Abstract
Revision after failed THA resulting from loosening of the femoral component can be challenging even for experienced surgeons. Aseptic loosening usually is associated with some degree of bone loss. We asked whether the Zweymüller SLR-Plus®, along with allograft reconstruction of the deficient femoral bone stock, would provide survivorship, osseointegration, and stability similar to or better than previously reported implants for femoral revision. We retrospectively reviewed 69 selected patients (70 hips) who underwent revision of the femoral component using the SLR-Plus® stem during a 10-year period. The indications for revision included aseptic and septic failure of biologic fixation, incorrect implantation, and periprosthetic fracture. Seven patients died and four were lost to followup. Fifty-eight of the 69 patients (59 hips) were available at a mean 8.3 ± 2.7 years (range, 4–14 years) after revision surgery. There were 14 men and 44 women (mean age, 69 years; range, 42–89 years). Four stems (7%) were rerevised. With rerevision for aseptic reasons, the survival at 10 years was 95% (95% confidence interval, 86%–98%). No femoral periprosthetic osteolysis occurred around the stem and 91% of stems appeared stable radiographically (osseointegration, fibrous). Based on the survival data, we believe the SLR-Plus® stems are reliable for patients undergoing hip revision surgery with central bone loss.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Revision after failed THA resulting from loosening of the femoral component can be challenging even for experienced surgeons [11, 26, 33, 44]. Aseptic loosening is the reason for revision in approximately 70% to 80% of patients [7] and usually is associated with some degree of bone loss [39]. Additionally, removal of a long cemented or uncemented stem often can result in damage to the femur. Various cemented and cementless techniques have been developed to address this issue. The amount of bone loss dictates the type of revision stem, the need for grafting, and the operative technique.
In revision surgery, fixation of a cemented femoral component is poor compared with that of a primary component [2, 3]. The results using early cementing techniques in femoral revision procedures were not encouraging (9% rerevision rate, 20% progressive radiolucencies at 1 to 10 years after surgery) [1, 7, 22, 27, 36, 43, 50], although second-generation cementing techniques have decreased the failure rate of revision stems to approximately 10% at 10 years and 15% to 20% at 15 years [15, 25, 27, 45]. However, it often is impossible to cement a prosthesis and achieve adequate fixation with proximal bony defects owing to the difficulty achieving macrointerlock of the polymethylmethacrylate with cancellous bone [12]. Cemented components used in revisions for femoral loosening have a high incidence of radiographic loosening when the revision does not include reconstruction of the deficient bone stock [2, 4, 5].
Impaction grafting along with allograft are the most widely used techniques to reconstruct the deficient proximal metaphysis of the femur. However, when the proximal femur is considerably compromised, fractured, or absent, prosthetic stabilization distal to the area of weakened bone is necessary for successful reconstruction [7, 16].
The Zweymüller SLR-Plus® stem (Smith and Nephew, Inc, Memphis, TN) (Fig. 1) was introduced as a design modification of the uncemented Zweymüller SL-Plus® stem to accommodate proximally located bony defects and provide enhanced load transfer from the proximal to the distal femur, allowing simultaneous incorporation of the proximally applied grafts on the porous-coated stem surface [21, 55]. Although the Zweymüller SL-Plus® stem has been used since 1992, to our knowledge, there is only one article reporting short-term outcome [36].
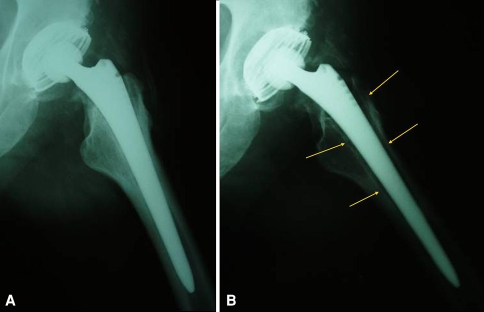
Fig. 1.

The Zweymüller SLR-Plus® cementless titanium stem for femoral revision has a dual-tapered rectangular shape that addresses the issue of initial secure axial positioning and rotational stability and is available in lengths of 181 to 227 mm.
The objectives of our study were to evaluate (1) survivorship, (2) osseointegration, and (3) stability of the Zweymüller SLR-Plus® stem in revision surgery in selected patients during an average 8-year period.
Materials and Methods
We retrospectively reviewed 69 selected patients (70 hips) who underwent revision of the femoral component using the Zweymüller SLR-Plus® stem between August 1994 and August 2004. During that same time, we performed 167 cementless stem revisions using the SL-Plus® (89), SLR-Plus® (70), and Modular-Plus® (eight) stems. The selection criteria for SLR-Plus® stem selection were an isthmus with sufficient femoral cortex thickness (mandatory for distal anchorage of this stem) and bone stock loss of different degree and location. We made the decision regarding the type of stem preoperatively with the use of templates provided by the manufacturer, and in no case was it necessary to change our decision intraoperatively. Seven patients died and four were lost to followup at an average 6.3 and 3.5 years, respectively, after SLR-Plus® stem implantation. The remaining 58 patients (59 hips), 44 women and 14 men with a mean age of 69 years (range, 42–89 years), were followed for a minimum of 4 years (mean, 8.3 years; range, 4–14 years).
Nineteen revised hips (18 patients) involved replacement of a cemented stem and 40 involved a cementless stem. Revision surgery was performed an average 8.7 years (range, 0.3–25 years) after previous implantation. Femoral and acetabular components were revised in 36 hips (35 patients), whereas only the stem was revised in 23 hips (23 patients). The indication for revision surgery of the stem was aseptic loosening in 47 hips (78%; 46 patients), dislocation resulting from incorrect stem implantation in two hips (3%; two patients), periprosthetic femoral fracture in six hips (10%; six patients), and septic loosening in four hips (7%; four patients). For 50 hips, it was the first revision, whereas it was the second in eight hips and the third in one hip. The SLR-Plus® stem is made of a titanium-aluminum-niobium alloy (Ti-6Al-7Nb), which is highly biocompatible and features elasticity that more closely matches bone than other materials. The entire stem is precision grit-blasted to create a uniform 4- to 6-μm surface roughness, which enhances bone apposition to the stem, providing increased secondary stability (Fig. 1). The shaft of the prosthesis has a dual-tapered rectangular shape that provides initial secure axial positioning and rotational stability (Fig. 1); it is available in lengths of 181 to 227 mm. Cementless anchoring of the stem is achieved after press-fit implantation in a previously broached femoral shaft. If there are large defects, as often are seen after cemented THAs, in the proximal part of the femur, stable fixation of the stem is achieved by distal anchorage in the cortical diaphyseal part of the femur. The rectangular cross-sectional shape of the stem contributes to this immediate axial and rotational stability.
Before surgery, all patients underwent templating to determine the appropriate length and diameter of revision stems and to assess adequacy of host bone stock and the possible need for allograft augmentation. We obtained plain anteroposterior (AP) and lateral views of the hip and femur and CT scans, if needed, for preoperative planning and followup. We classified preoperative femoral bony defects according to the American Academy of Orthopaedic Surgeons Committee on the Hip system [10] as follows: 45 Type II, six Type III, one Type IV, one Type V, and six Type VI. Overall, 31% of the preoperative femoral defects were limited to Level I (lesser trochanter), 56% had cortical damage extending to Level II (< 10 cm below the lesser trochanter), and 14% had cortical damage extending to Level III (> 10 cm below the lesser trochanter).
All surgeries were performed by the senior surgeon (PK). We used a modified anterolateral Watson-Jones approach in all operations. Tissue samples for histologic analysis and cultures and Gram stain were routinely obtained. The femoral cavity then was cleaned meticulously and subsequently broaching of the femoral canal was performed to avoid cracks and fractures. Although preoperative manual templating identified the approximate (± 1 size) stem size, the actual size was based on intraoperatively achieved stability findings and femoral anatomy. We securely fixed the stem when it stopped advancing and manually tested it for rotational stability. Ceramic ball heads (28 mm) were used in 43 hips paired with a polyethylene socket and metal ball heads (28-mm metal-on-metal articulating surface) in 16 hips. Femoral bone cavities were filled immediately before and during insertion of the stem with autologous iliac bone graft (seven hips), allogeneic cancellous chips, demineralized bone matrix (Regeneration Technologies, Inc, Alachua, FL), or mixed grafts (50 hips). In two hips, we used structural strut femoral allografts to reinforce the proximal femoral bone weakened by osteolysis. In all 58 patients (59 hips), we used titanium Compression Cerclage Gundolf (CCG®) bands (Smith and Nephew) [30] to fix remnants of the proximal femur or fractured femur to the stem.
Postoperative mobilization depended on primary stability of the femoral reconstruction and the cooperation and ability of the patients to use crutches. Physiotherapy started on the first postoperative day with active muscle training. Partial (15–20 kg) weightbearing started on Day 2 postoperatively under the supervision of a physiotherapist twice per day. After 2 to 4 months postoperatively, patients were advised to progress without ambulatory aids. Patients were discharged after a mean of 18 days (range, 14–26 days).
Clinical evaluation of the patients was performed at 3 and 6 months postoperatively and annually thereafter by one orthopaedic surgeon (TR) who did not participate in the surgery. Pain, range of motion of the hip, and any leg length discrepancy were recorded. We used the Harris hip score (HHS) [19] for preoperative and postoperative functional evaluations of the patients. We also used the SF-36 Health Survey [9] with eight domains preoperatively and at the last evaluation.
Standardized AP supine radiographs of the pelvis and AP and lateral supine radiographs of the hip and femur, taken immediately postoperatively (AP only), 3 and 6 months postoperatively (AP and lateral), and annually thereafter, were used to assess position of the implant restoration of the proximal part of the femur and implant stability immediately after implantation to the last evaluation. A senior orthopaedic radiologist (PI) performed the preoperative radiographic evaluation (staging) of the femoral defects and assessed implant stability by comparing the last postoperative radiographs with those obtained immediately after surgery. Any progression of preexisting periprosthetic osteolysis by more than 2 mm was recorded digitally with the DiagnosticPRO™ Advantage (VIDAR Systems Corp, Herndon, VA) in the 14 zones around the stem described by Gruen et al. [17]. We measured stem axial subsidence using bone-prosthetic landmarks on comparison radiographs; the distance between the lesser trochanter and the tip of the prosthesis was used in the majority of the patients. Focal osteolysis [54] appeared as a sharply demarcated radiolucent space with a rounded or scalloped appearance greater than 2 mm wide. Osteolytic areas and radiolucencies adjacent to the stem were recorded according to the Gruen zones [17]. Definite radiographic loosening of the stem was defined as axial subsidence greater than 2 mm, new varus inclination of the stem greater than 3°, continuous new radiolucent lines greater than 2 mm, or progression of preexisting radiolucencies greater than 2 mm in more than two adjacent Gruen zones [31]. We radiographically classified femoral implant stability of the nonrevised stems according to the criteria of Engh et al. [13] as stable through osseointegration, fibrous stable, and unstable.
We performed survival analysis for all patients using the Kaplan-Meier method [24], using removal of the stem because of aseptic loosening and removal of the stem for any cause as failure criteria. A worst-case survival curve counting patients lost to followup as having failed results also was included. Hips at risk at different times after surgery also were calculated. All survivorship data were reported with 95% confidence intervals (CIs).
Results
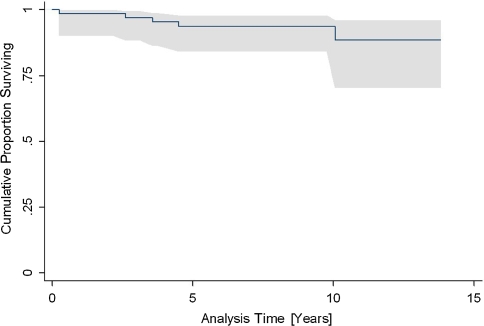
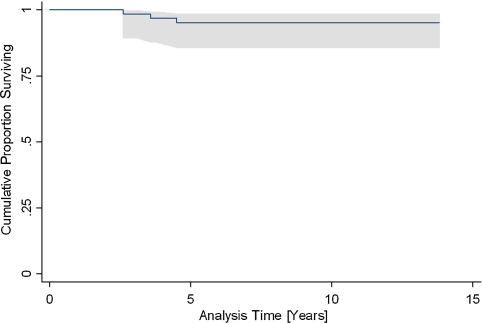
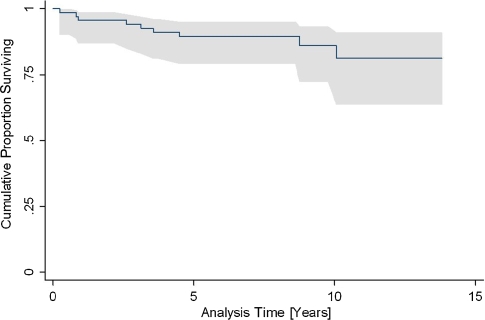
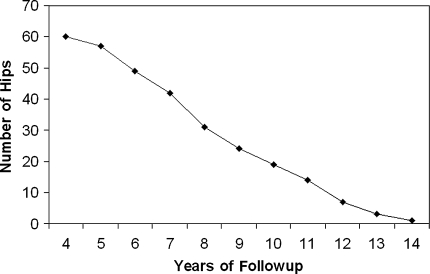
The survivorship at 10 years was 94% (95% CI, 84%–98%) with removal of the stem for any cause as the end point (Fig. 2), 95% (95% CI, 86%–98%) with removal of the stem for aseptic loosening as the end point (Fig. 3), and 86% (95% CI, 72%–93%) with removal of the stem and lost to followup as the worst-case scenario (Fig. 4). The number of hips at risk for aseptic loosening decreased from 60 hips at 4 years postoperatively to 19 hips at 10 years postoperatively (Fig. 5). Four stems (7%) were rerevised, two for aseptic loss of biologic fixation, one for recurrent dislocation, and one for deep infection.
Fig. 2.
The survivorship of the SLR-Plus® stem at 10 years according to the Kaplan-Meier method is 94% (95% CI, 84%–98%) with removal of the stem for any cause as the end point.
Fig. 3.
The survivorship of the SLR-Plus® stem at 10 years according to the Kaplan-Meier method increases to 95% (95% CI, 86%–98%) with removal of the stem resulting from aseptic loosening as the end point.
Fig. 4.
The survivorship of the SLR-Plus® stem at 10 years according to the Kaplan-Meier method decreases to 86% (95% CI, 72%–93%) with the worst-case scenario (removal of the stem and counting patients lost to followup as having failed results) as the end point.
Fig. 5.
This graph shows the number of hips at risk at each interval.
We observed no focal osteolysis around the stem at last evaluation. The number of hips without radiolucencies around the stem increased from 23 (39%) immediately postoperatively to 32 (54%) at the latest followup. Furthermore, the number of hips with radiolucencies greater than 2 mm decreased from 28 (48%) immediately postoperatively to 15 (25%) at the last followup. Postoperative radiolucencies greater than 2 mm were seen proximally in Gruen Zone 1 (25%), Zone 7 (21%), Zone 8 (20%), and Zone 14 (21%) of the hips. This pattern of radiolucency topography did not change at the latest followup, although percentages were lower (13% in Zone 1, 10% in Zone 7, 13% in Zone 8, 13% in Zone 14).
Fifty-four (91%) stems were radiographically stable at the last evaluation. Forty-eight hips (81%) had radiographic evidence of bone ingrowth and six (10%) had stable fibrous fixation of the stem. At an average of 5 years after surgery, three stems (5%) were recorded as radiographically unstable associated with distal axial subsidence (3–5 mm) and thigh pain (Fig. 6). Two of these unstable stems (3%) were rerevised. During revision surgery, failure of biologic fixation of the stem was evident in both hips. The remaining two hips were revised at an early stage owing to deep infection and recurrent dislocation, respectively, and therefore were not included in the last assessment of radiographic stability.
Fig. 6A–B.
(A) In this postoperative radiograph of an SLR-Plus® stem implanted in a 69 year old man, the stem is in full contact with the femoral canal. (B) After 31/2 years followup, loosening of the stem was evident. The arrows indicate the radiolucent areas around the proximal 2/3 of the stem.
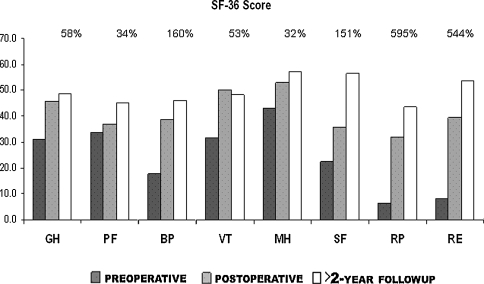
The HHS improved from an average preoperative value of 31.5 to 65.5 at the last postoperative evaluation. All eight domains of the SF-36 Health Survey improved at the latest followup (Fig. 7).
Fig. 7.
Results of the clinical evaluation according to the SF-36 Health Survey are shown in the graph. All eight domains of the SF-36 Health Survey were improved at the latest followup. The percentage of improvement is shown at the upper part of the graph. (GH = General Health; PF = Physical Functioning; BP = Bodily Pain; VT = Vitality; MH = Mental Health; SF = Social Functioning; RP = Role-Physical; RE = Role-Emotional).
Discussion
Proximal femoral bone stock deficiency after failed cemented and cementless THAs presents a challenge for hip surgeons. Restoration of bone stock is believed necessary for long-lasting results [3, 11, 42, 47]. There are various techniques for biologic reconstruction of the proximal part of the femur [3]. Our rationale was to enhance deficient proximal bone stock with autograft, allograft, and strut graft, providing simultaneous distal anchorage through the rectangular construction of the Zweymüller SLR-Plus® stem. The objectives of this study were to evaluate (1) survivorship, (2) osseointegration, and (3) stability of Zweymüller SLR-Plus® stems in revision surgery in selected patients during an average 8-year period.
Our study is limited by its relatively short minimum followup (4 years), relatively high percentage (16%) of patients who have surgery but who did not participate (either died or lost to followup) at the last evaluation, and the fact that we considered revision the definition of failure. Qualitative plain radiographic assessment of periprosthetic bone formation also presents, at least theoretically, a limitation affecting the variability of the method. Direct quantitative analysis of periprosthetic bone is not ethical (invasive techniques, biopsy) whereas dual-energy xray absorptiometry is not reliably applicable in the presence of metal stems. However, these limitations do not jeopardize the results of this study. The response rate was high for surveys of this type, and with a mean followup greater than 8 years, we can comment on midterm survival. A worst-case survival including not only revisions but also patients lost to followup was computed. All operations were performed by the senior surgeon always using the same operative technique, and data were collected and evaluated in an independent blind manner. The absence of focal osteolysis around the SLR-Plus® stem in combination with a decrease of hips with periprosthetic radiolucencies should, at least theoretically, be considered evidence for enhancement of osseointegration on the stem surface by bone graft and local bone remnants.
The 10-year survivorship for the SLR-Plus® stem (95%) in our series was greater than that reported with proximally porous-coated stems (74%–93%) [4, 38, 53], and within the reported survivorship range with the extensively coated chromium-cobalt stem (90.6%–97.7%) (Table 1) [14, 34]. The reported survival with the Wagner stem, which uses the philosophy of achieving initial stability through a long uncemented stem that bypasses the compromised proximal femur and gains fixation to the diaphysis, was 95.2% [6, 7, 18, 29] at 14.1 years (Table 1), comparable to survival for the SLR-Plus® stem, although our study includes selected cases and is not a consecutive series.
Table 1.
Cementless femoral revision
| Study | Type of femoral component | Fixation | Type of proximal bone defect | Age at surgery (average years) | Followup (years) | Survival (percent failure) |
|---|---|---|---|---|---|---|
| Head et al. [20] | Proximally porous coated | Proximal | III | 58 | 10 | 96 (3.2%) |
| Hedley et al. [21] | Harris-Galante | Proximal | 54 | 1.7 | (3%) | |
| Hungerford et al. [23] | Proximally porous coated | Proximal | Della Valle and Paprosky I–IV | 46 | 8.2 | 54.8% |
| Kim [28] | Proximally porous coated | Proximal | AAOS I–IV | 56.8 | 6.5 | 97 |
| Mulliken et al. [41] | Mallory Head | Proximal | Moderate to severe | 59 | 4.6 | (10%) |
| Walter et al. [51] | Porous-coated S-ROM | Proximal | Della Valle and Paprosky I–IIIb | 6 | (5%) | |
| Van Kleunen et al. [48] | Collared textured stems | Proximal | Massive (requiring greater than 150 cm3 allograft) | Minimum 2 | (5.6%) | |
| Paprosky et al. [42] | Extensively porous coated | Proximal and distal | 61.2 | 13.2 | (4.1%) | |
| Engh et al. [14] | Extensively porous coated | Proximal and distal | 29% less than 10 cm and 12% greater than 10 cm below the lesser trochanter | 15.0 | 95.8 | |
| Soteranos et al. [47] | Fully porous HA-coated | Distal screws | Della Valle and Paprosky IIIB–IV | 54 | 5.3 | 100 |
| Volkmann et al. [49] | BiCONTACT | Distal interlocking | 70% high grade | 5.3 | 85.3 | |
| Malhotra et al. [37] | IOTA interlocking | Distal interlocking | AAOS I–III | 57 | 3 | 100 |
| Schuh et al. [46] | Titanium MRP revision stem | Distal | 68 | 2.9 | (1%) | |
| Böhm and Bischel [7] | Wagner-SL | Distal | Pak classification | 65 | 8.1 | 95.2 |
| Grünig et al. [18] | Wagner-SL | Distal | 70 | 3.9 | (10%) | |
| Kolstad et al. [29] | Wagner-SL | Distal | 2.8 | (16%) | ||
| Weber et al. [52] | Wagner-SL | Distal | 5.4 | (5%) | ||
| Loehr et al. [36] | Zweymüller-SLR | Distal | 66 | 3 | (3%) 9.3% subsidence | |
| Current study | Zweymüller-SLR-Plus | Distal | AAOS II–IV | 69 | 8.3 | 95 (6.8%) |
AAOS = American Academy of Orthopaedic Surgeons.
Similar to stability reported in studies of the Wagner stem implant [6, 7, 18, 29], we found a high percentage (90%) of the SLR-Plus® stems appeared radiographically stable [13] at the last evaluation. This stem shares with the SLR-Plus® stem the principle of obtaining an immediate tight fit and mechanical stability through diaphyseal fixation of a long titanium alloy stem with a rough-blasted surface. Subsidence of the SLR-Plus® stem occurred in 3% of the hips in our series, considerably lower than that reported with stems using proximal (23%–66%) [4, 38, 53] and distal fixation (8%) [18, 29]. In a previous study [36], it was reported 10% of the SLR-Plus® devices subsided at a mean of 3 years after surgery and 1% of the patients reported thigh pain. In our series, thigh pain was present only in two patients (two hips, 3%) in contrast to 16% to 38% reported with proximally porous-coated femoral components [4, 38, 42, 53].
The reported improvement of HHS after revision surgery in similar studies is, on average, 25 (from a preoperative average of 50 to an average of 75 at the last evaluation) [28, 37, 46]. The postoperative absolute value of HHS in our series was lower than that reported and this mainly should be the result of the increased average age of our patients. However, a postoperative increase of HHS of at least 20 is a well-accepted improvement [47]. Also, the self-assessment evaluation showed all SF-36 Health Survey domains improved at the latest followup. In particular, the Bodily Pain and Physical Functioning domains improved 160% and 35%, respectively.
Our patients had a lower rerevision rate (7%) with the cementless SLR-Plus® stem than that reported using even modern cementing techniques (9%–10%), with regression of radiolucencies in contrast to progression in cemented stems with comparable followup [1, 15, 22, 25–27, 43, 45]. Our rerevision rate for aseptic failure of biologic fixation (5%) was within that previously reported (2.4%–6%) in extensively proximally coated revision stems with comparable followup [32, 42] (Table 1).
Complications have been encountered during femoral revision surgeries (Table 2). In revision THA, intraoperative split fractures and cortical perforation are becoming a more common concern, ranging between 3.6% and 20.9% when cemented or uncemented prostheses are used, respectively [35]. This is often a consequence of attempting to obtain sufficient press-fit to gain initial stem stability [40]. In our series, implantation of the SLR-Plus® stem was associated with a low rate (1.4%) of intraoperative split femoral shaft fractures, which were fixed intraoperatively with CCG® titanium cerclage bands.
Table 2.
Complications
| Complication | Number of hips |
|---|---|
| Anterior dislocation | 5 (7%) |
| Deep infection | 1 (1.4%) |
| Periprosthetic femoral shaft fracture | 1 (1.4%) |
| Temporary sciatic nerve palsy | 1 (1.4%) |
| Heterotopic ossification [8] | 12 (17%) |
| Brooker III | 9 |
| Brooker IV | 3 |
Our data suggest (1) survivorship of the SLR-Plus® stem is comparable to that of other stems reported in studies involving revision surgery for deficient proximal femoral bone stock, (2) there was no periprosthetic osteolysis and a high rate of radiographic osseointegration of the stem, and (3) there was sufficient immediate and long-term stability. Our medium-term results are encouraging and similar to those reported in similar studies (comparable age and proximal bone defects) (Table 1). We believe the unique technique of SLR-Plus® stem implantation provides, under certain indications, improved initial rotational control and reduces the likelihood of subsidence of the stem, owing to its rectangular cross-sectional area. This immediate stability, at least theoretically, enhanced proximal bone graft incorporation, as suggested by the absence of osteolysis and reduction of periprosthetic radiolucencies. However, longer followup is needed to study the long-term survival of the SLR-Plus® stem in revision surgery.
Acknowledgments
We thank Panagiotis Iliopoulos, MD, PhD, for evaluating the hip radiographs and Petter Fennema for statistical and survivorship analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This paper is a part of the thesis of the resident Thomas Repantis, that is in progress at the University of Patras, Medical School, Greece.
Contributor Information
Panagiotis Korovessis, Phone: +30-2610-227202, FAX: +30-2610-227202, Email: korovess@otenet.gr.
Thomas Repantis, Email: tomrep@gmail.com.
References
- 1.Amstutz HC, Ma SM, Jinnah RH, Mai L. Revision of aseptic loose total hip arthroplasties. Clin Orthop Relat Res. 2004;420:2–9. [DOI] [PubMed]
- 2.Barnett E, Nordin BE. The radiological diagnosis of osteoporosis: a new approach. Clin Radiol. 1960;11:166–174. [DOI] [PubMed]
- 3.Barrack RL, Folgueras AJ. Revision total hip arthroplasty: the femoral component. J Am Acad Orthop Surg. 1995;3:79–85. [DOI] [PubMed]
- 4.Berry DJ. Femoral revision: distal fixation with fluted, tapered grit-blasted stems. J Arthroplasty. 2002;17(suppl 1):142–146. [DOI] [PubMed]
- 5.Berry DJ, Harmsen WS, Ilstrup D, Lewallen DG, Cabanela ME. Survivorship of uncemented proximally porous-coated femoral components. Clin Orthop Relat Res. 1995;319:168–177. [PubMed]
- 6.Böhm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 48 years. J Bone Joint Surg Am. 2001;83:1023–1031. [DOI] [PubMed]
- 7.Böhm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res. 2004;420:148–159. [DOI] [PubMed]
- 8.Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed]
- 9.Busija L, Osborne RH, Nilsdotter A, Buchbinder R, Roos EM. Magnitude and meaningfulness of change in SF-36 scores in four types of orthopedic surgery. Health Qual Life Outcomes. 2008;6:55. [DOI] [PMC free article] [PubMed]
- 10.D’Antonio J, McCarthy JC, Bargar WL, Borden LS, Cappelo WN, Collis DK, Steinberg ME, Wedge JH. Classification of femoral abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1993;296:133–139. [PubMed]
- 11.Della Valle CJ, Paprosky WG. The femur in revision total hip arthroplasty evaluation and classification. Clin Orthop Relat Res. 2004;420:55–62. [DOI] [PubMed]
- 12.Dohmae Y, Bechtold JE, Sherman RE, Puno RM, Gustilo RB. Reduction in cement-bone interface shear strength between primary and revision arthroplasty. Clin Orthop Relat Res. 1988;236:214–220. [PubMed]
- 13.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55. [DOI] [PubMed]
- 14.Engh CA Jr, Hopper RH Jr, Engh CA Sr. Distal ingrowth components. Clin Orthop Relat Res. 2004;420:135–141. [DOI] [PubMed]
- 15.Estok DM, Harris WH. Long-term results of cemented femoral revision surgery using second-generation techniques: an average 11.7-year follow-up evaluation. Clin Orthop Relat Res. 1994;299:190–202. [PubMed]
- 16.Gorab RS, Covino BM, Borden LS. The rationale for cementless revision total hip replacement with contemporary technology. Orthop Clin North Am. 1993;24:627–633. [PubMed]
- 17.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed]
- 18.Grünig R, Morscher E, Ochsner PE. Three- to 7-year results with the uncemented SL femoral revision prosthesis. Arch Orthop Trauma Surg. 1997;116:187–197. [DOI] [PubMed]
- 19.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end result study using a new method of results evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed]
- 20.Head WC, Malinin TI, Emerson RH Jr, Mallory TH. Restoration of bone stock in revision surgery of the femur. Int Orthop. 2000;24:9–14. [DOI] [PMC free article] [PubMed]
- 21.Hedley AK, Gruen TA, Ruoff DP. Revision of failed total hip arthroplasties with uncemented porous-coated anatomic components. Clin Orthop Relat Res. 1988;235:75–90. [PubMed]
- 22.Hungerford DS, Jones LC. The rationale of cementless revision of cemented arthroplasty failures. Clin Orthop Relat Res. 1988;235:12–24. [PubMed]
- 23.Hungerford MW, Hungerford DS, Khanuja HS, Pietryak BP, Jones LC. Survivorship of femoral revision hip arthroplasty in patients with osteonecrosis. J Bone Joint Surg Am. 2006;88(suppl 3):126–130. [DOI] [PubMed]
- 24.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [DOI]
- 25.Katz RP, Callaghan JJ, Sullivan PM, Johnston RC. Long-term results of revision total hip arthroplasty with improved cementing technique. J Bone Joint Surg Br. 1997;79:322–326. [DOI] [PubMed]
- 26.Kavanagh BF, Fitzgerald RH Jr. Multiple revisions for failed total hip arthroplasty not associated with infection. J Bone Joint Surg Am. 1987;69:1144–1149. [PubMed]
- 27.Kershaw CJ, Atkins RM, Dodd CA, Bulstrode CJ. Revision total hip arthroplasty for aseptic failure: a review of 276 cases. J Bone Joint Surg Br. 1991;73:564–568. [DOI] [PubMed]
- 28.Kim YH. Cementless revision hip arthroplasty using strut allografts and primary cementless proximal porous-coated prosthesis. J Arthroplasty. 2004;19:573–581. [DOI] [PubMed]
- 29.Kolstad K, Adalberth G, Mallmin H, Milbrink J, Sahlstedt B. The Wagner revision stem for severe osteolysis: 31 hips followed for 1.5–5 years. Acta Orthop Scand. 1996;67:541–544. [DOI] [PubMed]
- 30.Korovessis P, Baikousis A, Stamatakis M. First experience with the use of compression cerclage Gundolf in orthopaedic and trauma surgery: a preliminary report. Arch Orthop Trauma Surg. 1998;117:448–452. [DOI] [PubMed]
- 31.Korovessis P, Petsinis G, Repanti M, Repantis T. Metallosis after contemporary metal-on-metal total hip arthroplasty: five to nine-year follow-up. J Bone Joint Surg Am. 2006;88:1183–1191. [DOI] [PubMed]
- 32.Krishnamurthy AB, Macdonald SJ, Paprosky WG. 5- to 13-year follow-up study on cementless femoral components in revision surgery. J Arthroplasty. 1997;12:839–847. [DOI] [PubMed]
- 33.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. [DOI] [PubMed]
- 34.Lawrence JM, Engh CA, Macalino GE. Revision total hip arthroplasty: long-term results without cement. Orthop Clin North Am. 1993;24:635–644. [PubMed]
- 35.Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury. 2007;38:651–654. [DOI] [PubMed]
- 36.Loehr JF, Schutz U, Zund T, Drobny T, Munzinger U. [Intermediate term outcome of a hip prosthesis revision system] [in German]. Orthopäde. 2001;30:304–309. [DOI] [PubMed]
- 37.Malhotra R, Dua A, Kiran EK, Bhan S. Femoral revision using long hydroxyapatite-coated interlocking stem. Arch Orthop Trauma Surg. 2008;128:355–362. [DOI] [PubMed]
- 38.Malkani AL, Lewallen DG, Cabanela ME, Wallrichs SL. Femoral component revision using an uncemented, proximally coated, long-stem prosthesis. J Arthroplasty. 1996;11:411–418. [DOI] [PubMed]
- 39.Maurer SG, Baitner AC, Di Cesare PE. Reconstruction of the failed femoral component and proximal femoral bone loss in revision hip surgery. J Am Acad Orthop Surg. 2000;8:354–363. [DOI] [PubMed]
- 40.Meek D, Garbuz D, Masri B, Greidanus N, Dunkan C. Intraoperative fracture of the femur in revision total hip arthroplasty with a diaphyseal fitting stem. J Bone Joint Surg Am. 2004;86:480–485. [DOI] [PubMed]
- 41.Mulliken BD, Rorabeck CH, Bourne RB. Uncemented revision total hip arthroplasty: a 4-to-6-year review. Clin Orthop Relat Res. 1996;325:156–162. [DOI] [PubMed]
- 42.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. [DOI] [PubMed]
- 43.Pellicci PM, Wilson PD Jr, Sledge CB, Salvati EA, Ranawat CS, Poss R, Callaghan JJ. Long-term results of revision total hip replacement: a follow-up report. J Bone Joint Surg Am. 1985;67:513–516. [PubMed]
- 44.Retpen JB, Varmarken JE, Rock ND, Jensen JS. Unsatisfactory results after repeated revision of hip arthroplasty 61 cases followed for 5 (1–10) years. Acta Orthop Scand. 1992;63:120–127. [DOI] [PubMed]
- 45.Rubash HE, Harris WH. Revision of nonseptic, loose, cemented femoral components using modern cementing techniques. J Arthroplasty. 1988;3:241–248. [DOI] [PubMed]
- 46.Schuh A, Holzwarth U, Zeiler G. [Titanium modular revision prosthesis stem in revision hip prosthesis] [in German]. Orthopade. 2004;33:63–67. [DOI] [PubMed]
- 47.Sotereanos N, Sewecke J, Raukar GJ, DeMeo PJ, Bargiotas K, Wohlrab D. Revision total hip arthroplasty with a custom cementless stem with distal cross-locking screws: early results in femora with large proximal segmental deficiencies. J Bone Joint Surg Am. 2006;88:1079–1084. [DOI] [PubMed]
- 48.Van Kleunen JP, Anbari KK, Vu D, Garino JP. Impaction allografting for massive femoral defects in revision hip arthroplasty using collared textured stems. J Arthroplasty. 2006;21:362–371. [DOI] [PubMed]
- 49.Volkmann R, Bretschneider C, Eingartner C, Weller S. Revision arthroplasty—femoral aspect: the concept to solve high grade defects. Int Orthop. 2003;27(suppl 1):S24–S28. [PubMed]
- 50.Wagner H. [Revision prosthesis for the hip joint in severe bone loss] [in German]. Orthopade. 1987;16:295–300. [PubMed]
- 51.Walter WL, Walter WK, Zicat B. Clinical and radiographic assessment of a modular cementless ingrowth femoral stem system for revision hip arthroplasty. J Arthroplasty. 2006;21:172–178. [DOI] [PubMed]
- 52.Weber M, Hempfing A, Orler R, Ganz R. Femoral revision using the Wagner stem: results at 2–9 years. Int Orthop. 2002;26:36–39. [DOI] [PMC free article] [PubMed]
- 53.Woolson ST, Delaney TJ. Failure of a proximally porous-coated femoral prosthesis in revision total hip arthroplasty. J Arthroplasty. 1995;10:S22–S28. [DOI] [PubMed]
- 54.Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg Am. 1995;77:432–439. [DOI] [PubMed]
- 55.Zweymuller KA, Schwarzinger UM, Steindl MS. Radiolucent lines and osteolysis along tapered straight cementless titanium hip stems: a comparison of 6-year and 10-year follow-up results in 95 patients. Acta Orthop. 2006;77:871–876. [DOI] [PubMed]