Abstract
Context:
Various consensus and position statements recommend a multifaceted approach when diagnosing a possible concussion. The effectiveness of these materials depends largely on their content being disseminated to educators and to those in the clinical setting.
Objective:
To identify the concussion management methods and guidelines currently taught in the athletic training classroom and clinical settings and to track the dissemination of the Vienna guidelines throughout the educational curriculum.
Design:
A 17-question Internet survey.
Setting:
A Web link was e-mailed to the program directors and certified athletic trainers holding educational positions in athletic training at 300 accredited programs in the United States.
Patients or Other Participants:
513 program directors and athletic trainers.
Main Outcome Measure(s):
Survey questions addressed education level, years of certification, employment setting, concussion assessment and return-to-play guidelines used in the clinical setting and the classroom, and clinical and teaching preferences for existing position statements and concussion grading systems. The Vienna guidelines' “simple” and “complex” definitions of concussions were provided with the return-to-play stepwise approach.
Results:
The National Athletic Trainers' Association position statement was the most widely used method of assessing, managing (61%), and making return-to-play decisions (47%) among participants. More than half of participants (66%) had never heard of the Vienna guidelines. After reading the Vienna guidelines' definitions and return-to-play criteria, nearly three-fourths of participants agreed with them. In addition, 68% said that they would use them, and 84% reported that they would teach them to students.
Conclusions:
The majority of program directors and certified athletic trainers used a multidimensional approach to assess and manage a concussion. The National Athletic Trainers' Association position statement and Vienna guidelines were underused in both the classroom and clinical settings.
Keywords: mild traumatic brain injuries, Vienna guidelines, grading scales, position statements
Key Points
Most of the program directors and athletic trainers used a multifaceted approach to assessing and managing concussions.
Even though the National Athletic Trainers' Association position statement was the most frequently used reference for assessing and managing concussion and making return-to-play decisions, both the position statement and the Vienna guidelines were underused in the classroom and clinical settings.
The evaluation and management of sport-related concussion continue to be controversial topics among sports medicine professionals. Currently, no consensus exists among researchers or clinicians with respect to concussion definition, severity measurement, diagnostic measures, or return-to-play criteria. In contrast with other athletic injuries, no simple test is available for diagnosing a concussion. Therefore, concussion evaluation and management should be considered a multifaceted protocol.1–5 Numerous consensus and position statements have recommended the use of a clinical examination, symptom checklist, postural stability assessment, and neurocognitive testing.2–4,6 Furthermore, many consensus and position statements have attempted to amalgamate current research on concussion in an attempt to provide clarity and agreement between research and practice.2–4 However, the utility of these consensus and position statements largely depends on the dissemination of this information to the clinical setting and to those responsible for educating future clinicians.
The classroom and clinical components of the athletic training education program are structured around the Competencies in Athletic Training7 (published by the National Athletic Trainers' Association [NATA] Education Council) and the Role Delineation Study, 5th edition (conducted and published by the Board of Certification).8 The Matrix for the Competencies, 4th edition (available for purchase at http://www.nataec.org), includes the following competency: “Define cerebral concussion, list the signs and symptoms of concussions, identify the methods for determining the neurocognitive status of a patient who sustains a concussion and describe contemporary concepts for the management and return-to-participation of a patient who sustains a concussion.”9 However, the NATA Education Council did not recommend which concussion guidelines should be taught in the classroom and the clinical setting. Therefore, it is up to each institution to stay current with the most up-to-date concussion guidelines.
Regardless of the position statement or consensus paper, very few authors10,11 have specifically examined which methods of assessing and managing concussion clinicians use. Furthermore, several investigators10,11 have suggested that athletic trainers (ATs) did not use one specific method for evaluation and return-to-play criteria. Ferrara et al11 administered a 21-item survey at the 1999 NATA Annual Meeting and Clinical Symposia to determine familiarity with standardized methods of concussion assessment and use of assessment tools and return-to-play guidelines. The ATs most often reported using a clinical examination and symptom checklist to evaluate a concussion and the Colorado Medical Society (CMS),12 American Academy of Neurology (AAN),13 and Cantu5 guidelines for grading the concussion. Of note, the majority of participants agreed that standardized methods of concussion assessment would provide more information than a clinical examination alone.
Notebaert and Guskiewicz10 surveyed 927 ATs about their clinical practices for concussion assessment and management. The ATs most often used the AAN13 guidelines, followed by the CMS12 and Cantu5 concussion guidelines, for return to play. The majority of participants reported using the clinical examination and symptom checklist to assess a concussion. The researchers concluded that only 3% of participants complied with the NATA position statement. However, the statement2 was only available to clinicians for approximately 1 year before the study; therefore, a lack of dissemination may have contributed to this low compliance rate.
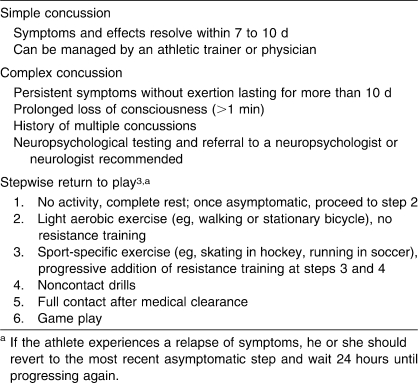
A group of neurosurgeons, neurologists, neuropsychologists, and sports medicine physicians—all regarded as experts in sport-related concussion—drafted a consensus statement at the First International Symposium on Concussion in Sport3 held in Vienna, Austria, in 2001. The statement was revised at the Second International Symposium on Concussion in Sport4 in Prague, Czech Republic, in 2004. The major considerations and recommendations made at these symposia consisted of replacing the grading scales with a “simple” and “complex” classification rubric, revised return-to-play criteria, and the endorsement of neurocognitive testing as the cornerstone for concussion management.4 More specifically, a simple concussion resolves within 7 to 10 days, can be managed by a physician or AT, and does not require formal neuropsychological testing.4 A complex concussion includes more prolonged symptoms or neurocognitive impairments and requires formal neuropsychological testing; any athlete who has sustained multiple concussions is automatically labeled as having a complex concussion.4 The NATA position statement2 suggested 3 approaches an AT could use when evaluating an athlete with a concussion: (1) grading the concussion at the time of injury based upon a previously agreed grading scale (eg, Cantu,5 AAN11), (2) deferring grading the concussion until all symptoms have resolved, or (3) not using a grading scale and making determinations based on the athlete's recovery. The AT should decide an approach for managing concussion before the season starts, and the approach should be consistent regardless of the situation (eg, athlete, sport, importance of competition).
The Prague guidelines3 did not endorse any return-to-play guidelines but recommended a new stepwise protocol for return to play. The Vienna return-to-play guidelines were based on the Canadian Academy of Sports Medicine Committee guidelines14 published in 2000. This protocol begins with no activity or complete rest until the concussed athlete is asymptomatic. Once asymptomatic, the athlete performs light aerobic exercise with no resistance training.3 If the athlete continues to be asymptomatic, he or she proceeds to the next stage. The remaining stages (eg, sport-specific exercise, noncontact drills) must be completed without symptoms returning over a 24-hour period.3 If symptoms return, the athlete must revert to the preceding stage until asymptomatic and then begin this stepwise progression again.3 Once the athlete can complete noncontact drills without experiencing symptoms, he or she can begin full contact drills and return to game play with medical clearance.3 The NATA position statement2 recommended a similar protocol for returning a concussed athlete to participation. If the athlete is asymptomatic after exertional maneuvers (eg, biking, push-ups, jogging), progression to sport-specific skills is appropriate. Upon completion of symptom-free sport-specific skills, neuropsychological and postural stability assessment is suggested before the athlete returns to full contact participation. The NATA position statement2 does not offer a time frame between steps, which is a major difference from the Vienna guidelines.3
The Concussion in Sport Group3 has been established to consider the findings from research and practice in order to make recommendations regarding the management of sport-related concussion. The education and clinical training of future practitioners should include these guidelines. However, no researchers to date have examined whether the dissemination of the Vienna guidelines3 has taken place. Therefore, our purpose was 2-fold: to identify current concussion management methods and guidelines being taught in the classroom and clinical settings and to investigate whether the Vienna guidelines3 were being disseminated throughout the educational curriculum.
METHODS
Approval for the study and use of human participants was granted by the university's institutional review board. By completing and returning the online survey, volunteers provided implied consent. Approximately 300 accredited program directors and 1200 ATs from all 300 accredited programs were contacted via e-mail during the fall of 2007. Our sample size did not include an equal number of staff ATs and faculty ATs, because we wanted to survey all ATs at each accredited institution. In addition, we did not include equal numbers of participants from each institution, because some institutions employed 10 staff ATs, whereas others employed only 1 or 2 staff ATs. We obtained program directors' e-mail addresses through the Commission on Accreditation of Athletic Training Education Web site and than obtained individual ATs' e-mail addresses by going to each institution's Web site. Most of the ATs' e-mail addresses were available on the Department of Intercollegiate Athletics Web site at each institution. The e-mail contained an overview and explanation of the study and a hyperlink to the survey. Three weeks after the initial e-mail, we sent a reminder e-mail to all participants. SurveyMonkey.com (Menlo Park, CA) was the host site for the survey, which took approximately 10 minutes to complete. The survey was a 17-item questionnaire adapted and modified from a 21-item survey used by Ferrara et al.11 An expert panel of program directors and ATs (n = 8) developed the questionnaire and also reviewed it for face and content validity. The questionnaire was pilot tested on ATs, resulting in a few modifications to survey questions. The survey evaluated program directors and ATs' clinical and teaching practices in relation to sport-related concussions. Our intent was not to differentiate between classroom and clinical settings, because clinicians teach clinical skills to athletic training students in the clinical setting. The survey obtained demographic information pertaining to education level, years of experience as an AT, employment setting, and whether the participant graduated from an internship or accredited program. The survey also contained 5 questions pertaining to the assessment of a concussion and return-to-play guidelines used in the clinical setting and in the classroom. More specifically, volunteers were asked to identify their usage of assessment and management measures such as the Balance Error Scoring System,15 Standardized Assessment of Concussion,16 neuropsychological tests (computerized or paper and pencil), and clinical examination. Participants also were asked whether they used or taught the NATA position statement2 or guidelines from the AAN,13 Cantu,5 Vienna,3 or CMS.12 Participants were then presented with the definitions of simple and complex concussions and return-to-play protocol from the Vienna guidelines3 (Table 1). Participants were asked whether they agree with the Vienna guidelines and whether they would use or teach them.3 The NATA position statement was published in 2004, and the Vienna guidelines3 were published in 2002; therefore, respondents had 3 and 5 years, respectively, to familiarize themselves with the concussion position statements. All responses were returned to the survey Web site as anonymous data. Participants were allowed to withdraw at any time without penalty and were allowed to skip any questions. Responses were downloaded to a Microsoft Excel (version 2007; Microsoft Corp, Redmond, WA) spreadsheet, and descriptive statistics were calculated for each response. In addition, a series of χ2 analyses were conducted to examine the relationships among level of education (bachelor's degree, master's degree, or doctorate) and years of experience (0 to 5, 6 to 10, 11 to 15, 16 to 20, or 21 or more years) and awareness, usage, and teaching of the Vienna guidelines.3
Table 1.
RESULTS
A total of 513 participants completed the survey, for a response rate of 34.2%. Participants had an average of 11.1 years of experience as an AT. Approximately half of the volunteers had earned MS degrees (216/511[42.3%]); 17.2% (88/511) earned PhD degrees, and 14.7% (75/511) had earned MEd degrees. In addition, more than half of the participant pool graduated from an accredited athletic training education program (301/509 [59.1%]). The most common employment position held by participants was assistant athletic trainer (147/509 [28.9%]), followed by program director (135/509 [26.5%]), head athletic trainer (98/509 [19.3%]), faculty or staff position (52/509 [10.2%]), clinical coordinator (41/509 [8.1%]), graduate assistant (32/509 [6.3%]), and clinical instructor (4/509 [0.8%]). The majority of volunteers were employed at the Division I university level (240/509 [47.2%]), followed by Division III (127/509 [25%]), Division II (99/509 [19.4%]), and other (43/509 [8.4%]).
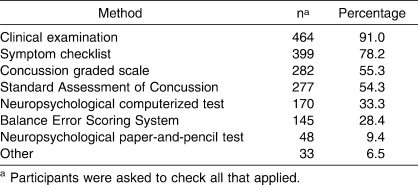
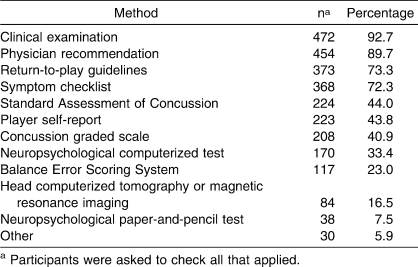
Participants reported using a variety of different methods to assess a concussion (Table 2). To evaluate a concussion, a higher percentage of participants used a clinical examination (464/510 [91%]) than a symptom checklist (399/510 [78.2%]), concussion grading scale (282/510 [55.3%]), Standard Assessment of Concussion14 (277/510 [54.3%]), or neuropsychological computer test (170/510 [33.3%]). Return-to-play decisions were made using a clinical examination (472/509[92.7%]) and physician recommendation (454/509 [89.2%]; Table 3). Three-quarters of participants also used return-to-play guidelines (373/509 [73.3%]) and a symptom checklist (368/509 [72.3%]) for return-to-play decisions.
Table 2.
Methods Used to Assess Concussion
Table 3.
Methods Used for Return-to-Play Decisions After Concussion
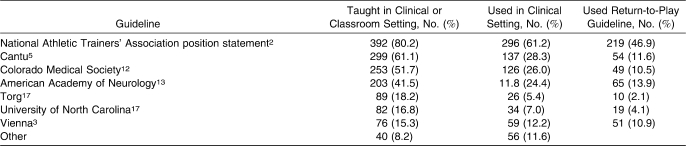
The NATA position statement2 was taught 80% of the time in the classroom or clinical setting (or both), followed by the Cantu5 (299/489 [61.1%]), CMS12 (253/489 [51.7%]), and AAN13 (203/489 [41.5%]) guidelines (Table 4). A total of 61% of the participants surveyed used the NATA position statement2 (296/484 [61.2%]) for concussion guidelines in the clinical setting. This was followed by the Cantu5 (137/484 [28.3%]), CMS12 (126/484 [26.0%]), and AAN13 (118/484 [24.4%]) guidelines. The Vienna guidelines3 were used only 12.2% (59/484) of the time. For decisions regarding return to play, almost half the participants used the NATA position statement2 (219/467 [46.9%]), and only 10.9% used the Vienna guidelines3 (Table 4). Approximately two-thirds of those surveyed (336/506 [66.4%]) had never heard of the Vienna guidelines3 for concussion management, and the majority (431/502 [85.9%]) did not use them. Moreover, only a small percentage of the participants (76/496 [15.3%]) taught the Vienna Guidelines.3 After participants were presented with the Vienna guidelines'3 definitions of simple and complex concussions and return-to-play stepwise process, 73.3% (357/487) agreed with them, 68.4% (331/484) stated they would use them, and 84% (404/481) stated they would now teach them.3
Table 4.
Guidelines and Grading Scales Participants Taught and Used
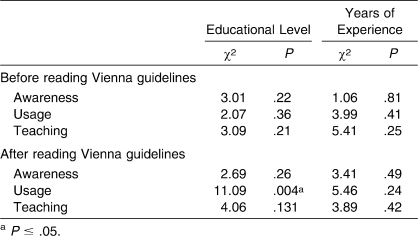
Relationships between participants' level of education and willingness to use the Vienna guidelines3 were noted (χ22 = 11.09, P = .004). No relationship was seen between participants' level of education and awareness (χ22 = 2.69, P = .26) and teaching (χ22 = 4.06, P = .13) of the Vienna guidelines3 (Table 5) or between years of experience and awareness (χ24 = 3.41, P = .49), usage (χ24 = 5.46, P = .24), and teaching (χ24 = 3.89, P = .42) of the Vienna guidelines.3
Table 5.
Relationships Among Participants' Level of Education, Years of Experience, and Awareness, Usage, and Teaching of the Vienna Guidelines3
DISCUSSION
The purpose of the present study was to identify concussion management methods and guidelines currently taught in the classroom and clinical settings. More specifically, we focused on the dissemination of the Vienna guidelines3 to the educational curriculum. Increased awareness and knowledge of new concussion assessment methods and tools has improved the identification and management of concussion in the clinical setting. Although concussion experts disagree on a standardized assessment of and management method for concussion, they do agree that a symptomatic athlete should not be allowed to return to participation.2–4
The Vienna guidelines3 were published in 2002; however, only 12% of participants in this study reported using them. This finding may be overestimated, because we did not delineate between researchers and clinicians. Some participants may have been in positions that require them to conduct research, and those who work in a scholarly setting are more likely to stay abreast of the current literature. Nonetheless, the low response rate could represent either a lack of knowledge or lack of agreement about the Vienna guidelines.3 The former seems to be a more plausible explanation for this finding, because more than 68% of participants indicated after reading a description that they agreed with or would use the Vienna guidelines. Therefore, the information in the Vienna guidelines may not have been effectively disseminated, and practitioners and clinicians may not be aware of the current literature on sport-related concussion.
The use of the Vienna guidelines3 as a return-to-play guide (12.2%) paralleled the extent to which the guidelines were taught (15.3% instruction, 12.2% clinical instruction). At the outset of the study, two-thirds of ATs surveyed had never heard of the Vienna guidelines. However, once participants read a description of them, 68% and 84% reported that they would use and teach them, respectively. This pretest to posttest shift from 15% to 84% is further evidence that education about the Vienna guidelines is a key concern. One could hypothesize that use of the guidelines would increase as more ATs are educated about them during their athletic training education programs or through continuing education programs sponsored by the NATA. As researchers and educators, we need to better disseminate this information to clinicians and instructors, so they can incorporate it in the academic curriculum.
We also identified the use of neuropsychological testing for managing concussion. More specifically, one-third (33.4%) of participants reported using a computerized neuropsychological test battery, which is twice the number Notebaert and Guskiewicz10 noted. This finding highlights the increasing popularity of neuropsychological testing among sports medicine practitioners. Another possible explanation for this finding is that we sampled only university ATs, whereas Notebaert and Guskiewicz10 conducted a random sample of ATs. In our study, the use of the Vienna guidelines was correlated with level of education; a similar relationship may exist with use of a neuropsychological test battery. The Vienna guidelines referred to neuropsychological testing as the cornerstone of concussion management.3 Furthermore, all consensus and position statements over the past 5 years have advocated the use of neuropsychological testing for concussion management.2–4
Our study is not without certain limitations inherent to survey research. This survey had a 34% response rate. One possible explanation for this low response rate may be that some program directors at accredited universities did not have clinical responsibilities. Therefore, these individuals may have chosen not to participate in this study because they had not been clinically active for numerous years. We have no way of knowing whether the 66% of invited ATs who elected not to participate were similar to or much different from the ATs who did participate. Another limitation was the exclusive use of accredited institutions. We selected accredited institutions because ATs educate athletic training students on the assessment and management of concussions at these facilities. However, limiting the population in this manner may have a negative effect on the external validity (generalizability) of this study.
Given the availability of numerous concussion methods and tools and increased awareness of concussion in both the media and publications, we would hope ATs are now in a better position to assess and manage concussions. Our findings indicate that the NATA position statement2 and Vienna guidelines3 may be underused in both the classroom and clinical settings. The athletic training education curriculum should focus more on teaching new assessment methods and management protocols that encompass a multidimensional approach, as noted in several consensus papers.2,3 These findings support the need for the Commission on Accreditation of Athletic Training Education to reevaluate relevant competencies that should be taught in the athletic training curriculum, including those regarding sport-related concussion.
Footnotes
Tracey Covassin, PhD, ATC; Robert Elbin III, MA; and Jennifer L. Stiller-Ostrowski, PhD, ATC, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article.
REFERENCES
- 1.Oliaro S, Anderson S, Hooker D. Management of cerebral concussion in sports: the athletic trainer's perspective. J Athl Train. 2001;36(3):257–262. [PMC free article] [PubMed] [Google Scholar]
- 2.Guskiewicz K.M, Bruce S.L, Cantu R, et al. National Athletic Trainers' Association position statement: management of sport-related concussion. J Athl Train. 2004;39(3):280–297. [PMC free article] [PubMed] [Google Scholar]
- 3.Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the 1st International Symposium on Concussion in Sport, Vienna 2001. Clin J Sport Med. 2002;12(1):6–11. doi: 10.1097/00042752-200201000-00005. [DOI] [PubMed] [Google Scholar]
- 4.McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Br J Sports Med. 2005;39(4):196–204. doi: 10.1136/bjsm.2005.018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cantu R.C. Posttraumatic retrograde and anterograde amnesia: pathophysiology and implications in grading and safe return to play. J Athl Train. 2001;36(3):244–248. [PMC free article] [PubMed] [Google Scholar]
- 6.Wojtys E.M, Hovda D, Landry G, et al. Current concepts: concussion in sports. Am J Sports Med. 1999;27(5):676–687. doi: 10.1177/03635465990270052401. [DOI] [PubMed] [Google Scholar]
- 7.National Athletic Trainers' Association. Athletic Training Educational Competencies. 4th ed. Dallas, TX: National Athletic Trainers' Association; 2006. [Google Scholar]
- 8.Board of Certification. Role Delineation Study. 5th ed. Omaha, NE: Board of Certification; 2006. [Google Scholar]
- 9.National Athletic Trainers' Association Education Council. Athletic Training Educational Competencies. 4th ed. Dallas, TX: 2006. [Google Scholar]
- 10.Notebaert A.J, Guskiewicz K.M. Current trends in athletic training practice for concussion assessment and management. J Athl Train. 2005;40(4):320–325. [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrara M.S, McCrea M, Peterson C.L, Guskiewicz K.M. A survey of practice patterns in concussion assessment and management. J Athl Train. 2001;36(2):145–149. [PMC free article] [PubMed] [Google Scholar]
- 12.Colorado Medical Society Sports Medicine Committee. Proceedings of the Mild Brain Injury in Sports Summit. Dallas, TX: National Athletic Trainers' Association; 1994. Guidelines for the management of concussion in sports; pp. 106–109. [Google Scholar]
- 13.American Academy of Neurology. Practice parameter: the management of concussion in sports (summary statement). Report of the Quality Standards Subcommittee. Neurology. 1997;48(3):581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- 14.Canadian Academy of Sport Medicine Concussion Committee. Guidelines for assessment and management of sport-related concussion. Clin J Sport Med. 2000;10(3):209–211. doi: 10.1097/00042752-200007000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Guskiewicz K.M, Ross S.E, Marshall S.W. Postural stability and neuropsychological deficits after concussion in collegiate athletes. J Athl Train. 2001;36(3):263–273. [PMC free article] [PubMed] [Google Scholar]
- 16.McCrea M, Kelly J.P, Randolph C, et al. Standardized assessment of concussion (SAC): on-site mental status evaluation of the athlete. J Head Trauma Rehabil. 1998;13(2):27–35. doi: 10.1097/00001199-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Scifers J.R. Special Tests for Neurological Examination. Thorofare, NJ: Slack Inc; 2008. pp. 65–71. [Google Scholar]