Abstract
The relationship between hantaviruses and their reservoir hosts is not well understood. We successfully passaged a mouse-adapted strain of Sin Nombre virus from deer mice (Peromyscus maniculatus) by i.m. inoculation of 4- to 6-wk-old deer mouse pups. After inoculation with 5 ID50, antibodies to the nucleocapsid (N) antigen first became detectable at 14 d whereas neutralizing antibodies were detectable by 7 d. Viral N antigen first began to appear in heart, lung, liver, spleen, and/or kidney by 7 d, whereas viral RNA was present in those tissues as well as in thymus, salivary gland, intestine, white fat, and brown fat. By 14 d nearly all tissues examined displayed both viral RNA and N antigen. We noted no consistent histopathologic changes associated with infection, even when RNA load was high. Viral RNA titers peaked on 21 d in most tissues, then began to decline by 28 d. Infection persisted for at least 90 d. The RNA titers were highest in heart, lung, and brown fat. Deer mice can be experimentally infected with Sin Nombre virus, which now allows provocative examination of the virus-host relationship. The prominent involvement of heart, lung, and brown fat suggests that these sites may be important tissues for early virus replication or for maintenance of the virus in nature.
Hantaviruses are rodent-borne pathogens with a worldwide distribution. As with other members of the family Bunyaviridae, hantaviruses are enveloped, negative-sense RNA viruses with a tripartite genome. Hantaviruses cause two human illnesses, hemorrhagic fever with renal syndrome (HFRS) and hantavirus cardiopulmonary syndrome (HCPS) (1). HCPS is now preferred by some authors over hantavirus pulmonary syndrome so as to help educate clinicians about the great importance of cardiac failure as a cause of death in HCPS patients. HFRS occurs in Asia and Europe, with a case fatality ratio of 0.1% to 10%. HCPS was first recognized after a 1993 outbreak in the Four Corners region of the southwestern United States (1–3). HCPS occurs only in North and South America (4). In North America, Sin Nombre virus (SNV) has been responsible for the large majority (>95%) of the approximately 300 cases recorded. The case-fatality ratio of HCPS is approximately 45%. The deer mouse (Peromyscus maniculatus) is the predominant carrier of SNV (5).
Little is known about the relationship between SNV and its rodent host, in part because no animal model is available (6). One reason such models have not yet been developed may be the requirement for high biological containment of the infected host rodent. Although the hantaviruses can be propagated in tissue culture at biosafety level 3, indoor handling of infected rodents requires containment at biosafety level 4 (7). However, it is safe to handle infected reservoir rodents in an outdoor setting if one uses respirators and barrier precautions and properly disposes of contaminated waste (8).
All four North American agents of HCPS have been isolated in cell culture. Of these viruses, New York virus and one strain of SNV were passed briefly through reservoir rodents before propagation in cell culture (9–14). Animal infection studies were not further developed. Black Creek Canal virus, which has been linked to only one case of HCPS, is the only New World hantavirus for which there is an animal infection model (15). The development of an animal model for infection with SNV is important for studies of the host-pathogen relationship and for development of vaccines and antiviral therapeutics. Using an outdoor quarantine laboratory, we show that deer mice can be used as an experimental model for SNV infection and demonstrate that during acute infection the virus shows a predilection for lung, heart, and brown fat.
Materials and Methods
Safety Precautions.
We adhered strictly to the biosafety recommendations of the United States Centers for Disease Control and Prevention (CDC) in all aspects of this work (7, 8). Workers wearing respirators and personal protective gear carried out all inoculations and manipulations of infected animals in the outdoor quarantine facility as described (8, 16). Propagation of the CC107 strain of SNV in tissue culture was conducted at biosafety level 3 (CDC registration number 19990408–665).
Animal Handling and Viral Inoculations.
Animals were handled according to University of New Mexico animal research facility guidelines by using an approved protocol. For blood samples collected for nonterminal experiments, animals were anesthetized with methoxyfluorane and blood was collected from the retro-orbital sinus. For terminal experiments, we used tribromoethanol for euthanasia. We homogenized tissues outdoors with a Bead-Beater homogenizer (BioSpec Products, Bartlesville, OK). Homogenates intended for inoculation were washed from the homogenization tube with a 10-fold excess of MEM. Sham-inoculated control mice were injected i.m. with tissue homogenates from an uninfected mouse. We extracted RNA by acid-phenol extraction in 4 M guanidinium chloride (3, 17). For histopathology and immunohistochemistry, we placed tissues in 10% neutral buffered formalin for at least 24 h before embedding them in paraffin (18).
Strip Immunoblot Assay.
We used a strip immunoblot assay for detection of antibodies to SNV nucleocapsid (N) antigen (19, 20). In separate lanes, we loaded 2 ml of 2 μl/ml deer mouse serum in PBS for a 3+ intensity control, a 0.2 μl/ml dilution of serum for a 1+ intensity control, and 3 μg of recombinant, affinity-purified SNV N antigen (20). The antigens were suctioned onto a wetted nitrocellulose membrane under vacuum. The membrane was cut lengthwise with a paper shredder into 1.6-mm strips, and each strip was placed into a well in a Western blot tray containing 1 ml of milk-PBS buffer and 5 μl of rodent periorbital sinus blood. The membranes were rocked gently overnight at room temperature. We applied a 1:1,000 dilution of alkaline phosphatase-conjugated goat anti-Peromyscus leucopus IgG antibodies (Kirkegaard & Perry) and rocked gently for 1 h. Bound alkaline phosphatase then was detected with nitroblue tetrazolium and 5-bromo-4-chloro-3-indoyl-phosphate substrate (21).
Immunohistochemistry (IHC).
IHC was performed with a hyperimmune polyclonal rabbit serum directed against the recombinant N antigen of SNV strain 3H226 (3, 18, 21, 22). We fixed tissues in 10% buffered formalin, embedded them in paraffin, then cut them into 4- to 6-μm sections. We mounted the sections on glass slides coated with poly-l Lys, deparaffinized them, and then stained them with the antiserum (1:10,000) on an automated processor after antigen retrieval as described (18). The immune complexes were detected with a biotinylated anti-rabbit secondary antibody, then a horseradish peroxidase-avidin conjugate, followed by detection with an amino-ethyl carbazole chromagen. Specific stain consisted of punctate, cytoplasmic granules. After applying hematoxylin as a counterstain, we mounted the slides with aqueous mounting media (18). Scoring was performed visually on a scale of 0 to 4+ intensity. Preimmune rabbit serum was extensively used initially to verify the specificity of the test during the development of the IHC procedure. We did not observe nonspecific staining in multiple studies using the preimmune serum with tissues from infected and uninfected deer mice and humans.
Nested Reverse Transcription (RT)-PCR.
Aliquots of 10–200 mg of tissue or 70–100 μl of blood from deer mice were used to prepare RNA. RNA derived from 2.5 mg of tissue was loaded in each PCR, except for blood, where we used RNA extracted from 7.5 μl per reaction. We used primers for the small (S) genomic segment of SNV. We first used single tube RT reactions and PCRs with outer primers, then conducted nesting reactions with internal primers as described (3, 17, 23). The coordinates of the outer primers were at 167 and 423 on the S segment of the NMR11 strain (GenBank accession no. L37904), whereas the inner primers were at 190 and 401. The sequences are available on request.
Focus Reduction Neutralization Test (FRNT).
Serially diluted (1:20 through 1:1,280) serum samples from infected mice were examined by FRNT individually in 48-well tissue culture plates as described (24). Diluted sera were mixed with equal volumes of 45 focus-forming units of SNV (strain CC107) for 1 h at 37° before incubation on Vero E6 cells. After adsorption for 4 h at 37°, cells were overlaid with media containing 1.2% methylcellulose for 7 d. The methylcellulose layer then was removed and the cells were fixed with methanol containing 0.5% H2O2. We then added rabbit anti-SNV N protein serum (1:5,000) followed by peroxidase-conjugated goat anti-rabbit IgG followed by diaminobenzoine-metal substrate (Pierce). The neutralization activity of a serum was expressed as the maximum dilution that would reduce the number of foci by 80% (24).
Quantitative TaqMan RT-PCR.
We used a PE Biosystems 5700 sequence detection system and the two-step TaqMan Gold RT-PCR protocol as described by the manufacturer. Each sample was tested in triplicate. For RT, 5 μl of template was mixed with random hexamers as primers in a volume of 100 μl at 25o for 10 min, 48o for 30 min, and 95o for 5 min. Five microliters of cDNA was removed for subsequent PCRs. The S segment primers used for the PCR were coordinate 179-sense GCAGACGGGCAGCTGTG and coordinate 245-antisense AGATCAGCCAGTTCCCGCT. The fluorescent probe was a positive-sense oligonucleotide at coordinate 198, TGCATTGGAGACCAAACTCGGAGAACTT. The probe was covalently labeled with the reporter dye FAM at the 5′ end and quencher dye TAMRA at the 3′ end (PE Biosystems). All oligonucleotides were used at 200 nM.
During the reaction, the quencher was dissociated from the reporter by endonucleolytic cleavage of the probe, and a sample was judged positive when the FAM fluorescence exceeded 0.05 reporter units. In our experiments, all curves that exceeded that value progressed with the expected sigmoid amplification curve in later cycles. At the point that the absorption curve exceeded 0.05 units, the threshold cycle number was determined, which is inversely related to the template copy number. PCR was conducted at 95o for 10 min, followed by 40 repetitions of 95o for 10 s, 50o for 10 s, then 72o for 30 s. A standard curve containing dilutions ranging from five copies to 5 × 107 copies of template was used on each 96-well plate. All of our standard curves produced a −0.995 or better correlation coefficient between the log of the quantity of template loaded and the cycle number value.
Sequencing.
To examine whether SN77734 had undergone mutations during passage from the wild-caught specimen NK77734 and later passages in deer mice, we compared 2.3 kb of M segment and 1.6 kb of S segment sequence from the lungs of NK77734 and those of passage 3 specimen 2450, using direct sequencing of viral amplification products.
Results
Establishment of a Deer Mouse Colony.
We trapped wild P. maniculatus rufinus from central New Mexico. Seronegative animals (n = 69) were placed in quarantine for 5 wk in individual nest boxes, spaced 3 m apart (16). After quarantine, one animal (NK77734) seroconverted and was killed. The remaining 68 mice were used to found a breeding colony at the University of New Mexico (J.B., R.R., and B.H., unpublished work).
Isolation of SN77734.
We inoculated 18 4- to 6-wk-old colony-bred deer mice with a tissue homogenate consisting of pooled, frozen-thawed lung, spleen, and kidney from mouse NK77734. The 18 mice received 100 μl of either a 1:10 (n = 6), 1:100 (n = 6), or 1:1,000 (n = 6) dilution of the homogenate in MEM, either i.m. or s.c. We collected blood at 5 d, 12 d, and 19 d postinoculation (pi) and examined them for viral RNA by nested RT-PCR and for seroreactivity to N antigen. One mouse, which had been inoculated i.m. with a 1:1,000 dilution, was positive for antibodies and SNV RNA by day 19. It was killed at 21 d, and a second viral stock was prepared from a pooled homogenate of heart, lung, spleen, kidney, and salivary gland.
The titer of this homogenate was approximately 3 × 105/ml animal ID50 by endpoint dilution by i.m. inoculation into deer mouse pups. Although this first-passage (P1) stock was infectious at titers of about 3 × 105 in deer mice, we were unable to infect greater than 50–70% of the animals we inoculated at any dilution. In an attempt to improve the infection efficiency, we inoculated two juvenile deer mice i.m. with 1,000 ID50 of the P1 stock, and after detecting viral RNA in their blood on day 14, killed them on day 15. Heart, lung, kidney, liver, and spleen were homogenized to make a P2 stock. This stock had an i.m. ID50 of 5 × 104. In contrast to the P1 stock, the P2 stock reliably infected 100% of mice regardless of the dose (n = 39). The P2 stock was used for all subsequent infections.
Sequence Analysis.
Of 3,957 total bases examined of the M and S genomes of the virus from the wild-caught deer mouse NK77734 and a passage 3 specimen, 2450, there were no changes (data not shown). A complete sequence analysis will be necessary to determine whether experimental passage of SN77734 through deer mice may have selected for a genetic variant that is more readily transmitted under our experimental conditions than the original wild virus. We intend to conduct that study after several more deer mouse passages. However, because SN77734 differed by 3% or more from any SN virus genomic sequence that is available in GenBank, it is clear that SN77734 is a new strain of SN virus.
Kinetics of Experimental Infection.
Juvenile deer mice (n = 31) were inoculated with five ID50 of the P2 stock. Fifteen juvenile deer mice were inoculated with tissue homogenate from a seronegative animal that had been prepared identically. We killed groups of animals on days 7, 14, 21, 28, and 35 d pi, examining a minimum of five infected mice and three control mice at each interval (Table 1). That infection had occurred could not be confirmed in two of the seven animals that were killed at 7 d, but infections were confirmed by nested RT-PCR, IHC, and/or serology in the remaining 29 specimens (Fig. 1; Table 1).
Table 1.
Distribution of viral N antigen by tissue, development of anti-N and neutralizing antibodies, and viral RNA in blood
| Days pi | Animal | Immunohistochemistry results
|
Blood results
|
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bladder | Brain | Heart | Intestine | Kidney | Liver | Lung | Ovary | Pancreas | Salivary | Spleen | Testis | Thymus | Uterus | B. fat | W. fat | Blood RT-PCR | Anti-N Ab | Neut. Ab titer | ||
| d7 | 2469 | 0+ | 0+ | 0+ | 0+ | 1+ | 0+ | 0+ | NA | 0+ | 0+ | 0+ | 0+ | 0+ | NA | 0+ | 0+ | − | − | <20 |
| 2470 | 0+ | 0+ | nd | 0+ | 0+ | 0+ | 0+ | nd | 0+ | nd | 0+ | nd | 0+ | nd | 0+ | 0+ | − | − | <20 | |
| 2471 | nd | 0+ | 0+ | nd | nd | 0+ | 1+ | NA | nd | nd | 0+ | 0+ | nd | NA | 0+ | 0+ | + | − | 20 | |
| 2473 | 0+ | 0+ | 0+ | 0+ | 0+ | 0+ | 0+ | NA | 0+ | 0+ | nd | 0+ | 0+ | NA | 0+ | 0+ | − | − | <20 | |
| 2474 | 0+ | 0+ | 0+ | 0+ | nd | 0+ | 0+ | nd | 0+ | 0+ | 0+ | nd | 0+ | nd | 0+ | 0+ | − | − | <20 | |
| 2475 | 0+ | 0+ | 1+ | 0+ | 0+ | 1+ | 1+ | NA | 0+ | 0+ | 1+ | 0+ | 0+ | NA | 0+ | 0+ | − | − | <20 | |
| 2476 | 0+ | 0+ | 0+ | 0+ | 0+ | 0+ | 0+ | NA | 0+ | 0+ | 0+ | 0+ | 0+ | NA | 0+ | 0+ | − | − | 20 | |
| d14 | 2463 | 0+ | 0+ | 2+ | 1+ | 1+ | 1+ | 2+ | NA | 1+ | 1+ | 2+ | 0+ | 0+ | NA | 2+ | 2+ | − | − | 80 |
| 2464 | 0+ | 0+ | 2+ | 1+ | 2+ | 2+ | 3+ | 0+ | 2+ | 2+ | 1+ | NA | 0+ | 0+ | 3+ | 2+ | + | + | 80 | |
| 2465 | 0+ | 0+ | 2+ | nd | 2+ | 2+ | 1+ | 0+ | 2+ | 1+ | 1+ | NA | 0+ | 0+ | 2+ | 1+ | − | − | 80 | |
| 2466 | 0+ | 0+ | 3+ | 0+ | 1+ | 3+ | 2+ | nd | 1+ | 1+ | 1+ | NA | 0+ | 0+ | 2+ | 2+ | + | + | 80 | |
| 2467 | 0+ | 0+ | 0+ | 0+ | 0+ | 0+ | 0+ | nd | 0+ | nd | 0+ | NA | 0+ | 0+ | 0+ | 0+ | − | − | 80 | |
| 2468 | 2+ | 0+ | 4+ | 0+ | 3+ | 3+ | 3+ | nd | 2+ | 1+ | 1+ | NA | 1+ | 0+ | 3+ | 4+ | + | + | 80 | |
| d21 | 2458 | 0+ | 0+ | 3+ | 0+ | 2+ | 1+ | 3+ | 0+ | 0+ | 0+ | 1+ | NA | nd | 0+ | 3+ | 2+ | + | + | 320 |
| 2462 | 0+ | 0+ | 3+ | 0+ | 1+ | 2+ | 3+ | nd | 0+ | 0+ | 0+ | NA | 0+ | 0+ | 2+ | 2+ | + | + | 320 | |
| 5139 | 1+ | 1+ | 4+ | 2+ | 3+ | 3+ | 4+ | NA | nd | 2+ | nd | 0+ | nd | NA | 4+ | 3+ | + | + | 1,280 | |
| 2450 | nd | 1+ | 3+ | 0+ | 2+ | 2+ | 4+ | NA | 2+ | 1+ | 2+ | 0+ | 1+ | NA | 3+ | 3+ | + | + | 320 | |
| 2477 | 0+ | 1+ | 3+ | 0+ | 1+ | 2+ | 3+ | NA | 2+ | 0+ | 1+ | 0+ | 1+ | NA | 3+ | 2+ | + | + | 640 | |
| 2481 | 1+ | 0+ | 4+ | 0+ | 2+ | 2+ | 4+ | 0+ | 2+ | 1+ | 2+ | NA | nd | 0+ | 3+ | 2+ | + | + | 640 | |
| d28 | 2423 | nd | 0+ | 2+ | 0+ | 1+ | 1+ | 2+ | nd | 1+ | 1+ | 1+ | NA | 0+ | 0+ | 2+ | 2+ | + | + | <=1,280 |
| 2435 | 0+ | 0+ | 3+ | 0+ | 2+ | 1+ | 3+ | nd | nd | 0+ | 1+ | NA | 0+ | 0+ | 2+ | 2+ | + | + | <=1,280 | |
| 2436 | 0+ | 0+ | 3+ | 0+ | 1+ | 1+ | 3+ | nd | 1+ | 0+ | 1+ | NA | 0+ | 0+ | 2+ | 1+ | + | + | <=1,280 | |
| 2438 | nd | 0+ | 3+ | 0+ | 2+ | 1+ | 3+ | nd | 2+ | 1+ | 1+ | NA | nd | 0+ | 3+ | 2+ | + | + | 640 | |
| 2430 | 0+ | 0+ | 3+ | 0+ | 1+ | 1+ | 3+ | 0+ | 1+ | 1+ | nd | NA | 0+ | 0+ | 2+ | 2+ | + | + | >=1,280 | |
| 2431 | 0+ | 0+ | 2+ | nd | 1+ | 2+ | 2+ | NA | nd | 0+ | 0+ | 0+ | nd | NA | 1+ | 2+ | + | + | >=1,280 | |
| 2433 | 0+ | 0+ | 1+ | 0+ | 1+ | 0+ | 1+ | nd | 1+ | 0+ | 0+ | NA | 0+ | 0+ | 1+ | 0+ | + | + | >=1,280 | |
| d35 | 2336 | 0+ | 1+ | 4+ | 2+ | 3+ | 4+ | 4+ | NA | 2+ | 2+ | nd | 0+ | 1+ | NA | 2+ | 2+ | + | + | nd |
| 2332 | 0+ | 0+ | 2+ | nd | 1+ | 1+ | 2+ | nd | nd | 1+ | 1+ | NA | 0+ | 0+ | 2+ | 2+ | + | + | nd | |
| 2352 | 0+ | 0+ | 2+ | 0+ | 1+ | 0+ | 1+ | NA | 1+ | nd | 1+ | 0+ | 0+ | NA | 0+ | 1+ | − | + | nd | |
| 2353 | 0+ | 0+ | 3+ | 0+ | nd | 2+ | 4+ | NA | 2+ | 1+ | 0+ | 0+ | 2+ | NA | 3+ | 1+ | − | + | nd | |
| 2328 | 0+ | 0+ | 4+ | 0+ | 2+ | 3+ | 4+ | NA | 2+ | 1+ | 3+ | 0+ | 1+ | NA | 1+ | 1+ | + | + | nd | |
Antigen scoring: 0+ = no positive cells; 1+ = rare positive cells; 2+ = few positive cells; 3+ = moderate number positive cells; 4+ = many positive cells; nd = not done; NA = not applicable.
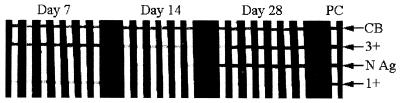
Figure 1.
Sera from all SNV-inoculated animals at days 7, 14, and 28 pi were examined for reactivity to the SNV N antigen by strip immunoblot assay (central band). In addition to the viral band, a Coomassie blue (CB) band was loaded for orientation, as well as high-intensity (3+) and low-intensity (1+) bands of deer mouse serum. Animals at 14 d were undergoing seroconversion, whereas the 28-d specimens were fully reactive.
Anti-N antibodies were evident by 14 d in three of six specimens, but seroconversion was complete in all of the remaining animals at later time points (Table 1; Fig. 1). Using nested RT-PCR, we could detect viral RNA in the blood of every animal at 21 d and 28 d, but at the other time points, only some animals were positive (Table 1). Nested RT-PCR studies were conducted on the remaining 14 tissues from all animals at 7 d and 14 d, and on three animals from each of the other time points. Of the seven animals examined at 7 d, two animals (2470 and 2473) were negative in every tissue; 2469, 2471, and 2475 were positive in heart, lung, kidney, liver, spleen, thymus, brown fat, and salivary gland, whereas 2474 and 2476 had a more limited distribution of positive tissues (heart, lung, kidney and liver, and heart, lung, salivary and brown fat, respectively). Animals 2469 and 2475 also had viral RNA in white fat, and 2475 was positive in the large intestine. By 14 d, most tissues of the six animals were positive for viral RNA, although three specimens lacked RNA in the pancreas, and one specimen each lacked RNA in the spleen, brain, bladder, or large intestine. By 21 d and onward, the three animals examined showed RNA in every tissue except pancreas, wherein it was undetectable in all specimens.
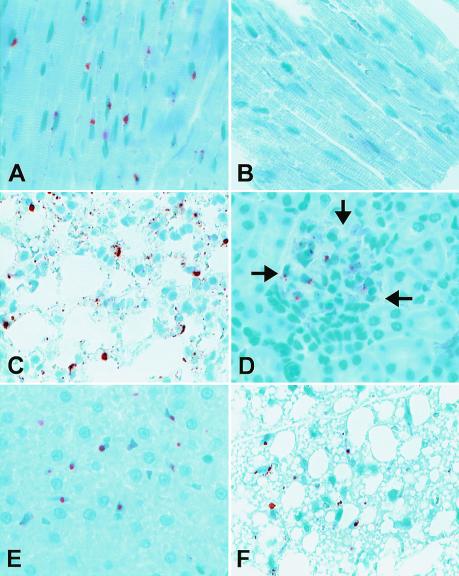
At 7 d, minimal expression of N antigen could be detected in the heart, lung, kidney, liver, and/or spleen of three animals. Antigen was not detected in any of the reproductive organs and infrequently in brain, bladder, and intestine. Heart, lung, brown fat, white fat, and liver demonstrated the most intense antigen staining throughout the experimental interval (Table 1; Fig. 2). The cells expressing N antigen had the morphological characteristics of endothelial cells throughout the tissues. In the liver, staining was confined to Kupfer cells and vascular endothelium (Fig. 2E).
Figure 2.
Localization of SNV N antigen in acutely infected deer mice by immunohistochemistry. Selected samples are shown at ×400. (A) Mouse no. 5139 heart, 21 d. (B) Heart of sham-injected mouse, 21 d. (C) Mouse no. 2450 lung, 21 d. (D) Mouse no. 5139 kidney. (E) Mouse no. 2468 liver, 14 d. (F) Mouse no. 2450, brown fat. Arrows indicate the borders of a glomerulus.
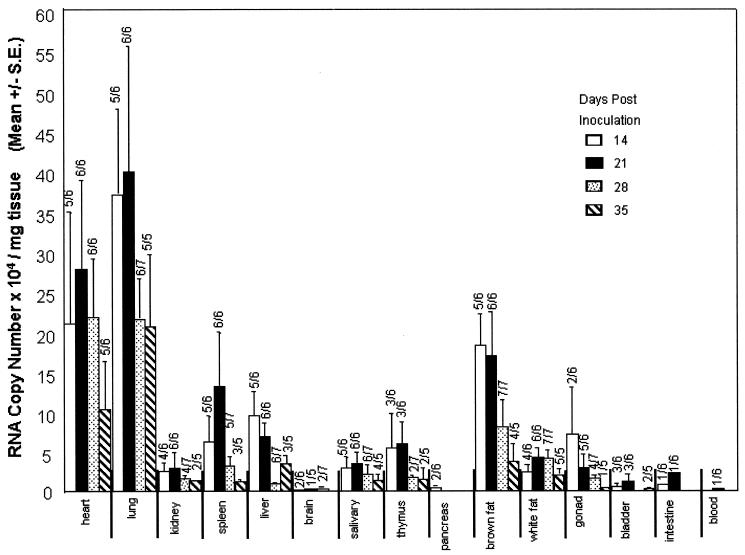
Quantitative RT-PCR.
Our quantitative RT-PCR system was less sensitive than nested RT-PCR, but still allowed us to quantitate viral RNA at levels of ≥1,000 copies/mg tissue (Fig. 3). We were only able to detect viral RNA in one sample (lung) at 7 d. Thus, we do not show the results from the 7-d samples in Fig. 3. For most tissues, RNA titers peaked at 21 d. The RNA load decreased by 28 d, coincident with the appearance of high titers of neutralizing antibodies (Table 1). Lung, heart, and brown fat consistently displayed the highest titers of viral RNA throughout the time course whereas blood, pancreas, brain, intestine, and bladder had the lowest titers. Most samples of the latter tissues had undetectable RNA levels. Neutralizing antibodies were present at low levels (1:20) in two of five 7-d sera and increased rapidly thereafter. Because the titers at 28 d were ≥1:1,280, we did not test sera at 35 d (Table 1).
Figure 3.
TaqMan quantitative RT-PCR analysis. The RNA copy number is expressed as the mean of all tissues with detectable signal at each time point. The number of tissues positive/tissues tested is expressed above each time point bar. Error bars indicate the SEM for three replicates. Threshold sensitivity was 1,000 copies/mg.
To determine whether infection caused any histopathologic changes, two pathologists blindly examined fixed tissue sections that were stained with hematoxylin and eosin (18). Many animals exhibited an array of very mild inflammatory changes in different tissues, including pleuritis or peribronchiolitis, and cholangiohepatitis. The same inflammatory changes also were seen in the controls, perhaps reflecting normal variation for species.
Persistent Infection.
The reservoir hosts for hantaviruses are thought to be persistently infected in nature (1). To examine whether this was true for experimentally infected deer mice, two animals (JB98 and JB105) were inoculated i.m. with 1,000 ID50 of the P1 stock and killed at 90 d to establish whether they had cleared the infection. Of 14 tissues examined at 90 d, JB105 exhibited viral RNA in heart, spleen, and brown fat, whereas in JB98, heart, lung, kidney, thymus, salivary gland, brain, brown fat, testes, bladder, and blood were positive, whereas spleen, liver, and pancreas were negative. By IHC, N antigen was detected in the brown fat (2+), heart (2+) lungs (1+), and salivary gland (1+) of JB98, but JB105 lacked any detectable antigen.
Discussion
We took several steps to help ensure that our experimental infections were similar to natural infections. Previous studies using the Puumala hantavirus have demonstrated that adaptation to cell culture resulted in a genetic change that reduced the infectivity of the isolate in its natural host (25). For that reason, we did not pass our virus in tissue culture. In addition, we obtained our virus from the same population of mice that was used to found our breeding colony, to minimize the effect of geographic (genetic) incompatibilities between virus and host (26). We compared ≈4 kb of sequence between the input virus and the virus at passage 3 and found no differences.
There is extensive dissemination of SN virus RNA throughout the tissues at 7 d, at a time when there is little viremia. We repeated the nested RT-PCR studies on all of the previously negative blood samples from the 7-d time point by loading five times as much blood RNA (data not shown). Only one new sample was positive for SN virus RNA (2475). However, it is possible that there was an earlier or very low-level viremia that we did not detect.
We were surprised to see that in addition to the lungs, both heart and brown fat demonstrated high titers of viral RNA and stained strongly for N antigen at each time point, suggesting that they may serve as sites for viral replication or maintenance. It is interesting that heart carries such high levels of viral RNA in light of the fact that although this tissue does not manifest histopathologic changes in humans with HCPS, expression of viral antigen can be intense and most deaths are caused by functional cardiac deficiencies (27, 28). Brown fat may be a tissue depot for Puumala hantavirus in wild, infected voles (29). A role for brown fat also has been suggested in the maintenance of rabies virus and murine cytomegalovirus (30, 31). It is possible that hantaviruses may overwinter in the brown fat and then exploit signals that are used by the host for thermoregulation to affect production of virions in the spring.
The exact mechanism(s) by which SNV is transmitted among deer mice in nature is not well understood. Field studies suggest that a horizontal mechanism is responsible, particularly among males (32). Biting or cross-grooming could facilitate transmission through saliva. We found substantial levels of viral RNA in salivary gland beginning on day 14. Although viral RNA is not synonymous with infectivity, it may indicate the potential for the production of infectious virus in a given tissue. We did not examine infectivity of tissues in this initial study, because it has been extremely difficult to isolate SNV in tissue culture compared with other hantaviruses such as Black Creek Canal virus (9, 15). Intermittent excretion/secretion of virus into saliva, feces, and urine has been detected for the more readily isolated Puumala and Hantaan viruses in their natural reservoirs (33, 34).
Transmission of SNV to humans is believed to occur through exposure to aerosolized virus from rodent urine, feces, or saliva. Although we did not look directly for fecal shedding, we found little evidence for viral expression in the large intestine. RNA titers were also low in the bladder, but viral antigens were consistently detected in the glomerular capillaries, suggesting a possible site for excretion.
Hantavirus infections have been considered to cause no ill effects in reservoir rodents, although some can elicit a neurologic disease in neonatal Mus musculus when inoculated intracranially (35). In the wild, hantavirus infection does not reduce the fertility or longevity of reservoir rodents (36). To our knowledge no investigators have reported any pathological effects from experimental infection. Recently, two groups have presented evidence suggesting that infection with SNV or New York hantaviruses in wild rodents may be associated with pulmonary edema and periportal hepatitis in wild-caught rodents (37, 38). Methodological problems such as absence of appropriate control rodents render these experiments difficult to interpret. The aerobic capacity of wild-caught seropositive deer mice is not impaired and may even be improved compared with seronegative controls, contrary to what would be expected in the presence of pulmonary edema (39). Using deliberate experimental inoculations, we have been unable to elicit consistent histopathological lesions as described in the previous studies, at least during the acute phase of infection. The pathologic effects, if any, of chronic infection will require separate evaluation.
Acknowledgments
We thank V. Bain, J. Dunnum, C. Fulhorst, D. Goade, M. Grady, F. Gurule, K. Hutchinson, K. Johnson, R. Lyons, R. Nofchissey, and T. Yates for helpful comments and technical assistance, and the University of New Mexico DNA Services and TriCore Corp. for technical support. C. Schmaljohn provided the CC107 strain of SNV. We also thank the United States Fish and Wildlife Service (Sevilleta National Wildlife Refuge) and the Museum of Southwestern Biology for their cooperation in this study. This work was supported by U.S. Public Health Service Grants RO1 AI 41692 and RO1 AI36336 and Defense Advanced Research Projects Agency Grant MDA972–97-1–0013. J.B. is an Infectious Diseases and Inflammation Training Grant Fellow (Public Health Service Grant T32 AI07538).
Abbreviations
- SNV
Sin Nombre virus
- HCPS
hantavirus cardiopulmonary syndrome
- IHC
immunohistochemistry
- RT
reverse transcription
- pi
postinoculation
- N
nucleocapsid
Footnotes
This paper was submitted directly (Track II) to the PNAS office.
Data deposition: The sequences reported in this paper have been deposited in the GenBank database (accession nos. AF281850–AF281857).
Article published online before print: Proc. Natl. Acad. Sci. USA, 10.1073/pnas.180197197.
Article and publication date are at www.pnas.org/cgi/doi/10.1073/pnas.180197197
References
- 1.Schmaljohn C, Hjelle B. Emerg Infect Dis. 1997;3:95–104. doi: 10.3201/eid0302.970202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nichol S T, Spiropoulou C F, Morzunov S, Rollin P E, Ksiazek T G, Feldmann H, Sanchez A, Childs J, Zaki S, Peters C J. Science. 1993;262:914–917. doi: 10.1126/science.8235615. [DOI] [PubMed] [Google Scholar]
- 3.Hjelle B, Jenison S, Torrez-Martinez N, Yamada T, Nolte K, Zumwalt R, MacInnes K, Myers G. J Virol. 1994;68:592–596. doi: 10.1128/jvi.68.2.592-596.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mertz G J, Hjelle B L, Bryan R T. Adv Intern Med. 1997;42:373–425. [PubMed] [Google Scholar]
- 5.Childs J E, Ksiazek T G, Spiropoulou C F, Krebs J W, Morzunov S, Maupin G O, Gage K L, Rollin P, Sarisky J, Enscore R, et al. J Infect Dis. 1994;169:1271–1280. doi: 10.1093/infdis/169.6.1271. [DOI] [PubMed] [Google Scholar]
- 6.Mori M, Rothman A L, Kurane I, Montoya J M, Nolte K B, Norman J E, Waite D C, Koster F T, Ennis F A. J Infect Dis. 1999;179:295–302. doi: 10.1086/314597. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Morbid Mortal Wkly Rep. 1994;48:1–7. [Google Scholar]
- 8.Mills J N, Yates T L, Childs J E, Parmenter R R, Ksiazek T G, Rollin P E, Peters C J. J Mammal. 1995;76:716–722. [Google Scholar]
- 9.Elliott L H, Ksiazek T G, Rollin P E, Spiropoulou C F, Morzunov S, Monroe M, Goldsmith C S, Humphrey C D, Zaki S R, Krebs J W, et al. Am J Trop Med Hyg. 1994;51:102–108. doi: 10.4269/ajtmh.1994.51.102. [DOI] [PubMed] [Google Scholar]
- 10.Schmaljohn A L, Li D, Negley D L, Bressler D S, Turell M J, Korch G W, Ascher M S, Schmaljohn C S. Virology. 1995;206:963–972. doi: 10.1006/viro.1995.1019. [DOI] [PubMed] [Google Scholar]
- 11.Rollin P E, Ksiazek T G, Elliott L H, Ravkov E V, Martin M L, Morzunov S, Livingstone W, Monroe M, Glass G, Ruo S, et al. J Med Virol. 1995;46:35–39. doi: 10.1002/jmv.1890460108. [DOI] [PubMed] [Google Scholar]
- 12.Ksiazek T G, Nichol S T, Mills J N, Groves M G, Wozniak A, McAdams S, Monroe M C, Johnson A M, Martin M L, Peters C J, et al. Am J Trop Med Hyg. 1997;57:445–448. doi: 10.4269/ajtmh.1997.57.445. [DOI] [PubMed] [Google Scholar]
- 13.Song J W, Baek L J, Gajdusek D C, Yanagihara R, Gavrilovskaya I, Luft B J, Mackow E R, Hjelle B. Lancet. 1994;344:1637. doi: 10.1016/s0140-6736(94)90430-8. [DOI] [PubMed] [Google Scholar]
- 14.Gavrilovskaya I N, Shepley M, Shaw R, Ginsberg M H, Mackow E R. Proc Natl Acad Sci USA. 1998;95:7074–7079. doi: 10.1073/pnas.95.12.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hutchinson K L, Rollin P E, Peters C J. Am J Trop Med Hyg. 1998;59:58–65. doi: 10.4269/ajtmh.1998.59.58. [DOI] [PubMed] [Google Scholar]
- 16.Botten J, Nofchissey R, Kirkendoll-Ahern H, Rodriguez-Moran P, Wortman I A, Goade D, Yates T, Hjelle B. J Mammal. 2000;81:250–259. [Google Scholar]
- 17.Hjelle B. In: Manual of Hemorrhagic Fever with Renal Syndrome and Hantavirus Pulmonary Syndrome. Lee H W, Calisher C, Schmaljohn C S, editors. Seoul: World Health Organization; 1999. pp. 131–137. [Google Scholar]
- 18.Green W, Feddersen R, Yousef O, Behr M, Smith K, Nestler J, Jenison S, Yamada T, Hjelle B. J Infect Dis. 1998;177:1696–1700. doi: 10.1086/515325. [DOI] [PubMed] [Google Scholar]
- 19.Hjelle B, Jenison S, Torrez-Martinez N, Herring B, Quan S, Polito A, Pichuantes S, Yamada T, Morris C, Elgh F, et al. J Clin Microbiol. 1997;35:600–608. doi: 10.1128/jcm.35.3.600-608.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hjelle B, Torrez-Martinez N, Bharadwaj M. In: Manual of Hemorrhagic Fever with Renal Syndrome and Hantavirus Pulmonary Syndrome. Lee H W, Calisher C, Schmaljohn C S, editors. Seoul: World Health Organization; 1999. pp. 122–130. [Google Scholar]
- 21.Yamada T, Hjelle B, Lanzi R, Morris C, Anderson B, Jenison S. J Virol. 1995;69:1939–1943. doi: 10.1128/jvi.69.3.1939-1943.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bharadwaj M, Botten J, Torrez-Martinez N, Hjelle B. Am J Trop Med Hyg. 1997;57:368–374. doi: 10.4269/ajtmh.1997.57.368. [DOI] [PubMed] [Google Scholar]
- 23.Hjelle B, Torrez-Martinez N, Koster F T, Jay M, Ascher M S, Brown T, Reynolds P, Ettestad P, Voorhees R E, Sarisky J, et al. J Infect Dis. 1996;173:781–786. doi: 10.1093/infdis/173.4.781. [DOI] [PubMed] [Google Scholar]
- 24.Bharadwaj M, Lyons C R, Wortman I A, Hjelle B. Vaccine. 1999;17:2836–2843. doi: 10.1016/s0264-410x(99)00096-1. [DOI] [PubMed] [Google Scholar]
- 25.Lundkvist Å, Cheng Y, Sjolander K B, Niklasson B, Vaheri A, Plyusnin A. J Virol. 1997;71:9515–9523. doi: 10.1128/jvi.71.12.9515-9523.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hjelle B, Yates T. In: Current Topics in Microbiology and Immunology (Hantaviruses) Schmaljohn C, Nichol S, editors. Berlin: Springer; 2000. , in press. [Google Scholar]
- 27.Hallin G W, Simpson S Q, Crowell R E, James D S, Koster F T, Mertz G J, Levy H. Crit Care Med. 1996;24:252–258. doi: 10.1097/00003246-199602000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Zaki S R, Greer P W, Coffield L M, Goldsmith C S, Nolte K B, Foucar K, Feddersen R M, Zumwalt R E, Miller G L, Khan A S, et al. Am J Pathol. 1995;146:552–579. [PMC free article] [PubMed] [Google Scholar]
- 29.Gavrilovskaya I N, Apekina N S, Myasnikov Y A, Bernshtein A D, Ryltseva E V, Gorbachkova E A, Chumakov M P. Arch Virol. 1983;75:313–316. doi: 10.1007/BF01314898. [DOI] [PubMed] [Google Scholar]
- 30.Botvinkin A D, Nikiforova T A, Sidorov G N. Acta Virol. 1985;29:44–50. [PubMed] [Google Scholar]
- 31.Lussier G. Can J Comp Med Vet Sci. 1974;38:179–184. [PMC free article] [PubMed] [Google Scholar]
- 32.Mills J N, Ksiazek T G, Ellis B A, Rollin P E, Nichol S T, Yates T L, Gannon W L, Levy C E, Engelthaler D M, Davis T, et al. Am J Trop Med Hyg. 1997;56:273–284. doi: 10.4269/ajtmh.1997.56.273. [DOI] [PubMed] [Google Scholar]
- 33.Yanagihara R, Amyx H, Gajdusek D. J Virol. 1985;55:34–38. doi: 10.1128/jvi.55.1.34-38.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee H W, Lee P W, Baek L J, Song C K, Seong I W. Am J Trop Med Hyg. 1981;30:1106–1112. doi: 10.4269/ajtmh.1981.30.1106. [DOI] [PubMed] [Google Scholar]
- 35.Tsai T F, Baner S, McCormick J B, Kurata T. Lancet. 1982;2:503–504. doi: 10.1016/s0140-6736(82)90537-2. [DOI] [PubMed] [Google Scholar]
- 36.Childs J E, Glass G E, Korch G W, LeDuc J W. J Wildlife Dis. 1989;25:469–476. doi: 10.7589/0090-3558-25.4.469. [DOI] [PubMed] [Google Scholar]
- 37.Lyubsky S, Gavrilovskaya I, Luft B, Mackow E. Lab Invest. 1996;74:627–633. [PubMed] [Google Scholar]
- 38.Netski D, Thran B H, St. Jeor S C. J Virol. 1999;73:585–591. doi: 10.1128/jvi.73.1.585-591.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O'Connor C S, Hayes J P, St. Jeor S C. J Mammal. 1997;78:661–668. [Google Scholar]