Abstract
Purpose
Identify baseline demographic and clinical factors associated with treatment failure after surgical treatment of stress urinary incontinence (SUI).
Materials & Methods
Data were obtained from 655 women randomized to Burch colposuspension or autologous rectus sling. Of those, 543 (83%) had stress failure status assessed at 24 months (269 Burch, 274 sling). Stress failure (n=261) was defined by any of the following: self-report of SUI by the Medical, Epidemiological, and Social Aspects of Aging (MESA) questionnaire, positive stress test, or re-treatment for SUI. Non-stress failure (n=66) was defined as positive 24-hr pad test (>15 ml) or any incontinent episodes by 3-day voiding diary with none of the three criteria for stress failure. Subjects not meeting any failure criteria were considered a treatment success (n=185). Adjusting for surgical treatment group and clinical site, logistic regression models were developed to predict the probability of treatment failure.
Results
Severity of urge incontinence symptoms (p=0.041), prolapse stage (p=0.013), and being post-menopausal without hormone therapy (p=0.023) were significant predictors for stress failure. Odds of non-stress failure quadrupled for every 10-point increase in MESA urge score (OR:3.93, CI:1.45,10.65) and decreased over 2 times for every 10-point increase in stress score (OR:0.36, CI:0.16,0.84). The associations of risk factors and failure remained similar regardless of surgical group.
Conclusion
Two years after surgery, risk factors for stress failure are similar after Burch and sling procedures and include greater baseline urge incontinence symptoms, more advanced prolapse, and menopausal not on HRT. Higher urge scores predicted failure by non stress-specific outcomes.
Keywords: Burch colpopexy, rectus facial sling, stress incontinence surgery, risk factors of failure
Introduction
Surgical treatment of stress urinary incontinence (SUI) in women offers relatively high success rates and immediate resolution of SUI symptoms. Failure rates for the most popular incontinence procedures vary depending on the criteria used to characterize urine loss and length of follow-up1. Reported failure rates are as high as 74%1 and may not be attributable to surgical technique alone2. Little scientific data exist to guide surgeons and patients in determining the likelihood of surgical success for an individual woman, making it difficult for surgeons to effectively prepare patients for surgery. This is especially pertinent given the rapidly increasing, but understudied, surgical options for treating SUI. If we could identify which women were at risk for surgical failure, we may be able to modify treatments according to an individual woman's needs.
Proposed risk factors for surgical failures include patient demographics,3 history of previous pelvic or incontinence surgeries, physical examination parameters,4 urodynamic variables,5 and type of anesthesia.6 However, our ability to use these variables to predict which patients are at risk for failure is limited by the fact that the previous studies are inconsistent and most are retrospective, poorly designed, underpowered, or lack consistency in evaluation and follow-up.7 Many studies did not control for potentially confounding variables, or include a robust definition of failure including the use of both subjective and objective outcome measures to define cure.
The Stress Incontinence Surgical Treatment Efficacy Trial (SISTEr) is a multisite randomized trial that compared treatment efficacy at 24 months between the Burch colposuspension and fascial sling procedures in women with stress predominant urinary incontinence (UI). The results of this clinical trial indicated that overall and stress specific success rates were higher in the group that received the sling than those that received the Burch procedures8. The purpose of this analysis and report was to identify baseline demographic and clinical variables associated with 24-month treatment failure in women undergoing surgical treatment in this randomized clinical trial.
Materials & Methods
Women planning SUI surgery were invited to participate in the trial. Eligibility requirements included documented pure or predominant SUI symptoms for at least three months and a positive standardized urinary stress test. Details of the study methods have been published previously 9. All study procedures were approved by the institutional review board of each participating clinical center and the Biostatistical Coordinating Center with written informed consent obtained from all women prior to enrollment.
Women were randomized on the day of surgery in the operating room to receive a Burch colposuspension or an autologous rectus fascial sling. Key elements of the two surgical procedures were standardized across all participating surgeons and included the use of preoperative antibiotics, skin incision length, number and type of Burch sutures, fascial sling length and width, and cystoscopic evaluation of the bladder. Because these procedures are frequently performed in conjunction with pelvic prolapse surgery, abdominal and vaginal approaches for both pelvic prolapse repair and hysterectomy were permitted. However, surgeons were required to declare which concomitant procedures would be done prior to randomization.
Baseline assessment included a complete medical history, physical examination, urodynamic evaluation and patient survey. SUI treatment failure (stress failure) was defined as self-report of SUI by the MESA questionnaire (response of sometimes or often), positive stress test (leakage on examination during cough or valsalva at a standardized bladder volume of 300 mL), or retreatment for SUI (including behavioral, pharmacologic or surgical therapies). The SUI treatment success (stress success) group was divided into two subgroups: non-SUI treatment failure (non-stress failure), defined as positive 24-hr pad test (>15 ml) or any incontinent episodes by 3-day voiding diary in the absence of any of the three criteria for stress failure, and total treatment success for those subjects not meeting any failure criteria. Data were collected by interview and clinical examination pre-operatively, at 6 weeks post-operatively, and at 3, 6, 12, 18 and 24 months post-operatively. A woman could be defined as a treatment failure by retreatment any time post surgery and by the other criteria at any time after 6 months post-surgery.
Potential variables thought to affect or be associated with treatment failure included sociodemographic characteristics (age, race/ethnicity, occupational score, education, marital status, household annual income); medical/surgical history (body mass index, vaginal parity, prior UI surgery, prior pelvic prolapse surgery, hysterectomy, menopausal status/hormone replacement treatment (HRT), diabetes, smoking status); characteristics of UI (self-reported frequency of stress and urge incontinence symptoms10, quantity of urine leakage on a 24-hour pad test, number of incontinence episodes on a 3-day voiding diary, symptom bother and incontinence-related quality of life); physical examination findings (urethral hypermobility measured by the Q-tip test, pelvic floor muscle strength, and pelvic organ prolapse). Self-reported UI was quantified by the stress and urge subscale scores from the Medical, Epidemiological and Social Aspects of Aging (MESA) questionnaire.10 Finally, because concomitant surgery might affect the outcome of the study surgery, an indicator (yes/no) of concomitant surgery was included.
To identify predictors of stress and non-stress treatment failure, bivariate logistic regression models were fit modeling the probability of stress-specific failure and non-stress failure as a function of each covariate separately, adjusting for treatment group (Burch and sling) and site. Both continuous and categorical predictors were considered. Odds ratios (ORs) and 95% confidence intervals (CIs) described the associations between clinical parameters and the outcomes. Based on significance at the 0.05 level from the bivariate logistic regression models and clinical relevance, multivariable logistic regression models were fit for each defined outcome. To assess whether the relationships between the predictors and failure were similar for each of the treatment groups, interaction terms between each predictor and treatment were considered. Interaction terms between significant main effects were also tested for inclusion in the multivariable models. Hosmer-Lemeshow goodness of fit tests were calculated to assess the fit of the models. A 5% two-sided significance level was used for all statistical testing. Analyses were performed using SAS Version 9.1 (SAS Institute, Inc. Cary, NC).
Results
Of the 655 subjects, 543 (83%) completed the stress failure assessment at 24 months. 261 patients met stress failure criteria and 282 did not. Table 1 compares the women who met the stress specific criteria for success and failure. The bivariate and multivariable analyses for stress failure are presented in Table 2. No statistically significant interactions between the covariates and treatment group were found for stress failure, implying that the relationships between each covariate and stress failure were similar for the Burch and sling groups. The multivariable models to predict stress failure were fit including treatment group, site and the following covariates: age, occupational score, body mass index, stress score, urge score, vaginal deliveries, prior surgery for urinary incontinence, menopausal status/HRT and prolapse stage.
Table 1. Selected Characteristics of Sample by Stress Success status (n=543).
| Characteristics | Stress success (n=282) |
Stress failure (n=261) |
|---|---|---|
| Demographic Characteristics | ||
| Age — years: mean (s.d.) | 51.4 (9.3) | 54.0 (10.9) |
| Racial and ethnicity group — %: | ||
| Hispanic | 10 | 11 |
| Non-Hispanic White | 77 | 73 |
| Non-Hispanic Black | 6 | 7 |
| Non-Hispanic Other | 7 | 9 |
| Marital status - % | ||
| Married/living as married | 69 | 68 |
| Not married | 31 | 32 |
| Education — %: | ||
| High School or less | 31 | 39 |
| Some post-HS training | 37 | 39 |
| Baccalaureate or more | 32 | 22 |
| Household Income — %: | ||
| <$20,000 | 16 | 23 |
| $20,000 - $49,999 | 28 | 34 |
| $50,000 - $79,999 | 21 | 20 |
| $80,000 + | 35 | 23 |
| Occupational Score: mean (s.d.) | 59.9 (25.0) | 54.5 (24.5) |
| Medical History | ||
| BMI:† mean (s.d.) | 29.5 (5.8) | 30.4(6.4) |
| Vaginal Deliveries — % | ||
| 0 | 13 | 6 |
| 1-2 | 43 | 41 |
| 3+ | 44 | 53 |
| Prior UI surgery — % | 14 | 18 |
| Prior Prolapse surgery — %: | 1 | 3 |
| Hysterectomy — %: | 30 | 34 |
| Menopausal Status/HRT Usage — %: | ||
| HRT | 37 | 33 |
| No HRT | 31 | 44 |
| Pre-menopausal | 32 | 23 |
| Diabetes — %: | 5 | 9 |
| Smoking Status-% | ||
| Never Smoked | 56 | 55 |
| Former Smoker | 32 | 33 |
| Current Smoker | 12 | 12 |
| Prolapse Stage‡ — %: | ||
| Stage 0/1 | 26 | 19 |
| Stage 2 | 62 | 59 |
| Stage 3/4 | 12 | 22 |
| Point Ba: mean (s.d.) | -0.70 (1.59) | -0.31 (1.94) |
| Point Bp: mean (s.d.) | -1.82 (1.33) | -1.53 (1.64) |
| Point Gh: mean (s.d.) | 3.51 (1.19) | 3.66 (1.21) |
| Brink Score: mean (s.d.) | 9.23 (2.01) | 8.65 (2.13) |
| Quality of Life | ||
| Total UDI Score:19 mean (s.d.) | 146.0 (48.6) | 157.9 (45.6) |
| Total IIQ Score:19 mean (s.d.) | 168.0 (101.0) | 176.7 (99.3) |
| Clinical Characteristics | ||
| Pad test weight — g: mean (s.d.) | 41.7 (69.5) | 46.3 (95.5) |
| Incontinence episodes/day: mean (s.d.) | 3.2 (3.2) | 3.2 (2.8) |
| Urinary Incontinence symptom score§ | ||
| Stress score: mean (s.d.) | 19.0 (4.8) | 19.9 (4.1) |
| Urge score: mean (s.d.) | 5.9 (3.9) | 7.4 (3.9) |
| Q-Tip test — degrees: | ||
| Resting angle: mean (s.d.) | 16.1 (18.1) | 14.3 (16.4) |
| Straining angle: mean (s.d.) | 61.6 (18.6) | 59.0 (17.9) |
| Delta = straining – resting: mean (s.d.) | 45.5 (18.3) | 44.7 (18.8) |
| Concomitant Surgery - % | ||
| None | 44 | 38 |
| Concomitant Pelvic Surgery: Prolapse repair: Anterior wall prolapse repair, +/- other repair OR | 56 | 62 |
| Prolapse repair: Other, no anterior wall prolapse repair (includes posterior wall, apex) OR | ||
| Concomitant Other Surgery (no prolapse) |
UI denotes urinary incontinence, UDI Urogenital Distress Inventory;20 and IIQ Incontinence Impact Questionnaire.20
BMI, body mass index: weight (kg) relative to square of height (m2).
Prolapse staging is based on the methods of the Pelvic Organ Prolapse Quantification System.18
UI Symptom scores: Total score on the Medical, Epidemiological and Social Aspects of Aging questionnaire.22 Response categories for each item 0 = “never” to 3 = “often.”
Table 2.
Bivariate and Multivariable Associations of Potential Predictors of Stress Failures Controlling for Treatment Group (Burch, Sling): Odds ratios (95% confidence intervals and p-values (n=543)
| Continuous predictors | Bivariate Analyses | Final Multivariable Analysis* | ||
|---|---|---|---|---|
| Adjusted Odds Ratio** (95% CI) | p-value | Adjusted Odds Ratio** (95% CI) | p-value | |
| Age (10 year increase) | 1.28 (1.08, 1.52) | 0.005 | 1.12 (0.87, 1.44) | 0.38 |
| Occupational score (10 unit increase) | 0.91 (0.85, 0.98) | 0.011 | 0.94 (0.87, 1.02) | 0.15 |
| Body mass index | 1.03 (1.00, 1.06) | 0.061 | 1.01 (0.98, 1.05) | 0.47 |
| Point Ba | 1.14 (1.03, 1.25) | 0.013 | ||
| Point Bp | 1.14 (1.01, 1.28) | 0.036 | ||
| Point Gh | 1.11 (0.96, 1.28) | 0.17 | ||
| Brink Score | 0.88 (0.81, 0.95) | 0.002 | ||
| UDI Score (10 point increase) | 1.06 (1.02, 1.10) | 0.003 | ||
| IIQ Score (10 point increase) | 1.01 (0.99, 1.03) | 0.37 | ||
| Pad test weight (10 g increase) | 1.01 (0.99, 1.03) | 0.49 | ||
| Incontinence episodes/day | 0.99 (0.93, 1.04) | 0.62 | ||
| Stress score (10 point increase) | 1.50 (1.02, 2.21) | 0.039 | 1.24 (0.75, 2.05) | 0.39 |
| Urge score (10 point increase) | 2.65 (1.69, 4.16) | <0.0001 | 1.84 (1.03, 3.30) | 0.041 |
| Resting angle (5° increase) | 0.97 (0.92, 1.02) | 0.23 | ||
| Straining angle (5° increase) | 0.96 (0.91, 1.00) | 0.068 | ||
| Delta (5° increase) | 0.98 (0.94, 1.03) | 0.49 | ||
| Categorical predictors | Adjusted Odds*** Ratio (95% CI) | p-value | ||
| Ethnicity | 0.59 | |||
| Hispanic | 0.91 (0.41, 2.03) | |||
| Non-Hispanic White | 0.73 (0.39, 1.37) | |||
| Non-Hispanic Black | 1.00 (0.41, 2.46) | |||
| Non-Hispanic Other | 1 Reference | |||
| Marital Status | 0.71 | |||
| Married/living as married | 0.93 (0.65, 1.35) | |||
| Not married | 1 Reference | |||
| Education | 0.025 | |||
| High School or less | 1 Reference | |||
| Some post-HS training | 0.81 (0.54, 1.20) | |||
| Baccalaureate or more | 0.54 (0.35, 0.85) | |||
| Household Income | 0.015 | |||
| <$20,000 | 1 Reference | |||
| $20,000 - $49,999 | 0.84 (0.50, 1.41) | |||
| $50,000 - $79,999 | 0.66 (0.37, 1.17) | |||
| $80,000 + | 0.45 (0.27, 0.77) | |||
| Vaginal Deliveries | 0.015 | 0.07 | ||
| 0 | 1 Reference | 1 Reference | ||
| 1-2 | 1.94 (1.00, 3.77) | 2.20 (1.03, 4.71) | ||
| 3+ | 2.55 (1.32, 4.93) | 2.45 (1.13, 5.28) | ||
| Prior UI surgery | 1.30 (0.82, 2.08) | 0.26 | 1.23 (0.73, 2.09) | 0.44 |
| Prior Prolapse surgery | 2.11 (0.62, 7.20) | 0.23 | ||
| Hysterectomy | 1.16 (0.81, 1.68) | 0.42 | ||
| Menopausal status/HRT | 0.003 | 0.023 | ||
| Yes | 1.20 (0.77, 1.86) | 0.94 (0.51, 1.75) | ||
| No | 2.03 (1.31, 3.14) | 1.67 (0.96, 2.89) | ||
| Pre-menopausal | 1 Reference | 1 Reference | ||
| Diabetes | 1.68 (0.85, 3.31) | 0.14 | ||
| Smoking Status | 0.92 | |||
| Never smoked | 1 Reference | |||
| Former smoker | 1.08 (0.74, 1.57) | |||
| Current smoker | 1.07 (0.62, 1.85) | |||
| Prolapse Stage | 0.002 | 0.013 | ||
| Stage 0/1 | 1 Reference | 1 Reference | ||
| Stage 2 | 1.30 (0.85, 1.99) | 1.25 (0.77, 2.02) | ||
| Stage 3/4 | 2.75 (1.56, 4.85) | 2.64 (1.34, 5.21) | ||
| Concomitant surgery | 1.27 (0.89, 1.79) | 0.18 | ||
In the multivariable analysis, clinical site is also controlled for.
Unless otherwise indicated in parentheses, odds ratios reported indicate the change in odds of stress failure for a one-unit change in the continuous predictor.
For the categorical predictors, odds ratios denote the change in the odds of stress failure compared to the referent group indicated (or not having the condition).
The covariates that continued to demonstrate a statistically significant relationship to 24-month stress failure included: urge score, menopausal without HRT and prolapse stage. Specifically, for each 10-unit increase in the urge score, odds of stress failure were 1.84 times greater. The odds of stress failure differed in the post-menopausal women depending on whether they were taking HRT or not. Compared to pre-menopausal women, menopausal patients not taking HRT had approximately 1.5 times the odds of stress failure, whereas post-menopausal women taking HRT had a lower odds of stress failure. The odds of stress failure for women with stage 3/4 prolapse were approximately 2.5 times greater than that of women with stage 0/1 prolapse. As in the bivariate analyses, no interactions between covariates and treatment group were statistically significant, nor were the interactions between main effects. The goodness-of-fit test did not reveal that the model fit was inadequate (p = 0.27).
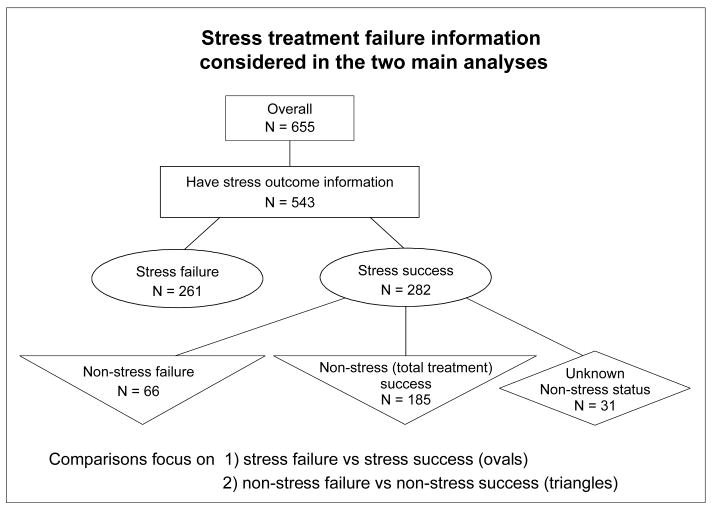
Of the 282 stress successes, 66 patients met non-stress failure criteria, 185 patients demonstrated no failure criteria and were considered total treatment successes, and 31 patients could not be classified due to missing information (Figure 1). Table 3 compares the women who met the non-stress failure criteria and those considered total treatment success. Table 4 presents the bivariate and multivariable analyses of non-stress failure in this group. The covariates that continued to demonstrate a statistically significant relationship to 24-month non-stress failure included the MESA urge and stress scores. The urge score demonstrated a positive relationship with non-stress failure, while the stress score demonstrated an inverse relationship. For each 10-point increase in the urge score, the odds of non-stress failure approximately quadrupled, while for every 10-point increase in stress score, the odds of non-stress failure decreased by over two. No interactions were statistically significant, and the goodness-of-fit test indicated reasonable model fit (p = 0.96).
Figure 1.
Table 3. Selected Characteristics of Women who met criteria for Stress success by non-Stress Success status (n=251).
| Characteristics | Non-stress success (n=185) |
Non-stress failure (n=66) |
|---|---|---|
| Demographic Characteristics | ||
| Age — years: mean (s.d.) | 51.6 (9.5) | 51.5 (9.6) |
| Racial and ethnicity group — %: | ||
| Hispanic | 9 | 14 |
| Non-Hispanic White | 76 | 77 |
| Non-Hispanic Black | 7 | 4.5 |
| Non-Hispanic Other | 8 | 4.5 |
| Marital status - % | ||
| Married/living as married | 70 | 68 |
| Not married | 30 | 32 |
| Education — %: | ||
| High School or less | 34 | 20 |
| Some post-HS training | 36 | 39 |
| Baccalaureate or more | 30 | 41 |
| Household Income — %: | ||
| <$20,000 | 15 | 18.5 |
| $20,000 - $49,999 | 31 | 24 |
| $50,000 - $79,999 | 19 | 18.5 |
| $80,000 + | 35 | 39 |
| Occupational Score: mean (s.d.) | 59.5 (24.7) | 61.7 (26.0) |
| Medical History | ||
| BMI:† mean (s.d.) | 29.2 (5.5) | 30.7 (7.0) |
| Vaginal Deliveries — % | ||
| 0 | 14 | 9 |
| 1-2 | 44 | 39 |
| 3+ | 42 | 52 |
| Prior UI surgery — % | 12 | 20 |
| Prior Prolapse surgery — %: | 1 | 3 |
| Hysterectomy — %: | 26 | 32 |
| Menopausal Status/HRT Usage — %: | ||
| HRT | 41 | 30 |
| No HRT | 26 | 38 |
| Pre-menopausal | 33 | 32 |
| Diabetes — %: | 4 | 5 |
| Smoking Status-% | ||
| Never Smoked | 53 | 61 |
| Former Smoker | 35 | 27 |
| Current Smoker | 12 | 12 |
| Prolapse Stage‡ — %: | ||
| Stage 0/1 | 24 | 27 |
| Stage 2 | 62 | 68 |
| Stage 3/4 | 14 | 5 |
| Point Ba: mean (s.d.) | -0.57 (1.68) | -1.02 (1.23) |
| Point Bp: mean (s.d.) | -1.76 (1.38) | -2.10 (1.10) |
| Point Gh: mean (s.d.) | 3.50 (1.29) | 3.42 (0.90) |
| Brink Score: mean (s.d.) | 9.29 (2.04) | 9.30 (1.84) |
| Quality of Life | ||
| Total UDI Score:19 mean (s.d.) | 146.6 (50.0) | 143.7 (47.6) |
| Total IIQ Score:19 mean (s.d.) | 166.6 (102.0) | 171.2 (104.3) |
| Clinical Characteristics | ||
| Pad test weight — g: mean (s.d.) | 40.4 (71.0) | 44.1 (62.8) |
| Incontinence episodes/day: mean (s.d.) | 3.3 (3.2) | 3.4 (3.7) |
| Urinary Incontinence symptom score§ | ||
| Stress score: mean (s.d.) | 19.1 (4.8) | 18.8 (4.8) |
| Urge score: mean (s.d.) | 5.6 (4.0) | 6.8 (3.6) |
| Q-Tip test — degrees: | ||
| Resting angle: mean (s.d.) | 16.0 (18.0) | 15.1 (17.8) |
| Straining angle: mean (s.d.) | 62.3 (19.6) | 59.6 (17.0) |
| Delta = straining – resting: mean (s.d.) | 46.3 (18.7) | 44.5 (16.4) |
| Concomitant Surgery - % | ||
| None | 42 | 48 |
| Concomitant Pelvic Surgery: Prolapse repair: Anterior wall prolapse repair, +/- other repair OR | 58 | 52 |
| Prolapse repair: Other, no anterior wall prolapse repair (includes posterior wall, apex) OR | ||
| Concomitant Other Surgery (no prolapse) |
UI denotes urinary incontinence, UDI Urogenital Distress Inventory;20 and IIQ Incontinence Impact Questionnaire.20
BMI, body mass index: weight (kg) relative to square of height (m2).
Prolapse staging is based on the methods of the Pelvic Organ Prolapse Quantification System.18
UI Symptom scores: Total score on the Medical, Epidemiological and Social Aspects of Aging questionnaire.22 Response categories for each item 0 = “never” to 3 = “often.”
Table 4.
Bivariate and multivariable associations of potential predictors of “non-stress” failures controlling for treatment group (Burch, Sling): Odds Ratios (95% confidence intervals) and p-value
| Continuous Predictor | Bivariate Analyses | Final Multivariable analysis* | ||
|---|---|---|---|---|
| Adjusted Odds Ratio** (95% CI) | p-value | Adjusted Odds Ratio** (95% CI) | p-value | |
| Age (10 year increase) | 1.00 (0.74, 1.34) | 0.98 | 0.97 (0.62, 1.50) | 0.88 |
| Occupational score (10 unit increase) | 1.04 (0.92, 1.16) | 0.54 | 1.11 (0.97, 1.27) | 0.12 |
| Body mass index | 1.04 (0.99, 1.09) | 0.088 | 1.04 (0.98, 1.10) | 0.23 |
| Point Ba | 0.82 (0.67, 1.00) | 0.046 | ||
| Point Bp | 0.79 (0.61, 1.03) | 0.079 | ||
| Point Gh | 0.94 (0.74, 1.20) | 0.63 | ||
| Brink Score | 1.00 (0.87, 1.16) | 0.97 | ||
| UDI Score (10 point increase) | 0.99 (0.93, 1.05) | 0.70 | ||
| IIQ Score (10 point increase) | 1.01 (0.98, 1.03) | 0.73 | ||
| Pad test weight (10 g increase) | 1.01 (0.97, 1.05) | 0.70 | ||
| Incontinence episodes/day | 1.01 (0.93, 1.10) | 0.79 | ||
| Stress score (10 point increase) | 0.88 (0.49, 1.59) | 0.68 | 0.36 (0.16, 0.84) | 0.017 |
| Urge score (10 point increase) | 2.18 (1.07, 4.48) | 0.033 | 3.93 (1.45, 10.65) | 0.007 |
| Resting angle (5° increase) | 0.99 (0.91, 1.07) | 0.74 | ||
| Straining angle (5° increase) | 0.96 (0.89, 1.04) | 0.33 | ||
| Delta (5° increase) | 0.97 (0.90, 1.05) | 0.49 | ||
| Categorical predictors | Adjusted Odds*** Ratio (95% CI) | p-value | ||
| Ethnicity | 0.57 | |||
| Hispanic | 2.54 (0.58, 11.23) | |||
| Non-Hispanic White | 1.74 (0.48, 6.30) | |||
| Non-Hispanic Black | 1.16 (0.19, 6.93) | |||
| Non-Hispanic Other | 1 Reference | |||
| Marital Status | 0.80 | |||
| Married/living as married | 0.93 (0.51, 1.70) | |||
| Not married | 1 Reference | |||
| Education | 0.075 | |||
| High School or less | 1 Reference | |||
| Some post-HS training | 1.88 (0.89, 3.99) | |||
| Baccalaureate or more | 2.39 (1.12, 5.08) | |||
| Household Income | 0.67 | |||
| <$20,000 | 1 Reference | |||
| $20,000 - $49,999 | 0.58 (0.23, 1.47) | |||
| $50,000 - $79,999 | 0.72 (0.27, 1.94) | |||
| $80,000 + | 0.83 (0.35, 1.99) | |||
| Vaginal Deliveries | 0.35 | 0.21 | ||
| 0 | 1 Reference | 1 Reference | ||
| 1-2 | 1.44 (0.53, 3.91) | 1.99 (0.61, 6.43) | ||
| 3+ | 1.93 (0.73, 5.12) | 2.78 (0.86, 8.95) | ||
| Prior UI surgery | 1.83 (0.86, 3.90) | 0.11 | 1.88 (0.75, 4.67) | 0.18 |
| Prior Prolapse surgery | 2.93 (0.40, 21.29) | 0.29 | ||
| Hysterectomy | 1.30 (0.71, 2.40) | 0.40 | ||
| Menopausal status/HRT | 0.15 | 0.57 | ||
| Yes | 0.80 (0.40, 1.60) | 0.73 (0.27, 1.97) | ||
| No | 1.56 (0.78, 3.11) | 1.13 (0.45, 2.85) | ||
| Pre-menopausal | 1 Reference | 1 Reference | ||
| Diabetes | 1.21 (0.30, 4.84) | 0.79 | ||
| Smoking Status | 0.48 | |||
| Never smoked | 1 Reference | |||
| Former smoker | 0.67 (0.35, 1.28) | |||
| Current smoker | 0.89 (0.36, 2.16) | |||
| Prolapse Stage | 0.14 | 0.13 | ||
| Stage 0/1 | 1 Reference | 1 Reference | ||
| Stage 2 | 0.96 (0.50, 1.83) | 0.87 (0.41, 1.86) | ||
| Stage 3/4 | 0.28 (0.08, 1.05) | 0.22 (0.05, 0.99) | ||
| Concomitant surgery | 0.76 (0.43, 1.34) | 0.34 | ||
In the multivariable analysis, clinical site is also controlled for.
Unless otherwise indicated in parentheses, odds ratios reported indicate the change in odds of non-stress failure for a one-unit change in the continuous predictor.
For the categorical predictors, odds ratios denote the change in the odds of non-stress failure compared to the referent group indicated (or not having the condition).
Discussion
Two years after surgery, risk factors for recurrent or persistent SUI were similar in women undergoing Burch colposuspension and autologous rectus fascial sling procedures. In contrast to previous studies, this randomized controlled trial did not find a significant impact of many commonly reported “risk factors,” such as age, BMI, prior UI surgery, prior hysterectomy and diabetes mellitus, on continence outcomes11-15.
The major finding in this study is that patients with higher urge scores demonstrated higher stress specific failure as well as overall failure. Therefore, it seems possible that urge symptoms are not merely a reflection of more urge incontinence episodes, but are associated with persistent or recurrent stress incontinence. In women with mixed incontinence, the underlying pathophysiology may be that the urge symptoms serve as a surrogate or manifestation of an intrinsic deficiency of the urethral sphincter from more advanced neuromuscular dysfunction, which may not be easily cured with continence surgery. Chaliha et al16 demonstrated that the normally observed increase in urethral pressure with bladder filling was not observed in patients with detrusor overactivity. This may suggest a primary urethral dysfunction in patients with urge incontinence symptoms.
Women with stage 3 or 4 prolapse were 2.5 times more likely than women without prolapse to have persistent or recurrent SUI. Advanced prolapse could be a manifestation of more extensive damage to the pelvic floor musculofascial support, its innervation, or its ultrastructural composition of elastin and collagen17. This finding is consistent with the observation of Daneshgari et al15 who found that pelvic organ prolapse and concomitant rectocele repair increased the risk of recurrent SUI. The finding that Burch and sling outcomes are worse in women with advanced pelvic organ prolapse cannot necessarily be extrapolated to other continence surgeries. Certainly, for the mid-urethral sling procedures, caution is recommended when quoting outcomes based on trials that exclude women with prolapse until more evidence becomes available in this group of women.
The results of this study contribute to the controversy over the relationship between estrogen status and continence. Contrary to others15,18, our data indicate that menopausal women not taking HRT were twice as likely to experience persistent or recurrent SUI after surgery compared to those taking HRT. These data are typically confounded by difficulty in assuring the duration of use as well as dosage and specific hormonal replacement regimens used. HRT may correct the hypoestrogenism associated with atrophic, thinner tissue and improve neuromuscular function as shown in animal models in which gonadal steroids had important neuro-regenerative effects on peripheral motor nerves19,20.
Our study findings are strengthened by our study design, a multi-center randomized trial with diverse surgeons from both urology and urogynecology, which contributes to the study's generalizability and limits potential biases. In addition, we had clearly defined and validated objective and subjective outcome measures and good follow-up for a 2-year period. Our conclusions are limited by the lack of information on the urodynamic studies done at 2 years, which will be reported in a separate paper.
Conclusion
In summary, patients with higher urge scores demonstrated higher stress specific failure as well as overall failure 2 years after surgery for stress predominant UI. Risk factors for persistent or recurrent SUI after a Burch or sling procedure are similar 2 years after surgery. These risk factors are potentially modifiable by separately addressing and treating concomitant pelvic floor disorders, such as urge incontinence, advanced prolapse, and/or hormone therapy. These observations might assist in counseling patients regarding the long-term efficacy of these 2 surgical procedures and discussing reasonable expectations, and proactively addressing the modifiable risk factors of urge incontinence and need for hormone replacement therapy.
Acknowledgments
Heather Litman had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (U01 DK58225, U01 DK58234, U01 DK58229, U01 DK58231, U01 DK60397, U01 DK60401, U01 DK60395, U01 DK60393, U01 DK60380, U01 DK60379 and K24 DK068389). Additional support provided by the National Institute of child Health and Human Development.
Steering Committee William Steers, MD, Chair (University of Virginia Charlottesville VA); Ananias C. Diokno, MD, Veronica Mallett, MD (William Beaumont Hospital, Royal Oak, MI and Oakwood Hospital, Dearborn MI; U01 DK58231); Linda Brubaker, MD, MaryPat FitzGerald, MD (Loyola University Medical Center, Maywood, IL; U01 DK60379); Holly E. Richter, PhD, MD, L. Keith Lloyd, MD (University of Alabama, Birmingham, AL; U01 DK60380); Michael Albo, MD, Charles Nager, MD (University of California, San Diego, CA; U01 DK60401); Toby Chai, MD, Harry W. Johnson, MD (University of Maryland, Baltimore, MD; U01 DK60397); Halina M. Zyczynski, MD, Michael Chancellor, MD, Wendy Leng, MD (University of Pittsburgh, Pittsburgh, PA; U01 DK58225); Philippe Zimmern, MD, Gary Lemack, MD (University of Texas Southwester, Dallas, TX; U01 DK60395); Stephen Kraus, MD, R. Duane Cespedes, MD (University of Texas Health Sciences Center, San Antonio, TX; U01 DK58234); Peggy Norton, MD, Lindsey Kerr, MD (University of Utah, Salt Lake city, UT; U01 DK60393); Sharon Tennstedt, PhD, Anne Stoddard, ScD (New England Research Institutes, Watertown, MA; U01 DK58229); John W. Kusek, PhD, Leroy M. Nyberg, MD, PhD (National Institute of Diabetes & Digestive & Kidney Diseases); Anne M. Weber, MD (National Institute of Child Health and Human Development).
Co-Investigators Jan Baker, APRN; Diane Borello-France, PT, PhD; Kathryn L. Burgio, PhD; Seine Chiang, MD; Ash Dabbous, MD; Patricia S. Goode, MD; Lee N. Hammontree, MD; Kimberly Kenton, MD; Salil Khandwala, MD; David Lesser, MD; Karl Luber, MD; Emily Lukacz, MD; Alayne Markland, MD; Shawn Menefee, MD; Pamela Moalli, MD; Mikio Nihira, MD; Kenneth Peters, MD; Curt Powell, MD; Elizabeth Sagan, MD; Joseph Schaffer, MD; Amanda Simsiman, MD; Larry Sirls, MD; Robert Starr, MD; R. Edward Varner, MD.
Study Coordinators Rosemary Bradt, RNC; Karen Debes, RN; Rosanna Dinh, RN; Judy Gruss, RN; Lynn Hall, RN, MSN, CURN; Alice Howell, RN, BSN, CCRC; Kathy Jesse, RN; D. Lynn Kalinoski, PhD; Kathryn Loches, RN; Barbara Leemon, RN; Karen Mislanovich, RN; Judith Murray, CCRC; Shelly O'Meara, RN; Norma Pope, RN, WHNP; Caren Prather, RN; Sylvia Sluder, CCRP; Mary Tulke, RN; Gisselle Zazueta-Damian, Research Assistant.
Biostatistical Coordinating Center Kimberly J. Dandreo, MSc; Corinne J. Leifer, BA; Heather Litman, PhD, Susan M. McDermott, MPH, GNP; Anne Stoddard, ScD (Co-PI); Sharon Tennstedt, PhD (PI); Liane Tinsley, BA; Yan Xu, MS.
Abbreviations
- SUI
Stress Urinary Incontinence
- MESA
Medical, Epidemiological & Social Aspects of Aging
- UI
Urinary Incontinence
- HRT
Hormone Replacement Therapy
- OR
Odds Ratio
- CI
Confidence Interval
- UDI
Urogenital Distress Inventory
- BMI
Body Mass Index
- IIQ
Incontinence Impact Questionnaire
- UDI
Urogenital Distress Inventory
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ward K, Hitlon P on Behalf of the United Kingdom and Ireland Tension Free Vaginal Tape Trial Group. Prospective Multicentre Randomized Trial of Tension Free Vaginal Tape and Colposuspension as Primary Treatment for Stress Incontinence. BMJ. 2002;325:67. doi: 10.1136/bmj.325.7355.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sand PK, Bowen LW, Ostergard DR, Nakanishi AM. Hysterectomy and prior incontinence surgery as risk factors for failed retropubic cystourethropexy. JRM. 1988;33:171. [PubMed] [Google Scholar]
- 3.Salin A, Conquy S, Elie C, Touboul C, Parra J, Zerbib M, et al. Identification of risk factors for voiding dysfunction following TVT placement. European Urology. 2007;51:782. doi: 10.1016/j.eururo.2006.10.056. [DOI] [PubMed] [Google Scholar]
- 4.Meschia M, Pifarotti P, Gate U, Bertozzi R. Tension-free vaginal tape: analysis of risk factors for failure. Int Urogynecol J. 2007;18:419. doi: 10.1007/s00192-006-0161-3. [DOI] [PubMed] [Google Scholar]
- 5.Bowen LW, Sand PK, Ostergard DR, Franti CE. Unsuccessful Burch retropubic urethropexy: A case-controlled urodynamic study. Am J Obstet Gynecol. 1989;160:452. doi: 10.1016/0002-9378(89)90471-7. [DOI] [PubMed] [Google Scholar]
- 6.Deval B, Jeffry L, Al Najjar F, Soriano D, Darai E. Determinants of patient dissatisfaction after a tension-free vaginal tape procedure for urinary incontinence. J Urol. 2002;167:2093. [PubMed] [Google Scholar]
- 7.Black NA, Downs SH. The effectiveness of surgery for stress incontinence in women: a systematic review. Br J Urol. 1996;78:497. doi: 10.1046/j.1464-410x.1996.01422.x. [DOI] [PubMed] [Google Scholar]
- 8.Albo ME, Richter HE, Brubaker L, Norton P, Kraus SR, Zimmern PE, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med. 2007;356:13. doi: 10.1056/NEJMoa070416. [DOI] [PubMed] [Google Scholar]
- 9.Tennstedt S Urinary Incontinence Treatment Network. Design of the Stress Incontinence Surgical Treatment Efficacy Trial (SISTEr) Urology. 2005;66:1213. doi: 10.1016/j.urology.2005.06.089. [DOI] [PubMed] [Google Scholar]
- 10.Herzog AR, Diokno AC, Brown MB, Normolle DP, Brock BM. Two-year incidence, remission, and change patterns of urinary incontinence in noninstitutionalized older adults. J Gerontol. 1990;45:M67. doi: 10.1093/geronj/45.2.m67. [DOI] [PubMed] [Google Scholar]
- 11.Stanton SL, Cardozo L, Williams JE, Ritchie D, Allan V. Clinical and urodynamic features of failed incontinence surgery in the female. Obstet Gynecol. 1978;51:515. doi: 10.1097/00006250-197805000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Berglund AL, Eisemann M, Lalos A, Lalos O. Predictive factors of the outcome of primary surgical treatment of stress incontinence in women. Scand J Urol Nephrol. 1997;31:49. doi: 10.3109/00365599709070302. [DOI] [PubMed] [Google Scholar]
- 13.Alcalay M, Monga A, Stanton SL. Burch colposuspension: a 10-20 year follow up. Br J Obstet Gynaecol. 1995;102:740. doi: 10.1111/j.1471-0528.1995.tb11434.x. [DOI] [PubMed] [Google Scholar]
- 14.Bowen LW, Sand PK, Ostergard DR, Franti CE. Unsuccessful Burch retropubic urethropexy: a case-controlled urodynamic study. Am J Obstet Gynecol. 1989;160:452. doi: 10.1016/0002-9378(89)90471-7. [DOI] [PubMed] [Google Scholar]
- 15.Daneshgari F, Moore C, Frinjari H, Babineau D. Patient related risk factors for recurrent stress urinary incontinence surgery in women treated at a tertiary care center. J Urol. 2006;176:1493. doi: 10.1016/j.juro.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 16.Chaliha C, Digesu GA, Salvatore S, Khullar V, Athanasiou S. Changes in urethral resistance in the presence of detrusor activity. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:215. doi: 10.1007/s00192-005-1363-9. [DOI] [PubMed] [Google Scholar]
- 17.Karam JA, Vazquez DV, Lin VK, Zimmern PE. Elastin expression and elastic fibre width in the anterior vaginal wall of postmenopausal women with and without prolapse. BJU International. 2007 May;100:346. doi: 10.1111/j.1464-410X.2007.06998.x. 2006. [DOI] [PubMed] [Google Scholar]
- 18.Sun MJ, Ng SC, Tsui KP, Chang NE, Lin KC, Chen GD. Are there any predictors for failed Burch colposuspension? Taiwan J Obstet Gynecol. 2006;45:33. doi: 10.1016/S1028-4559(09)60187-X. [DOI] [PubMed] [Google Scholar]
- 19.Tanzer L, Jones KJ. Gonadal steroid regulation of hamster facial nerve regeneration: effects of dihydrotestosterone and estradiol. Exp Neurol. 1997;146:258. doi: 10.1006/exnr.1997.6529. [DOI] [PubMed] [Google Scholar]
- 20.Tetzlaff JE, Huppenbauer CB, Tanzer L, Alexander TD, Jones KJ. Motoneuron injury and repair: New perspectives on original gonadal steroids as neurotherapeutics. J Mol Neurosci. 2006;28:53. doi: 10.1385/jmn:28:1:53. [DOI] [PubMed] [Google Scholar]