Abstract
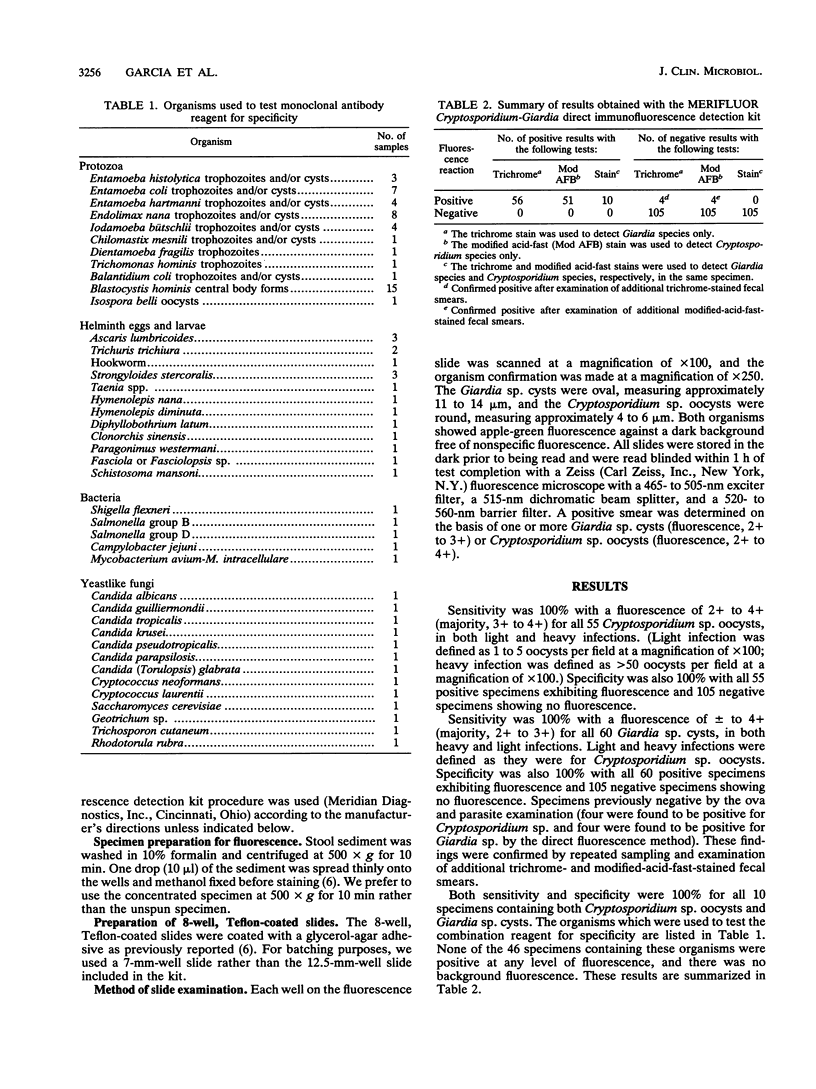
Giardia lamblia and Cryptosporidium parvum can cause severe symptoms in humans, particularly in the immunologically compromised. Monoclonal antibody reagents offer increased sensitivity and an excellent alternative to conventional staining methods. These reagents are helpful when screening large numbers of patients or those with minimal symptoms. Problems of false-positive and false-negative results with routine staining methods for stool parasites can be eliminated with monoclonal antibody reagents. Known positive formalinized specimens [Giardia sp. (n = 60), Cryptosporidium sp. (n = 55), and mixed Giardia-Cryptosporidium spp. (n = 10)] and negative formalinized specimens (n = 105), of which 46 contained other yeast or human cells or protozoa), were tested by the MERIFLUOR Cryptosporidium-Giardia direct immunofluorescence detection procedure. The MERIFLUOR reagent exhibited +/- to 4+ (majority, 2+ to 3+) on all Giardia cysts and 2+ to 4+ (majority, 3+ to 4+) on all Cryptosporidium oocysts. The cysts were generally oval (11 to 15 microns), while the oocysts were round (4 to 6 microns); both showed apple-green fluorescence against a background free of nonspecific fluorescence. All specimens positive for Giardia sp. and/or Cryptosporidium sp. showed fluorescence, and all specimens negative for the two organisms showed no fluorescence. There were eight specimens previously negative by the ova and parasite examination which were positive by the direct fluorescence method; four contained Giardia sp., and four contained Cryptosporidium sp. These positive results were confirmed after the examination of additional trichrome and modified acid-fast smears. The MERIFLUOR reagent was very easy to use, and even with a lower fluorescence intensity for Giardia sp. cysts, no false-negative or false-positive results among the specimens tested for either organism were found.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baxby D., Blundell N. Sensitive, rapid, simple methods for detecting Crysporidium in faeces. Lancet. 1983 Nov 12;2(8359):1149–1149. doi: 10.1016/s0140-6736(83)90669-4. [DOI] [PubMed] [Google Scholar]
- Current W. L., Garcia L. S. Cryptosporidiosis. Clin Microbiol Rev. 1991 Jul;4(3):325–358. doi: 10.1128/cmr.4.3.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupont H. L., Sullivan P. S. Giardiasis: the clinical spectrum, diagnosis and therapy. Pediatr Infect Dis. 1986 Jan-Feb;5(1 Suppl):S131–S138. [PubMed] [Google Scholar]
- Fayer R., Ungar B. L. Cryptosporidium spp. and cryptosporidiosis. Microbiol Rev. 1986 Dec;50(4):458–483. doi: 10.1128/mr.50.4.458-483.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L. S., Brewer T. C., Bruckner D. A. Fluorescence detection of Cryptosporidium oocysts in human fecal specimens by using monoclonal antibodies. J Clin Microbiol. 1987 Jan;25(1):119–121. doi: 10.1128/jcm.25.1.119-121.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L. S., Bruckner D. A., Brewer T. C., Shimizu R. Y. Techniques for the recovery and identification of Cryptosporidium oocysts from stool specimens. J Clin Microbiol. 1983 Jul;18(1):185–190. doi: 10.1128/jcm.18.1.185-190.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L. S., Current W. L. Cryptosporidiosis: clinical features and diagnosis. Crit Rev Clin Lab Sci. 1989;27(6):439–460. doi: 10.3109/10408368909114594. [DOI] [PubMed] [Google Scholar]
- Henriksen S. A., Pohlenz J. F. Staining of cryptosporidia by a modified Ziehl-Neelsen technique. Acta Vet Scand. 1981;22(3-4):594–596. doi: 10.1186/BF03548684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokipii L., Pohjola S., Jokipii A. M. Cryptosporidiosis associated with traveling and giardiasis. Gastroenterology. 1985 Oct;89(4):838–842. doi: 10.1016/0016-5085(85)90581-5. [DOI] [PubMed] [Google Scholar]
- Lo Cascio V., Adami S., Galvanini G., Cominacini L., Scuro L. A. The time course of a hypercalcaemic crisis in acute primary hyperparathyroidism. Lancet. 1984 Mar 31;1(8379):735–736. doi: 10.1016/s0140-6736(84)92246-3. [DOI] [PubMed] [Google Scholar]
- Ma P., Soave R. Three-step stool examination for cryptosporidiosis in 10 homosexual men with protracted watery diarrhea. J Infect Dis. 1983 May;147(5):824–828. doi: 10.1093/infdis/147.5.824. [DOI] [PubMed] [Google Scholar]
- Sterling C. R., Arrowood M. J. Detection of Cryptosporidium sp. infections using a direct immunofluorescent assay. Pediatr Infect Dis. 1986 Jan-Feb;5(1 Suppl):S139–S142. doi: 10.1097/00006454-198601001-00022. [DOI] [PubMed] [Google Scholar]
- Ungar B. L., Yolken R. H., Nash T. E., Quinn T. C. Enzyme-linked immunosorbent assay for the detection of Giardia lamblia in fecal specimens. J Infect Dis. 1984 Jan;149(1):90–97. doi: 10.1093/infdis/149.1.90. [DOI] [PubMed] [Google Scholar]
- Zierdt W. S. Concentration and identification of Cryptosporidium sp. by use of a parasite concentrator. J Clin Microbiol. 1984 Nov;20(5):860–861. doi: 10.1128/jcm.20.5.860-861.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]



