Abstract
The epidemic of HIV in St. Petersburg, which is currently concentrated among injection drug users (IDUs), may be penetrating into the general population. Non-IDUs who have IDU sex partners (SP) could be potential bridges in an expanding epidemic. To investigate potential bridges, we accrued a convenience sample of 288 non-IDUs whose HIV diagnosis was attributed to sexual transmission and we determined the proportion that had IDUs among their SP. Having IDU SP ever (lifetime) and IDU SP in the last year were the key variables for the analysis of potential bridges in this study. The interaction of gender and age was found to be a significant predictor of having lifetime IDU SP (p = 0.006, χ2 test) and IDU SP in the last year (p = 0.05, χ2 test): females aged 26 and younger were more likely to have both lifetime IDU SP and IDU SP in the last year. Among the group of young females, 46% reported ever having an IDU SP. Out of young women reporting ever having an IDU SP, 85% also reported at least one lifetime non-IDU SP. Among the females aged 26 or younger, a lower level of education (odds ratio [OR] = 2.7, confidence interval [CI] = 1.1–6.7), being born in St. Petersburg (OR = 2.9, CI = 1.2–7.2), and alcohol use in the last 30 days (OR = 3.5, CI = 1.3–9.6) were significant correlates for ever having had an IDU SP. Urgent efforts are necessary to expand HIV prevention to target the potential bridging population to prevent further transmission.
Keywords: Russia, Heterosexual, HIV transmission, General population, Bridging
Introduction
Beginning in 1996, the Russian Federation has experienced a rapid and large-scale HIV epidemic that has been concentrated among injection drug users (IDUs).1–5 St. Petersburg, the second largest city with a population of five million people and the biggest seaport in Russia, reflects the situation of HIV in Russia. Up to 80% of the HIV infections have been attributed to injection drug use.6 HIV prevalence among IDUs grew from 2% in 1999 to 30% in 2003 and 50% in 2006;7–9 modeling data suggests a prevalence of 64%.10 HIV incidence among IDUs was 4.5/100 person-years in 2003.2 High levels of sexual risk behaviors both among IDUs and in the general population suggest that HIV infection may be increasing among the groups that acquire HIV through sexual transmission from IDUs.11–14 Therefore, it is important to study the “bridging population” of non-IDUs who have unprotected sex with IDUs.15,16 To meet conditions needed to sustain a generalized sexual HIV epidemic, a bridge population must have two parts: (1) IDUs who have sex with non-IDUs and (2) non-IDUs who have sex with both IDUs and non-IDUs.3 This study seeks to identify individuals in this bridge population and better understand the nature of the risks of HIV transmission with these populations.
The study was conducted by the Biomedical Center as a site-specific component of the ongoing multisite study of Sexual Acquisition and Transmission of HIV–Cooperative Agreement Program (SATH-CAP). A main aim of the parent study was to investigate HIV transmission from IDUs to the general population; this site-specific component took the opposite approach of identifying individuals in the general population who had recently been diagnosed with HIV and determining the likelihood that IDUs, who comprise the core of the HIV epidemic in St. Petersburg, would be among their sexual contacts.
The goals of this particular analysis were the following:
to describe demographic and behavioral characteristics of the sample of non-IDUs recently identified as HIV-positive whose HIV diagnosis was attributed to sexual transmission,
to study gender and age differences in sexual behavior in order to identify among the newly diagnosed those who serve as potential bridges for HIV transmission from IDUs,
to determine factors associated with having IDU SP within the potential bridge population.
Materials and Methods
Study Population
The study population included individuals who were recently diagnosed as HIV-positive and who did not identify themselves as members of the high-risk core groups traditionally associated with HIV infection: IDUs, commercial sex workers (CSW), and men who have sex with men (MSM). IDUs and MSM were targeted in the main cross-site SATH-CAP study. Cases of HIV among individuals outside these core groups were recruited into a convenience sample at the Municipal AIDS Center in St. Petersburg. People from all city districts are referred to the Municipal AIDS Center for confirmation, registration, and future observation. Specialists in infectious diseases were informed about the study and asked to refer potential participants to psychologists of the Biomedical Center who screened, consented, and interviewed them at the AIDS Center. The eligibility criteria for the study were the following: HIV transmission attributed to heterosexual mode, age 18 years and older, referral by AIDS Center doctors within 6 months of their initial confirmed diagnosis, and no history of injection drug use, MSM activity, or commercial sex work.
Data collection was conducted between November 2005 and June 2008. Approximately 350 people referred by infectious disease physicians were screened for the study. The resulting sample consists of 288 people. Others either refused to participate or were found ineligible. The participation in the study was anonymous; no names or personal identifiers were collected. The study protocol was reviewed and approved by the institutional review board of the Biomedical Center and Yale University for the protection of human subjects in research. Participants received condoms, phone cards, and psychological counseling if necessary for participation in this study.
Interview
Participants completed a face-to-face interview that took 15–30 min. The interview consisted of sociodemographic questions; detailed questions about lifetime SP to ascertain who amongst them belonged to risky groups such as IDUs, MSM, CSW; questions regarding casual partners, HIV-positive partners and SP who had been incarcerated, and condom use with these SP; IDU SP during the last year; and questions concerning condom use with all SP.
Statistical Analysis
Statistical analysis was conducted using SAS, version 9.1.3.
Descriptive statistics, such as frequencies and percentages, were used to examine the demographic and behavioral characteristics of the sample. Having lifetime IDU SP (IDU SP ever) and IDU SP in the last year were the key variables for the identification of potential bridges.
To study gender and age differences in sexual behavior, linear logistic models were constructed for the presence of lifetime IDU SP and IDU SP in the last year as outcomes. Age, gender, and their interaction were included in the models as covariates. Interaction of age and gender was added to determine whether the same difference exists between sexual behavior of older and younger people in both gender categories.
Further analysis was conducted for the group of potential bridges, i.e., those individuals who reported sex with IDUs. Bivariate analysis identified factors specific to participants who had lifetime IDU SP at the significance level of 0.2 (χ2 test). Then these factors were included in a multivariate model. Factors were removed using backward selection, until all remaining covariates in the model were significant at value of 0.05 (χ2 test). The following factors were tested for being associated with having lifetime IDU SP: nationality, place of birth, education, marital status, employment, surgery experience, history of sexually transmitted infections (STI), alcohol use in the last 30 days, age at first sex, number of lifetime SP, and years of enrollment.
Results
Demographic and Behavioral Characteristics of the Sample
Table 1 provides the demographic and medical data on the study sample of 288 people who met the eligibility criteria and consented to participate in the study. Most (n = 197, 68%) were women. Ages ranged from 18 to 61 with a median of 26. Ethnically, the vast majority (n = 263, 91%) were Russians; 197 (68%) were born in St. Petersburg. In terms of education, the largest group of study participants had completed their secondary education and had additional vocational school education. For the purpose of further analysis, we divided the sample into two groups by education: 83 people (29%) with any university education and 205 people (71%) with lower levels of education. Almost a quarter of the sample was legally married (n = 70, 24%), while 97 (34%) were in common law, ten (3%) were separated, 20 (7%) were divorced, seven (2%) were widowed, and 84 (30%) were single. For the purpose of further analysis, we divided the sample into two groups: 167 (58%) people who had a steady partner and 121 (42%) who did not. More than two thirds (n = 195, 68%) were employed and few (n = 6, 3%) had been incarcerated. In terms of medical history, more than two thirds (n = 174, 71%) reported a history of surgery, 134 people (47%) had a history of sexually transmitted disease (STD), and 80 (28%) had used alcohol during the past 30 days.
Table 1.
Demographic and medical history characteristics of the sample infected with HIV through heterosexual intercourse (n = 288)
| Characteristic | Frequencies, n (%) |
|---|---|
| Aged 26 and younger | 149 (52) |
| Male | 91 (32) |
| Russian nationality | 263 (91) |
| Born in St. Petersburg | 197 (68) |
| Education | |
| Primary | 23 (8) |
| Secondary | 54 (19) |
| Vocational | 128 (44) |
| University level courses | 36 (13) |
| University | 47 (16) |
| Marital status | |
| Legally married | 70 (24) |
| Common law | 97 (34) |
| Separated | 10 (4) |
| Divorced | 20 (7) |
| Widowed | 7 (2) |
| Single | 84 (29) |
| Employed | 195 (68) |
| Incarceration experience | 6 (3) |
| Surgery experience | 174 (71) |
| Lifetime STI experience | 134 (47) |
Individuals were asked about their SP and their behavior with these partners (Table 2). One third of the study participants (n = 94, 33%) reported ever having sex with a person they knew to be an IDU, and 56 (67%) had never used condoms with these partners. About one fourth (n = 69, 27%) had had sex with a partner who had been in prison, and 37 (65%) of them had never used condoms. Finally, sex with a known HIV-positive partner was reported by 29% (n = 75), and 45 (68%) of them had never used condoms. Approximately half of the sample (n = 150, 52%) had at least one partner who was either IDU, HIV-positive, or had been incarcerated, and 23 people (8%) had partners with all three characteristics.
Table 2.
Behavioral characteristics of the sample infected with HIV through heterosexual intercourse (n = 288)
| Characteristic | Frequencies, n (%) |
|---|---|
| Alcohol use in the past 30 days | 80 (28%) |
| Non-injected drug use in the past 30 days | 17 (6%) |
| Age at first sex 16 and younger | 137 (48%) |
| Number of lifetime sex partners-eight or less | 144 (51%) |
| Sex for money | 6 (2%) |
| Lifetime IDU SP | 94 (33%) |
| IDU SP in the last year | 67 (23%) |
| Never use condoms with IDU SP (n=84) | 56 (67%) |
| Sex with MSM | 3 (1%) |
| Never use condoms with MSM (n=3) | 2 (67%) |
| Sex with CSW | 45 (18%) |
| Never use condoms with CSW (n=42) | 3 (7%) |
| Sex with casual partners | 115 (47%) |
| Never use condoms with casual partners (n=112) | 42 (37%) |
| Sex with foreign citizens | 67 (28%) |
| Never use condoms with foreign citizens (n=56) | 37 (66%) |
| Sex with partners who had been incarcerated | 69 (27%) |
| Never use condoms with partners who had been incarcerated (n=57) | 37 (65%) |
| Sex with HIV positive partners | 75 (29%) |
| Never use condoms with HIV positive partners (n=66) | 45 (68%) |
Gender and Age Differences
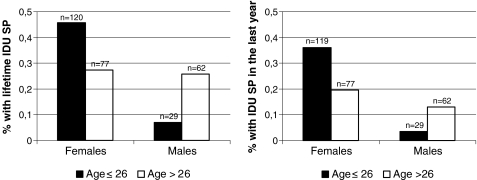
The interaction of gender and age was found to be a significant predictor of having lifetime IDU SP (p = 0.006, χ2 test) and IDU SP in the last year (p = 0.05, χ2 test). Females aged 26 and younger were more likely to have both lifetime IDU SP (p = 0.01, χ2 test) and IDU SP in the last year (p = 0.02, χ2 test) in comparison with females older than 26; males aged 26 and younger, on the contrary, were less likely to have lifetime IDU SP (p = 0.05, χ2 test) and IDU SP in the last year (not statistically significant at the level p = 0.05) in comparison with males older than 26 (Figure 1). Among the group of 120 young females, 55 (46%) reported ever having an IDU SP and 43 (36%) reported having IDU SP in the past year, and these frequencies are the highest among the groups mentioned above. Out of 55 young women reporting ever having an IDU SP, 47(85%) also reported at least one lifetime non-IDU SP.
FIGURE 1.
Frequencies in having IDU SP by gender (left lifetime IDU SP, n = 288; right IDU SP in the last year, n = 287, one missed value).
Factors Associated with Having Lifetime IDU Sex Partner for Females Aged 26 and Younger
Females aged 26 and younger comprised 42% of the total sample and 61% of the female subsample. Because many in this group had characteristics of potential bridges for sexual transmission of HIV from IDUs to the general population, we focused on this particular group in further analysis.
Bivariate analysis using having lifetime IDU SP as an outcome and demographic and behavioral characteristics as covariates revealed that less education, being a native of St. Petersburg, alcohol use in the last 30 days, a history of surgery, and age at first sex were significant correlates for having lifetime IDU SP at the level p = 0.2. The multivariate model with these factors as covariates revealed that education (odds ratio [OR] = 2.7, confidence interval [CI] = 1.1–6.7), being born in St. Petersburg (OR = 2.9, CI = 1.2–7.2), and alcohol use in the last 30 days (OR = 3.5, CI = 1.3–9.6) remained significant at the level p = 0.05 (Table 3).
Table 3.
Factors associated with having lifetime IDU SP for the group of females aged 26 and younger (n = 120)
| Characteristic | Had IDU SP (n = 55, 46%), n (%) | Did not have IDU SP (n = 65, 54%), n (%) | Unadjusted OR (CI) | Adjusted OR (CI) |
|---|---|---|---|---|
| Nationality | ||||
| Russian | 53 (47) | 60 (53) | 2.2 (0.4, 11.9) | |
| Other | 2 (29) | 5 (71) | 1.0 | |
| Place of birth | ||||
| St. Petersburg | 46 (52) | 43 (48) | 2.6** (1.1, 6.3) | 2.7** (1.1, 6.7) |
| Other | 9 (29) | 22 (71) | 1.0 | 1.0 |
| Education | ||||
| Secondary or vocational | 45 (52) | 41 (48) | 2.6** (1.1, 6.2) | 2.9** (1.2, 7.2) |
| High | 10 (29) | 24 (71) | 1.0 | 1.0 |
| Married status | ||||
| Married or common law | 33 (44) | 42 (56) | 0.8 (0.4, 1.7) | |
| Without permanent partner | 22 (49) | 23 (51) | 1.0 | |
| Employed | ||||
| Yes | 31 (46) | 36 (54) | 1.0 (0.5, 2.2) | |
| No | 24 (45) | 29 (55) | 1.0 | |
| Surgery experience | ||||
| Yes | 25 (40) | 38 (60) | 0.4* (0.2, 1.1) | |
| No | 17 (61) | 11 (39) | 1.0 | |
| Alcohol use in the past 30 days | ||||
| Yes | 16 (67) | 8 (33) | 2.9** (1.1, 7.5) | 3.5** (1.3, 9.6) |
| No | 39 (41) | 57 (59) | 1.0 | 1.0 |
| STD | ||||
| Yes | 24 (47) | 27 (53) | 1.1 (0.5, 2.3) | |
| No | 31 (45) | 38 (55) | 1.0 | |
| Age at first sex | ||||
| ≤16 | 38 (55) | 31 (45) | 2.5** (1.2, 5.2) | |
| >16 | 17 (33) | 34 (67) | 1.0 | |
| Lifetime SP | ||||
| ≤8 | 38 (46) | 44 (54) | 1.1 (0.5, 2.3) | |
| >8 | 17 (45) | 21 (55) | 1.0 | |
| Years of enrollment | ||||
| 2005–2006 | 17 (50) | 17 (50) | 1.7 (0.7, 4.4) | |
| 2006–2007 | 24 (50) | 24 (50) | 1.7 (0.7, 4.1) | |
| 2007–2008 | 14 (37) | 24 (63) | 1.0 |
*p = 0.2; **p = 0.05
Discussion
The main goal of this study was to investigate the potential of HIV transmission from IDU to the general population by identifying IDUs among SP of non-IDUs recently identified as HIV-positive. Women aged 26 and younger were found to be the group at greatest risk for having a partner at any time in the past who was known to be an IDU. This group is well-represented in our sample (n = 120, 42% of the total sample). A key finding of this study is that women aged 26 and younger may serve as “bridges” for sexual transmission of HIV from IDUs to the general population where “general” is defined as persons who are unrelated to the drug injecting culture.
Secondary and lower levels of education, being born in St. Petersburg, and alcohol use in the last 30 days were found to be significant correlates for having a lifetime IDU SP for the group of women aged 26 and younger. The result about education level contradicts other findings from Russia but can be explained by insufficient HIV prevention knowledge, lower perception of HIV risk, and earlier beginning of the sexual life for this group. Being born in St. Petersburg as a risk factor is possible due to greater cautions about SP and drugs among women born outside of St. Petersburg compared to those born in this major metropolitan city. We did not ask about lifetime alcohol use in this study; thus alcohol use in the last 30 days can serve as an argument for previous alcohol use that could lead to involvement in risky sexual behaviors.
Our results show that 85% of young females who had lifetime IDU SP had non-IDU SP as well. This finding supports, but does not prove, the conditions for generalized sexual HIV epidemic. Thus, our data show that HIV infection is being transmitted heterosexually now, and this finding is consistent with epidemiological data of the Municipal AIDS Center in St. Petersburg.6
In the whole sample (n = 288), a lack of condom use with potentially risky SP is worth noting and that is consistent with other findings from Russia. Many respondents never used condoms with IDU SP (67%), with SP from countries other than Russia (66%), with partners who were previously incarcerated (65%), and with HIV-positive partners (68%). Failure to use condoms also supports the primary hypothesis for potential bridging transmission. Because we did not determine the temporal relationship between risk behaviors such as condom use and the timing of learning their partner’s HIV status, the high rate of intercourse without a condom with HIV-positive partners might be explained by the fact that a partner’s HIV status was revealed after or during sexual relationship. With other partners, we can observe that knowledge of a condom’s effectiveness in blocking virus transmission was either insufficient or did not influence condom use at all, which is consistent with other findings from Russia.17 Another suggestive finding needing further study was that nearly half of the sample had experienced an STI, a major facilitator of HIV transmission.
The study has several limitations. First, we were not able to trace sexual contacts of respondents and compare their knowledge about their SP with corroborating information. The actual number of IDU SP could be higher than that reported in the study. Second, this is a convenience sample that may not be representative of HIV-positive non-IDUs and HIV-positive young women in St. Petersburg. Third, the study was conducted in St. Petersburg and the results may not be applicable to Russia, especially to its rural areas.
Despite these limitations, data from this study has certain epidemiological value; the findings can be used to plan immediate HIV prevention interventions to target bridging populations in St. Petersburg and conduct HIV primary prevention programs with particular attention to young women. Recent advances in epidemiologic sciences suggest that the next generation of interventions for young females should focus on parenting and parenting skills, sexual risk networks in which drug use and other high-risk behaviors are prevalent, and neighborhoods where these networks exist.18 Particular attention should be paid to the development of new interventions in the Russian context and careful adaptation of established interventions and findings.
Acknowledgments
This work was supported by a grant from the National Institutes of Health (U01DA017387) to Yale School of Medicine and The Biomedical Center. The authors acknowledge the great dedication and enthusiasm of the SATH-CAP research team at The Biomedical Center including E. Fedorova, L. Senkovski, and I. Romanenko and the staff of the Municipal AIDS Center in St. Petersburg, Russia. The authors also thank the investigators at other sites of the SATH-CAP research project and RAND Corporation for the careful attention and interest to this site-specific part of the study.
References
- 1.Dehne KL, Khodakevich L, Hamers FF, Schwartländer B. The HIV/AIDS epidemic in eastern Europe: recent patterns and trends and their implications for policy-making. AIDS. 1999; 13(7): 741–749 Review. [DOI] [PubMed]
- 2.Kozlov AP, Shaboltas AV, Toussova OV, et al. HIV incidence and factors associated with HIV acquisition among injection drug users in St. Petersburg, Russia. AIDS. 2006; 20: 901–906. [DOI] [PubMed]
- 3.Lowndes CM, Renton A, Alary M, Rhodes T, Garnett G, Stimson G. Conditions for widespread heterosexual spread of HIV in the Russian Federation: implications for research, monitoring and prevention. Int J Drug Pol. 2003; 14: 45–62. [DOI]
- 4.Rhodes T, Stimson GV, Crofts N, Ball A, Dehne K, Khodakevich L. Drug injecting, rapid HIV spread, and the ‘risk environment’: implications for assessment and response. AIDS. 1999; 13(Suppl A): S259–S269. [PubMed]
- 5.Rhodes T, Platt L, Maximova S, et al. Prevalence of HIV, hepatitis C and syphilis among injecting drug users in Russia: a multi-city study. Addiction. 2006; 101(2): 252–266. [DOI] [PubMed]
- 6.Zholobov VE, Dvorak SI, Uliukin IM, Vinogradova EN, Volkova GV, Tiusova OV. Current features of HIV-infection in St. Petersburg. Zh Mikrobiol Epidemiol Immunobiol. 2008; 3: 79–81. [PubMed]
- 7.Smolskaia TT, Tretiakova V, Ostrovski DV, Suvorova SV, Ogurtcova S. Three years of experience on HIV control in St. Petersburg among IDUs. XIV International Conference on AIDS. Barcelona, July 2002 [abstract WePeC6119].
- 8.Shaboltas AV, Toussova OV, Hoffman IF, et al. HIV prevalence, sociodemographic, and behavioral correlates and recruitment methods among injection drug users in St. Petersburg, Russia. J Acquir Immune Defic Syndr. 2006; 41: 657–663. [DOI] [PubMed]
- 9.Niccolai LM, Toussova OV, Verevochkin SV, Barbour R, Heimer R, Kozlov AP. High HIV prevalence, suboptimal HIV testing, and low knowledge of HIV-positive serostatus among injection drug users in St. Petersburg, Russia. AIDS Behav. 2008;in press. [DOI] [PMC free article] [PubMed]
- 10.Long EF, Brandeau ML, Galvin CM, et al. Effectiveness and cost-effectiveness of strategies to expand antiretroviral therapy in St. Petersburg, Russia. AIDS. 2006; 20(17): 2207–2215. [DOI] [PubMed]
- 11.Abdala N, Krasnoselskikh TV, Durante AJ, Timofeeva MY, Verevochkin SV, Kozlov AP. Sexually transmitted infections, sexual risk behaviors and the risk of heterosexual spread of HIV among and beyond IDUs in St. Petersburg, Russia. Eur Addict Res. 2008; 14(1): 19–25. [DOI] [PubMed]
- 12.Aral SO, St Lawrence JS, Dyatlov R, Kozlov A. Commercial sex work, drug use, and sexually transmitted infections in St. Petersburg, Russia. Soc Sci Med. 2005; 60(10): 2181–2190. [DOI] [PubMed]
- 13.Benotsch EG, Pinkerton SD, Dyatlov RV, et al. A comparison of HIV/AIDS knowledge and attitudes of STD clinic clients in St. Petersburg, Russia and Milwaukee, WI, USA. J Community Health. 2004; 29(6): 451–465. [DOI] [PubMed]
- 14.Wall M, Tkatchenko-Schmidt E, Renton A. Sexual behaviour in Russia: who exhibits a higher risk? Evidence from longitudinal data. Int J STD AIDS. 2006; 17(11): 759–763. [DOI] [PubMed]
- 15.Burchell AN, Calzavara LM, Orekhovsky V, Ladnaya NN. Characterization of an emerging heterosexual HIV epidemic in Russia. Sex Transm Dis. 2008; 35(9): 807–813. [DOI] [PubMed]
- 16.Field MG. HIV and AIDS in the former Soviet Bloc. N Engl J Med. 2004;351:117–120. [DOI] [PubMed]
- 17.Gerber TP, Berman D. Heterogeneous condom use in contemporary Russia. Stud Fam Plann. 2008; 39(1): 1–17. [DOI] [PubMed]
- 18.Ellen JM. The next generation of HIV prevention for adolescent females in the United States: linking behavioral and epidemiologic sciences to reduce incidence of HIV. J Urban Health. 2003; 80(4 Suppl 3): iii40–iii49. [DOI] [PMC free article] [PubMed]