Abstract
A case demonstrating compression of the right ventricular outflow tract by an unruptured coronary sinus of Valsalva aneurysm in which repair resulted in symptomatic improvement is presented. The pathology report revealed that the patient’s younger brother had died from a ruptured aneurysm of the coronary sinus of Valsalva. The present report is the first to describe a familial unruptured coronary sinus of Valsalva aneurysm raising questions regarding the screening of relatives of patients with sinus of Valsalva aneurysms of unknown etiology.
Keywords: Aneurysm, Aorta, Aortic valve, Congenital heart disease, Valsalva
Abstract
Les auteurs présentent ici un cas de compression de la chambre de chasse du ventricule droit par un anévrisme non rompu du sinus de Valsalva dont les symptômes ont pu être améliorés après une réparation. Le rapport de pathologie a révélé que le frère cadet du patient était décédé d’une rupture d’anévrisme du sinus de Valsalva. Il s’agit du premier rapport à décrire un cas d’anévrisme familial non rompu du sinus de Valsalva qui soulève la question du dépistage chez les proches de patients présentant un anévrisme du sinus de Valsalva d’étiologie inconnue.
Aneurysm of the coronary sinus of Valsalva (ASV) is rare. It may be congenital, sometimes in association with other cardiac defects (most commonly ventricular septal defect or coarctation), or it may be acquired. The first manifestation of ASV is most often related to rupture, whereas unruptured ASVs are rare. Although unruptured aneurysms are frequently asymptomatic without physical findings, they can be associated with complications and can compress adjacent structures. We present a case of a familial unruptured right ASV causing obstruction of the right ventricular outflow tract (RVOT) and subsequent evolution following repair.
CASE PRESENTATION
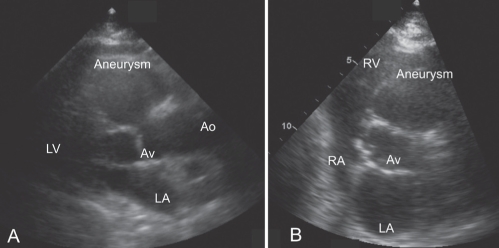
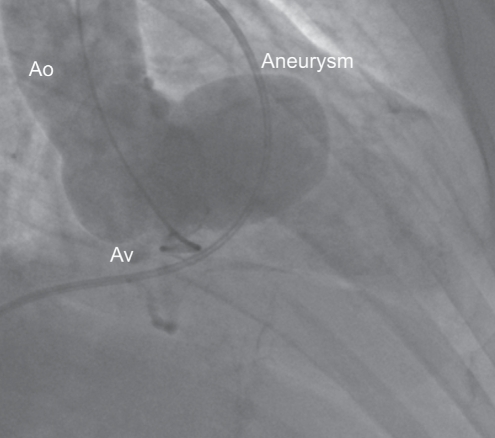
A 77-year-old woman presented with stable dyspnea on exertion (New York Heart Association [NYHA] class III), which she had been experiencing for the past year. Her medical history revealed only hypothyroidism and hysterectomy with bilateral salpingooophorectomy. A transthoracic echocardiography performed five years earlier was normal except for a mild increase in peak transvalvular pulmonary velocities (1.3 m/s). Examination revealed normal blood pressure and a systolic heart murmur (grade 3/6) best heard along the left sternal border. Further examination showed distension of the jugular veins and mild ankle edema. Recorded electrocardiogram alterations were a mild Q wave with inversion of the T wave in inferior leads. Computed tomography angiography of the chest showed no pulmonary embolism but revealed moderate proximal thoracic aorta ectasia. Pulmonary function tests were normal. Controlled transthoracic echocardiography (Figure 1) showed a right ASV and RVOT obstruction with a subvalvular pulmonary systolic gradient of 45 mmHg. Left ventricular contractility was normal on echocardiography with moderate aortic regurgitation (grade 3/4). Aortic angiography (Figure 2) confirmed a right ASV while cardiac catheterization confirmed RVOT obstruction with no shunt. Coronary angiography was normal. The patient was unable to undergo magnetic resonance imaging due to claustrophobia.
Figure 1).
Two-dimensional transthoracic echocardiographic images of parasternal long-axis (A) and parasternal short-axis (B) views showing a right coronary sinus of Valsalva aneurysm measuring 37 mm by 40 mm. Ao Aorta; Av Aortic valve; LA Left atrium; LV Left ventricle; RA Right atrium; RV Right ventricle
Figure 2).
Aortic angiography in the right anterior oblique view confirming the right coronary sinus of Valsalva aneurysm. Ao Aorta; Av Aortic valve
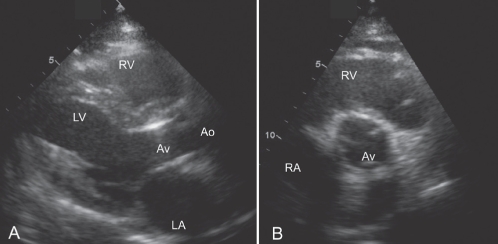
The decision was made to repair the aneurysm because the patient’s symptoms were likely related to RVOT obstruction and there was evidence of aneurysm progression on serial echocardiography. It was also known from the pathology report that the patient’s younger brother had died 24 years earlier at 48 years of age from a ruptured ASV. The ASV was repaired with a pericardial patch. The aortic valve was also replaced with a Carpentier-Edwards porcine valve (Edwards Lifesciences, Canada) because of aortic valve regurgitation progression during surgery. The postoperative course was uneventful. Transmission electron microscopy of the aneurysm wall showed degeneration of the media with fragmentation of elastin fibres. Transthoracic echocardiography performed three months after surgery (Figure 3) showed no recurrence of the aneurysm and no RVOT obstruction with normal pulmonary flow velocities. The patient’s symptoms on exertion also improved (NYHA class II).
Figure 3).
Two-dimensional transthoracic echocardiographic images of parasternal long-axis (A) and parasternal short-axis (B) views showing regression of the sinus of Valsalva aneurysm following repair with a pericardial patch and aortic valve replacement with a Carpentier-Edwards porcine valve (Edwards Lifesciences, Canada). Ao Aorta; Av Aortic valve; LA Left atrium; LV Left ventricle; RA Right atrium; RV Right ventricle
DISCUSSION
An ASV usually affects only one sinus, most commonly the right, although more than one sinus can be involved (1). Congenital ASVs are more common than acquired ASVs and are frequently associated with ventricular septal defect. Acquired ASVs may result from trauma, infection (syphilis or endocarditis) or atherosclerosis (2). The clinical presentation of unruptured ASV is commonly an asymptomatic incidental finding, although it can be associated with complications such as various valvular regurgitation, compression of a coronary artery (3), conduction blocks or, more often, obstruction of adjacent cardiac chambers, namely the right ventricle. Nine cases of compression of the RVOT by a sinus of Valsalva aneurysm have been reported, all of which involved the right coronary sinus of Valsalva, consistent with the aneurysm observed in our patient. More importantly, in three of these cases in which surgery for symptomatic RVOT obstruction was performed, repair of the ASV resulted in symptomatic improvement (1,4,5). Although the standard of care for a ruptured ASV entails repair of the aneurysm (6), reported experience with unruptured ASVs is limited (7). For our patient, we decided to perform surgery to prevent rupture of the aneurysm and hopefully improve symptoms.
Etiology of the current patient’s ASV was more likely a familial form of connective tissue disease because her sibling was also affected. Furthermore, in the present case, there was no evidence of infection, trauma or atherosclerotic disease. There is growing evidence of familial thoracic aortic aneurysms and dissections, inherited in an autosomal-dominant manner with a recently demonstrated association of certain gene loci (8). However, to our knowledge, the current report is the first to present a case of familial ASV. The current finding raises the question of whether relatives of an individual with an ASV of unknown origin should be screened.
REFERENCES
- 1.Malcolm I. Unruptured aneurysm of the sinus of Valsalva. Can J Cardiol. 1996;12:783–5. [PubMed] [Google Scholar]
- 2.Golberg N, Krasnow N. Sinus of Valsalva aneurysms. Clin Cardiol. 1990;13:831–6. doi: 10.1002/clc.4960131204. [DOI] [PubMed] [Google Scholar]
- 3.Lijoi A, Parodi E, Passerone GC, Scarano F, Caruso D, Ianneti MV. Unruptured aneurysm of the left sinus of Valsalva causing coronary insufficiency: Case report and review of the literature. Tex Heart Inst J. 2002;29:40–4. [PMC free article] [PubMed] [Google Scholar]
- 4.Huang CF, Liang CD, Chang JP, Tiao MM. Unruptured aneurysm of sinus of Valsalva with right ventricular outflow tract obstruction. Chang Gung Med J. 2001;24:746–50. [PubMed] [Google Scholar]
- 5.Haraphongse M, Ayudhya RK, Jugdutt B, Rossall RE. Isolated unruptured sinus of Valsalva aneurysm producing right ventricular outflow obstruction. Cathet Cardiovasc Diagn. 1990;19:98–102. doi: 10.1002/ccd.1810190208. [DOI] [PubMed] [Google Scholar]
- 6.Lin CY, Hong GJ, Lee KC, Tsai YT, Tsai CS. Ruptured congenital sinus of Valsalva aneurysms. J Cardiac Surg. 2004;19:99–102. doi: 10.1111/j.0886-0440.2004.04022.x. [DOI] [PubMed] [Google Scholar]
- 7.Vural KM, Sener E, Tasdemir O, Bayazit K. Approach to sinus of Valsalva aneurysms: A review of 53 cases. Eur J Cardiothorac Surg. 2001;20:71–6. doi: 10.1016/s1010-7940(01)00758-8. [DOI] [PubMed] [Google Scholar]
- 8.Milewicz DM, Fadulu VT.Thoracic aortic aneurysms and aortic dissections<http://www.geneclinics.org> (Version current at May 13, 2004).