82t | .070 |
| avoidance of occupational activities, n (%) | 66 (75.9) | 145 (61.4) | 6.54c | .011 |
| avoidance of social interactions, n (%) | 73 (84.9) | 176 (74.6) | 3.82c | .051 |
| housebound for at least one week, n (%) | 32 (37.2) | 50 (21.2) | 8.53c | .004 |
| temporarily dropped out of school, n (%) | 15 (17.4) | 26 (11.1) | 2.30c | .129 |
| permanently dropped out of school, n (%) | 15 (20.3) | 17 (18.9) | 6.49c | .011 |
| Suicidality and hospitalizations, n (%) | ||||
| History of suicidal ideation due to OCD | 45 (52.3) | 94 (39.8) | 4.01c | .045 |
| History of at least one suicide attempt | 23 (27.1) | 27 (11.5) | 11.5c | .001 |
| History of psychiatric hospitalization | 44 (50.6) | 62 (26.2) | 17.0c | <.001 |
For statistic column: c=chi-square and t=t-test. For all chi-square analyses, df=1. For all t-test analyses, df=314
Functional impairment was assessed by asking participants to recall the worst period of OCD lifetime. Impairment ranged from no impairment (0) to extreme impairment (4).
The majority of the sample met lifetime criteria for another Axis I disorder (see Table 2). Axis I comorbidity patterns were similar between the two groups with the exception of higher rates of body dysmorphic disorder (BDD) in participants with OCD+SUD than in participants without SUD. Regarding personality disorders, 40% of the entire sample met criteria for a personality disorder and the most common disorders were Avoidant, Obsessive-Compulsive, and Borderline Personality Disorders. Very few participants (n=4, 1%) met criteria for Antisocial Personality Disorder. Compared to participants without an SUD, those with OCD+SUD were more likely to be diagnosed with any personality disorder, Obsessive-Compulsive (OCPD) or Borderline Personality Disorder (BPD).
Relationship of OCD and SUD Onset
As illustrated in Figure 1, the majority (70%, n=61) of participants with OCD+SUD reported that OCD onset preceded SUD onset by at least one year (range 1-27 years, median= 8 years). Less than one-quarter (n=21) reported an onset of OCD at least one year after the onset of the SUD (range 1-36 years, median= 4 years) and 6% (n=5) reported that both disorders onset within the same year. Mean age at OCD onset was late adolescence (18.5 years ±9.79), while the mean age of onset of SUD was in early adulthood (22.4 ± 6.99 years).
Figure 1.
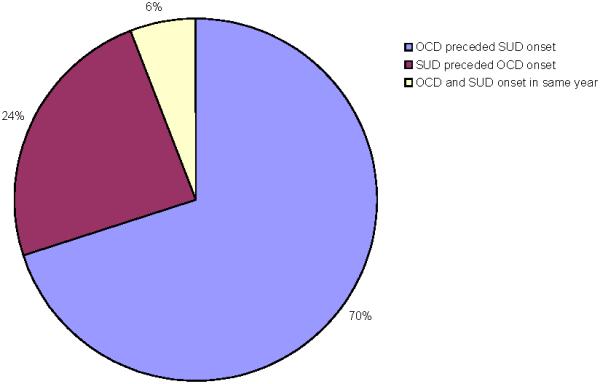
Temporal sequence of OCD and SUD onset (n=87)
The 61 participants who reported OCD onset preceded the SUD onset were compared to the 26 participants who reported OCD onset in the same year or later than the SUD onset. Individuals who reported OCD onset predated SUD onset were significantly younger at OCD onset (M=14.13, SD=6.6 years versus M=26.12, SD=9.1 years, t85=6.89, p<0.001) and older at SUD onset (M=23.6, SD=7.9 years versus 19.8, SD=2.9 years, t83.8=6.89, p<0.001). The two groups did not differ on any other of the demographic or clinical variables listed in Tables 2-3. Individuals with an alcohol use disorder were as likely to report that OCD onset preceded SUD onset as individuals with a drug use disorder (76% vs 65% respectively , χ2 (1) = 1.11, p=.29).
Potential Predictors of SUD
We used logistic regression models to identify potential predictors of SUDs. We excluded the 26 participants who developed an SUD prior to OCD onset because our aim was to explore potential risk factors for developing an SUD among individuals with OCD. Thus, we were most interested in individuals who reported OCD onset preceded or coincided with their SUD onset (i.e. SUD onset secondary to OCD). We included as predictors the following lifetime variables found to have a p-value of <.01 in univariate analyses: gender, education, age at OCD onset 15 or younger (median for this sample), education, history of being housebound due to OCD, suicide attempts, psychiatric hospitalization, lifetime BDD, presence of a personality disorder, OCPD, and BPD. All variables were simultaneously entered as potential predictors. Because different types of substances may be linked to OCD in different ways, we ran two separate regression models using alcohol use disorder (n=77) or drug disorder (n=46) as the outcome variable.
The first model significantly predicted presence of an alcohol use disorder (χ2 =40.25, df=10, p <.001, -2 log likelihood=234.348) and correctly classified 84% of the sample (97% of those with no history of alcohol use disorder and 25% of those with comorbid alcohol use disorders). Significantly increased odds of comorbid SUD were associated with onset of OCD at age 15 or younger (OR= 2.09, p =.04, CI =1.03 to 4.2) and presence of borderline personality disorder (OR=6.05, p =.006, CI=1.70 to 21.62). None of the other variables made a significant contribution to the model.
The second model, using presence of a drug use disorder as the outcome variable, significantly predicted lifetime drug use disorder (χ2 =47.00, df=10, p <.001, -2 log likelihood=135.878) and correctly classified 93% of the sample (99% of those without a drug use disorder and 32% of those with a comorbid drug use disorder). Significantly increased odds of comorbid drug use disorders were associated with number of suicide attempts (OR= 1.54, p =.032, CI =1.04 to 2.29) and presence of borderline personality disorder (OR=9.17, p <.001, CI=2.71 to 31.05). None of the other variables made a significant contribution to the model.
Discussion
This is the first study to systematically examine characteristics of individuals with OCD and comorbid SUDs in a large, clinical sample of individuals who identify OCD as their primary psychiatric disorder. Unlike previous studies, we recruited consecutive patients from diverse treatment settings including an OCD specialty clinic, inpatient and day treatment programs for mental health and substance use, private practice settings, and a community mental health center. Our finding that 27% of our sample met lifetime criteria for an SUD is consistent with rates reported in another study of 334 outpatients seeking treatment at an OCD specialty clinic in Great Britain (Denys et al., 2004). However, rates of SUDs in this sample were nearly double the lifetime prevalence of SUDs reported in the U.S. general population (Kessler et al., 2005). OCD symptoms often go undetected in individuals with SUDs (Eisen & Rasmussen, 1989; Hasin & Grant, 1987) and only half of individuals with these co-occurring disorders seek treatment for their OCD (Hasin & Grant, 1987; Mayerovitch et al., 2003) which suggests that these results may underestimate actual comorbidity rates. Nonetheless, rates of SUDs in this sample are lower than those reported for other psychiatric disorders such as Schizophrenia, Body Dysmorphic Disorder, and Bipolar Disorders (J. E. Grant, Menard, Pagano, Fay, & Phillips, 2005; Kessler et al., 1994; Regier et al., 1990).
An interesting finding was the low rate of current SUDs (5%) which is consistent with other studies of OCD samples (Denys et al., 2004) but lower than current SUD rates for the general population (8-11%), body dysmorphic disorder (13-17%), non-OCD anxiety disorders (9-16%), or major depression (9%) (B. F. Grant et al., 2004; J. E. Grant et al., 2005; Gunstad & Phillips, 2003; Kessler et al., 1994; Merikangas & Angst, 1995; Regier et al., 1990; Rodriguez et al., 2004; Zimmerman, Chelminski, & McDermut, 2002). Perhaps the majority of patients with OCD are able to quit or reduce their substance use as they receive treatment. Although we collected data regarding OCD treatment history, we did not collect SUD treatment history. Prospective data are being collected to better understand whether SUD remission is associated with treatment focused on OCD and/or SUD symptoms. Clinical experience yields yet another hypothesis that some individuals may develop SUDs as a way to cope with OCD symptoms (self-medication hypothesis) but eventually view substance use as an ineffective coping strategy.
Individuals with and without SUDs were similar in characteristics with a few exceptions. Univariate analyses showed that participants with OCD+SUD were less educated and had higher rates of certain comorbidities (BDD, OCPD and BPD, specifically) than those without SUDs. However, logistic regression analyses indicated that only BPD was independently associated with increased risk of alcohol and/or drug use disorder which is not surprising given that impulsive behaviors (such as substance use) are a diagnostic criterion for BPD and previous studies have documented high rates of SUDs in individuals with BPD (Cohen, Chen, Crawford, Brook, & Gordon, 2007; Feske, Tarter, Kirisci, & Pilkonis, 2006). Cluster B personality traits (borderline, histrionic, narcissistic) in adolescence have also been linked to later onset of SUD onset in prospective studies of adolescent community samples (Cohen et al., 2007).
An unexpected finding was that juvenile-onset of OCD (defined as age 15 or younger) was independently associated with increased lifetime rates of alcohol use disorders. This finding is consistent with reports from STAR*D that a younger age at onset of depression is associated with increased risk of SUDs (Davis et al., 2006) and suggests that individuals who experience distressing psychiatric symptoms at a young age may be more vulnerable to using substances. It is unclear why we did not also find an association between juvenile-onset OCD and drug use disorders. One explanation could be that individuals with OCD are more risk aversive and may perceive more risk associated with drug use than alcohol use. A second explanation could be that alcohol is more readily accessible than illicit substances. Finally, a sample selection bias could also explain these findings. That is, individuals with drug use disorders (especially those that are currently using) may be less likely to participate in a longitudinal research study.
While there were no differences in history of suicidal ideation, individuals with substance use disorders had higher rates of suicide attempts and psychiatric hospitalizations. This is inconsistent with previous literature that supports a relationship between alcohol use and suicidality (McCloud, Barnaby, Omu, Drummond, & Aboud, 2004; Sher, 2006). Specifically, comorbid drug use disorders were associated with increased number of suicide attempts suggesting that these individuals are at greater risk for acting on suicidal ideation. One explanation for these findings is that individuals with OCD and drug use disorders may be more likely to act on their suicidal ideation. An alternative explanation is that this group may have a common vulnerability for both disorders (e.g. impulsivity).
Although differences in (current) OCD symptom severity and psychosocial functioning at the time of assessment were statistically significant, the differences in mean scores (e.g. 3-point difference on the YBOCS) do not appear to be clinically significant. A limitation of our study is that only 5% of our sample met full DSM-IV (current) criteria for an SUD at the time of assessment. Therefore, the relationship of current substance use and OCD symptom severity remains unclear and is an important area of investigation for future research. Substance use may interfere with OCD treatment and for this reason is often an exclusion criterion for controlled trials of cognitive-behavioral therapy (CBT) and/or medications. Future studies examining the impact of substance use symptoms on OCD course or treatment outcome would be beneficial as there is very little known about the efficacy of treatment for individuals with these co-occurring disorders.
The majority of participants with OCD+SUD reported that OCD onset preceded the SUD onset. This finding is consistent with epidemiological data indicating that onset of anxiety disorders (median age =11) usually precedes onset of SUDs (median age = 20) (Karno et al., 1988; Kessler et al., 2005; Merikangas et al., 1998). These results are also consistent with self-medication and tension-reduction models that suggest that substance use may be functioning to reduce anxiety states (Conger, 1956). Future studies may explore these models by examining reasons for substance use and the short-term effects on OCD symptoms.
Our study has several strengths including a large, well-characterized clinical sample, standardized assessments, and recruitment from several sites where OCD patients typically receive psychiatric treatment. This increases the generalizability of our findings to other clinical samples of OCD (Pinto et al., 2006) . However, results should be interpreted in the context of the study limitations. Results cannot be generalized to individuals with OCD in the community. In addition, our sample consisted mostly of Caucasian individuals and thus results may not generalize to individuals of different ethnic and racial groups. The cross-sectional design also limited conclusions to clinical correlates of SUDs rather than causal inferences. Finally, age of onset of each of the disorders was retrospectively ascertained and thus susceptible to recall bias. Despite these limitations, we believe our results are of interest to clinicians and OCD researchers.
This study has important clinical and research implications. Results suggest that a comprehensive assessment of lifetime history of substance use is necessary as patients with comorbid SUDs and OCD can be expected to require treatment for a longer duration and possibly require additional interventions. Future research focusing on the mechanism underlying this relationship could identify risk factors and have important treatment development implications for this particularly challenging clinical problem. Treatment of SUDs and co-occurring psychiatric disorders is an area of research that seems promising for other disorders but has yet to be developed in OCD (Myrick & Brady, 2003).
Acknowledgments
This study was supported by a grant (R01 MH060218) to the last author from the National Institute of Mental Health, Bethesda, MD, USA.
The study was carried out at Butler Hospital, 345 Blackstone Boulevard, Providence, RI 02906
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Fourth ed. American Psychiatric Association; Washington, D.C.: 2000. [Google Scholar]
- Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disorders. 2001;3(4):181–188. [PubMed] [Google Scholar]
- Cohen P, Chen H, Crawford TN, Brook JS, Gordon K. Personality disorders in early adolescence and the development of later substance use disorders in the general population. Drug and Alcohol Dependence. 2007;88(Suppl 1):S71–84. doi: 10.1016/j.drugalcdep.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger JJ. Alcoholism: theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Davis LL, Frazier E, Husain MM, Warden D, Trivedi M, Fava M, et al. Substance use disorder comorbidity in major depressive disorder: a confirmatory analysis of the STAR*D cohort. American Journal of Addictions. 2006;15(4):278–285. doi: 10.1080/10550490600754317. [DOI] [PubMed] [Google Scholar]
- Denys D, Tenney N, van Megen HJ, de Geus F, Westenberg HG. Axis I and II comorbidity in a large sample of patients with obsessive-compulsive disorder. Journal of Affective Disorders. 2004;80(23):155–162. doi: 10.1016/S0165-0327(03)00056-9. [DOI] [PubMed] [Google Scholar]
- Diniz JB, Rosario-Campos MC, Shavitt RG, Curi M, Hounie AG, Brotto SA, et al. Impact of age at onset and duration of illness on the expression of comorbidities in obsessive-compulsive disorder. Journal of Clinical Psychiatry. 2004;65(1):22–27. doi: 10.4088/jcp.v65n0104. [DOI] [PubMed] [Google Scholar]
- Drake RE, Bartels SJ, Teague GB, Noordsy DL, Clark RE. Treatment of substance abuse in severely mentally ill patients. Journal of Nervous and Mental Disease. 1993;181(10):606–611. doi: 10.1097/00005053-199310000-00006. [DOI] [PubMed] [Google Scholar]
- Eisen JL, Goodman WK, Keller MB, Warshaw M, DeMarco LM, Luce DD, et al. Patterns of remission and relapse in obsessive-compulsive disorder: a 2-year prospective study. Journal of Clinical Psychiatry. 1999;60(5):346–351. doi: 10.4088/jcp.v60n0514. [DOI] [PubMed] [Google Scholar]
- Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, Rasmussen SA. The Brown Assessment of Beliefs Scale: reliability and validity. American Journal of Psychiatry. 1998;155(1):102–108. doi: 10.1176/ajp.155.1.102. [DOI] [PubMed] [Google Scholar]
- Eisen JL, Rasmussen SA. Coexisting obsessive compulsive disorder and alcoholism. Journal of Clinical Psychiatry. 1989;50(3):96–98. [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, Blumenthal R. Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacology Bulletin. 1993;29(2):321–326. [PubMed] [Google Scholar]
- Fals-Stewart W, Angarano K. Obsessive-compulsive disorder among patients entering substance abuse treatment: prevalence and accuracy of diagnosis. The Journal of Nervous and Mental Disease. 1994;182:715–719. doi: 10.1097/00005053-199412000-00007. [DOI] [PubMed] [Google Scholar]
- Feske U, Tarter RE, Kirisci L, Pilkonis PA. Borderline personality and substance use in women. American Journal of Addictions. 2006;15(2):131–137. doi: 10.1080/10550490500528357. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) American Psychiatric Press; Washington, D.C.: 1997. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I Disorders - Patient Edition (SCID/IP Version 2.0) Biometrics Research Department, New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Foa EB, Kozak MJ, Goodman WK, Hollander E, Jenike MA, Rasmussen SA. DSM-IV field trial: obsessive-compulsive disorder. American Journal of Psychiatry. 1995;152(1):90–96. doi: 10.1176/ajp.152.1.90. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry. 1989;46(11):1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischman RL, Hill CL, et al. The Yale-Brown obsessive-compulsive scale: I. Development, use and reliability. Archives of General Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61(4):361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Grant JE, Menard W, Pagano ME, Fay C, Phillips KA. Substance use disorders in individuals with body dysmorphic disorder. Journal of Clinical Psychiatry. 2005;66(3):309–316. doi: 10.4088/jcp.v66n0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunstad J, Phillips KA. Axis I comorbidity in Body Dysmorphic Disorder. Comprehensive Psychiatry. 2003;44:270–276. doi: 10.1016/S0010-440X(03)00088-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology and Neurosurgical Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Grant BF. Psychiatric diagnosis of patients with substance abuse problems: a comparison of two procedures, the DIS and the SADS-L. Alcoholism, drug abuse/dependence, anxiety disorders and antisocial personality disorder. Journal of Psychiatric Research. 1987;21(1):7–22. doi: 10.1016/0022-3956(87)90005-7. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Tsai WY, Endicott J, Mueller TI, Coryell W, Keller M. Five-year course of major depression: effects of comorbid alcoholism. Journal of Affective Disorders. 1996;41(1):63–70. doi: 10.1016/0165-0327(96)00068-7. [DOI] [PubMed] [Google Scholar]
- Karno M, Golding I, Sorenson S, Burnam M. The epidemiology of obsessive-compulsive disorder in five US communities. Archives of General Psychiatry. 1988;45:1094–1099. doi: 10.1001/archpsyc.1988.01800360042006. [DOI] [PubMed] [Google Scholar]
- Keel PK, Dorer DJ, Eddy KT, Franko D, Charatan DL, Herzog DB. Predictors of mortality in eating disorders. Archives of General Psychiatry. 2003;60(2):179–183. doi: 10.1001/archpsyc.60.2.179. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Koizumi HM. Obsessive-compulsive symptoms following stimulants. Biological Psychiatry. 1985;20(12):1332–1333. doi: 10.1016/0006-3223(85)90120-9. [DOI] [PubMed] [Google Scholar]
- Koran LM, Aboujaoude E, Bullock KD, Franz B, Gamel N, Elliott M. Double-blind treatment with oral morphine in treatment-resistant obsessive-compulsive disorder. Journal of Clinical Psychiatry. 2005;66(3):353–359. doi: 10.4088/jcp.v66n0312. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings. Clinical Psychology Review. 2000;20(2):149–171. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- Mayerovitch JI, du Fort GG, Kakuma R, Bland RC, Newman SC, Pinard G. Treatment seeking for obsessive-compulsive disorder: role of obsessive-compulsive disorder symptoms and comorbid psychiatric diagnoses. Comprehensive Psychiatry. 2003;44(2):162–168. doi: 10.1053/comp.2003.50005. [DOI] [PubMed] [Google Scholar]
- McCloud A, Barnaby B, Omu N, Drummond C, Aboud A. Relationship between alcohol use disorders and suicidality in a psychiatric population: in-patient prevalence study. British Journal of Psychiatry. 2004;184:439–445. doi: 10.1192/bjp.184.5.439. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Angst J. Comorbidity and social phobia: evidence from clinical, epidemiologic, and genetic studies. Eur Arch Psychiatry Clin Neurosci. 1995;244(6):297–303. doi: 10.1007/BF02190407. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, et al. Comorbidity of substance use disorders with mood and anxiety disorders: results of the international consortium in psychiatric epidemiology. Addictive Behaviors. 1998;23(6):893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Miller IW, Bishop S, Norman WH, Maddever H. The Modified Hamilton Rating Scale for Depression: reliability and validity. Psychiatry Research. 1985;14(2):131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Yarnold PR, Levinson DF, Singh H, Bellack AS, Kee K, et al. Prevalence of substance abuse in schizophrenia: demographic and clinical correlates. Schizophrenia Bulletin. 1990;16(1):31–56. doi: 10.1093/schbul/16.1.31. [DOI] [PubMed] [Google Scholar]
- Myrick H, Brady K. Current review of comorbidity of affective, anxiety, and substance use disorders. Current Opinions in Psychiatry. 2003;16:261–270. [Google Scholar]
- Pinto A, Mancebo MC, Eisen JL, Pagano ME, Rasmussen SA. The Brown Longitudinal Obsessive Compulsive Study: clinical features and symptoms of the sample at intake. Journal of Clinical Psychiatry. 2006;67:703–711. doi: 10.4088/jcp.v67n0503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen SA, Eisen JL. Epidemiology and clinical features of obsessive-compulsive disorder. In: Jenike MA, Baer L, editors. Obsessive-compulsive disorders: Practical management. 3rd ed. Mosby; Boston: 1998. pp. 12–43. [Google Scholar]
- Rasmussen SA, Tsuang MT. Clinical characteristics and family history in DSM-III obsessive-compulsive disorder. American Journal of Psychiatry. 1986;143(3):317–322. doi: 10.1176/ajp.143.3.317. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. Journal of the American Medical Association. 1990;264(19):2511–2518. [PubMed] [Google Scholar]
- Riemann BC, McNally RJ, Cox WM. The comorbidity of obsessive-compulsive disorder and alcoholism. Journal of Anxiety Disorders. 1992;6:105–110. [Google Scholar]
- Robins LN, Helzer JE, Weissman MM, Orvaschel H, Gruenberg E, Burke JD, Jr., et al. Lifetime prevalence of specific psychiatric disorders in three sites. Archives of General Psychiatry. 1984;41(10):949–958. doi: 10.1001/archpsyc.1984.01790210031005. [DOI] [PubMed] [Google Scholar]
- Rodriguez BF, Weisberg RB, Pagano ME, Machan JT, Culpepper L, Keller MB. Frequency and Patterns of Psychiatric Comorbidity in a Sample of Primary Care Patients with Anxiety Disorders. Comprehensive Psychiatry. 2004:129–137. doi: 10.1016/j.comppsych.2003.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satel SL, McDougle CJ. Obsessions and compulsions associated with cocaine abuse. American Journal of Psychiatry. 1991;148(7):947. doi: 10.1176/ajp.148.7.947a. [DOI] [PubMed] [Google Scholar]
- Sher L. Alcoholism and suicidal behavior: a clinical overview. Acta Psychiatrica Scandinavica. 2006;113(1):13–22. doi: 10.1111/j.1600-0447.2005.00643.x. [DOI] [PubMed] [Google Scholar]
- Tohen M, Stoll AL, Strakowski SM, Faedda GL, Mayer PV, Goodwin DC, et al. The McLean First-Episode Psychosis Project: six-month recovery and recurrence outcome. Schizophrenia Bulletin. 1992;18(2):273–282. doi: 10.1093/schbul/18.2.273. [DOI] [PubMed] [Google Scholar]
- Yaryura-Tobias JA, Grunes MS, Todaro J, McKay D, Neziroglu FA, Stockman R. Nosological insertion of axis I disorders in the etiology of obsessive-compulsive disorder. Journal of Anxiety Disorders. 2000;14(1):19–30. doi: 10.1016/s0887-6185(99)00027-4. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Chelminski I, McDermut W. Major depressive disorder and axis I diagnostic comorbidity. Journal of Clinical Psychiatry. 2002;63(3):187–193. doi: 10.4088/jcp.v63n0303. [DOI] [PubMed] [Google Scholar]


