Abstract
The Tobacco Craving Questionnaire (TCQ) is a valid and reliable 47-item self-report instrument that assesses tobacco craving in four dimensions: emotionality, expectancy, compulsivity, and purposefulness. For use in research and clinical settings, we constructed a 12-item version of the TCQ by selecting three items from each of the four factors that exhibited optimal within-factor reliability (Cronbach’s alpha coefficient) and inter-item correlation. Smokers (N = 196) completed the TCQ–Short Form (TCQ–SF) after overnight tobacco deprivation and on a separate day during ad libitum smoking. Confirmatory factor analyses indicated acceptable model fit for a 4-factor model, with congruence coefficients suggesting high to very high similarity in factor patterns and magnitude of factor loadings between the TCQ and TCQ–SF in both conditions. Scores on each factor were significantly greater after tobacco deprivation than ad libitum smoking, were associated with measures of tobacco withdrawal, and varied with degree of nicotine dependence. Cronbach’s alpha coefficients and average inter-item correlations were similar in both conditions and were consistent with reliability values obtained in the initial validation of the TCQ. Test-retest correlation coefficients were also similar to those found in a previous study. These findings suggest that the TCQ–SF is as valid and reliable as the 47-item TCQ in measuring tobacco craving.
Introduction
Tobacco craving has been the focus of much discussion and research with respect to its role as a symptom of nicotine dependence and as a relapse factor in maintaining tobacco use (Piasecki, 2006; Shiffman et al., 1997; Tiffany, Carter, & Singleton, 2000). Individuals attempting to quit smoking typically report intense craving for cigarettes (Hughes & Hatsukami, 1986; West & Schneider, 1987). Laboratory and clinical studies have shown that reports of tobacco craving increase during periods of abstinence (Bell, Taylor, Singleton, Henningfield, & Heishman, 1999; Hughes & Hatsukami, 1986; Shiffman, Paty, Gnys, Kassel, & Elash, 1995) and that craving predicts relapse in smokers trying to quit (Killen et al., 2006; Shiffman et al., 1997). Although craving plays a significant role in the maintenance of nicotine dependence and treatment outcome, little research has focused on development of multidimensional measures of tobacco craving or assessment of their psychometric properties.
To this end, we recently developed the Tobacco Craving Questionnaire (TCQ), a multidimensional scale with 47 items covering a broad range of clinically and theoretically distinct explanations for tobacco craving: desire to smoke, anticipation of positive outcomes from smoking, anticipation of relief from withdrawal symptoms or negative mood, lack of control over use, and intention and planning to smoke (Heishman, Singleton, & Moolchan, 2003). Craving is often measured using single-item questions that have face validity, but can vary widely in test-retest reliability and preclude the determination of internal consistency reliability (Wewers, Rachfal, & Ahijevych, 1990). Single-item measures are also unable to capture the range of theoretical and experiential perspectives of craving described above (Mezinskis, Honos-Webb, Kropp, & Somoza, 2001).
In the initial validation study of the TCQ, exploratory and confirmatory factor analyses yielded 17 items with significant (>.30) loadings on four latent constructs (factors) that characterized tobacco craving (Heishman et al., 2003). Results also suggested that the 4-factor solution was more appropriate than either a 3-factor or 5-factor primary solution or a 1-factor higher-order solution. Thus, we evaluated content validity and assigned meaning to the factors by examining item content and correlations between factor scores and variables of interest commonly found in smoking studies. Negative mood and craving (visual analog scale [VAS]) were significantly associated with Factor 1 that consisted of items from the anticipation of relief from withdrawal symptoms or negative mood domain. Liking and desire to smoke were significantly correlated with Factor 2 that contained items from the anticipation of positive outcomes from smoking domain. Craving (VAS) and expectations about the positive benefits of smoking were significantly associated with Factor 3, comprising items from the lack of control over use and desire to smoke domains. Desire and need to smoke and average number of daily cigarettes were significantly correlated with Factor 4 that contained items from the intention and planning to smoke domain. Factors 1–4 were named emotionality, expectancy, compulsivity, and purposefulness, respectively.
Singleton, Anderson, and Heishman (2003) further documented the reliability and validity of the 47-item TCQ by demonstrating internal consistency and unidimensionality of the four factors and establishing criterion-related, convergent, and discriminant validity. Additional research has shown that repeated administration of the TCQ is sensitive to changes in craving and mood, as demonstrated by orderly increases in TCQ factor scores as a function of increasing intensity of smoking-urge content of imagery scripts (Lee et al., 2007; Singleton et al., 2003). One limitation of these studies was that participants were tested only under ad libitum smoking conditions. Drobes and Tiffany (1997) reported that tobacco deprivation produced an enhancement of craving self-report, but did not increase responses to smoking cues. In the present study, we compared the effects of tobacco deprivation versus nondeprivation on TCQ responses to validate its ability to assess changes in craving states.
An added concern was the length of the questionnaire. The average time to complete the 47-item TCQ was 8 min (Heishman et al., 2003), which might limit its use in clinical settings where patients are often assessed with many forms and in research studies where measures are repeated frequently. Theoretically, a shorter form of any multiple-item questionnaire can be created without reducing reliability (Tiffany et al., 2000). Heishman et al. (2006) conducted a preliminary study of imagery-induced craving using only the 17 items with significant loadings from the rotated factor structure of the TCQ (Heishman et al., 2003) and found significant increases in Factor 1 (emotionality) and Factor 3 (compulsivity). Similar to the TCQ, the four factor scales derived from the 17 items had low to high internal consistencies and inter-item correlations; exhibited low to moderate positive intercorrelations; and were significantly correlated with single-item measures of craving, current mood, and daily cigarette smoking.
Using only the items with significant factor loadings made the TCQ easier to administer, but even a 17-item questionnaire might prove too lengthy for brain imaging or cue-reactivity studies. Additionally, two of the factor scales on both versions (expectancy and purposefulness) were worded negatively to reduce variance due to acquiescence and might be more indicative of participants’ inattention to rating compared with their responding to item content (Heinz et al., 2006). Thus, we constructed a 12-item version of the TCQ (TCQ–Short Form, TCQ–SF) by selecting 3 of the 17 items that exhibited optimal within-factor internal consistency (Cronbach’s alpha coefficient) as indicators for each of the four TCQ factors; all items were worded positively. In a study of 40 smokers, there was no evidence that any of the four factor scale responses was adversely affected by assessment reactivity bias when the TCQ–SF was repeated every minute for 15 min (Heishman, Saha, & Singleton, 2004). The small sample size, however, precluded reporting the psychometric properties of the TCQ–SF.
The purpose of this study was to compare the factor structure of the TCQ–SF to that of the TCQ by testing smokers under tobacco-deprived and nondeprived conditions. We examined congruence in factor loadings and structure between the TCQ and TCQ–SF separately for each condition and between repeated administrations of the TCQ–SF. We hypothesized that craving intensity would be greater following tobacco deprivation compared with ad libitum smoking and that the TCQ factor structure would be replicated in the TCQ–SF. We also included commonly used measures of tobacco craving, withdrawal, and mood to explore the convergent validity of the TCQ–SF. To assess discriminant validity, we examined the association between degree of nicotine dependence and TCQ–SF scores, hypothesizing a direct relationship.
Methods
Setting
This study was performed at the NIDA Intramural Research Program.
Participants
Cigarette smokers were recruited from the greater Baltimore community via print, radio, and television advertisements. A total of 201 smokers were tested, but 5 participants were excluded from analyses because of failure to abstain from smoking. The final sample consisted of 196 smokers (47 Black men, 53 Black women, 50 White men, and 46 White women). Inclusionary criteria were smoking at least 15 cigarettes per day for the past 2 years and no interest in quitting. Before the study, participants received a medical and psychiatric examination. Participants gave written informed consent according to guidelines for the protection of research volunteers of the U.S. Department of Health and Human Services and were paid for their participation. The NIDA Institutional Review Board approved the study.
Procedure
The study used a within-subjects design and consisted of two experimental sessions, separated by at least 24 hr. Sessions lasted 2 hr and entailed completion of a battery of cognitive and psychomotor tests and self-report questionnaires, designed to examine individual differences in acute tobacco deprivation. Participants smoked normally before arriving at the laboratory for one session and smoked one of their preferred-brand cigarettes before the session to standardize the time since last tobacco exposure. At the other session, participants were tobacco deprived for at least 12 hr. Bell et al. (1999) reported that mean expired air carbon monoxide (CO) level was 11.1 and 6.7 parts per million (ppm) after 8 and 16 hr, respectively, of enforced tobacco abstinence. Thus, in this study, we chose a CO cutoff of ⩽ 11 ppm to verify abstinence. Order of the two conditions was counterbalanced across participants.
Measures
TCQ–SF
The distribution of TCQ–SF items based on the 4-factor scale structure of the TCQ is shown in Table 1. Items were rated on a Likert-type scale from 1 (strongly disagree) to 7 (strongly agree). Factor scores for each participant were obtained by summing the three items in each factor scale, yielding a score ranging from 3 to 21. The TCQ–SF factors were operationally defined the same as those of the TCQ: (a) emotionality, smoking in anticipation of relief from withdrawal or negative mood; (b) expectancy, anticipation of positive outcomes from smoking; (c) compulsivity, an inability to control tobacco use; and (d) purposefulness, intention and planning to smoke for positive outcomes. In the initial validation study (Heishman et al., 2003), estimates of internal consistency (Cronbach’s alpha; Cronbach, 1951) of TCQ Factors 1–4 and number of items in each factor (in parentheses) were 0.82(4), 0.70(3), 0.75(5), and 0.48(3), respectively.
Table 1.
Factor structure of Tobacco Craving Questionnaire–Short Form.
| Factor 1 (emotionality) | |
| 5. | I would be less irritable now if I could smoke. |
| 9. | If I were smoking now I could think more clearly. |
| 12. | I could control things better right now if I could smoke. |
| Factor 2 (expectancy) | |
| 1. | I would enjoy a cigarette right now. |
| 4. | A cigarette would taste good right now. |
| 8. | Smoking a cigarette would be pleasant. |
| Factor 3 (compulsivity) | |
| 2. | If I smoked right now, I would not be able to stop. |
| 7. | I could not stop myself from smoking if I had some cigarettes here. |
| 10. | I would not be able to control how much I smoked if I had some cigarettes here. |
| Factor 4 (purposefulness) | |
| 3. | If I had a lit cigarette in my hand, I probably would smoke it. |
| 6. | It would be hard to pass up the chance to smoke. |
| 11. | I could not easily limit how much I smoked right now. |
Fagerström Test for Nicotine Dependence (FTND)
The FTND is a reliable and valid measure of nicotine dependence (Heatherton, Kozlowski, Frecker, & Fagerström, 1991). Scores range from 0 to 10. We used the FTND to characterize the sample and to distinguish highly dependent (⩾6) from less dependent (⩽5) smokers (Fagerström et al., 1996; Ferguson et al., 2003).
Minnesota Nicotine Withdrawal Scale (MNWS)
We used a modified version of the MNWS (Hughes & Hatsukami, 1986) to assess tobacco withdrawal symptoms. Items were rated on a 0–5 interval scale (not present to severe). The item assessing tobacco craving was scored separately. The remaining 10 items (irritable, anxious, difficulty concentrating, restless, impatient, hunger, somatic symptoms, increased eating, drowsy, headaches) were averaged, yielding a total withdrawal score. The individual craving item and the total score have high reliability and good construct validity (Hughes & Hatsukami, 1986; West, Ussher, Evans, & Rashid, 2006).
Positive and Negative Affect Schedule (PANAS)
The PANAS (Watson, Clark, & Tellegen, 1988) consists of two 10-item scales that measure aspects of positive affect (PA: active, alert, attentive, determined, enthusiastic, excited, inspired, interested, proud, strong) and negative affect (NA: afraid, ashamed, distressed, guilty, hostile, irritable, jittery, nervous, scared, upset). Each item was rated on a 5-point scale (not at all to extremely). The PANAS has demonstrated high internal consistency and test-retest reliability (Watson et al., 1988).
Data analyses
The statistical package Comprehensive Exploratory Factor Analysis (CEFA) (Browne, Cudeck, Tateneni, & Mels, 2004) was used to determine if the TCQ–SF maintained the 4-factor structure of the TCQ. We conducted confirmatory factor analysis (CFA) using maximum Wishart likelihood estimation and oblique rotation without normalization to a least squares fit to match the 4-factor TCQ target matrix. Target specification for the assignment of TCQ–SF items to each respective factor matched the manner in which similar items were assigned to the same factor in the TCQ: (a) factor 1 would include items 5, 9, and 12; (b) factor 2 would include items 1, 4, and 8; (c) factor 3 would include items 2, 7, and 10; and (d) factor 4 would include items 3, 6, and 11. Models assumed no higher-order factors, correlated first-order factors, and uncorrelated residuals. Goodness-of-fit for the unrotated factors was examined using the Steiger-Lind root mean square error of approximation statistic (RMSEA; Steiger, 1980) produced in CEFA. For RMSEA, values <0.05 constitute good fit, values 0.05–0.08 acceptable fit, values 0.08–0.10 marginal fit, and values >0.10 poor fit of the model (Browne & Cudeck, 1993). We used hypothesis tests developed to test the statistical significance of the fit (Browne & Cudeck, 1993) for the 4-factor model, with exceedance probabilities for perfect fit (H0: RMSEA = 0) and close fit (H0: RMSEA ⩽ 0.05). Models for the tobacco-deprived and nondeprived conditions were derived and evaluated independently.
We compared next the rotated matrices of factor loadings obtained for the 4-factor TCQ–SF model (comparison) and for the assigned items in the original TCQ model (target) using Tucker’s coefficient of congruence (f) as a statistical index of similarity in factor patterns and magnitude of factor loadings between sets of factors derived from identical items (Wrigley & Neuhaus, 1955). Empirical studies indicate f values of 0.70–0.79 represent moderate, 0.80–0.89 high, and >0.90 very high similarity between target and comparison factors (Koschat & Swayne, 1991; ten Berge, 1986).
Following MacCallum, Widaman, Preacher, and Hong (2001), we also calculated the mean coefficient of congruence (K) across the four factors to evaluate the overall discrepancy in factor structure between the TCQ–SF and TCQ. Guidelines for interpreting K are 0.98–1.00 = excellent, 0.92–0.98 = good, 0.82– 0.92 = borderline, 0.68–0.82 = poor, and <0.68 = terrible fit between the comparison and target matrices (MacCallum et al., 2001). We derived f and K values for tobacco-deprived and nondeprived conditions to measure the similarity in configurations of the assigned factor items for repeated administration of the TCQ–SF.
We evaluated homogeneity of factors two ways. First, we conducted principal components analysis (PCA) of the assigned items for each factor. If more than one component were retained by the PCA, this would indicate a significant departure from unidimensionality (homogeneity). Second, Cronbach’s alpha coefficients, inter-item correlations, and factor intercorrelations were calculated separately for each TCQ–SF factor scale in the tobacco-deprived and nondeprived conditions. To evaluate test-retest reliability of each factor scale, we calculated Pearson’s r and intraclass correlation coefficients (ICC).
For validity testing, data from the TCQ–SF, MNWS, and PANAS were analyzed using within-subjects multivariate analysis of variance (MANOVA) and multivariate analysis of covariance (MANCOVA) with condition order, race, and sex as covariates. The test of significance was based on Wilks’ lambda and was converted to an F value (Rao’s R). Pairwise comparisons between degree of nicotine dependence (based on FTND score) and experimental condition (tobacco deprivation vs. nondeprivation) means were performed with Tukey’s Honestly Significant Difference tests. Homogeneity and validity analyses were conducted using STATISTICA (StatSoft, Inc.)
Results
Participant characteristics
Table 2 compares characteristics of participants in this study with those in the initial TCQ validation study (Heishman et al., 2003). The samples were similar with the exception of a smaller percentage of Blacks in the present study. Table 3 shows characteristics of subgroups in this study. Compared with Whites, Black participants were 5 years older (p<.001), had smoked for 3.5 more years (p<.05), and smoked almost three fewer cigarettes per day (p<.01). There was no difference between Blacks and Whites on number of quit attempts and FTND score and no sex difference on any variable.
Table 2.
Participant characteristics in the initial TCQ validation studya and the TCQ–SF validation study.
| TCQ Studya | TCQ–SF Study | |
|---|---|---|
| Number of participants | 213 | 196 |
| Male, percent | 54 | 49 |
| Black, percent | 75 | 51 |
| Mean age, years (SD) | 36.6 (7.7) | 36.6 (10.0) |
| Mean years smoked (SD) | 22.2 (9.0) | 19.7 (10.3) |
| Mean cigarettes per day (SD) | 26.3 (14.5) | 22.1 (6.6) |
| Mean quit attempts (SD) | 3.3 (2.7) | 3.4 (3.5) |
| Mean FTND score (SD) | 5.8 (2.3) | 6.5 (1.7) |
Note. TCQ, Tobacco Craving Questionnaire; TCQ–SF, Tobacco Craving Questionnaire–Short Form; FTND, Fagerström Test for Nicotine Dependence.
Table 3.
Characteristics of participant subgroups (N= 196).
| Blacks (n= 100) | Whites (n= 96) | Men (n= 97) | Women (n= 99) | |
|---|---|---|---|---|
| Percent of N | 51.0 | 49.0 | 49.5 | 50.5 |
| Mean age, years (SD) | 39.0 (9.5) | 34.1 (10.0) | 36.4 (9.9) | 36.7 (10.2) |
| Mean years smoked (SD) | 21.4 (10.3) | 17.9 (10.0) | 19.4 (10.3) | 19.9 (10.4) |
| Mean cigarettes per day (SD) | 20.7 (6.9) | 23.5 (6.0) | 22.2 (6.5) | 22.0 (6.7) |
| Mean quit attempts (SD) | 3.1 (2.2) | 3.6 (4.4) | 3.6 (3.5) | 3.1 (3.6) |
| Mean FTND score (SD) | 6.5 (1.6) | 6.5 (1.8) | 6.3 (1.6) | 6.7 (1.8) |
Note. FTND, Fagerström Test for Nicotine Dependence.
Highly dependent smokers (n = 138: 71 Blacks, 67 Whites; 64 men, 74 women) and less dependent smokers (n = 58: 29 Blacks, 29 Whites; 33 men, 25 women) differed with respect to mean FTND score (7.4 vs. 4.4, p<.001) and mean cigarettes per day (23.1 vs. 19.6, p<.001). They did not differ significantly in the distribution of Blacks and Whites or by sex, age, years smoked, and number of quit attempts.
Baseline CO
Expired air CO was significantly lower after 12 hr of tobacco deprivation than during ad libitum smoking (p<.001). Mean (SD) baseline CO level was 30.3 ppm (12.1) at the nondeprived session and 6.9 ppm (2.4) at the deprived session, confirming compliance with the overnight smoking restriction (cf., Bell et al., 1999).
Factor analysis and reliability of the TCQ–SF
Table 4 compares factor loadings for the TCQ–SF (deprived and nondeprived conditions) with those of the TCQ validation study (Heishman et al., 2003). CFA of the TCQ–SF items in the nondeprived condition showed a close but imperfect fit with the 4-factor target model, χ2(24, n = 196) = 42.0; RMSEA = 0.062 (90% confidence interval [CI] = .00–.08), perfect fit p>.012, close fit p>.242. Factors exhibited positive intercorrelations (all p’s<.001), with Pearson’s r ranging from 0.59 to 0.74. Hierarchical factor analysis yielded two secondary higher-order factors. Cronbach’s alpha coefficient and average inter-item correlation (in parentheses) were 0.90(0.77), 0.89(0.72), 0.78(0.54), and 0.69(0.43) for factors 1–4, respectively. Individual PCA extracted only one component per measured construct (factor); component loadings exceeded 0.76 for all items comprising each factor. The variance accounted for was 84.2%, 81.4%, 69.2%, and 61.9% for factors 1–4, respectively. Individual congruence coefficients between TCQ–SF factors 1–4 and corresponding factors on the TCQ were f = 0.88, 0.84, 0.90, and 0.75, respectively. The mean congruence coefficient (K) for the nondeprived condition was 0.84.
Table 4.
Oblique rotated factor matrix for the TCQ and TCQ–SF.
| Factor 1 Emotionality |
Factor 2 Expectancy |
Factor 3 Compulsivity |
Factor 4 Purposefulness |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item | TCQa | NDb | Dc | TCQa | NDb | Dc | TCQa | NDb | Dc | TCQa | NDb | Dc |
| 1. | .17 | .13 | −.03 | .52 | .51 | .46 | .00 | .17 | −.04 | .27 | .46 | .48 |
| 2. | .19 | .06 | .07 | .03 | .19 | .12 | .59 | .59 | .51 | .09 | .13 | .26 |
| 3. | −.03 | −.07 | −.03 | .11 | .45 | −.09 | .26 | .13 | −.11 | .48 | .45 | .89 |
| 4. | .12 | .07 | −.01 | .51 | .58 | .61 | .13 | .16 | .12 | .25 | .45 | .21 |
| 5. | .62 | .74 | .43 | .16 | .19 | .23 | .19 | .11 | .10 | .04 | −.05 | .18 |
| 6. | .09 | .25 | .12 | .10 | .38 | .35 | .04 | .22 | .12 | .48 | .40 | .50 |
| 7. | .15 | .06 | .04 | .14 | .06 | .07 | .69 | .52 | .66 | .13 | .46 | .30 |
| 8. | .17 | .03 | .15 | .52 | .47 | .77 | .00 | −.05 | .04 | .09 | .72 | .06 |
| 9. | .74 | .30 | .85 | .04 | .05 | .10 | .23 | .02 | .11 | .05 | .15 | .04 |
| 10. | .24 | −.06 | −.02 | .00 | −.13 | −.09 | .49 | .72 | .94 | .02 | .67 | .36 |
| 11. | −.03 | −.04 | −.03 | .12 | −.19 | −.04 | .26 | .56 | .75 | .35 | .58 | .36 |
| 12. | .69 | .78 | .74 | .12 | −.06 | −.08 | .24 | .14 | .19 | .02 | .17 | .22 |
Note. TCQ, Tobacco Craving Questionnaire; TCQ–SF, Tobacco Craving Questionnaire–Short Form. Bolded factor loadings indicate target (TCQ) and comparison (TCQ–SF) item pattern.
Initial TCQ validation study (N= 213; Heishman et al., 2003).
Nondeprived condition in present study (n= 196).
Deprived condition in present study (n= 196).
CFA of the TCQ–SF items in the tobacco-deprived condition also indicated a close but imperfect fit of the 4-factor model, χ2(24, n = 196) = 49.6; RMSEA = 0.074 (90% CI = 0.04–0.10), perfect fit, p>.003; close fit, p>.085. Factors were significantly correlated; Pearson’s r ranged from 0.37 to 0.60 (all p<.001). Hierarchical factor analysis yielded two secondary higher-order factors. Cronbach’s alpha coefficient and average inter-item correlation (in parentheses) were 0.81(0.62), 0.84(0.65), 0.79(0.58), and 0.59(0.44) for factors 1–4, respectively. PCA indicated that factor loadings exceeded 0.53 for all items comprising each factor. The variance accounted for by factors 1–4, respectively, was 74.7%, 72.5%, 69.4%, and 55.3%. Congruence coefficients between TCQ–SF factors 1–4 and corresponding factors on the TCQ were f = 0.94, 0.91, 0.85, and 0.91, respectively; for the tobacco-deprived condition, K = 0.90. For the repeated administration of the TCQ–SF, f = 0.84, 0.85, 0.95, and 0.74 for factors 1–4, respectively, and K = 0.84. Pearson’s test-retest correlation coefficients and ICC (in parentheses) for factors 1–4 were 0.64(0.60), 0.22(0.20), 0.53(0.46), and 0.31(0.30), respectively. For comparative purposes, congruence coefficients for the original TCQ sample indicated high to very high similarity (f = 0.93, 0.94, 0.80, and 0.87 for factors 1–4, respectively) and borderline fit (K = 0.89) with the population.
Validity of the TCQ–SF
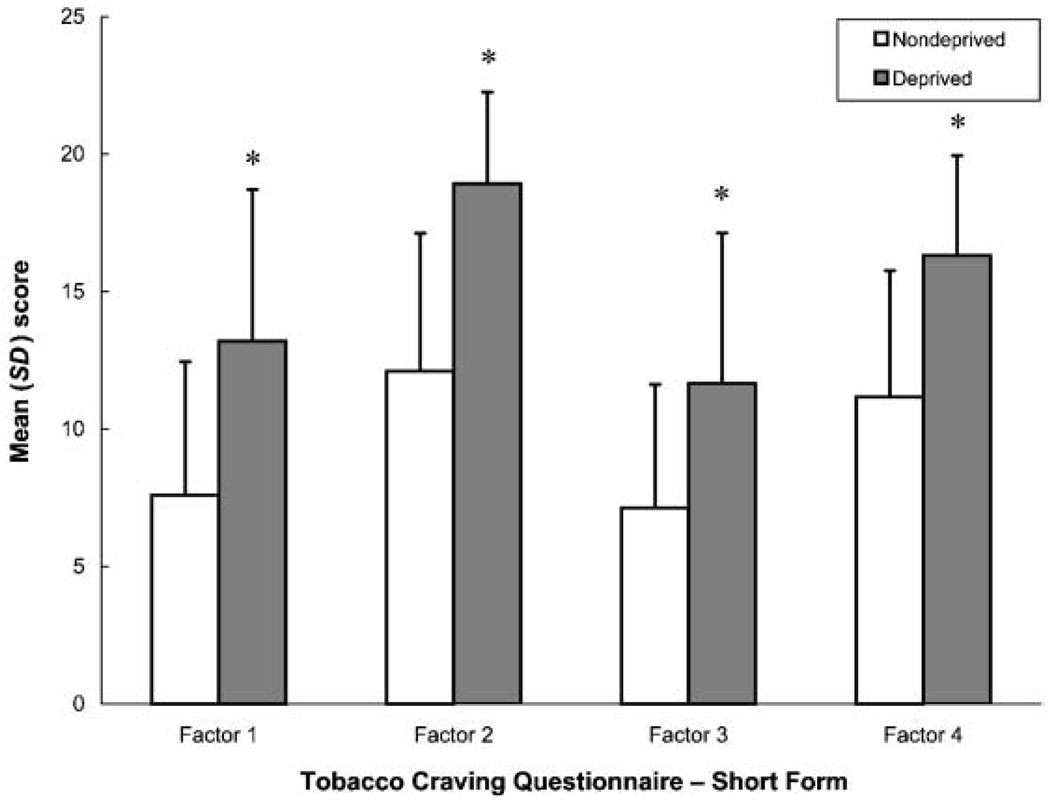
In the primary analysis, a two-way (degree of nicotine dependence by condition), within-subjects MANOVA revealed significant main effects for dependence, Rao’s R(8,187) = 2.06, p<.05, and condition, Rao’s R(8,187) = 58.21, p<.001, but no dependence by condition interaction. MANCOVA controlling for order, race, and sex did not alter the outcome. Figure 1 shows TCQ–SF responses as a function of condition. Post hoc comparisons indicated that TCQ–SF Factors 1–4, MNWS craving, MNWS total score, and PANAS-NA scores were greater, and PANAS-PA score was lower, in the deprived condition compared with the nondeprived condition (all p<.001). Post hoc tests also indicated TCQ–SF factor 2 (p<.01), factor 3 (p<.05), and MNWS craving (p<.05) were greater for highly dependent (FTND ⩾6) than less dependent smokers. Correlational analyses (Pearson’s r) indicated that TCQ–SF factors 1–4 were positively associated with MNWS craving (range 0.41–0.50, all p<.001) and MNWS total score (range 0.19–0.33, all p<.05).
Figure 1.
Mean (±SD) factor scores on the Tobacco Craving Questionnaire–Short Form. Each column represents the mean of 196 participants tested under conditions of tobacco deprivation (12 hr) and nondeprivation. *p<.001 different from the nondeprived condition.
In a secondary analysis, we conducted separate MANOVAs to examine potential confounds of order, race, and sex. A three-way (order by dependence by condition), within-subjects MANOVA revealed a significant main effect for order, Rao’s R(8,185) = 2.88, p<.01; dependence, Rao’s R(8,185) = 2.04, p<.05; and condition, Rao’s R(8,185) = 57.30, p<.001, but no significant higher-order interactions. Post hoc tests showed that participants randomly assigned to the nondeprived condition for the first session and the deprived condition for the second session had lower mean TCQ–SF Factor 4 scores averaged over both sessions than those randomly assigned to the opposite order (12.8 vs. 14.3, respectively, p<.01).
A three-way (race by dependence by condition), within-subjects MANOVA yielded a significant main effect for race, Rao’s R(8,185) = 2.08, p<.05; dependence, Rao’s R(8,185) = 2.05, p<.05; and condition, Rao’s R(8,185) = 58.82, p<.001, but no significant higher-order interactions. Blacks scored higher than Whites on PANAS-PA (3.2 vs. 2.8, p<.01).
A three-way (sex by dependence by condition), within-subjects MANOVA revealed significant main effects for dependence, Rao’s R(8,185) = 2.03, p<.05 and condition, Rao’s R(8,185) = 58.50, p<.001, and a significant sex by condition interaction, Rao’s R(8,185) = 2.05, p<.05. The sex main effect and higher-order interactions were not significant (p>.20). Because there is no unambiguous choice of the appropriate error term for comparisons involving between-group and within-group interactions, we could not compute post hoc tests. Visual inspection of means suggested that in the tobacco-deprived condition, women scored higher on TCQ–SF Factor 1 (14.1 vs. 11.8) and Factor 3 (12.1 vs. 10.5), MNWS total score (27.8 vs. 23.8), and PANAS-NA (1.8 vs. 1.6) compared with men.
Discussion
We originally developed the TCQ to be a multidimensional questionnaire using clinically-based categories of craving and found that four factors best characterized tobacco craving. Several studies have demonstrated the reliability and validity of the TCQ (Heishman et al., 2003, 2004; Lee et al., 2007; Singleton et al., 2003). Results of the present study suggest that the TCQ–SF is also a reliable and valid measure of tobacco craving.
Confirmatory factor analysis of the TCQ–SF indicated an acceptable model fit to the TCQ in the tobacco-deprived and nondeprived conditions. Visual inspection indicated that factor patterns for significant items (>.30) loaded exactly between target (TCQ) and comparison (TCQ–SF) factors for both conditions, suggesting convergent validity (Kline, 2005). Nevertheless, the common practice of assigning items to the factor with the highest loading would have resulted in items 1 and 11 being assigned incorrectly to factors 4 and 3, respectively, in the deprived condition. Similarly, item 8 would have been assigned incorrectly to factor 4 in the nondeprived condition. There were high cross loadings for these items probably because all three items were negatively-keyed on the TCQ, but were positively-keyed to ease scoring of the TCQ–SF.
Congruence coefficients indicated high to very high similarity in factor loadings and structure between the TCQ and TCQ–SF in each condition and between repeated administrations of the TCQ–SF. Cronbach’s alpha coefficients and average inter-item correlations were similar in both conditions and were consistent with reliability values obtained in the initial validation of the TCQ (Heishman et al., 2003). Test-retest correlation coefficients were also similar to those found previously (Singleton et al., 2003). Taken together, these findings indicate that the TCQ–SF reliably measures the same multidimensional aspects of tobacco craving as the TCQ when tested under different experimental conditions and over repeated assessments. Additionally, the replicable factor structure across different samples and manipulations provides support for a multidimensional perspective of tobacco craving, consistent with previous research (Cox, Tiffany & Christen, 2001).
Although Cronbach’s alpha coefficient, which reflects the internal consistency of an instrument’s mulitple items, is the conventional measure of a questionnaire’s reliability, an equally important aspect of reliability is unidimensionality. A unidimensional questionnaire measures unique aspects of the construct being assessed and thus provides a clear, unambiguous interpretation of the construct (Schmitt, 1996). In the tobacco-deprived and nondeprived conditions, PCAs extracted only one measured component per factor, indicating no significant departure from unidimensionality and suggesting that each factor consistently tapped a unique aspect of tobacco craving.
High intercorrelations (Pearson’s r) among the four primary factors could indicate that an alternative model with one secondary higher-order factor may be able to explain much of the common variance. Hierarchical factor analysis, however, yielded two secondary higher-order factors in both the tobacco-deprived and nondeprived conditions. Thus, the four primary factors of the TCQ–SF continue to demonstrate unique variance and homogeneity, which supports craving as a multidimensional, rather than a single, construct.
The TCQ–SF was sensitive to the effects of overnight tobacco deprivation. Scores on each factor were significantly greater after deprivation than during ad libitum smoking and were associated with increases in traditional measures of craving, withdrawal, and negative mood. Discriminant validity of the TCQ–SF was suggested by the increased responsivity of highly nicotine-dependent smokers compared with those who were less dependent. Highly dependent smokers (mean FTND score = 7.4) reported increased scores on TCQ–SF factors 2 and 3 compared with less dependent smokers (mean FTND score = 4.4). Factor 2 (expectancy) reflects the anticipation of positive outcomes from smoking (Table 1). Previous studies also reported that a greater degree of nicotine dependence or level of smoking was associated with greater ratings of positive smoking outcome expectancies (Copeland, Brandon, & Quinn, 1995; Sayette, Martin, Wertz, Shiffman, & Perrott, 2001). TCQ–SF Factor 3 (compulsivity) assesses the inability to control tobacco use (Table 1), a widely accepted component of addictive behavior (Lyvers, 2000). Consistent with our findings, Spinella (2005) found that frequency of tobacco use correlated directly with degree of self-reported compulsive behaviors. These data indicate that highly dependent smokers experience heightened craving with respect to positive expectancies and a lack of control over tobacco use, suggesting targets for specific behavioral interventions during treatment of nicotine dependence.
This distinction in self-reported craving between highly dependent and less dependent smokers is consistent with other studies showing differences as a function of nicotine dependence on a variety of outcome measures, including responsivity to smoking cues and tobacco deprivation (Payne, Smith, Sturges, & Holleran, 1996; van den Eijnden, Spijkerman, & Fekkes, 2003), cue-related brain activation (Smolka et al., 2006), and long-term tobacco abstinence (Ferguson et al., 2003). In the present study, there was no interaction between deprivation condition and degree of nicotine dependence. Thus, although we found that craving intensity increased after 12 hr of tobacco deprivation (Figure 1) and that TCQ–SF responses differed as a function of nicotine dependence, highly dependent and less dependent smokers were not differentially affected by the overnight deprivation manipulation. These results and those of the studies mentioned above emphasize the complex processes that underlie the manifestation of craving response in smokers across the dependence continuum.
The only racial difference we observed was that Blacks scored higher than Whites on the positive affect scale of the PANAS. This result in our adult smoking population is intriguing given the finding that negative mood was a significant predictor of smoking persistence among White (but not Black) adolescents (Griesler, Kandel, & Davies, 2002). Sex differences were observed only in the tobacco-deprived condition. Women scored higher than men on TCQ–SF Factor 1 (emotionality) and Factor 3 (compulsivity), MNWS total score, and PANAS negative affect scale. A recent review suggests that during the luteal phase of the menstrual cycle, women experience more intense nicotine withdrawal and craving (Carpenter, Upadhyaya, LaRowe, Saladin, & Brady, 2006). Because we did not control for the menstrual cycle phase of women participants, the sex differences observed in craving and withdrawal scores may have been influenced by premenstrual symptoms.
Several other limitations of the study should be mentioned. The reliability and validity of the TCQ and TCQ–SF have been investigated with smokers who were not interested in reducing or quitting smoking in this and previous studies (Heishman et al., 2003, 2004; Lee et al., 2007; Singleton et al., 2003). Thus, these results may not generalize to smokers trying to quit, former smokers, or those who are not nicotine dependent and thus do not experience strong craving or withdrawal when tobacco deprived. Finally, we have not yet investigated the utility of the TCQ–SF or TCQ in predicting treatment outcomes in smoking cessation programs. Because self-reported craving is a predictor of treatment success (Killen et al., 2006; Shiffman et al., 1997), evaluation of the TCQ–SF in a treatment trial is a next logical step in its ongoing validity and reliability testing.
Few studies have assessed the psychometric properties of self-report measures of tobacco craving or reported the consequences of changes in the length and content of the original instrument. In this study, we reported the development of a short form of the TCQ and examined its reliability and validity. Results suggest that the TCQ–SF is as valid and reliable as the 47-item TCQ in measuring tobacco craving. The use of the TCQ–SF is recommended in clinic and research settings where time may be limited, yet a multidimensional assessment of tobacco craving is desired.
Acknowledgments
We thank Dr. Susan Boyd for medical screening of participants and Eun Lee, Rudy Murillo, and Nicole Eid for their assistance with the conduct of the study. This research was supported by and performed at the Intramural Research Program of the NIH, National Institute on Drug Abuse.
Footnotes
Full terms and conditions of use: http://www.informaworld.com/terms-and-conditions-of-access.pdf
This article maybe used for research, teaching and private study purposes. Any substantial or systematic reproduction, re-distribution, re-selling, loan or sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden.
The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
Contributor Information
Stephen J. Heishman, Nicotine Psychopharmacology Unit, Clinical Pharmacology and Therapeutics Branch, Intramural Research Program, National Institute on Drug Abuse, National Institutes of Health, Baltimore, MD
Edward G. Singleton, SCenter for Prevention and Treatment Research, The MayaTech Corporation, Silver Spring, MD
Wallace B. Pickworth, Battelle Centers for Public Health Research and Evaluation, Baltimore, MD.
References
- Bell SL, Taylor RC, Singleton EG, Henningfield JE, Heishman SJ. Smoking after nicotine deprivation enhances cognitive performance and decreases tobacco craving in drug abusers. Nicotine & Tobacco Research. 1999;1:45–52. doi: 10.1080/14622299050011141. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–161. [Google Scholar]
- Browne MW, Cudeck R, Tateneni K, Mels G. CEFA: Comprehensive Exploratory Factor Analysis, Version 2.00 [Computer software and manual] 2004 Retrieved from http://quantrm2.psy.ohio-state.edu/browne/
- Carpenter MJ, Upadhyaya HP, Larowe SD, Saladin ME, Brady KT. Menstrual cycle phase effects on nicotine withdrawal and cigarette craving: A review. Nicotine & Tobacco Research. 2006;8:627–638. doi: 10.1080/14622200600910793. [DOI] [PubMed] [Google Scholar]
- Copeland AL, Brandon TH, Quinn EP. The Smoking Consequences Questionnaire-Adult: Measurement of smoking out-come expectancies of experienced smokers. Psychological Assessment. 1995;7:484–494. [Google Scholar]
- Cox LS, Tiffany ST, Christen AG. Evaluation of the brief questionnaire of smoking urges (QSU-brief) in laboratory and clinical settings. Nicotine & Tobacco Research. 2001;3:7–16. doi: 10.1080/14622200020032051. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- Drobes DJ, Tiffany ST. Induction of smoking urge through imaginal and in vivo procedures: Physiological and self-report manifestations. Journal of Abnormal Psychology. 1997;106:15–25. doi: 10.1037//0021-843x.106.1.15. [DOI] [PubMed] [Google Scholar]
- Fagerström KO, Kunze M, Schoberberger R, Breslau N, Hughes JR, Hurt RD, Puska P, Ramström L, Satonski W. Nicotine dependence versus smoking prevalence: Comparisons among countries and categories of smokers. Tobacco Control. 1996;5:52–56. doi: 10.1136/tc.5.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson JA, Patten CA, Schroeder DR, Offord KP, Eberman KM, Hurt RD. Predictors of 6-month tobacco abstinence among 1224 cigarette smokers treated for nicotine dependence. Addictive Behaviors. 2003;28:1203–1218. doi: 10.1016/s0306-4603(02)00260-5. [DOI] [PubMed] [Google Scholar]
- Griesler PC, Kandel DB, Davies M. Ethnic differences in predictors of initiation and persistence of adolescent cigarette smoking in the National Longitudinal Survey of Youth. Nicotine & Tobacco Research. 2002;4:79–93. doi: 10.1080/14622200110103197. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heinz AJ, Epstein DH, Schroeder JR, Singleton EG, Heishman SJ, Preston KL. Heroin and cocaine craving and use during treatment: Measurement validation and potential relationships. Journal of Substance Abuse Treatment. 2006;31:355–364. doi: 10.1016/j.jsat.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Heishman SJ, Boas ZP, Hager MC, Taylor RC, Singleton EG, Moolchan ET. Effect of tobacco craving cues on memory encoding and retrieval in smokers. Addictive Behaviors. 2006;31:1116–1121. doi: 10.1016/j.addbeh.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Heishman SJ, Saha S, Singleton EG. Imagery-induced tobacco craving: Duration and lack of assessment reactivity bias. Psychology of Addictive Behaviors. 2004;18:284–288. doi: 10.1037/0893-164X.18.3.284. [DOI] [PubMed] [Google Scholar]
- Heishman SJ, Singleton EG, Moolchan ET. Tobacco Craving Questionnaire: Reliability and validity of a new multifactorial instrument. Nicotine & Tobacco Research. 2003;5:645–654. doi: 10.1080/1462220031000158681. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry. 1986;43:289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- Killen JD, Fortmann SP, Murphy GM, Hayward C, Arredondo C, Cromp D, Celio M, Wang Y, Schatzberg AF. Extended treatment with bupropion SR for cigarette smoking cessation. Journal of Consulting and Clinical Psychology. 2006;74:286–294. doi: 10.1037/0022-006X.74.2.286. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York: Guilford Press; 2005. [Google Scholar]
- Koschat MA, Swayne DF. A weighted procrustes criteria. Psychometrica. 1991;56:229–239. [Google Scholar]
- Lee DC, Myers CS, Taylor RC, Moolchan ET, Berlin I, Heishman SJ. Consistency of subjective responses to imagery-induced tobacco craving over multiple sessions. Addictive Behaviors. 2007;32:2130–2139. doi: 10.1016/j.addbeh.2007.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyvers M. “Loss of control” in alcoholism and drug addiction: A neuroscientific interpretation. Experimental and Clinical Psychopharmacology. 2000;8:225–249. doi: 10.1037//1064-1297.8.2.225. [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Widaman KF, Preacher KJ, Hong S. Sample size in factor analysis: The role of model error. Multivariate Behavioral Research. 2001;36:611–637. doi: 10.1207/S15327906MBR3604_06. [DOI] [PubMed] [Google Scholar]
- Mezinskis JP, Honos-Webb L, Kropp F, Somoza E. The measurement of craving. Journal of Addictive Diseases. 2001;20:67–85. doi: 10.1300/J069v20n03_07. [DOI] [PubMed] [Google Scholar]
- Payne TJ, Smith PO, Sturges LV, Holleran SA. Reactivity to smoking cues: Mediating roles of nicotine dependence and duration of deprivation. Addictive Behaviors. 1996;21:139–154. doi: 10.1016/0306-4603(95)00043-7. [DOI] [PubMed] [Google Scholar]
- Piasecki TM. Relapse to smoking. Clinical Psychology Review. 2006;26:196–215. doi: 10.1016/j.cpr.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Sayette MA, Martin CS, Wertz JM, Shiffman S, Perrott MA. A multi-dimensional analysis of cue-elicited craving in heavy smokers and tobacco chippers. Addiction. 2001;96:1419–1432. doi: 10.1080/09652140120075152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt N. Uses and abuses of cofficient alpha. Psychological Assessment. 1996;8:350–353. [Google Scholar]
- Shiffman S, Engberg JB, Paty JA, Perz WG, Gnys M, Kassel JD, Hickcox M. A day at a time: Predicting smoking lapse from daily urge. Journal of Abnormal Psychology. 1997;106:104–116. doi: 10.1037//0021-843x.106.1.104. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JD, Elash C. Nicotine withdrawal in chippers and regular smokers: Subjective and cognitive effects. Health Psychology. 1995;14:301–309. doi: 10.1037//0278-6133.14.4.301. [DOI] [PubMed] [Google Scholar]
- Singleton EG, Anderson LM, Heishman SJ. Reliability and validity of the Tobacco Craving Questionnaire and validation of a craving-induction procedure using multiple measures of craving and mood. Addiction. 2003;98:1537–1546. doi: 10.1046/j.1360-0443.2003.00449.x. [DOI] [PubMed] [Google Scholar]
- Smolka MN, Bühler M, Klein S, Zimmermann U, Mann K, Heinz A, Braus DF. Severity of nicotine dependence modulates cue-induced brain activity in regions involved in motor preparation and imagery. Psychopharmacology. 2006;184:577–588. doi: 10.1007/s00213-005-0080-x. [DOI] [PubMed] [Google Scholar]
- Spinella M. Compulsive behavior in tobacco users. Addictive Behaviors. 2005;30:183–186. doi: 10.1016/j.addbeh.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Steiger JH. Tests for comparing elements of a correlation matrix. Psychological Bulletin. 1980;87:245–251. [Google Scholar]
- ten Berge JMF. Rotation to perfect congruence and the cross-validation of component weights across populations. Multivariate Behavioral Research. 1986;21:41–64. doi: 10.1207/s15327906mbr2101_3. [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Carter BL, Singleton EG. Challenges in the manipulation, assessment and interpretation of craving relevant variables. Addiction. 2000;95:S177–S187. doi: 10.1080/09652140050111753. [DOI] [PubMed] [Google Scholar]
- van den Eijnden R, Spijkerman R, Fekkes D. Craving for cigarettes among low and high dependent smokers: Impact of norharman. Addiction Biology. 2003;4:463–472. doi: 10.1080/13556210310001646457. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- West R, Schneider N. Craving for cigarettes. British Journal of Addiction. 1987;82:407–415. doi: 10.1111/j.1360-0443.1987.tb01496.x. [DOI] [PubMed] [Google Scholar]
- West R, Ussher M, Evans M, Rashid M. Asssessing DSM-IV nicotine withdrawal symptoms: A comparison and evaluation of five different scales. Psychopharmacology. 2006;184:619–627. doi: 10.1007/s00213-005-0216-z. [DOI] [PubMed] [Google Scholar]
- Wewers ME, Rachfal C, Ahijevych K. A psychometric evaluation of a visual analogue scale of craving for cigarettes. Western Journal of Nursing Research. 1990;12:672–681. doi: 10.1177/019394599001200508. [DOI] [PubMed] [Google Scholar]
- Wrigley CS, Neuhaus JO. The matching of two sets of factors. American Psychologist. 1955;10:418–419. [Google Scholar]