Abstract
Objective
To determine whether a computerized clinical decision support system providing patient-specific recommendations in real-time improves the quality of prescribing for long-term care residents with renal insufficiency.
Design
Randomized trial within the long-stay units of a large long-term care facility. Randomization was within blocks by unit type. Alerts related to medication prescribing for residents with renal insufficiency were displayed to prescribers in the intervention units and hidden but tracked in control units.
Measurement
The proportions of final drug orders that were appropriate were compared between intervention and control units within alert categories: (1) recommended medication doses; (2) recommended administration frequencies; (3) recommendations to avoid the drug; (4) warnings of missing information.
Results
The rates of alerts were nearly equal in the intervention and control units: 2.5 per 1,000 resident days in the intervention units and 2.4 in the control units. The proportions of dose alerts for which the final drug orders were appropriate were similar between the intervention and control units (relative risk 0.95, 95% confidence interval 0.83, 1.1) for the remaining alert categories significantly higher proportions of final drug orders were appropriate in the intervention units: relative risk 2.4 for maximum frequency (1.4, 4.4); 2.6 for drugs that should be avoided (1.4, 5.0); and 1.8 for alerts to acquire missing information (1.1, 3.4). Overall, final drug orders were appropriate significantly more often in the intervention units—relative risk 1.2 (1.0, 1.4).
Conclusions
Clinical decision support for physicians prescribing medications for long-term care residents with renal insufficiency can improve the quality of prescribing decisions.
Trial Registration: http://clinicaltrials.gov Identifier: NCT00599209
Introduction
Older adults residing in long-term care facilities have a high prevalence of renal insufficiency with increased potential for adverse events. 1,2 For these residents, dosing recommendations for many commonly prescribed drugs are based on the level of renal function. The complex association between levels of renal insufficiency and dosing recommendations for the wide variety of available drugs can be a challenge for prescribers. Not surprisingly, several studies in the hospital and long-term care settings have demonstrated substantial rates of inappropriate dosing for patients with renal insufficiency. 3–11
Individualized estimation of appropriate dosing for patients at varying levels of renal function is an issue that could be addressed by computerized clinical decision support systems (CDSS). With the advent of electronic medical records linked to computerized prescriber order entry (CPOE), several experiments with this approach have been assessed in the hospital setting and have demonstrated improved prescribing. 12–15 We hypothesized that implementation of a CDSS providing specific dose recommendations for long-term care residents with renal insufficiency would result in a higher rate of appropriate medication orders and a lower rate of the use of drugs that should be avoided for these patients.
We developed a CDSS built on a commercially purchased CPOE system and conducted a randomized trial of its impact on prescribing in a large long-term care facility.
Methods
The setting for this study is an academically affiliated long-term care facility in Canada with an electronic medical record system including integrated CPOE. 16,17 The study was approved by the institutional review boards of the University of Massachusetts Medical School and the participating facility. The facility's CPOE software was fully linked to information in the electronic medical record and was capable of being programmed to present alerts in real-time during medication orders. Ten community-based physicians provided regular care to long-stay residents. Units are not assigned to physicians by specialty and there is frequent cross-over among units as physicians and partners from their medical groups cover for colleagues on nights, weekends and vacations. The facility had wireless capabilities and physicians could access the system and place medication orders from their off-site offices and homes. Physicians usually ordered medications personally through the CPOE system.
The CDSS for adjusting dose and frequency of medication orders for long-term residents with renal insufficiency was developed by a team of physicians, pharmacists, and informatics professionals. Sixty-two drugs were selected for inclusion based on published guidelines and lists from hospital-based dosing alert systems. We included oral drugs commonly prescribed in the long-term care setting that are primarily eliminated by the kidney and have known nephrotoxic effects or for which drug efficacy may be modified due to renal insufficiency. Decisions on dosing recommendations were based on dose adjustment suggestions in geriatric 18 and psychotropic drug dosing handbooks 19 and the Micromedex® online knowledge base. Further details of the development process have been published previously. 20
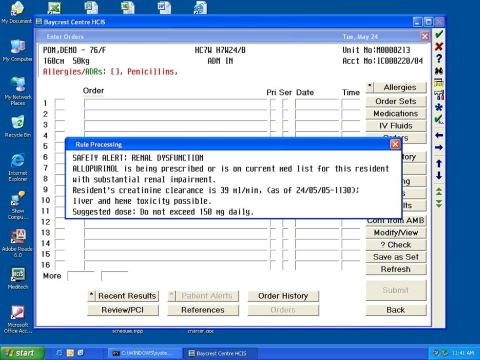
Four types of alerts were developed: (1) alerts recommending maximum total daily dose of the medication; (2) alerts recommending maximum frequency of administration; (3) alerts recommending that the medication be avoided; and (4) alerts notifying prescribers that no creatinine clearance could be calculated for this resident because of missing serum creatinine test results or weight. Calculation of creatinine clearance used the Cockcroft-Gault equation based on age, weight, sex, and serum creatinine. 21 Recommendations in the alerts were directly related to specific levels of renal impairment for each drug. Ninety-four alerts were developed for the 62 drugs. Alerts were triggered when a physician used the CPOE system to initiate an order for one of the specific medications included in the CDSS for a resident with renal insufficiency (▶). After initiating the order, the prescriber could have chosen to continue with the order, modify the dose or frequency, or cancel the order. Alerts were not provided during renewals. The underlying software system could not present alerts from which prescribers could directly submit drug orders so the alerts were solely informational.
Figure 1.
Screen shot of an alert that displays when the physician orders allopurinol for a resident with severe renal impairment.
The 22 long-stay units were randomly assigned for prescribing physicians to receive or not receive the alerts. Randomization was done within blocks by unit type with blocks defined as (1) Alzheimer's disease, (2) stroke and cognition problems, (3) complex medical conditions, (4) behavioral and mental health problems, and (5) functional support. In the control units, current creatinine clearance was displayed during the drug orders with no further recommendations, as had been previously generated in all units of the facility. During the twelve months of the trial, we captured in an audit file each alert that was displayed to a physician when starting to order a drug for a resident of an intervention unit as well as the hidden alerts triggered by initiation of drug orders for residents in the control units. We also output data files containing full details on all electronic drug orders that were actually submitted and all serum creatinine tests with dates and results. Our analysis includes all alerts for drug orders that were directly input into the CPOE system by physicians.
Each alert appearing in an audit trail was categorized as a dose, frequency, avoid, or missing information alert. Alerts were linked to drug orders by resident and date and we determined whether the final drug order's dose or frequency was within the recommended maximum for that drug, based on the resident's calculated creatinine clearance. For each alert to avoid a medication, we reviewed the drug orders for the resident and considered the response to the alert appropriate if the medication was not ordered on the day of the alert. For missing information alerts, we determined whether the alert resulted from a lack of serum creatinine test results or resident weight. Weighing of residents and entry of that information into the electronic medical record was a component of the facility's nursing function, so we focused only on alerts related to missing serum creatinine. These alerts were linked to serum creatinine test results and the physician's actions were considered appropriate if a test was scheduled for the resident within the day following the alert.
Analysis
We output files containing the date of birth and gender of each resident who was present on one of the units involved in the trial during the 12-month period, together with dates of admission, discharge, transitions between units, and temporary absences. We calculated the total resident days, descriptive information including residents' age and gender and the proportion of residents whose calculated creatinine clearance was below 60 mL/min per 1.73 m2 of body-surface area 22 at any time during the year of observation. Intervention and control units were compared using χ2 for the categorical variables and unpaired t test for age.
This trial of a system-level intervention was directed at improving the ordering of drugs for long-term care residents with renal insufficiency. The unit of randomization and analysis was the resident care unit. As in most long-term care facilities, residents were distributed across units by the type of support they needed, rather than by specific medical conditions. Therefore, there were likely to be differences among units in terms of the specific drugs ordered during the 12-month period of the trial. We responded to this by tracking the alerts that identified the initiation of every order of a drug included in the CDSS when it was being prescribed for a resident with renal insufficiency in any unit. This allowed us to compare the proportions of alerts that led to an appropriate final drug order as well as the overall rate of prescribing of drugs that should be avoided among residents with renal insufficiency between the intervention and control units.
We calculated the rates of alerts triggered based on the total resident days in intervention and control units. For each category of alerts, we compared the proportions of final drug orders that were appropriate between intervention and control units by calculating the relative risk and 95% confidence intervals. In a secondary analysis, the rates of prescribing of drugs that should be avoided for residents with renal insufficiency were also calculated as the number of these drugs that were actually ordered divided by the resident days in the intervention and control units. These rates were compared using the rate ratio and 95% confidence interval.
Results
During the 12 months of the trial, more than 800 distinct, individual residents were present on the participating units (▶). In total, there were 107,856 resident days in the intervention units and 106,111 days in the control units. The average age of residents in the intervention and control units was nearly matched but the intervention units had a significantly higher percent of women. Approximately eighty percent of the residents had a creatinine clearance of less than 60 mL/min per 1.73 m2 of body-surface area at some point during the year and the percent did not differ significantly across the intervention and control units.
Table 1.
Table 1 Characteristics of Residents of the Long-stay Units
| Intervention Units | Control Units | p Value | |
|---|---|---|---|
| Number residents | 400 | 433 | |
| Total resident days | 107856 | 106111 | |
| Unit type | |||
| Number resident days | |||
| Alzheimer's units | 38791 | 46722 | |
| Behavioral and mental health units | 10059 | 18115 | |
| Complex medical condition units | 32922 | 21011 | |
| Functional support units | 17784 | 10015 | |
| Stroke and cognition units | 8300 | 10248 | |
| Average age | 86.3 | 86.2 | 0.9443 |
| Percent female | 72.2% | 64.9% | 0.0252 |
| Creatinine clearance % residents < 60 mL/min | 81.0% | 80.9% | 0.9788 |
The rates of alerts were nearly equal in the intervention and control units. Physicians prescribing medications for residents in the intervention units received 274 alerts for a rate of 2.5 per 1,000 resident days. In the control units, 257 alerts were generated during physician medication orders and output to the audit trail for a rate of 2.4 per 1,000 resident days.
The proportions of final drug orders for which doses were appropriate were similar between the intervention and control units (relative risk 0.95, 95% confidence interval 0.83, 1.1) (▶). For each of the remaining alert categories a significantly higher proportion of drug orders was appropriate in the intervention units. The relative risks comparing the intervention to control units for appropriate drug orders were 2.4 for the alert category recommending maximum frequency (1.4, 4.4), 2.6 for the category recommending that a drug be avoided (1.4, 5.0), and 1.8 for alerts about missing serum creatinine (1.1, 3.4). Across all categories of alerts, drug orders in the intervention units were appropriate significantly more often—relative risk 1.2 (1.0, 1.4).
Table 2.
Table 2 Rates of Appropriate Drug Orders by Alert Type
| Alert Type |
Intervention Units |
Control Units |
RR |
95% CI |
||||
|---|---|---|---|---|---|---|---|---|
| Alerts Number | Appropriate Orders |
Alerts Number | Appropriate Orders |
|||||
| Number | % | Number | % | |||||
| Dose | 114 | 86 | 75.4 | 134 | 107 | 79.9 | 0.95 | 0.83, 1.1 |
| Frequency | 49 | 30 | 61.2 | 35 | 9 | 25.7 | 2.4 | 1.4, 4.4 |
| Avoid | 64 | 26 | 40.6 | 65 | 10 | 15.4 | 2.6 | 1.4, 5.0 |
| Missing information | 47 | 30 | 63.8 | 23 | 8 | 34.8 | 1.8 | 1.1, 3.4 |
| Total | 274 | 172 | 62.8 | 257 | 134 | 52.1 | 1.2 | 1.0, 1.4 |
In a further analysis of drugs that should have been avoided, we found that final orders for these drugs were submitted less often in the intervention units, 3.5 per 1,000 resident-days compared to 5.2 per 1,000 resident days in the control units. The rate ratio was 0.68 and this was of borderline statistical significance (95% confidence interval 0.45, 1.0).
Among the drugs triggering alerts, the most common were levofloxacin, nitrofurantoin, cephalexin, metformin, gabapentin, and glyburide (▶).
Table 3.
Table 3 Alerts and Appropriate Drug Orders by Drug
| Drug |
Total Alerts | Intervention Units |
Control Units |
||||
|---|---|---|---|---|---|---|---|
| Alerts Number | Appropriate Orders |
Alerts Number | Appropriate Orders |
||||
| Number | Number | % | Number | % | |||
| Allopurinol | 2 | 0 | 0 | 2 | 1 | 50 | |
| Amantadine | 5 | 2 | 0 | 0 | 3 | 0 | 0 |
| Amoxicillin | 1 | 1 | 1 | 100 | 0 | 0 | |
| Cefprozil | 1 | 0 | 0 | 1 | 1 | 100 | |
| Cefuroxime | 1 | 1 | 1 | 100 | 0 | 0 | |
| Cephalexin | 54 | 31 | 16 | 52 | 23 | 3 | 13 |
| Ciprofloxacin | 33 | 7 | 7 | 100 | 26 | 24 | 92 |
| Clarithromycin | 1 | 1 | 1 | 100 | 0 | 0 | |
| Colchicine | 3 | 0 | 0 | 3 | 2 | 67 | |
| Cotrimoxazole | 31 | 21 | 18 | 86 | 10 | 4 | 40 |
| Diclofenac | 5 | 0 | 0 | 5 | 1 | 20 | |
| Digoxin | 18 | 9 | 8 | 89 | 9 | 9 | 100 |
| Famciclovir | 5 | 4 | 4 | 100 | 1 | 0 | 0 |
| Gabapentin | 38 | 10 | 9 | 90 | 28 | 28 | 100 |
| Glyburide | 37 | 22 | 4 | 18 | 15 | 2 | 13 |
| Ibuprofen | 3 | 0 | 0 | 3 | 0 | 0 | |
| Indomethacin | 2 | 2 | 1 | 50 | 0 | 0 | |
| Levofloxacin | 118 | 68 | 50 | 74 | 50 | 31 | 62 |
| Lithium | 7 | 1 | 1 | 100 | 6 | 6 | 100 |
| Loratadine | 7 | 5 | 4 | 80 | 2 | 0 | 0 |
| Meloxicam | 5 | 0 | 0 | 5 | 0 | 0 | |
| Memantine | 3 | 2 | 1 | 50 | 1 | 1 | 100 |
| Metformin | 39 | 26 | 10 | 39 | 13 | 3 | 23 |
| Metoclopropamide | 2 | 2 | 1 | 50 | 0 | 0 | |
| Metronidazole | 5 | 4 | 4 | 100 | 1 | 1 | 100 |
| Nitrofurantoin | 58 | 26 | 15 | 58 | 32 | 6 | 19 |
| Norfloxacin | 1 | 0 | 0 | 1 | 1 | 100 | |
| Pentoxifyline | 1 | 1 | 1 | 100 | 0 | 0 | |
| Pramipexole | 1 | 1 | 1 | 100 | 0 | 0 | |
| Primidone | 1 | 1 | 0 | 0 | 0 | 0 | |
| Ranitidine | 11 | 4 | 2 | 50 | 7 | 2 | 29 |
| Tetracycline | 2 | 2 | 2 | 100 | 0 | 0 | |
| Trimethoprim | 1 | 1 | 1 | 100 | 0 | 0 | |
| Venlafaxine | 29 | 19 | 9 | 47 | 10 | 8 | 80 |
Discussion
The renal dosing CDSS was successful in improving many aspects of prescribing, including improved frequency of administration, lower rates of orders for drugs that should be avoided, and higher rates of orders for serum creatinine tests when test results were not available. The system did not improve the rate at which physicians ordered appropriate doses for residents with renal insufficiency. In the control units, the rate of appropriate dosing was high (79.9%), substantially higher than has been found during control periods in hospital-based trials of renal dosing CDSS. 12–15
Several studies of the impact of decision support on medication dosing have been conducted in the hospital setting 12–15 although only a few provided recommendations in real-time during prescribing. 14,15 The current project differs from these in several ways. Most of the previous studies were conducted in either the Brigham and Women's Hospital or LDS Hospital, each of which use home-grown CPOE systems designed specifically to provide optimum support for CDSS. The renal dosing CDSS in the current project was developed within a commercially purchased electronic medical record and CPOE system (the Meditech MAGIC platform using Provider Order Management [POM4.9 upgraded to 5.5 during the project]). This system could not present alerts from which prescribers could directly submit drug orders, a capacity that has been considered an important component of effective clinical decision support. 23 Nevertheless, the CDSS did produce a substantial improvement in prescribing.
Previous assessments of the impact of renal dosing CDSS have used time series or alternating periods to compare prescribing with and without decision support. The current project employed a 12-month randomized trial with long-stay units block randomized by type of resident care unit, providing additional assurance that the impact is not confounded by underlying changes in the physician's practice patterns, the facility's infrastructure and management, or the overall patient safety culture.
Long-term care residents and the long-term care setting differ from the acute in-patient setting in several important ways that may impact the value of CDSS. Residents are long-stay and have long term relationships with their physicians. However, physicians working in the long-term care setting see residents less frequently than physicians in hospitals, who often see their patients daily and are more likely to be aware of day-to-day changes in medical status. In contrast, prescribing for long-term care residents is frequently done from a distance. These residents have a complex array of chronic mental and physical conditions and are frequently taking a large number of regularly scheduled medications. In addition, hospitalized patients may suffer acute fluctuations in renal function while long-term care residents frequently have age-related declines in renal function coupled with long-standing underlying chronic diseases and medication regimens that impact the kidney. One study comparing older adults in the ambulatory, hospital and nursing home settings found much higher rates of renal impairment among the nursing home residents. 2 Improving the ability of physicians to prescribe medications accounting for the level of renal function is especially important in the long-term care setting, but has largely been neglected.
There are several limitations to this study. It was set in one long-term care facility with long-standing use of electronic medical records and CPOE. Physicians caring for residents had prior experience with CDSS. They provided care for residents in both intervention and control units. Seeing alerts in the intervention units may have influenced their prescribing in the control units. However, in a previous study of physician responses to alerts in a similar long-term care facility, we found that prescribing in the control units did not improve over a 1-year period of the study. 24
We conclude that provision of clinical decision support for physicians prescribing medications for long-term care residents with renal insufficiency can improve care and that CDSS can be successfully implemented within a commercial CPOE system that has the capacity for linkage to patient-specific clinical data. The impact may be even greater with software that includes the capacity for direct ordering within the alert or in settings without current display of creatinine clearance during drug ordering. Although long-term care facilities have lagged behind other medical settings in adopting electronic medical records and CPOE, larger long-term care facilities and nursing home chains are increasingly implementing these systems. As these efforts expand further, computerized clinical decision support provides the potential to improve the quality of care provided to this vulnerable population.
Acknowledgments
The authors thank Peter Anderson, Mary Thomson, Yen Mee Low Sin, Yana Gurevich, Janet Erramuspe-Mainard, and Jackie Cernieux, MPH for their assistance with technical aspects of this study, and Bessie Petropoulos for assistance with manuscript preparation.
Footnotes
Supported by grants from the Agency for Healthcare Research and Quality (HS010481 and HS15430).
References
- 1.Papaioannou A, Ray JG, Ferko NC, et al. Estimation of creatinine clearance in elderly persons in long-term care facilities Am J Med 2001;111:569-573. [DOI] [PubMed] [Google Scholar]
- 2.Nygaard HA, Naik M, Ruths S, Kruger K. Clinically important renal impairment in various groups of old persons Scand J Prim Health Care 2004;22:152-156. [DOI] [PubMed] [Google Scholar]
- 3.Papaioannou A, Clarke J, Campbell G, Bedard M. Assessment of adherence to renal dosing guidelines in long-term care facilities J Am Geriatr Soc 2000;48:1470-1473. [DOI] [PubMed] [Google Scholar]
- 4.Falconnier AD, Haefeli WE, Schoenenberger RA, Surber C, Martin-Facklam M. Drug dosage in patients with renal failure optimized by immediate concurrent feedback J Gen Intern Med 2001;16:369-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salomon L, Deray G, Jaudon MC, et al. Medication misuse in hospitalized patients with renal impairment Int J Qual Health Care 2003;15:331-335. [DOI] [PubMed] [Google Scholar]
- 6.Long CL, Raebel MA, Price DW, Magid DJ. Compliance with dosing guidelines in patients with chronic kidney disease Ann Pharmacother 2004;38:853-858. [DOI] [PubMed] [Google Scholar]
- 7.Nash IS, Rojas M, Hebert P, et al. Reducing excessive medication administration in hospitalized adults with renal dysfunction Am J Med Qual 2005;20:64-69. [DOI] [PubMed] [Google Scholar]
- 8.van Dijk EA, Drabbe NR, Kruijtbosch M, De Smet PA. Drug dosage adjustments according to renal function at hospital discharge Ann Pharmacother 2006;40:1254-1260. [DOI] [PubMed] [Google Scholar]
- 9.Sweileh WM, Janem SA, Sawalha AF, et al. Medication dosing errors in hospitalized patients with renal impairment: A study in Palestine Pharmacoepidemiol Drug Saf 2007;16:908-912. [DOI] [PubMed] [Google Scholar]
- 10.Quartarolo JM, Thoelke M, Schafers SJ. Reporting of estimated glomerular filtration rate: Effect on physician recognition of chronic kidney disease and prescribing practices for elderly hospitalized patients J Hosp Med 2007;2:74-78. [DOI] [PubMed] [Google Scholar]
- 11.Sheen SS, Choi JE, Park RW, et al. Overdose rate of drugs requiring renal dose adjustment: Data analysis of 4 years prescriptions at a tertiary teaching hospital J Gen Intern Med 2007;223:423-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rind DM, Safran C, Phillips RS, et al. Effect of computer-based alerts on the treatment and outcomes of hospitalized patients Arch Intern Med 1994;154:1511-1517. [PubMed] [Google Scholar]
- 13.Evans RS, Pestotnik SL, Classen DC, Burke JP. Evaluation of a computer-assisted antibiotic-dose monitor Ann Pharmacother 1999;33:1026-1031. [DOI] [PubMed] [Google Scholar]
- 14.Chertow GM, Lee J, Kuperman GJ, et al. Guided medication dosing for inpatients with renal insufficiency J Am Med Assoc 2001;286:2839-2844. [DOI] [PubMed] [Google Scholar]
- 15.Galanter WL, Didomenico RJ, Polikaitis A. A trial of automated decision support alerts for contraindicated medications using computerized physician order entry J Am Med Inform Assoc 2005;12:269-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rochon P, Field TS, Bates DW, et al. Computerized physician order entry with clinical decision support in the long-term care setting: Insights from the Baycrest Center for Geriatric Care J Am Geriatr Soc 2005;53:1780-1789. [DOI] [PubMed] [Google Scholar]
- 17.Rochon PA, Field TS, Bates DW, et al. Clinical application of a computerized system for physician order entry with clinical decision support to prevent adverse drug events in long-term care CMAJ 2006;174:52-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aronoff GR, Berns JS, Brier ME. Drug Prescribing in Renal Failure: Dosing Guidelines for Adults4th edn. Philadelphia, PA: American College of Physicians; 1999.
- 19.In: Bezchlibnyk-Butler KZ, Jeffries JJ, editors. Clinical Handbook of Psychotropic Drugs. 16th edn. Cambridge, MA: Hogrefe & Huber Publishers; 2006.
- 20.Field TS, Rochon P, Lee M, et al. Costs associated with developing and implementing a computerized clinical decision support system for medication dosing for patients with renal insufficiency in the long-term care setting J Am Med Inform Assoc 2008;15:466-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine Nephron 1976;16:31-41. [DOI] [PubMed] [Google Scholar]
- 22.Stevens LA, Levey AS. Chronic kidney disease in the elderly—How to assess risk N Engl J Med 2005;352:2122-2124. [DOI] [PubMed] [Google Scholar]
- 23.Bates DW, Kuperman GJ, Wang S, et al. Ten commandments for effective clinical decision support: Making the practice of evidence-based medicine a reality J Am Med Inform Assoc 2003;10:523-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Judge J, Field TS, DeFlorio M, et al. Prescribers' responses to alerts during medication ordering in the long term care setting J Am Med Inform Assoc 2006;13:384-390. [DOI] [PMC free article] [PubMed] [Google Scholar]