Abstract
Nucleoside reverse transcriptase inhibitors (NRTIs) are effective antiretroviral therapy for the treatment of HIV-infected patients. NRTIs can induce mitochondrial impairment that leads to a number of adverse events, including symptomatic lactic acidosis. In the present review, we describe the underlying mechanism of NRTI-induced toxicity and the main clinical features of this infrequent, but severe, emerging complication. We also summarise experimental data and clinical observations that support the use of L-carnitine supplementation to reverse NRTI-induced mitochondrial impairment.
Keywords: antiretroviral drug, critically ill patients, HIV, lactic acidosis, mitochondria
Introduction
Nucleoside analogue reverse transcriptase inhibitors (NRTIs) are effective antiretroviral therapies for the treatment of HIV-infected patients. Treatment with NRTIs has been associated with mitochondrial toxicity [1] responsible for adverse events including hepatic steatosis [2], myopathy [3], neuropathy [4], myelotoxicity [5] and overproduction of lactate [1].
Symptomatic lactic acidosis following the use of NRTIs was first described by Jolliet and Widmann [6] and by Chatta and colleagues [7] in HIV-infected patients treated with azidothymidine. Several reports since then have established that other NRTIs can induce lactic acidosis [8-30]. This severe adverse event is infrequent but its occurrence may be underestimated [31]. Progression of lactic acidosis can lead to irreversible multiple organ failure despite drug withdrawal [8].
In the present review, based on Medline research and using personal data, we describe the pathophysiology and the clinical spectrum of lactic acidosis in an attempt to define a population with a poor prognosis. Based on clinical data and experimental evidence, we discuss the use of L-carnitine as a specific treatment for life-threatening NRTI-induced lactic acidosis.
Mitochondrial functions and NRTI toxicity Mitochondrial respiratory chain
The main function of mitochondria is to produce energy through electron-chain transport and oxidative phosphorylation (summarised in Fig. 1). The core of the pathway is a complex of five subunits (subunits I–V) located on the inner mitochondrial membrane. Electrons pass the chain from various substrates, providing energy to the proton pump that creates an electrochemical gradient between mitochondria and their environment. Different substrates can enter the electron-chain transport at complex I (the reduced form of nicotinamide adenine dinucleotide [NADH]–coenzyme Q oxidoreductase) or complex II (succinate–coenzyme Q oxidoreductase), which provide electrons to complex III (coenzyme QH2–cytochrome oxidoreductase). Complex III then reduces cytochrome c, which passes electrons to complex IV (cytochrome c oxidase). Complex V (ATP synthase) produces ATP.
Figure 1.
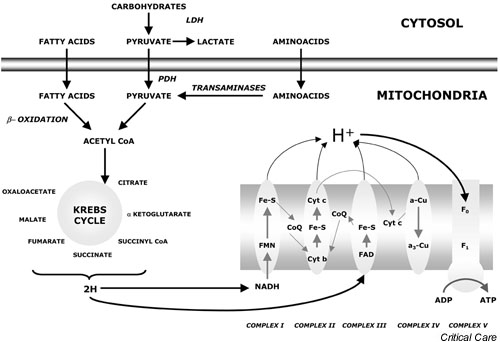
Mitochondrial electron chain transport and oxydative phosphorylation. Most of the energy produced by metabolic pathways is contained in the reduced form of nicotinamide adenine dinucleotide (NADH) and in the reduced form of flavine adenine dinucleotide (FADH2), and is transformed in ATP by mitochondria. Reduced mitochondrial coenzymes give their two electrons to carriers that carry them to molecular oxygen, the final electron acceptor, using oxydo-reduction reactions. A protonic gradient allows hydrogen to cross the inner membrane and produce ATP. a-Cu, coenzyme a-copper; a3-Cu, coenzyme 13-copper; CoA, coenzyme A; CoQ, coenzyme Q; Cyt, cytochrome; F0, F0 family ATP synthase; F1, F1 family ATP synthase; Fe-S, iron-suphur cluster; FMN, flavine-adenine mononucleotide; H, hydrogen; LDH, lactate dehydrogenase; PDH, pyruvate dehydrogenase.
To feed this chain, degradative metabolic pathways transform substrates into energetic compounds. The oxidative decarboxylation of pyruvate leads to the production of acetylcoenzyme A. Fatty acids enter the mitochondrial metabolism after β-oxidation, which allows the production of two acetylcoenzyme A molecules and one acyl-coenzyme A molecule shorter than the initial substrate. Acetylcoenzyme A then enters the citric acid cycle or Krebs cycle to release carbon dioxide, hydrogen, NADH, the reduced form of flavine adenine dinucleotide (FADH2), GTP and coenzyme A.
Mechanisms of NRTI-induced lactate elevation
The toxicity of NRTI is related to alterations of the mitochondrial breathing pathway at different levels. The mechanisms of toxicity related to the use of NRTI are summarised in Table 1.
Table 1.
Cellular effects of nucleosidic reverse transcriptase inhibitors (NRTIs) and carnitine
| Toxicity of NRTIs | References | Effect of carnitine | References | |
| Metabolism | Impairment of β-oxidation cycle | [1] | Long-chain fatty acids carrier | [55] |
| Accumulation of long-chain fatty acids into the cytosol | [34] | Protection of cytochrome c oxidase from octanoic acid-induced damage | [61] | |
| Decrease in ATP concentration | [32] | Cofactor of the electron chain from complex I-V | [60] | |
| Decreased electron-chain transport | [32] | |||
| γDNA polymerase damage | [33] | |||
| NAD+/NADH impairment | ||||
| Apoptosis | Increased apoptosis | [36-38] | Decreased global apoptosis | [44-46] |
| Overexpression of the receptor Fas | [38] | Decreased ceramide generation | [46,49-52] | |
| Decreased mitochondrial apoptosis | [49] | |||
| Link with Bcl2? | [50] |
NAD+, nicotinamide adenine dinucleotide; NADH, reduced form of nicotinamide adenine dinucleotide
Longstanding use of NRTI induces damage of βDNA and γDNA polymerases. The dysfunction of γDNA polymerase leads to mitochondrial accumulation of abnormal nucleoside acids that alter termination and internalisation of mitochondrial DNA [32]. A recent article confirms that mitochondrial DNA levels are significantly decreased in patients with symptomatic, nucleoside-related hyperlactataemia, and confirms that reduction of mitochondrial DNA precedes symptomatic hyperlactataemia and resolves on the discontinuation of therapy [33]. Nevertheless, another report states that, despite the mitochondrial DNA depletion, the oxidative capacity of the mitochondrial respiratory chain is preserved in lymphocytes derived from treated asymptomatic HIV-infected patients. This does not exclude the possibility of decreased mitochondrial respiratory-chain function in other tissues [34].
As mitochondrial DNA encodes 13 out of 80 enzymes of the breathing pathway, this dysregulation leads to the decrease in ATP synthesis and metabolism. In addition, NRTIs also decrease electron transfer by impairing the NAD+/NADH cycle [35].
NRTIs thus impair the β-oxidation cycle and disrupt oxidative phosphorylation [1]. These pathways physiologically allow fatty acids and pyruvate to enter as energetic substrates in the mitochondrion. When NRTI toxicity occurs, long-chain fatty acids (characterised by a carbon scaffold above 12 residues) do not contribute to ATP production and accumulate into the cytosol of myocytes and hepatocytes. An increase in glycolysis then leads to the overproduction of lactic acid, which imbalances the lactate:pyruvate ratio [36]. The hepatic failure sometimes observed in this context compromises clearance of lactate and contributes to the development of what is then classified as type II lactic acidosis (i.e. related to the deregulation of cell metabolism and not directly linked to tissue hypoxaemia).
Apoptosis, the programmed cell death phenomenon driven by specific signalling pathways (reviewed in [37]) in response to stress conditions, also contributes to NRTI toxicity. This physiologic event is tightly regulated by the balance between proapoptotic and antiapoptotic signals. The imbalance in favour of proapoptotic signals can lead to activation of caspases, the cysteine proteases that cleave target proteins to determine apoptosis. Several studies suggest that NRTIs play a proapoptotic role. In B-lymphoid cell types [38,39] and peripheral blood mononuclear cells [40], azidothymidine can trigger apoptosis and inhibition of the cell cycle [39] associated with overexpression of the death domain receptor Fas [40], although it is established that mitochondrial apoptosis can be responsible for an increased lactate production [41].
Clinical features of NRTI-induced lactic acidosis in HIV-infected adults
Although the incidence of symptomatic lactic acidosis in adult HIV-infected patients treated with NRTIs may have been previously underestimated, recent data suggest that the occurrence of NRTI-induced lactic acidosis is increasing [31]. The estimated incidence varies between 1.3/1000 in 1995 [9] and 14.8/1000 recently [28], but this discrepancy may be related to differences in case definition [31]. Descriptions of clinical features and laboratory findings are sparse and the literature does not precisely define the clinical spectrum of this disorder.
To identify the clinical features of NRTI-induced lactic acidosis in HIV-infected adults, we recently reviewed charts from published observations and personal cases [42]. Twenty patients were survivors and 19 patients did not survive the disorder. The occurrence of symptomatic lactic acidosis or hepatic failure attributed to the use of NRTIs in adult HIV-infected patients defines severe mitochondrial cytopathy. Although this disorder often occurs in overweight females, no risk factor has been clearly identified. Most patients are diagnosed with AIDS at the time of the occurrence of the adverse event. Cases have been attributed to the use of all NRTIs currently used in human therapy, although they seem to occur more frequently when stavudine and lamivudine are combined. The average delay between the introduction of NRTI and the diagnosis of mitochondrial cytopathy is 8 months. The time from admission to death was 5 days (range 1–17 days) in the nonsurvivor population.
Clinical manifestations are often nonspecific (summarized in Table 2. Asthaenia is encountered in 70% of cases. Anorexia (40%) and weight loss (20%) are also commonly reported. The body temperature is normal in 50% of the cases, but it can range between 35.3 and 39°C for the remaining patients. Abdominal signs are reported in most patients: nausea and vomiting are frequent (87.5%), as is abdominal pain (82%), often localised in the right upper quadrant. Examination finds hepatomegaly (75%), confirmed by ultrasound tomography findings consistent with hepatic steatosis. Muscular weakness is reported in 20% of the cases. Tachypnoea is very common (83% of the cases) and mostly related to severe acidosis.
Table 2.
Common findings in 39 cases of nucleosidic reverse transcriptase inhibitor-induced lactic acidosis
| Clinical feature | Percent of cases |
| Asthaenia | 70 |
| Muscular weakness | 20 |
| Anorexia | 40 |
| Loss of weight | 20 |
| Fever or hypothermia | 50 |
| Nausea and vomiting | 87.5 |
| Abdominal pain | 82 |
| Hepatomegaly | 75 |
| Tachypnea | 83 |
| Laboratory findings | |
| Hyperlactataemia and metabolic acidosis | 100 |
| Hepatic cytolysis | 79 |
| Hepatic cholestasis | 73 |
| Low prothrombin rate | 45 |
| Elevated lacticodehydrogenase | 100 |
| Macrovacuolar or microvacuolar steatosis | 100 |
Lactic acidosis is indeed a constant biological feature of mitochondrial cytopathy. The first recorded arterial blood lactate concentration ranges between 2.9 and 43 mmol/l, and life-threatening acidosis occurs in 42% of the cases. Enzyme liver assays show marked cytolysis (79%) and anicteric cholestasis (73%). The prothrombin time is significantly decreased in 45% of the patients. Other common laboratory test abnormalities include elevated pancreatic enzymes (33%) and increased creatine phosphokinase or lacticodehydrogenase concentrations. The liver is constantly involved, and pathology examination usually reveals steatosis (n = 11) that can be classified as macrovacuolar, microvacuolar or mixed. Electronic microscopy of the liver, when available [8,12], shows ballonised mitochondria with loss of cristae. Inflammation and necrosis of the pancreas gland are also described. Lung pathology mostly indicates nonspecific inflammatory oedema. Light microscopy never shows any involvement of skeletal muscles in this setting.
The outcome of NRTI-induced lactic acidosis is often unfavourable. Uncontrolled shock and/or hepatic failure usually leads to death within 8 days following hospital admission. Supportive care including haemodialysis, alkalinisation, vasoactive drugs and mechanical ventilation is inefficient. In some cases, patients have been treated with prostaglandin [13] and with thiamine [15] without any improvement.
In an attempt to identify prognostic factors, we compared available data and the clinical course from hospital charts of survivors and of nonsurvivors [43]. Clinical features did not differ between the two populations. Conversely, arterial blood pH and bicarbonates almost reached statistical significance, probably because of the limited number of available observations. In fact, the first registered blood lactate was significantly different between survivors and nonsurvivors. The mean values of the initial blood lactate level in survivors and in nonsurvivors were 7.3 ± 3.8 and 18.6 ± 8.8 mmol/l, respectively (P < 0.01). We used the LOWESS smoothing function and the locally weighted least-squares method to identify a blood lactates threshold that is likely to predict poor outcome. A value of 9 mmol/l was associated with a positive predictive value of 82%, with a negative predictive value of 94.5%, and with high sensitivity and specificity.
The initial blood lactate level can thus predict the course in symptomatic lactic acidosis related to the use of NRTIs. Blood lactate below 9 mmol/l at diagnosis is associated with a less severe disorder, whereas a value above this threshold is predictive of a fatal outcome.
L-carnitine as a possible treatment for NRTI-induced severe lactic acidosis in HIV-infected patients
Rationale for the use of L-carnitine in NRTI-induced lactic acidosis
Carnitine is derived from γ-hydroxy-β-butyric acid. Although a regular diet is the primary supply of carnitine, endogenous synthesis is possible from sulphated amino acids (reviewed in [44]). Carnitine levels are decreased in HIV-infected patients through several mechanisms, including malabsorption, increased excretion, overconsumption of energy in fatty acids metabolism and the use of drugs, including NRTIs [44,45].
Carnitine is a pivotal cofactor for mitochondrial aerobic metabolism [46]. It carries long-chain fatty acids through the inner mitochondrial membrane to allow their use in the β-oxidation circle. It also interacts downstream at different steps as a cofactor between complex I–complex V of the electron chain [47]. Carnitine directly stimulates phase IV of the mitochondrial breathing cycle, and prevents the detrimental effect of octanoic acid on the cytochrome c oxidase [48].
An emerging concept suggests that carnitine could also modulate apoptosis. Carnitine decreases the number of apoptotic cells and lowers caspase 3-like activity in Jurkat T cells after stimulation of the death domain receptor Fas [49], in the serum-starved P19 teratoma cell line [50] and in cardiomyocytes exposed to doxorubicin [51]. In the latter model, L-carnitine seems to lower the doxorubicin-induced sphyngomyelinase activity and decreases the concentration of ceramides, messengers involved in programmed cell death. Fibroblasts deficient for carnitine palmitoyl transferase 1, the enzyme that converts carnitine into palmitoylcarnitine, are resistant to apoptosis induced by staurosporine [52], a drug that triggers the mitochondrial apoptotic pathway by opening mitochondria transition pores. In addition, a clear association between carnitine palmitoyl transferase 1 and the antiapoptotic mitochondrial protein Bcl2 has been found using several techniques including a yeast two-hybrid system [53]. These data suggest that L-carnitine modulates apoptosis at the mitochondrial level.
L-carnitine reverses the mitochondrial toxicity of NRTIs in vitro. Incubation of cell lineages with NRTIs reproduces features encountered in human NRTI-related cytopathy (i.e. modification of the ultrastructure of the mitochondria and accumulation of lipid droplets in the cytoplasm) [54]. In human myotube cultures, the addition of carnitine in the medium improves these changes whether or not azidothymidine is withdrawn [55]. A clinical study confirmed the antiapoptotic activity of carnitine in CD4-positive lymphocytes from peripheral blood of HIV-infected patients [56]. Samples analysed after treatment by daily infusions of L-carnitine show a decreased number of apoptotic cells that correlates with a drop in ceramide concentration.
Hypertriglyceridaemia is a disorder commonly related to the use of NRTIs [57]. The underlying mechanism involves mitochondrial impairment and would preferentially target hepatocytes. In a preliminary study, L-carnitine dramatically reversed antiretroviral therapy-related hypertriglyceridaemia in HIV-infected adults [58]. Reversal of lactic acidosis related to NRTIs after treatment including L-carnitine has also been reported in patients with blood lactate above 10 mmol/l at the beginning of the treatment [43,59].
L-carnitine as a potential treatment for life-threatening NRTI-induced lactic acidosis
Carnitine is an important compound for the mitochondria bioenergetic system that may modulate apoptosis. It has also been observed that carnitine could reverse the mitochondrial toxicity of NRTIs in vitro and in vivo [44,55,58,59].
In an attempt to define whether L-carnitine could be an effective treatment for patients with life-threatening NRTI-related lactic acidosis, we prospectively investigated the effects of L-carnitine in six critically ill, HIV-infected patients [43]. These patients had arterial blood lactate above 10 mmol/l and severe organ dysfunction, possibly requiring dialysis. L-carnitine was used as a specific treatment, with a dosing regimen of 50 or 100 mg/kg per day if continuous dialysis was required. Six patients received the treatment according to the protocol. With a mean Simplified Acute Physiology Score II score of 81, with blood lactate levels ranging from 13 to 20.1 mmol/l and with pH values between 7.3 and 6.7, these patients had a predicted intrahospital death probability of 91% [60]. When available, carnitine dosages revealed a decrease in the free cartinine:total serum carnitine ratio and an increase in urine excretion, features commonly encountered in this setting. Three patients out of six survived. Their arterial blood lactate level returned to baseline within 15 days and no increase in blood lactate was noted during the followup. These preliminary results suggest that L-carnitine may be useful for the treatment of life-threatening lactic acidosis related to the use of NRTIs.
Conclusion
Following the widespread use of NRTIs for the treatment of HIV-infected patients, increasing evidence has demonstrated that these drugs can induce mitochondrial dysfunction and lactic acidosis. Experimental data show that NRTIs alter mitochondrial breathing at different steps [1]. Increased lactacidaemia induced by NRTIs is explained by a shift toward anaerobic metabolism with inverted lactate:pyruvate ratio [36], by increased apoptosis leading to lactate overproduction, and by decreased lactate clearance secondary to hepatic dysfunction [28]. The pathophysiology of NRTI-induced acidosis might be even more complex, and genetic risk factors could also play a role.
Despite increased physician awareness of NRTI-related lactate overproduction, clinical features are so aspecific that lactic acidosis can rapidly progress to life-threatening conditions before NRTIs are withdrawn. In NRTI-related lactic acidosis, the blood lactate concentration, a potential marker of mitochondrial impairment, seems to have a highly significant prognostic value. Whereas some workers consider mitochondrial cytopathy severe if blood lactate levels are above 5 mmol/l [26], we have found that arterial blood lactate at the time of diagnosis can predict outcome and that patients with lactate levels above 9 mmol/l are likely to develop life-threatening NRTI-induced lactic acidosis and die [43].
Very few HIV-infected patients with severe lactic acidosis have survived with the use of specific therapies [22,25]. Considering the rationale for the use of L-carnitine to treat NRTI-induced severe lactic acidosis and related organ failures, we conducted a small open trial of L-carnitine in critically ill patients and reported survival of three out of six patients with initial lactate levels above 9 mmol/l [43]. Several drugs have been proposed for the treatment of symptomatic lactic acidosis related to NRTIs because of their antiapoptotic and metabolic effects. Nevertheless, these promising data are very preliminary. Added to other studies, this preliminary result suggests that L-carnitine is a potential treatment for NRTI-induced mitochondrial dysfunction with severe lactic acidosis, although additional data should be provided to determine its efficiency.
Competing interests
None declared.
Abbreviations
NADH = reduced form of nicotinamide adenine dinucleotide; NRTI = nucleosidic reverse transcriptase inhibitor.
References
- Lewis W, Dalakas MC. Mitochondrial toxicity of antiviral drugs. Nat Med. 1995;1:417–422. doi: 10.1038/nm0595-417. [DOI] [PubMed] [Google Scholar]
- Stein DS. A new syndrome of hepatomegaly with severe steatosis in HIV-seropositive patients. AIDS Clin Care. 1994;6:17–21. doi: 10.1097/00002030-199303000-00012. [DOI] [PubMed] [Google Scholar]
- Dalakas MC, Illa I, Pezeshkpour GH, Laukaitis JP, Cohn B, Griffin JL. Mitochondrial myopathy caused by long-term zidovudine therapy. N Engl J Med. 1990;322:1098–1105. doi: 10.1056/NEJM199004193221602. [DOI] [PubMed] [Google Scholar]
- Fauld G. Didanoside – a review of its antiviral activity, pharmacokinetics and therapeutic potential in human immunodeficiency infection. Drugs. 1992;44:94–116. doi: 10.2165/00003495-199244010-00008. [DOI] [PubMed] [Google Scholar]
- Gribaldo L, Malerba I, Collotta A, Casati S, Pessina A. Inhibition of CFU-E/BFU-E by 3'-azido-3'-deoxythymidine, chlorpropamide, and protoporphyrin IX zinc (II): a comparision between direct exposure of progenitor cells and long term exposure of bone marrow cultures. Toxicol Sci. 2000;58:96–101. doi: 10.1093/toxsci/58.1.96. [DOI] [PubMed] [Google Scholar]
- Jolliet P, Widmann JJ. Reye's syndrome in adult with AIDS [letter]. Lancet. 1989;335:1457. doi: 10.1016/0140-6736(90)91481-o. [DOI] [PubMed] [Google Scholar]
- Chattha G, Arieff AI, Cummings C, Tierney LM., Jr Lactic acidosis complicating the acquired immunodeficiency syndrome. Ann Intern Med. 1993;118:37–39. doi: 10.7326/0003-4819-118-1-199301010-00007. [DOI] [PubMed] [Google Scholar]
- Sundar K, Suarez M, Banogon PE, Shapiro JM. Zidovudine-induced fatal lactic acidosis and hepatic failure in patients with acquired immunodeficiency syndrome: report of two patients and review of literature. Crit Care Med. 1997;25:1425–1430. doi: 10.1097/00003246-199708000-00034. [DOI] [PubMed] [Google Scholar]
- Fortgang IS, Belitsos PC, Chaisson RE, Moore RD. Hepatomegaly and steatosis in HIV-infected patients receiving nucleoside analog antiretroviral therapy. Am J Gastroenterol. 1995;90:1433–1436. [PubMed] [Google Scholar]
- Aggarwal A, al-Talib K, Alabrash M. Type B lactic acidosis in an AIDS patient treated with zidovudine. Mol Med J. 1996;45:929–931. [PubMed] [Google Scholar]
- Maslo C, Jacomet C, Jupas JJ, Lebrette MG, Rozenbaum W. Acidose lactique chez des patients infectés par le VIH [letter]. Press Med. 1994;23:717. [PubMed] [Google Scholar]
- Olano JP, Borucki MJ, Wen JW. Massive hepatic steatosis and lactic acidosis in a patient with AIDS who was receiving zidovudine. Clin Infect Dis. 1995;21:973–976. doi: 10.1093/clinids/21.4.973. [DOI] [PubMed] [Google Scholar]
- Lai KK, Gang DL, Zawaki JK, Cooley TP. Fulminant hepatic failure complicating the acquired immunodeficiency syndrome. Ann Intern Med. 1991;115:283–284. doi: 10.7326/0003-4819-115-4-283. [DOI] [PubMed] [Google Scholar]
- Acosta BS, Grimsley EW. Zidovudine-associated type B lactic acidosis and hepatic steatosis in an HIV-infected patient. South Med J. 1999;92:421–423. doi: 10.1097/00007611-199904000-00015. [DOI] [PubMed] [Google Scholar]
- Bissuel F, Bruneel F, Habersetzer F, Chassard D, Cotte L, Chevallier M, Bernuau J, Lucet JC, Trepo C. Fulminant hepatitis with severe lactate acidosis in HIV-infected patients on didanoside therapy. J Intern Med. 1994;235:367–372. doi: 10.1111/j.1365-2796.1994.tb01088.x. [DOI] [PubMed] [Google Scholar]
- Megarbane B, Fromont C, Nion I, Chary I, Axler O, Slama A, Brivet M, Rustin P, Munnich A, Brivet F. Un patient infecté par le VIH très très essouflé. Rev Med Interne. 1999;20(suppl 2):256–259. doi: 10.1016/s0248-8663(99)80456-1. [DOI] [PubMed] [Google Scholar]
- Allaouiche B, Duflo F, Cotte L, Mathon L, Chassard D. Acute pancreatitis with severe lactic acidosis in an HIV-infected patient on didanoside therapy. J Antimicrob Chemother. 1999;44:137–138. doi: 10.1093/jac/44.1.137. [DOI] [PubMed] [Google Scholar]
- Verma A, Schein RM, Jayaweera DT, Kett DH. Fulminant neuropathy and lactic acidosis associated with nucleoside analog therapy. Neurology. 1999;53:1365–1367. doi: 10.1212/wnl.53.6.1365. [DOI] [PubMed] [Google Scholar]
- Charton-Bain MC, Flamant M, Aubertin JM, Belair MF, Gilquin J, Kazatchkine M, Bruneval P. Lactic acidosis and hepatic mitochondrial changes during a treatment with zidovudine [in French]. Gastroenterol Clin Biol. 1997;21:979–981. [PubMed] [Google Scholar]
- Chariot P, Drogou I, de Lacroix-Szmania I, Eliezer-Vanerot MC, Chazaud B, Lombes A, Schaeffer A, Zafrani ES. Zidovudine-induced mitochondrial disorder with massive liver steatosis, myopathy, lactic acidosis, and mitochondrial DNA depletion. J Hepatol. 1999;30:156–160. doi: 10.1016/s0168-8278(99)80020-8. [DOI] [PubMed] [Google Scholar]
- Fouty B, Frerman F, Reves R. Riboflavin to treat nucleoside analogues-induced lactic acidosis. Lancet. 1998;352:291–292. doi: 10.1016/S0140-6736(05)60266-8. [DOI] [PubMed] [Google Scholar]
- Luzzati R, Del Bravo P, Di Perri G, Luzzani A, Concia E. Riboflavine and severe acidosis. Lancet. 1999;353:901–902. doi: 10.1016/S0140-6736(99)00523-1. [DOI] [PubMed] [Google Scholar]
- Lenzo NP, Garas BA, French MA. Hepatic steatosis and lactic acidosis associated with stavudine treatment in a HIV patient: a case report. AIDS. 1997;11:1294–1296. doi: 10.1097/00002030-199710001-00003. [DOI] [PubMed] [Google Scholar]
- Schramm C. Thiamine for the treatment of nucleoside analogue-induced severe lactic acidosis. Eur J Anaesthesiol. 1999;16:733–735. doi: 10.1046/j.1365-2346.1999.00586.x. [DOI] [PubMed] [Google Scholar]
- Roy PM, Gouello JP, Pennison-Besnier I, Chennebault JM. Severe lactic acidosis induced by nucleoside analogues in an HIV-infected man. Ann Emerg Med. 1999;34:282–284. doi: 10.1016/s0196-0644(99)70244-1. [DOI] [PubMed] [Google Scholar]
- ter Hofstede HJ, de Marie S, Foudraine NA, Danner SA, Brinkman K. Clinical features and risk factors of lactic acidosis following long-term antiretroviral therapy: 4 fatal cases. Int J STD AIDS. 2000;11:611–666. doi: 10.1258/0956462001916498. [DOI] [PubMed] [Google Scholar]
- Mokrzycki MH, Harris C, May H, Laut J, Palmisano J. Lactic acidosis associated with stavudine administration: a report of five cases. Clin Infect Dis. 2000;30:198–200. doi: 10.1086/313594. [DOI] [PubMed] [Google Scholar]
- Lonergan JT, Behling C, Pfander H, Hassanein TI, Mathews WC. Hyperlactatemia and hepatic abnormalities in 10 human immunodeficiency virus-infected patients receiving nucleoside analogue combination regimens. Clin Infect Dis. 2000;31:162–166. doi: 10.1086/313912. [DOI] [PubMed] [Google Scholar]
- Chodock R, Mylonakis E, Shemin D, Runarsdottir V, Yodice P, Renzi R, Tashima K, Towe C, Rich JD. Survival of a human immunodeficiency patient with nucleoside-induced lactic acidosis – role of haemodialysis. Nephrol Dial Transplant. 1999;14:2484–2486. doi: 10.1093/ndt/14.10.2484. [DOI] [PubMed] [Google Scholar]
- John M, Moore CB, James IR, Nolan D, Upton RP, McKinnon EJ, Mallal SA. Chronic hyperlactatemia in HIV-infected patients taking antiretroviral therapy. AIDS. 2001;15:717–723. doi: 10.1097/00002030-200104130-00007. [DOI] [PubMed] [Google Scholar]
- Brinkman K. Editorial response: hyperlactatemia and hepatic steatosis as features of mitochondrial toxicity of nucleoside analogue reverse transcriptase inhibitors. Clin Infect Dis. 2000;31:167–169. doi: 10.1086/313921. [DOI] [PubMed] [Google Scholar]
- Parker WB, Cheng YC. Mitochondrial toxicity of antiviral nucleoside analogs. J NIH Res. 1994;6:57–61. [Google Scholar]
- Cote HC, Brumme ZL, Craib KJ, Alexander CS, Wynhoven B, Ting L, Wong H, Harris M, Harrigan PR, O'Shaughnessy MV, Montaner JS. Changes in mitochondrial DNA as a marker of nucleoside toxicity in HIV-infected patients. N Engl J Med. 2002;346:811–820. doi: 10.1056/NEJMoa012035. [DOI] [PubMed] [Google Scholar]
- Casademont J, Miró O, Cardellach F. Mitochondrial DNA and nucleoside toxicity. N Engl J Med. 2002;347:216–218. [PubMed] [Google Scholar]
- Modica-Napolitano JS. AZT causes tissue specific inhibition of mitochondrial bioenergetic function. Biochem Biophys Res Commun. 1993;194:170–177. doi: 10.1006/bbrc.1993.1800. [DOI] [PubMed] [Google Scholar]
- Chariot P, Monnet I, Mouchet M, Rohr M, Lefaucheur JP, Dubreuil-Lemaire ML, Chousterman M, Gherardi R. Determination of the blood lactate:pyruvate ratio as a non invasive test for the diagnosis of zidovudine myopathy. Arthritis Rheum. 1994;37:583–586. doi: 10.1002/art.1780370421. [DOI] [PubMed] [Google Scholar]
- Green DR. Apoptotic pathways: the roads to ruin. Cell. 2001;94:695–698. doi: 10.1016/s0092-8674(00)81728-6. [DOI] [PubMed] [Google Scholar]
- Sailaja G, Nayak R, Antony A. Azydothymidine induces apoptosis in mouse myeloma cell lineage Sp2/0. Biochem Pharmacol. 1996;52:857–862. doi: 10.1016/0006-2952(96)82183-6. [DOI] [PubMed] [Google Scholar]
- Lee RK, Cai JP, Deyev V, Gill PS, Cabral L, Wood C, Agarwal RP, Xia W, Boise LH, Podack E, Harrington WJ., Jr Azydothymidine and interferon-alpha induce apoptosis herpesvirus-associated lymphoma. Cancer Res. 1999;59:5514–5520. [PubMed] [Google Scholar]
- Viora M, Di Genova G, Rivabene R, Malorni W, Fattorossi A. Interference with cell cycle progression and induction of apoptosis by dideoxynucleoside analogs. Int J Immunopharmacol. 1997;19:311–321. doi: 10.1016/s0192-0561(97)00041-6. [DOI] [PubMed] [Google Scholar]
- Tiefenthaler M, Amberger A, Bacher N, Hartmann BL, Ma R, Kofler R. Increased lactate production follows loss of mitochondrial membrane potential during apoptosis of human leukemia. Br J Haematol. 2001;114:574–580. doi: 10.1046/j.1365-2141.2001.02988.x. [DOI] [PubMed] [Google Scholar]
- Claessens YE, Cariou A. Severe lactic acidosis and multiple organ failure in HIV patients treated with nucleoside analogues reverse transcriptase inhibitors: a pilot study of treatment with L-carnitine. In: Desnuelle C, DiMauro S, editor. In Mitochondrial Disorders: From Pathophysiology to Acquired Defects. Heidelberg: Springer Verlag; 2002. pp. 161–172. [Google Scholar]
- Claessens YE, Cariou A, Monchi M, Soufir L, Azoulay E, Rouges P, Golgran-Toledano D, Branche F, Dhainaut JF. Detecting life-threatening lactic acidosis related to nucleoside-analogues treatment of HIV-infected patients, and treatment with L-carnitine. Crit Care Med. 2002. [DOI] [PubMed]
- Famularo G, Matricardi F, Nucera E, Santini G, De Simone C. Carnitine deficiency: primary and secondary syndroms. In: De Simone C, Famularo G, editor. In Carnitine Today. Heidelberg: Landes Bioscience; 1997. pp. 119–161. [Google Scholar]
- De Simone C, Tzantzoglou S, Jirillo E, Marzo A, Vullo V, Arrigoni Martelli E. L-carnitine deficiency in AIDS patients. AIDS. 1992;6:203–205. doi: 10.1097/00002030-199202000-00011. [DOI] [PubMed] [Google Scholar]
- Di Lisa F, Barbato R, Menabo R, Siliprandi N. Carnitine and mitochondrial dysfunction. In: De Simone C, Famularo G, editor. In Carnitine Today. Heidelberg: Landes Bioscience; 1997. pp. 95–104. [Google Scholar]
- Barile M, Valenti D, Hobbs GA, Abruzzese MF, Keilbaugh SA, Passarelle S, Quagliarello E, Simpson MV. Mechanism of toxicity of 3'-azido-3'-deoxythymidine: its interaction with adenylate kinase. Biochem Pharmacol. 1994;48:1405–1412. doi: 10.1016/0006-2952(94)90564-9. [DOI] [PubMed] [Google Scholar]
- Mhiri C, Baudrimont M, Bonne G, Geny C, Degoul F, Marsac C, Roullet E, Gherardi R. Zidovudine myopathy: a distinctive disorder associated with mitochondrial dysfunction. Ann Neurol. 1991;29:606–614. doi: 10.1002/ana.410290607. [DOI] [PubMed] [Google Scholar]
- Mutomba MC, Yuan H, Konyavko M, Adachi S, Yokoyama CB, Esser V, McGarry JD, Babior BM, Gottlieb RA. Regulation of the activity of caspases by L-carnitine and palmitoylcarnitine. FEBS Lett. 2000;478:19–25. doi: 10.1016/s0014-5793(00)01817-2. [DOI] [PubMed] [Google Scholar]
- Galli G, Fratelli M. Activation of apoptosis by serum deprivation in a teratocarcinoma cell line; inhibition by L-acetylcarnitine. Exp Cell Res. 1993;204:54–60. doi: 10.1006/excr.1993.1008. [DOI] [PubMed] [Google Scholar]
- Andrieu-Abadie N, Jaffresou JP, Hatem S, Laurent G, Levade T. L-carnitine prevents doxorubicin-induced apoptosis of cardiomyocytes: role of inhibition of ceramides generation. FASEB J. 1999;13:1501–1510. doi: 10.1096/fasebj.13.12.1501. [DOI] [PubMed] [Google Scholar]
- Paumen MB, Ishida Y, Muramatsu M, Yamamoto M, Honjo T. Inhibition of carnitine palmitoyltransferase I augments sphingolipid synthesis and palmitate-induced apoptosis. J Biol Chem. 1997;272:3324–3329. doi: 10.1074/jbc.272.6.3324. [DOI] [PubMed] [Google Scholar]
- Paumen MB, Ishida Y, Han H, Muramatsu M, Egushi Y, Tsudjimoto Y, Honjo T. Direct interaction of the mitochondrial membrane protein palmitoyl carnitine transferase I with Bcl2. Biochem Biophys Res Commun. 1997;231:523–525. doi: 10.1006/bbrc.1997.6089. [DOI] [PubMed] [Google Scholar]
- Pezeshkpour GH, Illa I, Dalakas MC. Ultrastructural characteristics and DNA immunochemistry in human immunodeficiency virus and zidovudine-associated myopathies. Hum Pathol. 1991;22:1281–1288. doi: 10.1016/0046-8177(91)90112-3. [DOI] [PubMed] [Google Scholar]
- Semino-Mora MC, Leon-Monzon M, Dalakas M. The effect of L-carnitine on the AZT-induced destruction of human myotubes. Part II: treatment with L-carnitine improves the AZT-induced changes and prevents further destruction. Lab Invest. 1994;71:773–781. [PubMed] [Google Scholar]
- Moretti S, Alesse E, Di Marzio L, Zazzeroni F, Ruggeri B, Marcellini S, Famularo G, Steinberg SM, Boschini A, Cifone MG, De Simone C. Effect of L-carnitine on human immunodeficiency virus-1 infection associated apoptosis: a pilot study. Blood. 1998;91:3817–3824. [PubMed] [Google Scholar]
- Brinkman K, Smeitink JA, Romijn JA, Reiss P. Mitochondrial toxicity induced by nucleoside-analogue reverse-transcriptase inhibitors is a key factor in the pathogenesis of antiretroviral-therapy-related lipodystrophy. Lancet. 1999;354:1112–1115. doi: 10.1016/S0140-6736(99)06102-4. [DOI] [PubMed] [Google Scholar]
- Loignon M, Toma E. L-carnitine for the treatment of highly active antiretroviral therapy-related hypertriglyceridemia in HIV-infected adults. AIDS. 2001;15:1194–1195. doi: 10.1097/00002030-200106150-00024. [DOI] [PubMed] [Google Scholar]
- Brinkman K, Vrouenraets S, Kauffmann R, Weigel H, Frissen J. Treatment of nucleoside reverse transcriptase inhibitor-induced lactic acidosis. AIDS. 2000;14:2801–2802. doi: 10.1097/00002030-200012010-00027. [DOI] [PubMed] [Google Scholar]
- Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiologic score (SAPSII) based on a European-North American multicenter study. JAMA. 1993;270:29057–29068. doi: 10.1001/jama.270.24.2957. [DOI] [PubMed] [Google Scholar]
- Cowan BN, Burns HJ, Boyle P, Ledingham IM. The relative prognostic value of lactate and haemodynamic measurements in early shock. Anaesthesia. 1984;39:750–755. doi: 10.1111/j.1365-2044.1984.tb06516.x. [DOI] [PubMed] [Google Scholar]


