Abstract
Background
Students attending ‘alternative’ high schools form relatively small, highly mobile high-risk populations, presenting challenges for the design and implementation of HIV-, other STI-, and pregnancy-prevention interventions. This paper describes the rationale, study design, and baseline results for the Safer Choices 2 program.
Study Design
Modified group-randomized intervention trial with crossover of schools but not of students. The study cohort was defined a priori as those who completed the baseline measures and were still enrolled at the time of first follow-up.
Design Results
Of 940 students initially enrolled in the study, 711 (76%) formed the study cohort. There were significant demographic differences between those included and those excluded from the study cohort in sex, age, sexual experience, experience with pregnancy, drug use, and some psychosocial measures. There were no significant differences between the intervention and control groups within the study cohort. The only significant difference between those students excluded from the intervention group and those excluded from the control group was reported age at first intercourse.
Baseline Data Results
Students (n = 940) enrolled were predominately African-American (29.7%) and Hispanic (61.3%); 57.3% were female; 66% had ever had sex; and reported drug use in the previous 30 days ran from 4.3% (cocaine) to 26.9% (marijuana). Of the 627 sexually experienced, 41.8% reported their age at first intercourse as 13 years or younger; 28.5% reported ever being or having gotten someone pregnant; 74% reported sex in the past 3 months. Of the 464 sexually active in the last 3 months, 55.4% reported unprotected intercourse and 31.3% reported using drugs beforehand.
Conclusion
The cross-over design will provide a rigorous test of the intervention; however, loss to follow-up of this population can result in some selection bias. Students attending dropout prevention and recovery schools are at high risk for HIV, STIs, and pregnancy, and are in need of interventions.
Keywords: Randomized Controlled Trial, Group Randomized Trial, Adolescent, Sexual Behavior, HIV Infections/prevention and control, Sexually Transmitted Diseases/prevention and control, Pregnancy in Adolescence/prevention and control, Sex Education, African-Americans, Hispanic-Americans, Unsafe Sex
1. Introduction and background
HIV, other sexually transmitted infections (STIs), and teen pregnancy are major public health problems for adolescents. In the US, nearly one-half of all STIs occur in young people under the age of 25, with an estimated 9.1 million new STI cases in that age group in 2000. [1] Minority youth are at particularly high risk for STIs, HIV, and pregnancy [2–4]: In 2003, of reported AIDS cases among 13- to 19-year-olds, 87% were among Black and Hispanic youth.[5]
While a number of research studies have developed and tested interventions to address these problems in mainstream school settings [6–12], this approach often fails to reach students who run the greatest risk of HIV infection [6]. One possible way of reaching a higher-risk population of students is through implementing programs in alternative schools. Nationally, these schools had an enrollment of 612,900 students (1.3% of all public school students) as of October 1, 2000. Students may be assigned to attend alternative schools for a variety of reasons, including behavioral problems, truancy, excessive absenteeism, poor grades, or pregnancy. Students in alternative schools are more likely to engage in behaviors that put them at high risk of contracting HIV [13–16]. The 1998 national Alternative High School Youth Risk Behavior Survey (ALT-YRBS) found that 87.8% of students reported having had sexual intercourse during their lifetime [13], compared to 49.9% of students in regular high schools in 1999 [17]. Alternative school students were also more likely to have initiated sexual intercourse at an early age, less likely to report using condoms at last sexual intercourse, and almost twice as likely to report using alcohol or drugs at last sexual intercourse [13, 16, 17].
While alternative schools provide a point of access to high-risk adolescents, they also give the researcher several challenges in designing and evaluating health promotion programs using a randomized trial design. This paper addresses some of the design and methodological issues in conducting a school-based intervention trial in alternative schools, in the context of a description of the rationale, study design, and baseline results of a particular intervention. The discussion may also be useful for those designing intervention trials to evaluate programs for other settings, such as clinics or community groups, where a small number of groups is available for randomization and populations are both high-risk and highly mobile.
2. Study Design
Safer Choices 2 is a 5-year research study to adapt, implement, and evaluate a theoretically based, multi-component HIV-, STI-, and pregnancy-prevention program, Safer Choices [7], for use in alternative schools. The adaptation process and program content of Safer Choices 2 is described elsewhere [18]. The adapted program consists of 15 lessons, a video, and journaling activities delivered in a classroom setting by a trained facilitator over an 8-week period. The intervention is based on social cognitive theories [19] and includes skill-based and experiential activities. The overall goal of the Safer Choices 2 intervention trial was to evaluate experimentally the impact of the Safer Choices 2 program in reducing levels of unprotected sexual intercourse relative to those in the comparison condition.
2.1 Cross-over and randomization
The goal of any comparative trial is to provide the basis for valid inference that the intervention as implemented caused the result as observed [20]. Currently, the most well-accepted study design for assessing the efficacy of school-based interventions is the group-randomized trial, whereby schools are the unit of randomization and students are nested within schools [20]. This usual type of design has methodological as well as practical advantages for conducting school-based research, particularly when examining both individual and school effects from the intervention.
The first challenge a researcher faces when using alternative schools as research sites is that the number of alternative schools available to randomize is usually limited. Moreover, there is greater variation among alternative schools in size of the student population, ethnic and racial composition, and enrollment criteria: different alternative schools may serve significantly different populations (e.g., adjudicated youth, pregnant and parenting youth, or youth who have failed academically). It can therefore be difficult to identify enough schools with similar characteristics for randomization into comparable groups. The limited number of alternative schools in any one geographic location and the costs of expanding to a larger geographic region restricts our ability to randomize a large number of schools to each condition, which is the typical way of dealing with this selection issue in school-based research. The nature and composition of alternative schools necessitate a different approach.
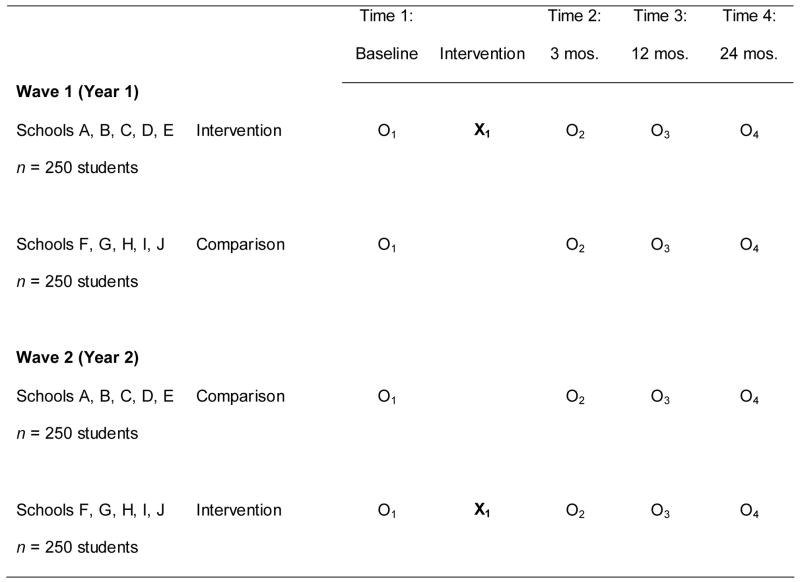
For this study, we used a modified group-randomized intervention trial to test the effectiveness of the program, as illustrated in Figure 1. The study was to be conducted in two waves. For Wave 1, 10 alternative schools were to be randomized (5 to intervention and 5 to comparison conditions), and then 500 students recruited and enrolled into the study. For Wave 2, the treatment conditions among the schools were to be crossed over and 500 new students enrolled into the study. Recruitment and measurement of Wave 1 and Wave 2 cohorts were conducted one year apart to ensure that the rapidly changing developmental trajectories were relatively consistent between cohorts, and that the timing of measurement relative to the school year and holidays was consistent between waves.
Figure 1.
Planned Study Design: 1000 students, 10 schools
Sample size calculations were carried out for each of the primary study outcomes; estimates were made of the sample sizes necessary to ensure 80% power to detect a significant difference for each of the primary outcomes between the intervention and control conditions at all three endpoints. The original sample size calculations were done assuming that the analysis would be performed using continuous outcomes. From previous research on the Safer Choices project, the number of occasions of unprotected sexual intercourse was estimated to have a mean of 2.57 (3.40) at the six-month follow-up, 2.87 (3.67) at the 12-month follow-up, and 3.50 (3.77) at the 24-month follow-up [7, 21]. We judged that a 35% reduction in the number of occasions of unprotected sexual intercourse was important to detect. For example, if the control mean were 2.50, a 35% reduction in the intervention condition would result in a mean of 1.63. (The original randomized trial of the original Safer Choices program showed a 56% reduction in the mean number of occasions of unprotected sexual intercourse.) Assuming an intra-school correlation of 0.01 and two waves of intervention each consisting of 10 schools, the proposed sample size would yield at least 80% power to detect the hypothesized intervention effect at each follow-up.
Intra-class correlation among students in the same school was also accounted for in sample size estimation, and sample sizes were inflated accordingly using an intra-class correlation of 0.01 [21]. We estimated that, due to attrition, we would retain 90% of the randomized students at the 3-month follow-up, 80% at the 12-month follow-up, and 70% at the 24-month follow-up. Final recruitment sample size was then determined based on the sample size calculations, attrition estimation, and recruitment feasibility. Baseline measurements were to be conducted prior to implementation of the intervention, and post-intervention measurements were planned for 3, 12, and 24 months.
To increase comparability of study groups, before randomization we used a modified version of the Multiattribute Utility Measurement (MAUM) procedure as described by Graham et al. [22]. The MAUM procedure uses principal components analysis to assign a score for each school on a single composite blocking factor. For this study, the blocking factor was used to take into account the percentage of Hispanic students, percentage of African-American students, and the overall number of students at each school. The MAUM procedure tends to assure balance on the ranking factor and thus on the underlying components of the score. The ten schools were ranked according to the score. Each adjacent pair of schools was then split, with one school assigned at random to either the intervention or control group and its partner going to the other group for the first year, with group assignment changing in the second year.
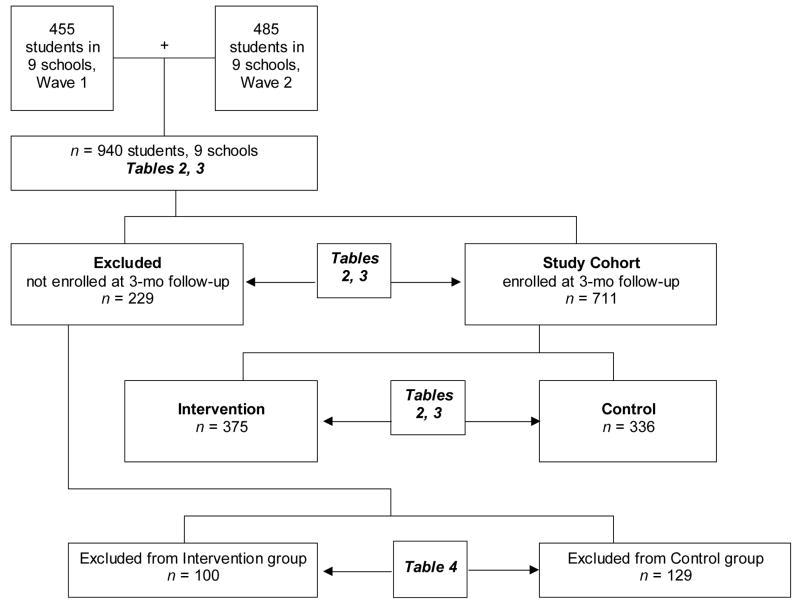
What we did not allow for in planning was the closure of a school after the first year of the study. When this happened, the effects were three-fold: First, the school could not be crossed-over to the other condition in Wave 2. Second, a new group of students could not be recruited from that school for Wave 2. Third, the students recruited from that school for Wave 1 were all lost to long-term follow-up. As the complete loss of a school meant loss of the data for school-level effects, we made the decision to exclude that school’s 34 students recruited in Wave 1 from all analyses. Accordingly, Figure 2 shows a total of 940 students in 9 schools.
Figure 2.
Summary of Recruitment and Retention of Sample and of Organization of Tables Reporting the Analyses
Note: Vertical axis does not reflect time sequence
2.2 Cohort definition
A second challenge in evaluating the effectiveness of any randomized intervention trial is the determination of the cohort: who will be followed to establish whether the intervention is effective. This is a particularly important problem when recruiting and following a population that is both high-risk and highly mobile [23]. The alternative school population is such a population; the drop-out rate is high and many students leave for other reasons (e.g., returning to their originating school). Many alternative schools have a rapid turnover of students, with teens enrolled only for 3 or 6 months, then returning to their originating school. Few alternative schools have stable populations from year to year. As a result, the one-year interval between Waves enabled us to have different samples, thereby minimizing cross-arm contamination. At the same time, the mobility of this population meant that 12-month followup would require tracking the widely dispersed students back to, e.g., their originating schools, worksites, and military postings.
While this population needs to be targeted for interventions, standard study design methodology for school-based intervention research may create nearly insupportable obstacles. Rather than defining the study cohort as those students who consented to participate and completed a baseline survey, we a priori defined the Safer Choices 2 study cohort as those who both completed the baseline survey and who were still enrolled in the school at the first follow-up, which averaged 4 months. This exclusion from the study cohort applied equally to students in the intervention and in the control conditions.
2.3 Hypotheses
With respect to the study design, we tested two hypotheses. The first hypothesis concerns the a priori definition of the study cohort as those both completing baseline measures and still enrolled in the same school at the time of first follow-up. The second hypothesis concerns the feasibility of using a cross-over design and the MAUM procedure to assure comparable intervention and comparison groups.
Students included and excluded from the study cohort (based on completion of baseline data and enrollment in school at first follow-up) are not significantly different regarding demographic characteristics, sexual risk behaviors, or psychosocial variables as measured at baseline.
Students in the intervention and control groups are not significantly different regarding demographic characteristics, sexual risk behaviors, or psychosocial variables as measured at baseline.
Figure 2 shows the organization of the tables used to report the analyses done to test these hypotheses.
3. Study Participants
3.1.1 Target schools
The inclusion criteria for schools were that they be in the metropolitan area where the study was conducted, have students in 9th and 10th grades, have a school-wide enrollment of at least 100 students, and be alternative schools in the sense that they were focused on dropout prevention and recovery (high-risk students). The largest school district in the metropolitan area assisted in locating appropriate schools. The school district itself had 2 schools that met criteria and had 2 additional private schools under contract; 5 charter schools to which it referred students also qualified. The tenth school was in an adjoining school district. The school that closed after the first year was one of the charter schools.
3.1.2 Target study population
Because many of the schools had mixed-grade classrooms, the target population could not be reasonably restricted to 9th and 10th grades. Some schools had ungraded classes, grouped by subject mastery; others had “pods” targeted to grade level; most had a wide range of ages attending. The target population was therefore English-speaking students enrolled in 7th- through 12th-grade classes in 10 alternative schools located in a large urban school district in southeast Texas. Students are in these programs for a variety of reasons including low school performance, high absenteeism, truancy, behavior problems, social problems, pregnancy, or being in the juvenile justice system. All of the students enrolled in the identified schools are considered high-risk adolescents; an estimated 3,605 students were enrolled at the time of the baseline survey. Study staff recruited subjects by providing information to all students enrolled in the schools and by distributing study materials and consent forms to all students, up to three times. Study staff and students were masked as to treatment condition at the time of subject recruitment for the Wave 1 data collection. While students at Wave 2 recruitment were unaware of treatment condition, study staff were not masked as to treatment condition assigned to schools during Wave 2 recruitment. The target sample size was to enroll approximately 50 students per school.
3.2 Consent
Active parental and student consent were obtained by three rounds of distributing information and parental consent forms to students in class to take home. To increase participation rates, two $5 gift certificates were offered as incentive to the students, one for returning the consent form and one for participating in the baseline survey. The study received approval from the Committee for the Protection for Human Subjects at the University of Texas Health Science Center at Houston (HSC-SPH-99-056) and conformed to the principles of the Declaration of Helsinki.
4. Data Collection
Baseline data were collected in two waves: between November 2000 and March 2001, and between November 2001 and March 2002. Data collection for the first follow-up occurred in the period 3–5 months after the intervention was completed, most commonly at 4 months.
Data collection was done in school, during regular school hours, by audio computer-assisted interviews (A-CASI) using laptops computers, set up in private meeting rooms and equipped with headphones to maintain privacy. The use of talking computers has been found to be an effective and reliable method for obtaining confidential information such as sexual risk-taking behaviors, and previous studies indicate that adolescents are more likely to disclose sensitive information such as sexual experience when using talking computers [24–29]. Because all questions are recorded and played back as audio tracks, the use of A-CASI overcomes problems youth might have with reading surveys. The data collection staff gave a brief overview of how to use the computer, and the respondent could ask the data collection staff questions, if needed. Students were again assured that their participation was voluntary and that neither their parents nor their teachers would see their responses. To protect confidentiality, a unique identification number was assigned to each respondent. Due to the nature of the design and the intervention, masking of the treatment groups themselves was not possible; however, data collectors and analysts were blinded to the treatment conditions.
5. Study Measures
Measures were adapted from the Safer Choices questionnaire, which was developed in cooperation with the Centers for Disease Control and Prevention and demonstrated to be valid and reliable [30]. All measures had been extensively pilot-tested and used among populations of multi-ethnic, urban-dwelling public school students. It was known at the outset that the majority of students in these schools are sexually experienced, and that it was likely many if not most were also currently sexually active; both the content of the intervention and the measures used reflected these realities. The self-report measures assessed demographic characteristics, sexual behaviors, drug behaviors, and sexuality-related psychosocial factors. Based on then-current popularities, drug behaviors queried were the use in the previous 30 days of marijuana, cocaine, and codeine cough syrup. Psychosocial factors measured included attitudes, knowledge, perceived normative beliefs, self-efficacy, and perceived barriers to condom use. Table 1 lists the psychosocial measures with their response format (e.g., yes/no, Likert scale) and Cronbach’s alpha. The primary outcomes to be examined to evaluate the effectiveness of the intervention trial will be the proportion of students ever having sexual intercourse, the proportion of students engaging in sexual intercourse in the past 3 months, and the proportion of students having unprotected sexual intercourse in the previous 3 months. In looking at all three factors—initiation, lifetime history, and current activity—the intention is to give a picture of the prevalence and incidence of the behavior in the study population.
Table 1.
Psychosocial variables
| Construct | Number of items | Example | Response | Chronbach’s Alpha |
|---|---|---|---|---|
| Attitudes | ||||
| sexual intercourse | 2 | “I believe it’s OK for people my age to have sex with a steady boyfriend or girlfriend” | 4-point response format, from “definitely yes” to “definitely no” | .68 |
| condoms | 3 | “I believe condoms should always be used if a person my age has sex.” | .80 | |
| Knowledge | ||||
| HIV | 4 | “STDs put you at higher risk of getting infected with HIV.” | true false not sure |
.38 |
| Other STDs | 5 | “Pain when urinating is a common sign of an STD (not including HIV).” | no yes not sure |
.72 |
| Normative Beliefs | ||||
| sexual intercourse | 2 | “Most of my friends believe people my age should wait until they are older before they have sex.” | 4-point response format, from “definitely yes” to “definitely no” | .51 |
| condoms | 3 | “Most of my friends believe condoms should always be used if a person my age has sex.” | .87 | |
| Self-Efficacy | ||||
| refusing sex | 3 | “How sure are you that you could keep from having sex until you feel ready?” | “totally sure” “kind of sure” “not sure at all” |
.69 |
| condom use | 3 | “How sure are you that you could use a condom (rubber) correctly or explain to your partner how to use a condom correctly?” | .69 | |
| communicating with a partner about condom use | 3 | “How sure are you that you could convince your partner that you also need to use condoms (rubbers)?” | .64 | |
| Perceived Barriers | 3 | “I would feel uncomfortable carrying condoms with me.” | 4-point response format, from “I strongly agree” to “I strongly disagree” | .8214 |
Note: Items and Chronbach’s Alphas: Basen-Engquist K, Masse LC, Coyle K, Kirby D, Parcel GS, Banspach S et al. Validity of scales measuring the psychosocial determinants of HIV/STD-related risk behavior in adolescents. Health Educ Res 1999; 14(1):25–38.
6. Statistical Methods
The primary goal of the analysis was to profile students in each of the study groups to ensure comparability between groups. The secondary purpose of the analysis was to look at the characteristics of those students retained in the cohort vs. those excluded. The results from this analysis helped with the ability to generalize the results to the larger population. For both sets of analyses, descriptive statistics were used to profile the characteristics of the groups (intervention vs. control and excluded vs. included). Means and standard deviations were calculated for the psychosocial and behavioral outcomes at baseline. Distributions of the key demographic measures were also explored in order to identify any key differences between the intervention and control conditions as well as between those students who were included vs. excluded from the cohort. Chi-square and t-tests were carried out to formally test for statistical differences between the two sets of conditions with regard to these measures. It was anticipated that some intra-class correlation (ICC) would be present among students in the same school. The presence of intra-class correlations can lead to an underestimation of the standard error, which in turn can lead to an increased type I error (probability of falsely finding a significant difference). Because the tests carried out in this analysis were looking to show no differences between groups, no adjustment for ICC would in fact lead to a more conservative test (a slightly increased risk of finding a difference that may not be present). Based on this rational and for simplicity of analysis and interpretation, no adjustment for ICC was made.
7. Results
Figure 2 shows the recruitment and retention of the study sample and the organization of the tables reporting the analyses done to test the hypotheses discussed in this paper.
Table 2 displays the overall demographic and behavioral and Table 3 the psychosocial characteristics of the study sample, of those students enrolled at the end of the spring semester and included in the study cohort compared to those not enrolled and excluded, and of those in the intervention group compared to the control group. Of the 940 students enrolled in the program at baseline, 61% were Hispanic, 30% were African American, and 9% were classified as “other ethnicities” (White, Asian, and mixed race/ethnicity). The age of students ranged from 12 to 20 years, with a median age of 16 years, and 57% were female. As expected, the majority of students had been sexually active, and, among those, more than a quarter had been pregnant or had gotten someone pregnant. Almost one-quarter (n = 229) of students who had initially enrolled in the study and completed baseline were not enrolled in school by the end of the spring semester, and therefore were not considered as part of the cohort to follow. Reasons for not being enrolled in school included dropping out of school, completing high school requirements and graduating, being arrested, and moving back to their originating school. Because of the substantial number (24%) of students who were excluded from the study, it is important to understand the differences between those who remained in the study and those who were excluded from the cohort definition to determine whether a substantial selection bias exists.
Table 2.
Baseline Demographic and Behavioral Data
| All Students n=940 |
Excluded n=229 |
Included n=711 |
χ2p-value | Intervention n=375 |
Control n=336 |
χ2p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |||
| Demographics | ||||||||||||
| Ethnicity | 0.16 | 0.40 | ||||||||||
| African-American | 279 | 29.7 | 78 | 34.1 | 201 | 28.3 | 111 | 29.6 | 90 | 26.8 | ||
| Hispanic | 576 | 61.3 | 128 | 55.9 | 448 | 63.0 | 228 | 60.8 | 220 | 65.5 | ||
| Other | 85 | 9.0 | 23 | 10.0 | 62 | 8.7 | 36 | 9.6 | 26 | 7.7 | ||
| Gender | 0.02 | 0.89 | ||||||||||
| Male | 401 | 42.7 | 113 | 49.3 | 288 | 40.5 | 151 | 40.3 | 137 | 40.8 | ||
| Female | 539 | 57.3 | 116 | 50.7 | 423 | 59.5 | 224 | 59.7 | 199 | 59.2 | ||
| Age | <0.001 | 0.08 | ||||||||||
| ≤13 years | 113 | 12.0 | 12 | 5.2 | 101 | 14.2 | 51 | 13.6 | 50 | 14.9 | ||
| 14 years | 138 | 14.7 | 19 | 8.3 | 119 | 16.7 | 50 | 13.3 | 69 | 20.5 | ||
| 15 years | 176 | 18.7 | 46 | 20.1 | 130 | 18.3 | 66 | 17.6 | 64 | 19.0 | ||
| 16 years | 173 | 18.4 | 45 | 19.7 | 128 | 18.0 | 73 | 19.5 | 55 | 16.4 | ||
| 17 years | 161 | 17.1 | 42 | 18.3 | 119 | 16.7 | 72 | 19.2 | 47 | 14.0 | ||
| ≥18 years | 179 | 19.0 | 65 | 28.4 | 114 | 16.0 | 63 | 16.8 | 51 | 15.2 | ||
| Grades in school (self-report) | 0.10 | 0.15 | ||||||||||
| Mostly A’s and B’s | 416 | 44.3 | 93 | 40.6 | 323 | 45.4 | 180 | 48.0 | 143 | 42.6 | ||
| Mostly B’s and C’s | 416 | 44.3 | 100 | 43.7 | 316 | 44.4 | 153 | 40.8 | 163 | 48.5 | ||
| Mostly C’s and D’s | 88 | 9.4 | 27 | 11.8 | 61 | 8.6 | 37 | 9.9 | 24 | 7.1 | ||
| Mostly D’s and F’s | 13 | 1.4 | 6 | 2.6 | 7 | 1.0 | 3 | 0.8 | 4 | 1.2 | ||
| Missing data | 7 | 0.7 | 3 | 1.3 | 4 | 0.6 | 2 | 0.5 | 2 | 0.6 | ||
| Highest level of parental education | 0.29 | |||||||||||
| Both parents < high school | 404 | 43.0 | 91 | 39.7 | 313 | 44.0 | 0.55 | 155 | 41.3 | 158 | 47.0 | |
| Parent is a high school grad | 247 | 26.3 | 61 | 26.6 | 186 | 26.2 | 101 | 26.9 | 85 | 25.3 | ||
| Parent has some college | 131 | 13.9 | 31 | 13.5 | 100 | 14.1 | 60 | 16.0 | 40 | 11.9 | ||
| Parent is a college graduate | 144 | 15.3 | 41 | 17.9 | 103 | 14.0 | 56 | 14.9 | 47 | 14.0 | ||
| Missing data | 14 | 1.5 | 5 | 2.2 | 9 | 1.3 | 3 | 0.8 | 6 | 1.8 | ||
| Sexual Behavior | ||||||||||||
| All | ||||||||||||
| Ever had sex | <0.001 | 0.48 | ||||||||||
| No | 310 | 33.0 | 33 | 14.4 | 277 | 39.0 | 141 | 37.6 | 136 | 40.5 | ||
| Yes | 627 | 66.6 | 196 | 85.6 | 431 | 60.6 | 231 | 61.6 | 200 | 59.5 | ||
| Missing data | 3 | 0.3 | 0 | 0 | 3 | 0.4 | 3 | 0.8 | 0 | 0 | ||
| Among Sexually Experienced Youth | n=627 | n=196 | n=431 | n=231 | n=200 | |||||||
| Age at first intercourse | 0.21 | 0.35 | ||||||||||
| ≤13 years | 262 | 41.8 | 89 | 45.4 | 173 | 40.1 | 88 | 38.1 | 85 | 42.5 | ||
| >13 years | 359 | 57.3 | 105 | 53.6 | 254 | 58.9 | 141 | 61.0 | 113 | 56.5 | ||
| Missing data | 6 | 1.0 | 2 | 1.0 | 4 | 0.9 | 2 | 0.9 | 2 | 1.0 | ||
| Ever pregnant or gotten someone pregnant | <0.001 | |||||||||||
| No | 444 | 70.8 | 120 | 61.2 | 324 | 75.2 | 173 | 74.9 | 151 | 75.5 | ||
| Yes | 179 | 28.5 | 74 | 37.8 | 105 | 24.4 | 57 | 24.7 | 48 | 24.0 | ||
| Missing data | 4 | 0.6 | 2 | 1.0 | 2 | 0.5 | 1 | 0.4 | 1 | 0.5 | ||
| Had sex in past 3 months | 0.17 | 0.55 | ||||||||||
| No | 163 | 26.0 | 44 | 22.4 | 119 | 27.6 | 61 | 26.4 | 58 | 29.0 | ||
| Yes | 464 | 74.0 | 152 | 77.6 | 312 | 72.4 | 170 | 73.6 | 142 | 71.0 | ||
| Among Sexually Active in the Last 3 Months | n=464 | n=152 | n=312 | n=170 | n=142 | |||||||
| Any unprotected occasions in last 3 months | 0.38 | 0.18 | ||||||||||
| No | 189 | 40.7 | 58 | 38.2 | 131 | 42.0 | 78 | 45.9 | 53 | 37.3 | ||
| Yes | 257 | 55.4 | 89 | 58.6 | 168 | 53.9 | 87 | 51.2 | 81 | 57.0 | ||
| Missing data | 18 | 4.9 | 5 | 3.3 | 13 | 4.2 | 5 | 2.9 | 8 | 5.6 | ||
| Any unprotected partners in last 3 months | 0.15 | 0.40 | ||||||||||
| No | 202 | 43.5 | 58 | 38.2 | 144 | 46.2 | 82 | 48.2 | 62 | 43.7 | ||
| Yes | 254 | 54.7 | 89 | 58.6 | 165 | 52.9 | 86 | 50.6 | 79 | 55.6 | ||
| Missing data | 8 | 1.7 | 5 | 3.3 | 3 | 1.0 | 2 | 1.2 | 1 | 0.7 | ||
| Used drugs before sexual intercourse | 0.04 | 0.46 | ||||||||||
| No | 319 | 68.8 | 95 | 62.5 | 224 | 71.8 | 125 | 73.5 | 99 | 69.7 | ||
| Yes | 145 | 31.3 | 57 | 37.5 | 88 | 28.2 | 45 | 26.5 | 43 | 30.3 | ||
| Drug Behavior | ||||||||||||
| Marijuana use in last 30 days | <0.001 | 0.78 | ||||||||||
| No | 677 | 72.0 | 138 | 60.3 | 539 | 75.8 | 286 | 76.3 | 253 | 75.3 | ||
| Yes | 253 | 26.9 | 89 | 38.9 | 164 | 23.1 | 85 | 22.7 | 79 | 23.5 | ||
| Missing data | 10 | 1.1 | 2 | 0.9 | 8 | 1.1 | 4 | 1.1 | 4 | 1.2 | ||
| Cocaine use in last 30 days | 0.01 | 0.92 | ||||||||||
| No | 876 | 93.2 | 202 | 88.2 | 674 | 94.8 | 358 | 95.5 | 316 | 94.0 | ||
| Yes | 40 | 4.3 | 16 | 7.0 | 24 | 3.4 | 13 | 3.5 | 11 | 3.3 | ||
| Missing data | 24 | 2.6 | 11 | 4.8 | 13 | 1.8 | 4 | 1.1 | 9 | 2.7 | ||
| Codeine use in last 30 days | <0.001 | 0.78 | ||||||||||
| No | 851 | 90.5 | 189 | 82.5 | 662 | 93.1 | 348 | 92.8 | 314 | 93.5 | ||
| Yes | 80 | 8.5 | 38 | 16.6 | 42 | 5.9 | 23 | 6.1 | 19 | 5.7 | ||
| Missing data | 9 | 1.0 | 2 | 0.9 | 7 | 1.0 | 4 | 1.1 | 3 | 0.9 | ||
Note: Percentages may not add up to 100 due to rounding.
Table 3.
Baseline Psychosocial Data for All Students, for Those Excluded from Study Cohort, and for Those Included in Study Cohort
| All Students (n=940) |
Excluded from Study Cohort (n = 229) |
Included in Study Cohort (n = 711) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Psychosocial | n | Mean | SD | n | Mean | SD | n | Mean | SD | T-test p-value | Scale Range |
| Attitudes | |||||||||||
| Sexual intercourse | 929 | 1.72 | 0.86 | 223 | 1.51 | 0.85 | 706 | 1.79 | 0.85 | <0.001 | (0,3) |
| Condoms | 929 | 2.62 | 0.58 | 225 | 2.54 | 0.64 | 704 | 2.65 | 0.55 | 0.03 | (0,3) |
| Knowledge | |||||||||||
| HIV | 931 | 2.18 | 1.06 | 226 | 2.28 | 1.04 | 705 | 2.15 | 1.07 | 0.11 | (0,4) |
| Other STDs | 932 | 3.04 | 1.59 | 226 | 3.23 | 1.58 | 706 | 2.98 | 1.59 | 0.04 | (0,5) |
| Normative beliefs | |||||||||||
| Sexual intercourse | 929 | 1.20 | 0.86 | 224 | 1.10 | 0.76 | 705 | 1.23 | 0.88 | 0.04 | (0,3) |
| Condoms | 925 | 2.18 | 0.79 | 225 | 2.14 | 0.85 | 700 | 2.19 | 0.77 | 0.36 | (0,3) |
| Self-efficacy | |||||||||||
| Refusing sex | 923 | 1.47 | 0.58 | 225 | 1.37 | 0.62 | 698 | 1.50 | 0.56 | 0.004 | (0,2) |
| Condoms | 925 | 1.41 | 0.59 | 224 | 1.54 | 0.53 | 701 | 1.36 | 0.61 | <0.001 | (0,2) |
| Communication | 923 | 1.79 | 0.38 | 223 | 1.78 | 0.38 | 700 | 1.79 | 0.38 | 0.97 | (0,2) |
| Perceived barriers to condom use | 929 | 1.03 | 0.96 | 226 | 0.81 | 0.88 | 703 | 1.09 | 0.97 | <0.001 | (0,3) |
Note: All psychosocial scales represent an average except for Knowledge, which is a sum.
Those who were excluded from the study cohort did not differ by race/ethnicity, by the grades they made in school, or by the educational level of their parents from those included. There were significant differences by gender and age: of the 401 boys initially enrolled in the study, 113 (28%) were not enrolled at the spring semester, whereas of the 539 girls initially enrolled, 116 (22%) were not enrolled at the end of spring semester. As a result, the included and excluded groups had different gender ratios (p<.02). Older students were significantly more likely to not be still enrolled by the end of the spring semester than younger students: 28% of excluded students were 18 or more years of age compared to 16% of students included. In contrast, 5% of excluded students were 13 years of age or younger while 14% of students in the included group were in that age group.
In examining sexual behavior of those who were included in the study cohort compared to those who were excluded, those who were excluded from the study had higher levels of ever having sexual intercourse (85.6% vs. 60.6%). No differences were observed with regard to age at first intercourse, proportion having sexual intercourse in the last 3 months, or proportion consistently using condoms. However, those who were excluded from the study were more likely to have been pregnant or have gotten someone pregnant (37.8% vs. 24.4%), to have reported using drugs before sexual intercourse (37.5% vs. 28.3%), and to report using marijuana, cocaine, or codeine in the past 30 days.
Those who were included in the study cohort had more positive attitudes about delaying sexual intercourse and using condoms, but had significantly less knowledge about sexually transmitted infections. Students who were enrolled in the study cohort reported more confidence in refusing sex, but less confidence in using a condom during sex, while at the same time identifying more barriers to using condoms than those who were dropped from the study. Those included in the study believed it was more normative to have sexual intercourse. No difference in the 2 groups were seen in knowledge, normative beliefs in using condoms, or in self-efficacy in communicating about sex to their partners.
Of the students enrolled in the study cohort, no differences by intervention and control status were observed in demographic factors including ethnicity, gender, age, grades in schools, and family education. In addition no differences in sexual risk-taking variables, such as age at first intercourse, ever having sexual intercourse, being currently sexually active, and consistent condom use, were seen between intervention and control groups. Further, no differences between the intervention and control groups were seen for drug use or for the psychosocial variables.
Table 4 shows the one significant difference in the baseline demographic and behavioral data and in the baseline psychosocial data for those who were excluded from the study cohort, by intervention and control group. There were no significant differences in demographic characteristics, in whether or not those in the group were sexually experienced, in the sexual behaviors of those currently sexually active, in their recent drug use, or in their psychosocial impact variables. The only significant difference between the two group was in the age at first intercourse: those excluded from the control group were much more likely to report their first intercourse as having been at age 13 or younger (55.9%) compared to those who were excluded from the intervention group (31.8%).
Table 4.
Significant Differences in Baseline Demographic and Behavioral Data for Those Excluded from the Study Cohort, by Intervention and Control Groups
| Excluded from Intervention (n = 100) |
Excluded from Control (n = 129) |
||||
|---|---|---|---|---|---|
| Demographics | n | % | n | % | Chi-square p-value |
| Among Sexually Experienced Youth | n = 85 | n = 111 | |||
| Age at first intercourse | <0.001 | ||||
| ≤13 years | 27 | 31.8 | 62 | 55.9 | |
| >13 years | 57 | 67.1 | 48 | 43.2 | |
| Missing data | 1 | 1.2 | 1 | 0.9 | |
Note: Percentages may not add up to 100 due to rounding.
8. Discussion
This paper addresses design and methodological issues in conducting school-based intervention research in alternative schools, including the feasibility of using a cross-over design for conducting school-based research and the definition of the cohort for follow-up evaluation. Baseline results suggest that this alternative school population is a predominantly minority population with parents who are not well educated. The majority are sexually active and many are not consistently using a condom during sexual intercourse. Many have initiated sexual intercourse at an early age, and one-fourth of those sexually experienced reported a history of pregnancy or getting someone pregnant. Another risk factor in this population is the high prevalence of reported drug use: one quarter of the students reported using marijuana in the past 30 days, 2.3% reported cocaine use, and 8.5% reported codeine use during this time period. These students are at much higher risk for sexual risk-taking than students who attend regular high schools. For example, compared to national data of students attending regular high schools [17], more of these alternative school students report ever having sex than regular high school students (66.6% vs. 49.9%), being currently sexually active (49.4% vs. 36.3%) and reporting ever being pregnant or getting someone pregnant (19.0% vs. 6.3%).
In our study population, we lost 24% of the students between baseline and the first follow-up. Anticipating the attendance and dropout problem, we chose a priori to define our cohort for the intervention trial as students who were enrolled at first follow-up. This was the only way to ensure that the intervention group would have some exposure to the intervention and that the definition of the cohort was compatible for both intervention and comparison groups. Accordingly, the cohort we are following for the entire study presents some selection bias in that they display less risky behaviors than students who were not enrolled at first follow-up. Students who were excluded from the study were more likely to be older, male, to report ever having sexual intercourse, and to use drugs. These students were also more likely to have less positive attitudes toward waiting to have sex and toward using condoms and to report fewer barriers to using a condom use. In addition those who were excluded from the study cohort had greater self-efficacy for using a condom, but less self-efficacy for refusing sex. We found no differences in those who were dropped from the study and those followed in race/ethnicity, parental education, being currently sexually active, or in using a condom. Consequently researchers should be aware of the selection bias [31] that may be operating in these types of studies, and intervention strategies designed to target the extremely hard-to-reach populations should be designed. Such strategies could include a more intensive approach such as the full-day sessions used by other researchers [32]. Despite the inherent selection bias in these types of studies, the examined population that is being followed still represents a high-risk population deserving of interventions and assessment.
We used a group-randomized study with a crossover design. This type of design deals with several limitations in evaluating interventions among alternative schools and similar settings while maintaining a rigorous research design. These design challenges included the limited number of schools available to randomize and the variations in school size, composition, and enrollment criteria. By evaluating the same schools at different times in the presence and the absence of the intervention, the variability among schools in the composition of the student population should not blur true differences in the efficacy of the intervention. We tested the feasibility of using a cross-over design in assuring comparable intervention and comparison groups. No differences in intervention and comparison schools were observed in demographic factors, behavioral factors, or psychosocial factors, providing evidence that the cross-over design can provide good balance between groups. This experimental design will provide a rigorous test of the intervention. The balance in baseline variables between the intervention and comparison conditions will help provide assurance that the trial’s intervention effectiveness results will be unbiased.
8.1 Limitations
A possible limitation is this type of crossover design is the potential for overlapping cluster membership. This could be a particular problem in school-based trials since students could enroll in different schools in successive years or alternately, they could remain in the same school and be subsequently randomized to a different condition. We dealt with this issue by excluding students who were already randomized in the first year of the study.
Another limitation of this study is that the students recruited to the study may not be representative of the target population. Because alternative school students are difficult to recruit and because these students were willing to obtain parental consent and to be randomized, they probably have some differences with the overall target population.
The effects of recruitment and measurement of Wave 1 and Wave 2 students at a one year interval could introduce two biases: 1) environmental or normative changes could be introduced during the one-year time intervalng that time period; and 2) while study staff and students were masked as to the treatment assignment of schools during Wave 1 recruitment and data collection, during Wave 2, study staff were aware of treatment conditions of the schools. These potential biases were addressed by examining baseline characteristics of Wave 1 and Wave 2 cohorts. No significant differences in demographic or behavioral characteristics were found when these comparisons were made
8.2 Conclusions
This paper demonstrates the need to intervene among high-risk youth attending alternative schools; however, studies should take into consideration special considerations of this high-risk, highly mobile population. This paper also demonstrates the feasibility of using a crossover design for a group-randomized trial. This design was feasible, efficient, and produced balanced groups in whom to evaluate the effectiveness of the intervention. This type of study design could be considered in other school or community settings where a limited number of units are available for randomization.
Acknowledgments
Funding source: NIH, National Institute of Child Health and Human Development, #R01 HD 38457-02.
The authors would like to thank Dr. Ralph Frankowski for his significant input into the study design and Karyn Popham for her editorial assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Weinstock H, Berman S, Cates W., Jr Sexually transmitted diseases among American youth: incidence and prevalence estimates. Perspectives on Sexual and Reproductive Health. 2000;36(1):6–10. doi: 10.1363/psrh.36.6.04. Last updated: 2004. Available: < http://www.guttmacher.org/pubs/journals/3600604.html>. [DOI] [PubMed]
- 2.DiLorenzo TA, Abramo DM, Hein K, et al. The evaluation of targeted outreach in an adolescent HIV/AIDS program. J Adolesc Health. 1993;14(4):301–306. doi: 10.1016/1054-139x(93)90178-r. [DOI] [PubMed] [Google Scholar]
- 3.Jemmott JB, III, Jemmott LS, Fong GT. Reductions in HIV risk-associated sexual behaviors among black male adolescents: Effects of an AIDS prevention intervention. Am J Public Health. 1992;82(3):372–377. doi: 10.2105/ajph.82.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacKay AP, Fingerhut LA, Duran CR. Health, United States, 2000 . DHHS Publication No. (PHS) 2000-1232-1. Hyattsville, MD: National Center for Health Statistics; 2000. Jul, Adolescent Health Chartbook. [Google Scholar]
- 5.National Institutes of Health. National Institute of Allergy and Infectious Diseases. HIV Infection in Adolescents and Young Adults in the U.S. fact sheet. 4 Last updated: 2005 Jul. Available: < http://www.niaid.nih.gov/factsheets/hivadolescent.htm>.
- 6.Kirby D. Emerging Answers: Research finding on programs to reduce teen pregnancy. Washington, DC: National Campaign to Prevent Teen Pregnancy; 2001. [Google Scholar]
- 7.Coyle K, Basen-Engquist K, Kirby D, et al. Safer Choices: Reducing teen pregnancy, HIV, and STDs. Public Health Rep. 2001;116(Suppl 1):82–93. doi: 10.1093/phr/116.S1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hubbard BM, Giese ML, Rainey J. A replication study of Reducing the Risk, a theory-based sexuality curriculum for adolescents. J Sch Health. 1998;68(6):243–247. doi: 10.1111/j.1746-1561.1998.tb06347.x. [DOI] [PubMed] [Google Scholar]
- 9.Kirby D, Barth RP, Leland N, Fetro JV. Reducing the risk: Impact of a new curriculum on sexual risk-taking. Fam Plann Perspect. 1991;23(6):253–263. [PubMed] [Google Scholar]
- 10.Main DS, Iverson DC, McGloin J, et al. Preventing HIV infection among adolescents: evaluation of a school-based education program. Prev Med. 1994;23(4):409–417. doi: 10.1006/pmed.1994.1056. [DOI] [PubMed] [Google Scholar]
- 11.Walter HJ, Vaughan RD. AIDS risk reduction among a multiethnic sample of urban high school students. JAMA. 1993;11(270):725–730. [PubMed] [Google Scholar]
- 12.Jemmott JB, III, Jemmott LS. HIV risk reduction behavioral interventions with heterosexual adolescents. AIDS (London) 2000;14(Suppl 2):s40–s52. [PubMed] [Google Scholar]
- 13.Grunbaum JA, Kann L, Kinchen SA, et al. Youth Risk Behavior Surveillance. National Alternative High School Youth Risk Behavior Survey, United States, 1998. J Sch Health. 2000;70(1):5–17. doi: 10.1111/j.1746-1561.2000.tb06439.x. [DOI] [PubMed] [Google Scholar]
- 14.Markham CM, Tortolero SR, Escobar-Chaves SL, et al. Family connectedness and sexual risk-taking among urban youth attending alternative high schools. Perspect Sex Reprod Health. 2003;35(4):174–179. doi: 10.1363/psrh.35.174.03. [DOI] [PubMed] [Google Scholar]
- 15.Buzi RS, Tortolero SR, Roberts RE, et al. The impact of a history of sexual abuse on high-risk sexual behaviors among females attending alternative schools. Adolescence. 2003;38(152):595–605. [PubMed] [Google Scholar]
- 16.Weller NF, Tortolero SR, Kelder SH, et al. Health risk behaviors of Texas students attending dropout prevention/recovery schools in 1997. J Sch Health. 1999;69(1):22–28. doi: 10.1111/j.1746-1561.1999.tb02338.x. [DOI] [PubMed] [Google Scholar]
- 17.Kann L, Kinchen SA, Williams BI, Ross JG, Lowry R, Grunbaum JA, Kolbe LJ. State and local YRBSS Coordinators. Youth Risk Behavior Surveillance--United States, 1999. MMWR Surveillance Summaries. 49(SS5):1–96. Last updated: 2000 Jun 9 [cited 2006 May 10]. Available: < http://www.cdc.gov/mmwr/PDF/SS/SS4905.pdf>.
- 18.Tortolero SR, Markham CM, Parcel GS, et al. Using Intervention Mapping to adapt an effective HIV, sexually transmitted disease, and pregnancy prevention program for high-risk minority youth. Health Promot Pract. 2005;6(3):286–298. doi: 10.1177/1524839904266472. [DOI] [PubMed] [Google Scholar]
- 19.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 20.Murray DM. Design and analysis of group randomized trials. New York: Oxford University Press; 1998. [Google Scholar]
- 21.Kish JL. Survey Sampling. NY: John Wiley; 1965. [Google Scholar]
- 22.Graham JW, Flay BR, Johnson CA, Hansen WB, Collins LM. Group comparability: A multiattribute utility measurement approach to the use of random assignment with small numbers of aggregated units. Eval Rev. 1984;8(1):247–260. [Google Scholar]
- 23.Gwadz M, Rotheram-Borus MJ. Tracking high-risk adolescents longitudinally. AIDS Educ Prev. 1992;(Suppl):69–82. [PubMed] [Google Scholar]
- 24.Perlis TE, Des Jarlais DC, Friedman SR, Arasteh K, Turner CF. Audio-computerized self-interviewing versus face-to-face interviewing for research data collection at drug abuse treatment programs. Addiction. 2004;99(7):885–896. doi: 10.1111/j.1360-0443.2004.00740.x. [DOI] [PubMed] [Google Scholar]
- 25.Ellen JM, Gurvey JE, Pasch L, et al. A randomized comparison of A-CASI and phone interviews to assess STD/HIV-related risk behaviors in teens. J Adolesc Health. 2002;31(1):26–30. doi: 10.1016/s1054-139x(01)00404-9. [DOI] [PubMed] [Google Scholar]
- 26.Jennings TE, Lucenko BA, Malow RM, Devieux JG. Audio-CASI vs interview method of administration of an HIV/STD risk of exposure screening instrument for teenagers. Int J STD AIDS. 2002;13(11):781–784. doi: 10.1258/095646202320753754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Des Jarlais DC, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353(9165):1657–1661. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- 28.Turner CF, Ku L, Rogers SM, et al. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 29.Lessler JT, O’Reilly JM. Mode of interview and reporting of sensitive issues: Design and implementation of audio computer-assisted self-interviewing. NIDA Research Monograph. 167:366–382. (The Validity of Self-Reported Drug Use: Improving the Accuracy of Survey Estimates) Last updated: 1997. Available: < http://www.drugabuse.gov/pdf/monographs/monograph167/download167.html>. [PubMed]
- 30.Basen-Engquist K, Masse LC, Coyle K, et al. Validity of scales measuring the psychosocial determinants of HIV/STD-related risk behavior in adolescents. Health Educ Res. 1999;14(1):25–38. doi: 10.1093/her/14.1.25. [DOI] [PubMed] [Google Scholar]
- 31.Green SB. Design of randomized trials. Epidemiol Rev. 2002;24(1):4–11. doi: 10.1093/epirev/24.1.4. [DOI] [PubMed] [Google Scholar]
- 32.Jemmott JB, III, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: A randomized controlled trial. Arch Pediatr Adolesc Med. 2005;159(5):440–449. doi: 10.1001/archpedi.159.5.440. [DOI] [PubMed] [Google Scholar]