Abstract
Callus formation and growth are an essential part of secondary fracture healing. Callus growth can be observed radiographically and measured using the “Callus Index,” which is defined as the maximum diameter of the callus divided by the diameter of the bone. We compared three groups of patients with tibial fractures treated by external fixation, intramedullary nailing, and casting to assess the validity of using serial measurements of callus index as a measure of fracture healing. When callus index was plotted against time for each patient, the point at which the fracture began to remodel, indicated by the highest point of the curve, was observed as a consistent feature regardless of fixation method. This occurred on average at 2½ weeks after plaster cast removal (14 weeks post injury), 5 weeks after external fixator removal (22 weeks post injury), and 27 weeks post injury for the intramedullary nailed fractures. Because remodeling only occurs once the fracture is stable, a peak in callus index is a reliable sign that the fracture has united. Serial measurements of callus index would therefore appear to offer a simple method of quantifying secondary fracture healing regardless of the treatment method used.
Level of Evidence: Level III, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Fracture healing is normally assessed in the clinic using a combination of subjective assessment of fracture stiffness and an assessment of radiological union by observing the presence of bridging callus or the obscuration of the fracture line. However, this may be unsatisfactory if union does not progress adequately or if a more exact evaluation of fracture healing is required, for example, in the evaluation of new treatments.
Existing methods of quantifying fracture healing have several limitations [25]. Most require specialized equipment that is not available in fracture clinics and are not applicable to many common fractures or fracture treatment methods. For example, fracture stiffness [4, 5, 20, 26] and acoustic emission [12] measurements can only be performed in those cases treated with external fixators and the fractured bone must be subcutaneous to enable testing using vibration or ultrasonic measurements [1, 7, 15, 18, 23].
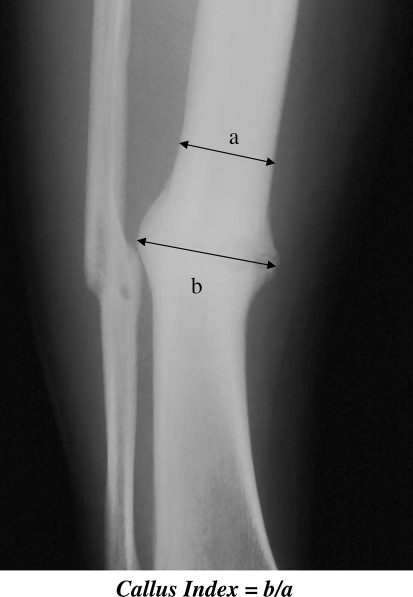
Several radiographic features are easily observed during indirect or secondary fracture healing with the production of an external callus, these being the formation and growth of a calcified callus and the bridging of the fracture with callus. Measurement of external callus from one radiograph was first described by Spencer [24] and used by Oni et al. [19], who measured callus index and calculated callus volume from tibial radiographs “when the fractures were united” but did not define this timeframe. They found no relationship between either of these values and a range of clinical factors including trauma severity and fracture morphology. Sano et al. [21] compared “cortex to callus ratio” with three-point bending stiffness in the tibias of euthanized beagles treated by internal fixation. In only one of the three groups (dogs euthanized at 24 weeks) was there any correlation between callus and mechanical stiffness. Spencer’s method can be refined using serial radiographs to produce a quantifiable measurement which we refer to as the “callus index.” Callus index is defined as the ratio of the maximum callus diameter to bone diameter at the same level as the callus (Fig. 1). As callus grows the callus index will increase, indicating that healing is progressing, and since remodeling of the fracture callus does not commence until sufficient stability of the fracture has been achieved, the time taken to reach a maximum callus diameter or “maximum callus index” could be a useful measurement of the time to clinical union.
Fig. 1.
A diagram of the method used to determine the callus index is shown. The callus index = b/a.
We have measured callus index at regular intervals during the healing period to observe the growth and remodeling of callus. By considering the relative size of callus we hypothesized it is possible to identify an end point of fracture union from radiographs alone. To attempt to prove this hypothesis we posed the following questions: (1) Can callus index be plotted and determined as a function of time and can the maximum callus index be determined from these plots? (2) Is there a difference in the time to achieve maximum callus index as a function of method of treatment? (3) Is callus index correlated with the mechanical stiffness of the fracture and does the of maximum callus index correlate with a given mechanical stiffness?
Materials and Methods
Three groups of 15 consecutive patients with tibial fractures treated by external fixation (ExFix), intramedullary nail (IMN), and plaster cast (POP) were identified from operating theatre records and the plaster room register. Details of the injury, fracture morphology, and recovery were recorded. The mean age of the 45 patients was 27 years (range, 14–57 years). Five were female (11%). There were no statistically significant differences in age between the three groups. The two most common mechanisms of injury were football and motorcycle road traffic accidents. Each group had similar proportions of high- and low-energy injuries.
The patient radiographs, which were normally taken every 3 to 4 weeks until healing was judged to be completed, were digitized using a Vidar VXR-12 scanner (Vidar Systems, Herndon, VA) and measurements taken using a bespoke software package [3]. Callus index was calculated by dividing the total diameter of callus by the diameter of the bone (Fig. 1). By using a ratio in this way, any variation in magnification or rotation is minimized. Callus index was determined for both anteroposterior (AP) and mediolateral (ML) radiographs for each patient in all three groups.
In the group of patients treated with external fixation, measurements of fracture stiffness were also performed. Fracture stiffness was measured using the Orthometer® (Orthofix SRL, Verona, Italy), which is a dedicated system of electronic goniometer, force-plate, and microprocessor that attaches to the bone pins of a fracture being treated by external fixation, the external fixation frame having been removed prior to the measurement. The heel is supported on the force plate, enabling measurement of the force required to produce a measured angular deflection. By pressing on the fracture and causing a small (typically < 1–2°) angular deflection in the sagittal plane, the stiffness of the fracture can be calculated in Newton meters per degree (Nm/deg) [11]. This device has previously been well-validated as a measure of fracture stiffness [9] and the refracture rate has been shown to be reduced when a value of bending stiffness of 15 Nm/deg is used as a guide to removal of the external fixator [20].
Data recording, display, and analysis were performed using Microsoft® Office Excel 2003 (Microsoft Corp., Redmond, WA) and all statistical analyses were performed using Minitab 15 for Windows (Minitab Inc., State College, PA). Certain common parameters were examined for each group. These were: the time of first appearance of callus (ie, when the callus index first exceeds unity); the maximum callus index achieved; and the time taken to reach the maximum value of callus index (as this can indicate approximately the point where callus growth ceases). Differences between the results for these parameters for each Group were tested statistically using a nonparametric Mann-Whitney U-test. The Bonferroni correction was applied when sequential testing of data from the same group of subjects was employed. To examine for any possible relationship between the callus indices and fracture stiffness for the ExFix group, linear correlation analyses were performed.
Results
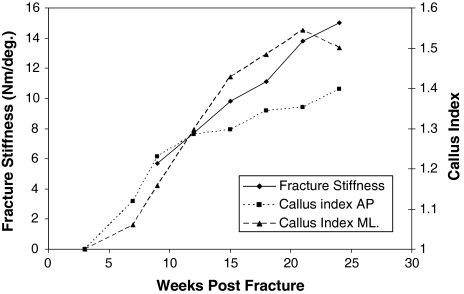
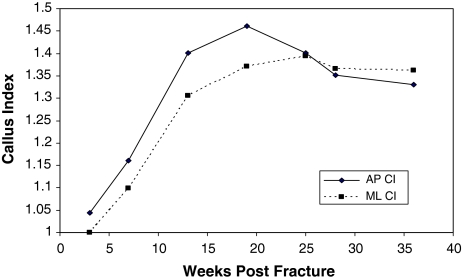
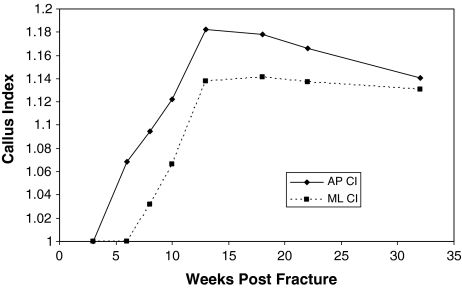
For an individual external fixation patient, both fracture stiffness and callus indices increased with time post-fracture (Fig. 2). When fracture stiffness reached 15 Nm/deg (representing “clinical” healing), the ML callus index began to decrease while the AP callus index continued to increase at a slower rate, suggesting the callus passed, or was shortly about to reach, its maximum dimensions. For individual patients in the IMN group and POP group, increases in callus index with time were also observed, as was the point at which the maximum values of callus index were reached (Figs. 3, 4). Linear correlation analyses were also performed between the AP and ML callus indices obtained for each group (ExFix, IMN and POP) (Table 1). Note that the time to maximum callus index for each radiographic projection (AP & ML) can be different. A peak in callus index was reached, i.e., a maximum callus index followed by a decrease in callus index (Fig. 3), in 63% and 53% of the ExFix group (AP and ML callus indices respectively), in 71% of the IMN group (both AP and ML callus indices) and in 79% and 77% of the POP group (AP and ML callus indices respectively).
Fig. 2.
A graph of fracture stiffness and AP and ML Callus Index versus time post fracture for a patient treated with external fixation is shown.
Fig. 3.
A graph of callus index versus time post fracture for a patient in the IMN group.
Fig. 4.
A graph of callus index versus time post fracture for a patient in the POP group is shown.
Table 1.
Linear correlation analyses between AP and ML callus indices
| Group | R2 | P |
|---|---|---|
| ExFix | 0.643 | < 0.001 |
| POP | 0.408 | < 0.001 |
| IMN | 0.551 | < 0.001 |
ExFix = external fixation; POP = plaster cast; IMN = intramedullary nail.
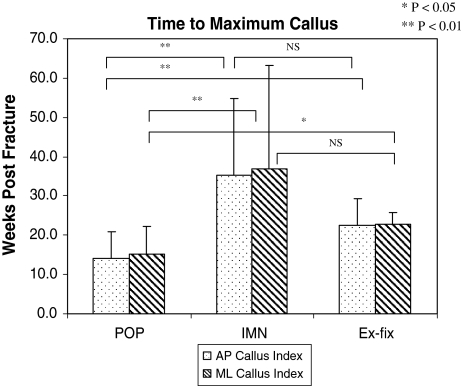
Callus was first seen after an average of 5.4 and 6.7 weeks (AP and ML radiographic projections respectively) in the POP group, after 10.2 and 11.4 weeks in the IMN group, and after 6.5 and 7.8 weeks in the ExFix group. There was no significant difference with the sole exception of the POP and IMN groups in the ML projection (p < 0.05), and this may partly be a reflection of the frequency of the postoperative radiographs. The time taken to reach the maximum callus indices was substantially different for each group for both AP and ML callus indices (Fig. 5). This was seen at a mean time of 14.1 and 15.2 weeks in the POP group, 35.1 and 36.8 weeks in the IMN group, and 22.5 and 22.7 weeks in the ExFix group. These times corresponded on average to 2½ weeks after removal of the cast, and 5 weeks after removal of the external fixator. The peak value of callus index reached in all three groups was not found to be significantly different between the groups on anteroposterior films and the only significant difference in the ML callus index was for the POP group and the ExFix group (p < 0.01).
Fig. 5.
A bar chart comparing the time to maximum AP and ML callus index in all three groups.
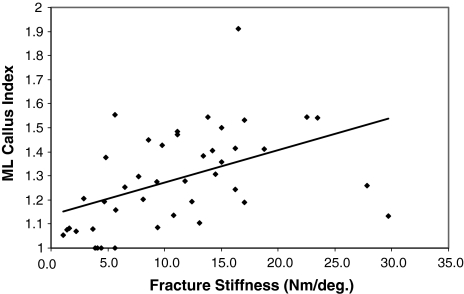
Linear correlation analyses of callus index with fracture stiffness demonstrated a poor correlation for the AP Callus Index, R2 = 0.053 (p = 0.19), and a tendency towards positive correlation for the ML Callus Index, R2 = 0.222 (p = 0.0013) (Fig. 6). The higher coefficient of determination in the ML group is explained by the fact that the stiffness is measured in this plane (the sagittal plane). The value of callus index when the measured fracture stiffness was closest to 15 Nm/deg. (mean 16.2 Nm/deg., SD = 1.32) was 1.36 (range 1.09–1.54, SD = 0.17) for the AP callus index and 1.43 (range 1.19–1.53, SD = 1.21) for the ML callus index.
Fig. 6.
A graph showing the correlation of ML callus index versus fracture stiffness for all of the patients in the ExFix group. The coefficient of determination, R2 = 0.222 (P = 0.0013).
Discussion
Clinical assessments of fracture healing are subjective and both manual and radiographic assessments of healing have been shown to be inaccurate. There is also a lack of consensus as to what is a reliable definition of fracture healing in the orthopaedic literature [6]. By examining and quantifying the radiographic changes in callus width during fracture healing (the callus index) we hypothesized it would be possible to identify an end point of fracture union from radiographs alone. The results presented above suggest it is possible to identify an end point of healing by measuring the callus index and that the time of occurrence of this end point will be different for different fracture treatments.
The callus index can usually be measured from standard radiographs that are obtained during the routine followup of most fractures. Although we used digital imaging to make these measurements, they can be done equally well by eye from the plain film using a ruler. Digital image analysis has been shown to be up to 20 times more accurate [3], but in this particular application, any errors produced by eye are unlikely to have a major influence on the results. Excessive variation of radiographic exposure or rotation can alter the appearance of callus. Overexposure reduces the apparent size of callus while underexposure can give the impression that soft tissue shadowing is callus. The quality of radiographs has improved with the introduction of digital radiography, reducing these problems. The effects of rotation on callus measurement are a result of the shape of the bone and hence the callus forming around it. Since the diaphysis of the tibia is essentially triangular in cross-section, small amounts of rotation can make a difference in the ratio of callus and cortical width. Gardner et al. [10] found the mean variation due to image rotation was only 1.4%. Our own studies show the variation in callus index due to rotation is up to 10% and is proportional to the callus size.
Certain fractures and fracture configurations are not amenable to callus measurement. Generally only diaphyseal long bone fractures treated with nonrigid fixation heal with sufficient callus production to enable their quantification. In fractures with translation at the fracture site, callus formation may be difficult to measure, as the callus tends to fill the gaps between the fractured bone ends rather than protrude from the cortical surfaces of the bone.
When the callus index obtained was compared to an objective measurement of fracture stiffness, the correlation between the two measurements was, at best, moderate, and this was in the same plane as the bending that occurred when the fracture stiffness measurements were made. Previous studies in this area have also demonstrated a poor correlation between radiographic parameters (such as callus diameter, callus volume, visibility of the fracture line, remodeling of the callus) and torsional fracture stiffness [2, 8]. This suggests that external callus size alone is not a major factor in determining the stiffness of a fracture and other factors, such as the extent of callus mineralization [8], whether the callus is fully bridged (although it has been previously shown that cortical bridging on its own is not a good predictor of healing [17]) the ability to weight-bear on the fractured limb [2, 13] and endosteal callus formation [16], must also be influential. The callus index values corresponding to a fracture stiffness of 15 Nm/deg were very variable and hence an equivalent callus index value which corresponds to this stiffness could not be determined.
Despite the fact that ML callus index is only moderately correlated to fracture stiffness and AP callus index is not correlated to fracture stiffness, both AP and ML callus indices were quite well correlated for all groups. This suggests a reasonable linear relationship between the callus index in both of the measured planes (AP and ML).
A peak in the callus index is an observable feature in the majority of the patients studied and it could be used as an indicator that healing has ceased and that remodeling has commenced. However the observation of a peak will be strongly dependent on the frequency of radiographs and, particularly in the latter stages of treatment when radiographs might be taken less frequently, a peak in the callus index could be easily missed.
Measuring the time to reach a maximum value of callus index can be used to compare different treatment methods. In this study we have demonstrated that the treatment method influences the time to reach the maximum value of callus index. There was also an influence of the fixation type on the maximum callus index reached between two of the groups (POP and ExFix). Those fractures treated by plaster cast (POP group) produced the most callus, probably due to the relatively large amounts of micromotion produced at the fracture site [14, 22], and also achieved the maximum size of callus in the shortest period of time. Rigid fixation such as locked intramedullary nailing tends to inhibit the production of large amounts of callus, and external fixation seems to produce an intermediate amount of callus between a cast and intramedullary nailing. So while not directly related to stiffness, callus index is able to distinguish between groups of patients being treated using different fixation methods.
Callus index is therefore potentially a useful measurement for quantifying fracture healing, particularly in the absence of other methods. Its simplicity means that it can be easily applied to patients in which the fracture is treated with any nonrigid fixation methods that will produce an external callus. While not strongly related to fracture stiffness it nevertheless produces measurements which demonstrate the progression of healing and, by determining the time to reach the maximum callus index, can be used to compare between treatment methods.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participating in the study was obtained.
References
- 1.Benirschke SK, Mirels H, Jones D, Tencer AF. The use of resonant frequency measurements for the noninvasive assessment of mechanical stiffness of the healing tibia. J Orthop Trauma. 1993;7:64–71. [DOI] [PubMed]
- 2.Blokhuis TJ, de Bruine JH, Bramer JA, den Boer FC, Bakker FC, Patka P, Haarman HJ, Manoliu RA. The reliability of plain radiography in experimental fracture healing. Skeletal Radiol. 2001;30:151–156. [DOI] [PubMed]
- 3.Bould M, Barnard S, Learmonth ID, Cunningham JL, Hardy JRW. Digital image analysis: Improving accuracy and reproducibility of radiographic measurement. Clin Biomech. 1999;14:434–437. [DOI] [PubMed]
- 4.Burny F, Bourgois R, Donkerwolcke M, Moulart F. Utilisation clinique de jauges de contrainte-situation actuelle et perspectives d’avenir. Acta Orthop Belg. 1978;44:895–920. [PubMed]
- 5.Claes L, Grass R, Schmickal T, Kisse B, Eggers C, Gerngross H, Mutschler W, Arand M, Wintermeyer T, Wentzensen A. Monitoring and healing analysis of 100 tibial shaft fractures. Langenbecks Arch Surg. 2002;387:146–152. [DOI] [PubMed]
- 6.Corrales LA, Morshed S, Bhandari M, Miclau T 3rd. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90:1862–1868. [DOI] [PMC free article] [PubMed]
- 7.Cunningham JL, Kenwright J, Kershaw CJ. Biomechanical measurements of fracture repair. J Med Eng Technol. 1990;14:92–101. [DOI] [PubMed]
- 8.Den Boer FC, Bramer JAM, Patka P, Bakker FC, Barentsen RH, Feilzer AJ, de Lange ESM, Haarman HJTM. Quantification of fracture healing with three-dimensional computed tomography. Arch Orthop and Trauma Surg. 1998;117:345–350. [DOI] [PubMed]
- 9.Eastaugh-Waring, SJ, Hardy JR, Cunningham JL. Fracture stiffness measurement using the Orthometer: reproducibility and sources of error. Clin Biomech. 2000;15:140–142. [DOI] [PubMed]
- 10.Gardner TN, Hardy JRW, Evans M, Kenwright J. Temporal changes in dynamic inter-fragmentary motion and callus formation in fractures. J Biomech. 1996;30:315–321. [DOI] [PubMed]
- 11.Hardy JRW, de Jong EJ, Richardson JB. Fracture stiffness. J Orthop Tech. 1994;2:177–189.
- 12.Hirasawa Y, Takai S, Kim WC, Takenaka N, Yoshino N, Watanabe Y. Biomechanical monitoring of healing bone based on acoustic emission technology. Clin Orthop Relat Res. 2002;402:236–244. [DOI] [PubMed]
- 13.Joslin CC, Eastaugh-Waring SJ, Hardy JRW, Cunningham JL. Weight bearing after tibial fracture as a guide to healing. Clin Biomech. 2008;23:329–333. [DOI] [PubMed]
- 14.Lippert FG, Hirsch C. The three dimensional measurement of tibia fracture motion by photogrammetry. Clin Orthop Relat Res. 1974;105:130–143. [DOI] [PubMed]
- 15.Malizos KN, Papachristos AA, Protopappas VC, Fotiadis DI. Transosseous application of low-intensity ultrasound for the enhancement and monitoring of fracture healing process in a sheep osteotomy model. Bone. 2006;38:530–539. [DOI] [PubMed]
- 16.Marsh D. Concepts of fracture union, delayed union and non-union. Clin Orthop Relat Res. 1998;355S:S22–S30. [DOI] [PubMed]
- 17.McClelland D, Thomas PBM, Bancroft G, Moorcroft CI. Fracture healing assessment comparing stiffness measurements using radiographs. Clin Orthop Relat Res. 2007;457:214–219. [DOI] [PubMed]
- 18.Nakatsuchi Y, Tsuchikane A, Nomura A. Assessment of fracture healing in the tibia using the impulse response method. J Orthop Trauma. 1996;10:50–62. [DOI] [PubMed]
- 19.Oni OOA, Dunning J, Mobbs RJ, Gregg PJ. Clinical factors and the size of the external callus in tibial shaft fractures. Clin Orthop Relat Res. 1991;273:278–283. [PubMed]
- 20.Richardson JB, Cunningham JL, Goodship AE, Connor BT, Kenwright J. Measuring stiffness can define healing of tibial fractures. J Bone Joint Surg Br. 1994;76:389–394. [PubMed]
- 21.Sano H, Uhthoff HK, Backman DS, Yeadon A. Correlation of radiographic measurements with biomechanical test results. Clin Orthop Relat Res. 1999;368:271–278. [DOI] [PubMed]
- 22.Sarmiento A, McKellop HA, Llinas A, Park SH, Lu B, Stetson W, Rao R. Effect of loading and fracture motions on diaphyseal tibial fractures. J Orthop Res. 1996;14:80–84. [DOI] [PubMed]
- 23.Saulgozis J, Pontaga I, Lowet G, Van der Perre G. The effect of fracture and fracture fixation on ultrasonic velocity and attenuation. Physiol Meas. 1996;17:201–211. [DOI] [PubMed]
- 24.Spencer RF. The effect of head injury on fracture healing. J Bone Joint Surg Br. 1987;69:525–528. [DOI] [PubMed]
- 25.Wade R, Richardson J. Outcome in fracture healing: a review. Injury. 2001;32:109–114. [DOI] [PubMed]
- 26.Wade RH, Moorcroft CI, Thomas PB. Fracture stiffness as a guide to the management of tibial fractures. J Bone Joint Surg Br. 2001;83:533–535. [DOI] [PubMed]