Abstract
COPD is a major cause of mortality and morbidity worldwide with an estimated 2.75 million deaths in 2000 (fourth leading cause of death). In addition to the considerable morbidity and mortality associated with COPD, this disease incurs significant healthcare and societal costs. Current COPD guidelines acknowledge that the following can improve COPD mortality: smoking cessation; long-term oxygen therapy; and lung volume reduction surgery in small subsets of COPD patients. To date, no randomized controlled trials have demonstrated an effect of pharmacological treatment on mortality, although several observational studies suggest that both long-acting bronchodilators and inhaled corticosteroids may provide a survival benefit. The possibility that these treatments reduce mortality is being investigated in ongoing large-scale clinical trials.
Keywords: COPD, epidemiology, mortality, morbidity, treatment
Introduction
COPD represents a significant and growing healthcare concern as a leading cause of morbidity and mortality worldwide. According to the Global Burden of Disease (GBD) study 2000, COPD was responsible for an estimated 2.75 million deaths worldwide (Lopez et al 2006), half of which were documented in the Western Pacific region. An earlier study estimated that 2.2 million deaths worldwide were caused by COPD (Murray and Lopez 1997a). In the USA, COPD is currently the fourth leading cause of death and is projected to be the third by 2020 (US Department of Health and Human Services 2003).
According to the American Thoracic Society/European Respiratory Society (ATS/ERS) guidelines, COPD is characterized by airflow limitation that is not fully reversible. This airflow limitation is usually progressive and is associated with an abnormal inflammatory response of the lungs to noxious particles or gases. Although COPD predominantly affects the lungs, it is also associated with significant systemic consequences. Important symptoms of COPD range from chronic cough and sputum production to dyspnea. The single most important risk factor is a history of exposure to tobacco smoke; other important factors include occupational exposure to dusts and chemicals, lower socio-economic status, and genetic predisposition.
A diagnosis of COPD should be considered if any of these key indicators are present and confirmed by spirometry. Both the ATS/ERS and the Global Initiative for Obstructive Lung Disease (GOLD) guidelines state that a FEV1/FVC ratio <0.7 confirms the diagnosis of COPD. It should be noted that there is a decline in FEV1/FVC ratio with age and it is possible that some older, healthy individuals may be incorrectly diagnosed as having COPD (Crapo and Morris 1989; Hardie et al 2002; Barreiro and Perillo 2004); however, this issue is subject to controversy and data from cohort studies are not yet available. Furthermore, patients classified as GOLD stage 0 or stage 1 may have FEV1 ≥ 80% of predicted and are defined as either being at risk for, or having, mild COPD (Table 1) (Celli et al 2004; GOLD 2005). Disease stage is regarded as a general indication of COPD severity which, together with other information such as presence and severity of symptoms, frequency of exacerbations, presence of comorbid conditions, and history of asthma or exposure to risk factors, determines the most optimal approach to management.
Table 1.
Classification of severity of COPD using GOLD criteria (GOLD 2005)
| Stage | Characteristic | ||
|---|---|---|---|
| FEV1/FVCa | FEV1, % predicteda | Chronic symptomsb | |
| 0 (at risk) | Normal | Normal | + |
| I (mild COPD) | <70% | ≥ 80% | ± |
| II (moderate COPD) | <70% | <80% but ≥ 50% | ± |
| III (severe COPD) | <70% | <50% but ≥ 30% | ± |
| IV (very severe COPD) | <70% | <30%; or <50% with chronic respiratory failurec | ± |
Classification based on post-bronchodilator FEV1.
Cough, sputum production.
Arterial partial pressure of oxygen (PaO2) less than 8.0 kPa (60 mmHg) with or without arterial partial pressure of CO2 (PaCO2) greater than 6.7 kPa (50 mmHg) while breathing air at sea level.
Abbreviations: FEV1, forced expiratory volume in one second; FVC, forced vital capacity.
COPD runs an insidious course and is often undiagnosed for many years, particularly in its early stages (Anto et al 2001). The progression of the disease varies by COPD phenotype, a concept that is currently poorly understood. From the early stages of COPD and as the disease develops, chronic inflammation of the airways and lung parenchyma result in progressive airflow limitation with an accelerated rate of decline in FEV1 and increased hyperinflation, which cause breathing difficulties and reduce exercise tolerance (Hogg et al 2004; Sutherland and Cherniack 2004). Pathological changes are observed in the central and peripheral airways, the parenchyma, and the pulmonary vasculature. In addition to inflammation, an imbalance of proteinases and antiproteinases in the lungs and oxidative stress are also important in the pathogenesis of COPD (Repine et al 1997). These pathological changes result in the well recognized physiological abnormalities of COPD: mucous hypersecretion and ciliary dysfunction; airflow limitation and hyperinflation; destruction of alveoli and emphysema; gas exchange abnormalities; pulmonary hypertension; and various systemic effects (Matsuba et al 1989; O’Donnell et al 2001; Hogg et al 2004).
The clinical manifestations of COPD are generally well understood, but the underlying pathogenesis of COPD is less well established. Even less certain are the true extent and burden of mortality associated with COPD, and whether this burden can be altered by non-pharmacological or pharmacological approaches. To address this knowledge gap, this paper reviews the published data on the mortality burden of COPD and considers the data describing the impact of currently available therapeutic interventions on mortality.
Causes of death in COPD
Despite the high global death toll and cost of COPD, we are still learning more about the mechanisms that cause death in patients with COPD. Clinical trial data and extensive review of clinical patients show that a range of factors including lung failure, cor pulmonale, cardiovascular disease, and lung cancer are all important contributors to death in patients with COPD (Braghiroli et al 1997; Zielinski et al 1997; Waterhouse et al 1999; Anthonisen et al 2005). Large population-based studies have also reported on the causes of death in COPD patients. Hansell et al (2003a) recently analyzed death certificate data in England and Wales between 1993 and 1999 that included more than 300 000 deaths in patients with COPD. The aims of the study were to quantify the extent to which obstructive lung disease (OLD) contributed to death and to better characterize specific causes of death in OLD patients. The authors noted that approximately 60% of deaths in COPD patients were attributed to COPD itself, while 25% of the patients died as a result of diseases of the circulatory system and more than 5% of deaths were attributed to neoplasms (Hansell et al 2003a).
In contrast, data from Finland gathered over a 20-year period indicated that coronary heart disease and other circulatory diseases were the primary causes of death in patients with COPD (37.3%), followed by COPD itself (30.2%), lung cancer (12.1%), and other malignancies (7.9%) (Vilkman et al 1997; Keistinen et al 1998). Taken together, these data indicate that COPD itself and other respiratory causes, cardiovascular disease, and lung cancer are the most important causes of death in COPD patients.
A growing body of trial data suggests that systemic and pulmonary inflammation may provide a mechanistic link between COPD, cardiovascular disease, lung cancer and other comorbid conditions (Mukhopadhyay et al 1995; Wedzicha et al 2000; Sin and Man 2003a; Wright and Christman 2003; Gan et al 2004; Greten et al 2004; Hogg et al 2004; Pikarsky et al 2004). COPD has been identified as a significant risk factor for death in patients with cardiac disease in two studies involving a total of 16 000 patients (Berger et al 2004; Curkendall et al 2004). Similarly, COPD was identified as an important risk factor for death in patients with lung cancer (Sekine et al 2002).
The burden of COPD mortality
While there is a considerable body of data concerning the number of deaths attributed each year to COPD throughout the developed world, particularly for the USA, there is a paucity of data for developing world regions. The availability of accurate epidemiological data for COPD mortality is hampered by the expense involved in collecting and collating the information, misclassification of cause of death by attributing COPD-related deaths to other causes, or under-diagnosis; all of these factors under-estimate the true burden of COPD mortality.
Misclassification potentially omits large categories of patients with COPD by focusing only on chronic bronchitis and emphysema (ICD [International Classification of Disease] codes 491–492). One of the largest categories of COPD mortality, ICD 496 (chronic airway obstruction not elsewhere classified) has previously not been consistently included in the World Health Organization (WHO) estimates of COPD mortality, leading to a potential under-estimation of COPD deaths (European Respiratory Society and European Lung Foundation 2003).
Another possible source of COPD death under-estimation is provided by evidence from asthma mortality reports. There are strong data that many deaths attributed to asthma, particularly in patients aged over 65 years, are due to misclassification of other respiratory diseases as asthma (Jenkins et al 1992; Smyth et al 1996; Reid et al 1998). For example, in the study by Reid and colleagues, based on death certificates in northern England, COPD was considered to be the true cause of 28 of the 55 deaths in which asthma was certified as the direct cause. Such “diagnostic transfer” over-represents asthma-related deaths and under-represents COPD-related deaths. Finally, difficulties in verifying death certificates and disease coding practices are a considerable potential problem in international mortality studies that include data from diverse national sources.
In general, COPD is under-diagnosed, even in developed countries (Mannino et al 2000). Published data probably under-estimate COPD deaths due to misclassification of cause of death due to attributing COPD-related deaths to other causes (Mannino et al 1997, 2003), or reliance only upon underlying causes of death and failure to consider accompanying diagnoses of COPD on death certificates (Hansell et al 2003b). The WHO previously published mortality rates for the combined category of “bronchitis, emphysema and asthma” (ICD codes 490–493), which omits the largest category of COPD mortality (ICD code 519.3 in the eighth revision and ICD code 496 in the ninth revision). As a result there may be considerable underestimation of the scale of COPD deaths (Loddenkemper et al 2003).
Despite these challenges, however, a number of large national and international surveys describing COPD mortality have been published.
Global data
The GBD study for 1990 (Murray and Lopez 1997a, 1997b, 1997c) and the recent update for 2000 (Lopez et al 2006) are important sources of worldwide data for COPD mortality. The original GBD study accessed various national and international data sources and requested expert opinion to estimate worldwide and regional cause-of-death patterns in 1990 for more than 100 causes of death, including COPD. In 1990, 2 211 000 deaths were attributed to COPD, representing 4.4% of all deaths recorded and making COPD then the sixth leading cause of worldwide mortality. The recent update of the GBD study shows 2.7 million deaths attributed to COPD in 2000 (4.8% of all deaths), making it the fifth leading cause of death worldwide after ischemic heart disease, cerebrovascular disease, lower respiratory tract infections, and human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS). Half of these deaths occurred in the Western Pacific region and the majority of these in China, where the incidence of COPD among subjects aged ≥ 60 years is 2–3 times higher than in other WHO regions. The updated report also shows about 400 000 deaths attributed to COPD each year in industrialized countries. However, the authors note that the 2000 data may still represent an under-estimate of the actual toll of COPD deaths. Table 2 shows the estimated COPD deaths by WHO region for 2002 (Lopez et al 2006).
Table 2.
Estimated COPD deaths by WHO region in 2000 (Lopez et al 2006)
| WHO region | Deaths (000s) |
|---|---|
| Africa Aa | 52 |
| Africa E | 65 |
| Americas A | 141 |
| Americas B | 90 |
| Americas D | 10 |
| Southeast Asia B | 100 |
| Southeast Asia D | 556 |
| Europe A | 140 |
| Europe B | 45 |
| Europe C | 76 |
| Eastern Mediterranean B | 15 |
| Eastern Mediterranean D | 80 |
| Western Pacific A | 21 |
| Western Pacific B | 1354 |
| World | 2748 |
Mortality strata: A, very low child/adult mortality; B, low child/adult mortality; C, low child and high adult mortality; D, high child and adult mortality; E, high child and very high adult mortality.
The WHO World Health Report, 2002, estimated that global mortality from COPD was 44.2/100 000 population (WHO 2002), with mortality highest in the Western Pacific region (79.8/100 000 population). Mortality due to COPD has been projected to rise to 4.5 million deaths in 2020, based upon the GBD data, with COPD by then the third leading cause of death (Murray and Lopez 1997a).
US data
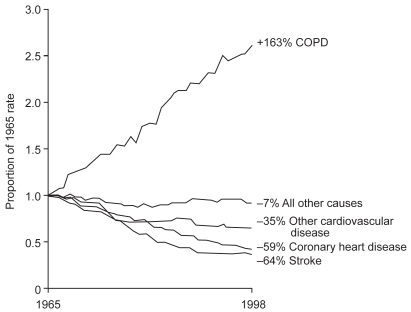
As with the global data, US mortality data show a marked increase in COPD mortality over recent decades, with a 163% increase in the age-adjusted COPD mortality rate from 1965 to 1998, to approximately 120 000 deaths per year by 2000 (Pauwels and Rabe 2004; GOLD 2005). These increases are particularly striking in light of the decreases in age-adjusted death rates for all other major causes of mortality (Figure 1). The most recent assessment specific to COPD mortality in the USA was reported in November 2004 by the American Lung Association (ALA) (ALA 2004), which included an analysis of data from 1979 to 2002 collected from US national surveys and statistics on mortality attributable to COPD. Age-adjusted death rates show an almost two-fold increase in COPD mortality from 24.2 per 100 000 population in 1979 to 42 deaths per 100 000 population in 2002. The overall mortality rate associated with COPD increased by 67% from 1980 to approximately 119 000 deaths in 2000 (Mannino et al 2002). Another important source of information on US mortality trends, the National Institutes of Health National Heart, Lung and Blood Institute (NHLBI) Morbidity and Mortality Chart Book on Cardiovascular, Lung and Blood Diseases, 2004 edition ranked COPD as the fourth leading cause of death in the USA for both men and women, including 125 500 deaths in 2002 for both genders (NHLBI 2004).
Figure 1.
Change in age-adjusted death rates for COPD and other leading causes of death in the USA from 1965 to1998. Reprinted from Pauwels RA, Rabe KF. 2004. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet, 364:613–20. Copyright © 2004 with permission from Elsevier.
European data
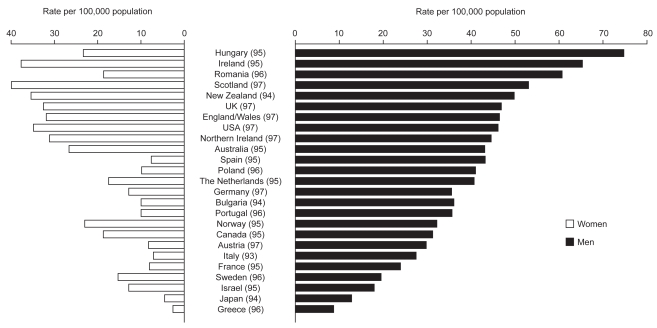
The European Lung White Book, a collaborative project published by the ERS and the European Lung Foundation, is the first comprehensive survey on respiratory health in Europe. Estimates based on 2004 WHO data indicate approximately 260 000 deaths due to COPD in 2002 (WHO 2004). This represents 2.7% of deaths from all causes, 3.3% of all deaths in European men, and 2.1% of all deaths in European women. WHO World Health Statistics Annual age-adjusted mortality data for men and women aged 35–74 years in 25 industrialized countries are shown in Figure 2 (Hurd 2000).
Figure 2.
Age-adjusted COPD mortality rates in individuals aged 35–74 years in selected European countries (non-European country data are provided for comparison). Reprinted from Hurd SS. 2000. International efforts directed at attacking the problem of COPD. Chest, 117:S336–8. Copyright © 2000 with permission from CHEST.
Encouraging data indicating a fall in overall COPD-related mortality have emerged from the UK and Lithuania. Since 1995, the COPD mortality rates in the UK and other countries, including the USA and Canada, have converged. A recent analysis using a Bayesian age-period-cohort method to project COPD mortality for the period 2000–2009 in England and Wales predicts a median fall in mortality rates of 24% for males (90% credible intervals −52% to +14%) by 2009 on a 1999 baseline (Lopez et al 2006). However, the same analysis projects a 2% rise in COPD mortality in females over this period (90% credible intervals −40% to +65%), perhaps reflecting the trend towards increased cigarette smoking in this group.
In Lithuania, mortality rates over the period 1989–1998 decreased by 5.7% (p=0.002) in men aged 35–64 years and by 2.9% for men in the ≥ 65-year age group (p=0.001). For women, the decrease in mortality over this period was 7.2% (p=0.006) in the 35–64 years age group and 2.5% (p=0.03) among those aged ≥ 65 years, respectively (Lesauskaite 2003). In a period when worldwide COPD mortality is increasing, these data indicating a decline in the rate of COPD mortality in Lithuania are noteworthy. Decreased prevalence of smoking, modernization of industry leading to reduced pollution in the workplace, and changes in treatment, including the use of long-term oxygen therapy (LTOT) and inhaled medications, may account for the decrease in COPD mortality in Lithuania.
Data from developing countries
Data on COPD mortality rates in WHO regions outside the USA and Europe are less abundant and, where data collection and record keeping are inadequate, may be less reliable. However, COPD is clearly a major health concern in developing countries and smoking-related mortality in general is expected to represent a particular problem in China, India, and the Middle East in future years, contrasting with predicted declines in developed countries. Using vital registration data provided by 112 member states, the WHO estimated that COPD accounted for 5.2% of all deaths in developing countries in 2000 (sixth leading cause of death), compared with 3.2% in developed countries (fifth leading cause of death).
COPD mortality rates in Asian countries are similar to, or in some cases markedly higher than, those in Western Europe and the USA. The WHO World Health Report for 2002 estimated a COPD mortality rate of 40.0/100 000 population for the Southeast Asia region and 79.8/100 000 population for the Western Pacific region, which includes China (Tan 2002; WHO 2002). The estimated COPD mortality rate for the Americas region (including the USA and Canada) was 26.8/100 000 population and for Africa it was 18.1/100 000 population. Although mortality data from Latin America and Africa are scant, epidemiological changes, increases in smoking, infectious diseases, and pollution are expected to lead to increased COPD mortality in these regions. Recently published data from the Latin American Project for the Investigation of Obstructive Lung Disease (PLATINO) prevalence study may support this notion (Menezes et al 2005). Although this study did not measure mortality, the relatively high prevalence rates (8%–20%) are likely to indicate a considerable burden of COPD mortality in this region. These rates are likely to be under-reported due to under-diagnoses of the disease.
Gender differences in COPD mortality
Evidence suggests there may be a relationship between gender and COPD mortality rates. For example, global mortality data from the WHO World Health Report (WHO 2002) show that COPD mortality rates were higher in men for almost all regions. The only exception was in the Western Pacific region, where mortality in women was estimated at 90/100 000 population compared with 70/100 000 population in men.
A notable trend in the US COPD mortality data is increased mortality in women in general (with the total number of women dying from COPD now exceeding that for men) and for white women in particular. A report by the US Centers for Disease Control (CDC) noted that, despite all-cause death rates decreasing by 32% for men and 14% for women from 1968 to 1999, the COPD mortality rate over this period increased by 382% for women to 41/100 000 population and by 27% for men to 44/100 000 population (Kazerouni et al 2004). The ALA report stated that 51% of deaths due to COPD in 2002 were in women; this was the third consecutive year in which deaths in women exceeded those in men (ALA 2004). A similar trend has also been observed in Canadian (Weir 2004), Spanish (Sunyer et al 1998), and Australian women (Crockett et al 1994). This rise in COPD mortality in women may reflect increased smoking prevalence amongst other factors (Kazerouni et al 2004).
In all European countries, mortality rates due to COPD are considerably higher in men than in women, with considerable differences in mortality trends from 1980 to 1990. While there was an increase in COPD mortality among women in northern European countries, including Denmark and the UK, decreased mortality rates have been reported for women from Central and Eastern European countries, including Bulgaria, Hungary, and Romania.
Societal burden of COPD morbidity and mortality
The most recent data from the GBD study indicate that worldwide in 2000, COPD resulted in 16.5 million years of life lost, almost 10 million years lived with disability, and 26.5 million disability-adjusted life years (Lopez et al 2006).
With regard to financial costs, the US NHLBI Chart Book estimated a total cost of COPD of US$37.2 billion in the USA in 2004, of which direct medical costs accounted for US$20.9 billion (NHLBI 2004). Of the indirect costs, US$7.4 billion was attributed to morbidity and US$8.9 billion to mortality. This analysis did not take into account costs for COPD as a secondary cause of morbidity or mortality.
The European Lung White Book 2003, estimated the total annual cost of COPD in Europe at €38.7 billion (US$51.2 billion) with a cost for ambulatory care of €4.7 billion, a cost for drugs of €2.7 billion, a cost for in-patient care of €2.9 billion (~US$5.6, 3.2, and 3.5 billion respectively, based on 2005 conversion rates), and a total of 28.5 million work days lost due to COPD. As these data exclude mortality costs, the actual cost incurred by COPD may be much higher.
In general, healthcare economics of COPD are characterized by an unwillingness to attribute the cost of a life lost. Available data suggest that COPD presents a large and under-estimated mortality-related cost to healthcare systems and to society.
Impact of therapeutic interventions on COPD mortality
Clearly, the burden of COPD can be reduced by preventing at-risk individuals from developing the disease. This can be achieved by screening for COPD in susceptible people and involves taking detailed patient history to assess risk factor exposure (eg, tobacco smoke), medical and family history, and presence of genetic risk factors or comorbid conditions. Early identification and prevention of COPD progression, eg, by reducing exposure to tobacco smoke, occupational substances, and air pollution, would impact positively the burden of COPD mortality.
Once established, a variety of effective treatments exists for COPD. Several studies report the impact of management and therapies on COPD, although survival is rarely the primary endpoint of such studies. Data for the impact of therapy on COPD survival are reviewed below, considering both non-pharmacological and pharmacological options.
Non-pharmacological interventions
Smoking cessation
Smoking cessation is the single most effective way to reduce the risk of developing COPD (Sin and Tu 2000a) and the only intervention proven to slow the accelerated decline in lung function related to the condition (Anthonisen et al 1994; Decramer et al 2005). However, there are few data on the effect of smoking cessation on COPD mortality among people with COPD. Follow-up of the Lung Health Study cohort of almost 6000 smokers with asymptomatic airway obstruction showed that a 10-week smoking cessation intervention program significantly reduced all-cause mortality compared with usual care, with a 14-year follow-up (Anthonisen et al 2005). The overall mortality rate in the smoking cessation intervention group (n=3923) was 8.83/1000 person-years, compared with 10.38/1000 person-years in the usual care group (n=1 964; p=0.03). Although smoking cessation reduced the incidence of most causes of death, only the reduction in respiratory deaths was statistically significant (Anthonisen et al 2005). The mortality rate for respiratory deaths unrelated to lung cancer was 0.56/1000 person-years in the smoking intervention group and 1.08/1000 person-years in the usual care group (p=0.01). Interestingly, there were salutary respiratory benefits with quitting smoking at any time during the 5-year intervention (Scanlon et al 2000; Anthonisen et al 2005); these effects were maintained during the 11-year follow-up of these data and even observed in intermittent quitters. Certainly, in the general population smoking cessation provides a survival benefit, but that topic is beyond the scope of this paper.
Oxygen therapy and non-invasive positive pressure ventilation (NPPV)
Two landmark studies conducted during the 1980s including a total of 290 patients with COPD and a resting mean PaO2 <60 mmHg demonstrated a 40% improvement in survival in patients given supplemental oxygen (relative risk [RR] for mortality = 0.61; 95% confidence interval [CI]: 0.46, 0.82) (MRCWP 1981; NOTTG 1980). In the first of these studies a significant (p=0.01) improvement in survival was observed for patients who received continuous oxygen therapy (mean 24-month mortality rate 22.4%) compared with those who received nocturnal oxygen therapy only (mean 24-month mortality rate 40.8%) (NOTTG 1980).
The survival advantage for oxygen therapy is most pronounced in patients with more severe disease and a greater degree of hypoxemia. In two further trials including a total of 211 patients with resting mean PaO2 ≥ 60 mmHg, therapy with supplemental oxygen did not significantly affect survival (RR=1.16; 95% CI: 0.85, 1.58) (Górecka et al 1997; Chaouat et al 1999).
A Cochrane systematic review and meta-analysis of NPPV for respiratory failure following COPD exacerbation showed that NPPV, as an adjunct to usual care, was associated with reduced mortality (RR=0.41; 95% CI: 0.26, 0.64) compared with usual care alone (Lightowler et al 2003). A number of other studies have reported (Confalonieri et al 1999; Bardi et al 2000) or suggested (Jones et al 1998) survival benefits for the use of NPPV in COPD patients. The mechanisms responsible for the increased survival benefit for oxygen therapy are unclear, but are thought to include improvement in pulmonary hemodynamics (Bergofsky 1983; Kawakami et al 1983; Petty and Bliss 2000) and partial reversal of autonomic nervous system dysfunction (Scalvini et al 1999).
Lung transplantation and lung volume reduction surgery (LVRS)
While lung transplantation may improve the functional status and exercise tolerance of patients with COPD, there is no evidence of a survival benefit. A study of patients listed for lung transplantation in the USA between 1992 and 1994 found no significant difference in 2-year survival between patients who received transplants and those who remained on a waiting list (Hosenpud et al 1998).
LVRS has been shown to prolong survival in a very select group of patients with severe COPD. A study of patients with severe emphysema (mean post-bronchodilator FEV1 27% predicted) who were randomized to undergo LVRS (n=608) or to receive continued medical treatment (n=610) showed that the overall mortality rate was 0.11 per person-year in both groups (RR for death in the surgery group 1.01, p=0.90) (Fishman et al 2003). However, among patients with predominantly upper lobe emphysema and low exercise capacity, mortality was lower in the surgery group (0.07 deaths per person-year) than in patients treated medically (0.15 deaths per person-year; RR for death 0.47, p=0.005). Conversely, for patients with non-upper lobe emphysema and high exercise capacity mortality was higher in the surgery group (0.10 deaths per person-year) than in medically treated patients (0.05 deaths per person-year; RR=2.06, p=0.02).
Pulmonary rehabilitation
Pulmonary rehabilitation programs appear to improve the health status and increase the exercise tolerance of patients with moderate-to-severe COPD, but there is little good evidence of a beneficial impact on mortality. Meta-analysis of data from eight studies investigating the use of pulmonary rehabilitation programs lasting from 8 weeks to 12 months for patients with COPD indicated no significant impact on mortality (RR=0.90; 95% CI: 0.65, 1.24) (Sin et al 2003).
Other potential interventions
Malnutrition, weight loss, and reduced skeletal muscle mass are all associated with a higher mortality rate in COPD patients (Wilson et al 1989; Schols et al 1998; Marquis et al 2002). Only recently has the management of weight loss and muscle wasting formed part of the COPD treatment strategy. The role of nutritional supplementation in COPD is questionable as meta-analysis of all available data shows that this intervention has no significant affect on anthropometric variables, lung function, or exercise capacity (Ferreira et al 2005). Based on these findings it seems unlikely that nutritional supplementation can reduce COPD mortality, although this has not been directly assessed. However, a combination of nutritional support and exercise can result in functional improvements, and patients responding to this approach have shown decreased mortality (Schols et al 1998). Unfortunately, these data are limited and more research into this area is clearly required (Schols 2003).
In addition, reduction in fine particulate air pollution has been linked to reduced mortality; this trend was observed specifically for deaths due to cardiovascular and respiratory causes, but not lung cancer (Laden et al 2006). Therefore, lifestyle adjustments to minimize exposure to air pollutants may also positively impact COPD mortality.
Pharmacological interventions
A wide range of pharmacological therapies have been used to treat patients with COPD. These include short-acting bronchodilators (including β2-agonists [SABA] and anticholinergics), long-acting bronchodilators (including β2-agonists [LABA], and muscarinic antagonists [LAMA] such as tiotropium), inhaled corticosteroids (ICS), oral steroids, oral theophyllines, antibiotics, and influenza and pneumococcal vaccines.
Short-acting bronchodilators
Short-acting bronchodilators, including SABA and short-acting anticholinergics, are commonly used to manage symptoms and improve exercise tolerance in patients with COPD, but there is no evidence of any effect of treatment on survival. Analysis of mortality data (149 deaths) from the 5-year Lung Health Study (Buist 1997) showed no significant differences between treatment groups for all-cause mortality, including patients treated with ipratropium (Anthonisen et al 2002).
Studies comparing short-acting combinations (ipratropium plus albuterol or metaproterenol) with SABA or anticholinergic monotherapies have not shown any benefit in terms of reduced mortality (Tashkin et al 1986; COMBIVENT Inhalation Aerosol Study Group 1994; COMBIVENT Inhalation Solution Study Group 1997).
Long-acting bronchodilators
A meta-analysis (Sin et al 2003) of nine randomized, placebo-controlled trials of LABA treatment, involving 4198 patients with moderate-to-severe COPD and study duration lasting from 12 to 52 weeks, did not show any significant improvement in all-cause mortality with active treatment (RR=0.76; 95% CI: 0.39, 1.48). However, individual trials carried out to date are too short and under-powered to evaluate the effects of long-acting bronchodilators on all-cause mortality.
Inhaled corticosteroids
Data from large, randomized, controlled trials, prospectively designed to assess the impact of ICS on mortality, are currently unavailable. However, a pooled analysis of data from randomized, placebo-controlled trials from the 1990s comparing ICS with placebo (with primary endpoints other than mortality) indicated a strong trend in favor of ICS improving mortality versus placebo (RR for mortality = 0.78; 95% CI: 0.58, 1.05), although statistical significance was not reached (Table 3) (Sin et al 2003). A separate meta-analysis (Alsaeedi et al 2002) reviewed data from five randomized, placebo-controlled trials of ICS in patients with COPD that included all-cause mortality data. Once again a non-significant trend towards improved survival in favor of ICS over placebo was observed (RR for mortality = 0.84; 95% CI: 0.60, 1.18). When two additional trials that compared combined therapy with ICS plus a LABA with placebo were included in an additional sensitivity analysis (Mahler et al 2002; Szafranski et al 2003), a stronger trend was observed (RR for mortality = 0.75; 95% CI: 0.57, 1.00), but again statistical significance was not achieved. The pooled data for these two studies alone showed a RR for mortality of 0.52 (95% CI: 0.20, 1.34) for active treatment with ICS plus salmeterol versus placebo.
Table 3.
Summary of data from randomized placebo-controlled clinical trials investigating the effect of pharmacotherapy on mortality in COPD patients
| Source of data | Comparison | RRa (95% CI) of mortality | Statistical significance |
|---|---|---|---|
| Clinical trials for ICS | |||
| (Burge et al 2000) | FP vs placebo | 0.77 (0.54, 1.11) | NS |
| (Van Der Valk et al 2002) | FP vs placebo | 0.98 (0.06, 15.55) | NS |
| (Lung Health Study Research Group 2000) | Triamcinolone vs placebo | 0.79 (0.40, 1.53) | NS |
| (Vestbo et al 1999) | Budesonide vs placebo | 0.80 (0.22, 2.92) | NS |
| (Pauwels et al 1999) | Budesonide vs placebo | 0.81 (0.22, 2.04) | NS |
| Pooled summary (n=3678) (Sin et al 2003) | ICS vs placebo | 0.78 (0.58, 1.05) | NS |
| Pooled summary (n=5085)(Sin et al 2005) | ICS vs placebo | 0.73 (0.55, 0.96) | Significant |
| Clinical trials for LABA + ICS | |||
| (Szafranski et al 2003) | Budesonide+formoterol vs placebo | 0.66 (0.24, 1.81) | NS |
| (Mahler et al 2002) | FP+salmeterol vs placebo | 0.16 (0.01, 3.01) | NS |
| Pooled summary (n=1486) (Sin et al 2003) | ICS+LABA vs placebo | 0.52 (0.20, 1.34) | NS |
Hazard ratio.
Abbreviations: CI, confidence interval; FP, fluticasone propionate; ICS, inhaled corticosteroids; LABA, long-acting β2-agonists; NS, not significant; RR, relative risk.
It is notable that none of the studies included in these meta-analyses were designed with improvement in COPD survival as their primary aim. The Inhaled Steroids in Obstructive Lung Disease in Europe (ISOLDE) trial did identify a trend towards improved survival among COPD patients treated with fluticasone proprionate (FP) (Waterhouse et al 1999). First analysis of data from the trial, in which 751 patients with moderate-to-severe COPD were randomized to 3 years’ treatment with FP or placebo, indicated no survival advantage for the steroid. However, when the data were re-analyzed using an intent-to-treat approach (identifying deaths in patients who dropped out of the study and conducting a more thorough search of deaths via the UK Office of National Statistics), there was a non-significant (p=0.069) trend for patients treated with FP to survive longer than those who received placebo.
The most recent analysis of the effect of ICS treatment on COPD mortality has been provided by the Inhaled Steroid Effects Evaluation in COPD (ISEEC) study, with a pooled analysis of individual patient-level data from seven randomized controlled trials of at least 12 months’ duration in COPD patients with stable disease (5085 patients in total) (Sin et al 2005). ICS treatment significantly reduced all-cause mortality by 27% compared with placebo (hazard ratio [HR]=0.73; 95% CI: 0.55, 0.96). This beneficial effect was most pronounced in women (HR=0.46; 95% CI: 0.24, 0.91), former smokers (HR=0.60; 95% CI: 0.39, 0.93), and patients with a baseline post-bronchodilator FEV1 <60% of predicted (HR=0.67; 95% CI: 0.48, 0.94). The use of individual patient-level data differentiates this analysis from previous meta-analyses that have not identified a significant survival benefit for ICS in COPD.
Non-randomized, observational cohort studies for ICS
A number of non-randomized, observational, population-based, cohort studies have evaluated the impact of ICS on COPD mortality (Table 4). In a population-based cohort study of data from Canadian databases on 22 620 elderly patients with COPD, patients who received ICS therapy within 90 days of hospital discharge were 29% (95% CI: 22%, 35%) less likely to die during a one-year follow-up than those who did not receive ICS (Sin and Tu 2001). Another Canadian cohort study used hospital discharge data to identify 6740 patients aged ≥ 65 years who had been hospitalized for COPD (Sin and Man 2003b). Analysis of all-cause mortality data for this cohort showed a 25% decrease in mortality in patients treated with an ICS following discharge from hospital.
Table 4.
Effect of ICS therapy on COPD mortality in non-randomized cohort studies
| Source of data | Comparison | Risk of death (95% CI) | Summary of outcome |
|---|---|---|---|
| (Sin and Tu 2001) | ICS vs no ICS | 0.71 (0.65, 0.78) | Significant survival benefit with ICS |
| (Soriano et al 2002) | FP + salmeterol vs no ICS or LABA | 0.48 (0.31, 0.73) | Significant survival benefit with FP and salmeterol |
| FP alone vs no ICS or LABA | 0.62 (0.45, 0.85) | Significant survival benefit with FP alone | |
| Salmeterol alone vs no ICS or LABA | 0.79 (0.58, 1.07) | Significant survival benefit with salmeterol alone | |
| (Soriano et al 2003)b | ICS + LABA | 10.5% | Reduction in risk of rehospitalization or death with ICS and/or LABA |
| ICS alone | 17.1% | ||
| LABA alone | 17.3% | ||
| SABA alone | 24.3% | ||
| (Sin and Man 2003a) | ICS vs no ICS | 0.75 (0.68, 0.82) | Significant survival benefit with ICS overall, and especially for medium- to high-dose ICS |
| Low-dosea ICS vs no ICS | 0.77 (0.69, 0.86) | ||
| Medium-dosea ICS vs no ICS | 0.48 (0.37, 0.63) | ||
| High-dosea ICS vs no ICS | 0.55 (0.44, 0.69) | ||
| (Suissa 2003) | ICS vs no ICS | 0.69 (0.55, 0.86) | No reduction in morbidity or mortality with ICS (after controlling for time dependence) |
| Time fixed adjusted rate | |||
| ICS vs no ICS | 1.00 (0.79, 1.26) | ||
| Time dependent rate | |||
| (Suissa 2004) | ICS vs bronchodilators | 0.66 (0.57, 0.76) | No reduction in all-cause mortality with ICS |
| (Fan et al 2003) | Low-dose ICS vs no ICS | 0.75 (0.53, 1.05) | No reduction in mortality or exacerbations with ICS |
| Medium-/high-dose ICS vs no ICS | 0.91 (0.73, 1.13) | ||
| (Kiri et al 2005b) | ICS vs no ICS | 0.69 (0.052, 0.93) | Survival benefit with ICS (in both models) |
| propensity scores | |||
| ICS vs no ICS | 0.71 (0.56, 0.90) | ||
| nested case control |
Dose was converted to beclomethasone equivalents and classified as low (≤ 500 μg/day), medium (501–1000 μg/day), and high (>1000 μg/day).
This study reported one-year mortality rates.
Abbreviations: CI, confidence interval; FP, fluticasone propionate; ICS, inhaled corticosteroids; LABA, long-acting β2-agonists; NS, not significant.
Three other large pharmaco-epidemiological studies have analyzed data from the UK General Practice Research Database (GPRD) (Soriano et al 2002, 2003; Kiri et al 2005a). In the first of these studies (Soriano et al 2002), newly diagnosed patients aged ≥ 50 years were identified in primary care between 1990 and 1999. Three-year survival was significantly higher in 1045 patients who received FP and/or salmeterol (78.6%) compared with 3620 patients who received no ICS or LABA (63.6%; p<0.05). After adjusting for confounding factors, the risk of death (compared with patients who received neither ICS nor LABA) was lowest in the patients who received concomitant therapy, followed by patients who received FP alone and those who received salmeterol alone. In the second GPRD study (Soriano et al 2003), survival data were evaluated for 3636 patients who received an ICS and/or a LABA within one year of their first hospitalization and compared with a reference group of 627 patients who were prescribed short-acting bronchodilators only. One-year mortality rates were 24.3% (reference group), 17.3% (LABA only), 17.1% (ICS only), and 10.5% (ICS plus LABA). Multivariate analysis indicated that, versus no treatment, the risk of re-hospitalization or death was reduced by 16% in patients who received ICS alone (p<0.05) and by 41% in patients who received both ICS and LABA (p<0.05). In the third GPRD study (Kiri et al 2005a), survival rates were evaluated in 437 pairs of patients (matched on disease severity) who either received ICS plus LABA or ICS plus SABA within one year of their first hospitalization. Significantly fewer patients prescribed ICS with LABA experienced re-hospitalization or death within 12 months compared with those given ICS with SABA (12.1 vs 18.1%; p<0.05). In multivariate analyses, use of ICS plus LABA was associated with 40% fewer deaths than use of ICS plus SABA (RR=0.60, 95% CI: 0.37, 0.98). As ICS are generally prescribed to patients with more advanced disease, a higher risk of mortality in these patients might be expected. However, these studies demonstrated a reduction in risk with ICS, given alone or in combination with a LABA, despite the expectation of poorer prognosis.
Although such studies are valuable to show associations between therapeutic interventions and particular outcomes in real-life settings and, as such, have provided tantalizing evidence that ICS may have a beneficial effect on mortality in COPD, not every observational study agrees with this contention (Fan et al 2003; Suissa 2003, 2004). Suissa, Fan and colleagues have criticized these studies as having been designed with bias (known as “immortal time bias”) which could lead to an overestimation of an effect of ICS. Immortal time bias arises when subjects cannot by definition incur the outcome event under the study (ie, death). For example, if a study design stipulates that a new treatment (eg, ICS) is added to a patient’s care at some time after an initial index date (ie death) then anyone dying before initiation of ICS would be allocated to a control group rather than the intervention group. This bias might lead to an overestimation of the effect of an ICS.
Recently, Kiri and co-workers explored the extent to which immortal time bias is responsible for the beneficial effects of ICS in patient’s with COPD (Kiri et al 2005b). Two designs free of any immortal time bias were used on the GPRD COPD patient data. Design one used only patients whose treatment status was defined on the same day of discharge to obtain a matched cohort based on propensity scores. Design two used all patients who had died or been re-hospitalized and matched each case with up to four non-cases by randomly sampling from the cohort risk sets, irrespective of treatment status. From the propensity scores matched-cohort analysis, treatment with ICS resulted in a HR estimate of 0.69 (95% CI: 0.52, 0.93). The matched nested case-control analysis gave rate ratio estimates of 0.71 (95% CI: 0.56, 0.90). The authors concluded that a beneficial association between ICS and the risk of death/re-hospitalization in patients with COPD does indeed exist and is free from immortal time bias.
Oral steroids
Some studies have indicated that oral corticosteroids may have a negative impact on mortality in COPD patients. In a retrospective cohort study of 556 patients receiving oral steroids for COPD, maintenance treatment with oral steroids (administered without ICS) was associated with an increased risk of mortality (RR=2.34; 95% CI: 1.24, 4.44 for a prednisone equivalent dose of 10 mg per day) (Schols et al 2001). This risk appeared to be dose-dependent and was almost doubled in patients who received a prednisone equivalent dose of 15 mg per day (RR=4.03, 95% CI: 1.99, 8.15). However, the risk of mortality appeared to be smaller when oral steroids were administered with ICS and the use of ICS alone was associated with decreased mortality (RR=0.55, 95% CI: 0.43, 0.70). A retrospective study of 403 Swedish COPD patients receiving LTOT found that increased mortality was associated with the use of oral steroids in women (RR=1.49; 95% CI: 1.00, 2.22), but not in men (RR=1.08; 95% CI: 0.74, 1.59) (Ström 1998). ICS therapy did not affect mortality in this study (RR=0.88; 95% CI: 0.62, 1.23).
Other treatments
There are at present insufficient data from clinical trials evaluating the effects of treatment with oral theophylline, antibiotics, or vaccines on COPD mortality.
A retrospective cohort study of more than 26000 Canadian patients who were hospitalized for COPD showed that outpatient use of antibiotics within 30 days before the index hospitalization was associated with a significant reduction in mortality in the 30 days following hospital entry (odds ratio = 0.83; 95% CI: 0.75, 0.92) (Sin and Tu 2000b). The early use of antibiotics might therefore be considered in COPD patients who experience an acute exacerbation.
Although there are no data on the impact of influenza and pneumococcal vaccines on mortality in COPD patients, they have been shown to reduce mortality by 30%–40% in the elderly (Nichol et al 2003). As many COPD patients are elderly and at increased risk of influenza and pneumonia, vaccination may be useful in this population.
Ongoing studies
A large, prospective, randomized placebo-controlled trial is clearly required to specifically evaluate the impact of ICS and LABAs, as monotherapy or in combination, on mortality in COPD patients and end current uncertainty on this topic. It is hoped that the ongoing landmark TORCH (Towards a Revolution in COPD Health) survival study will achieve this. This international, multicenter, randomized, double-blind, placebo-controlled, parallel-group study includes more than 6000 patients with moderate-to-severe COPD from 45 countries (Vestbo and The Torch Study Group 2004). Patients were randomized to receive three years of treatment with FP and salmeterol, FP alone, salmeterol alone, or placebo. The primary endpoint is the difference in all-cause mortality between combination FP and salmeterol therapy and placebo. The first patient was recruited in September 2000 and results are expected in 2006. The ongoing UPLIFT (Understanding the Potential Long-term Impacts on Function with Tiotropium) study (Decramer et al 2004) will also report on mortality (respiratory and all-cause), but this study is not designed or powered to specifically investigate this endpoint. Results from this trial are expected in 2008.
Conclusions
COPD represents an important and growing healthcare concern as a leading cause of death and disability worldwide. It is likely that the impact of COPD has been under-estimated due to a lack of accurate epidemiologic data from some countries, misdiagnosis, and inconsistent use of ICD codes when reporting causes of death in patients with COPD. Particularly worrying is the marked increase in deaths (in most, but not all countries) due to COPD over the past couple of decades, a trend that is predicted to continue. Also cause for concern is the dramatic rise in COPD mortality seen in women in many countries. In addition to the considerable mortality and morbidity burden of COPD, this condition also incurs significant financial costs associated with the care of patients and lost productivity of patients and carers. Improved treatment of COPD, and the ability of a therapeutic intervention to improve survival, therefore represents an important goal.
Currently, smoking cessation is the single most effective intervention to improve outcomes in patients with COPD; however, even in the best programs less than one-third of patients sustain abstinence, and dyspnea and other symptoms may persist. Supplemental oxygen and LVRS have also been shown to improve survival in selected patients. With regard to pharmacotherapy, a growing body of evidence indicates that there may be a survival benefit for treatment with ICS or long-acting bronchodilators. However, conclusive data are currently lacking so the results of ongoing studies are awaited with interest.
Acknowledgments
The authors would like to thank Marshall Naden and Karen Runcie of Gardiner-Caldwell Communications for medical writing assistance in drafting this manuscript; this assistance was funded by GlaxoSmithKline.
Abbreviations
- AIDS
acquired immunodeficiency syndrome
- ALA
American Lung Association
- ATS
American Thoracic Society
- CDC
Centers for Disease Control
- CI
confidence interval
- COPD
chronic obstructive pulmonary disease
- ERS
European Respiratory Society
- FEV1
forced expiratory volume in one second
- FP
fluticasone propionate
- FVC
forced vital capacity
- GBD
Global Burden of Disease
- GOLD
Global Initiative for Obstructive Lung Disease
- GPRD
General Practice Research Database
- HIV
human immunodeficiency virus
- HR
hazard ratio
- ICD
International Classification of Disease
- ICS
inhaled corticosteroids
- ISEEC
Inhaled Steroid Effects Evaluation in COPD
- ISOLDE
Inhaled Steroids in Obstructive Lung Disease in Europe
- LABA
long-acting β2-agonists
- LAMA
long-acting muscarinic antagonists
- LTOT
long-term oxygen therapy
- LVRS
lung volume reduction surgery
- OLD
obstructive lung disease
- MMWR
Morbidity and Mortality Weekly Report
- NHLBI
National Institutes of Health National Heart, Lung and Blood Institute
- NPPV
non-invasive positive pressure ventilation
- NS
not significant
- PLATINO
Latin American Project for the Investigation of Obstructive Lung Disease
- RR
relative risk
- SABA
short-acting β2-agonists
- TORCH
TOwards a Revolution in COPD Health
- UPLIFT
Understanding the Potential Long-term Impacts on Function with Tiotropium
- WHO
World Health Organization
Footnotes
Disclosures
DMM has acted as a consultant and speaker for Pfizer, GlaxoSmithKline, Dey, Ortho Biotech, and Boeringher-Ingelheim, and received research grants from Pfizer and GlaxoSmithKline. VAK is an employee of GlaxoSmithKline.
References
- Alsaeedi A, Sin DD, McAlister FA. The effects of inhaled corticosteroids in chronic obstructive pulmonary disease: a systematic review of randomized placebo-controlled trials. Am J Med. 2002;113:59–65. doi: 10.1016/s0002-9343(02)01143-9. [DOI] [PubMed] [Google Scholar]
- [ALA] American Lung Association EaSU, Research and Scientific Affairs. Trends in chronic bronchitis and emphysema: morbidity and mortality. New York, NY: American Lung Association; 2004. [Google Scholar]
- Anthonisen NR, Connett JE, Kiley JP, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994;272:1497–505. [PubMed] [Google Scholar]
- Anthonisen NR, Connett JE, Enright PL, et al. Hospitalizations and mortality in the Lung Health Study. Am J Respir Crit Care Med. 2002;166:333–9. doi: 10.1164/rccm.2110093. [DOI] [PubMed] [Google Scholar]
- Anthonisen NR, Skeans MA, Wise RA, et al. The effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trial. Ann Intern Med. 2005;142:233–9. doi: 10.7326/0003-4819-142-4-200502150-00005. [DOI] [PubMed] [Google Scholar]
- Anto JM, Vermeire P, Vestbo J, et al. Epidemiology of chronic obstructive pulmonary disease. Eur Respir J. 2001;17:982–94. doi: 10.1183/09031936.01.17509820. [DOI] [PubMed] [Google Scholar]
- Bardi G, Pierotello R, Desideri M, et al. Nasal ventilation in COPD exacerbations: early and late results of a prospective, controlled study. Eur Respir J. 2000;15:98–104. doi: 10.1183/09031936.00.15109800. [DOI] [PubMed] [Google Scholar]
- Barreiro TJ, Perillo I. An approach to interpreting spirometry. Am Fam Physician. 2004;69:1107–14. [PubMed] [Google Scholar]
- Berger JS, Sanborn TA, Sherman W, et al. Effect of chronic obstructive pulmonary disease on survival of patients with coronary heart disease having percutaneous coronary intervention. Am J Cardiol. 2004;94:649–51. doi: 10.1016/j.amjcard.2004.05.034. [DOI] [PubMed] [Google Scholar]
- Bergofsky EH. Tissue oxygen delivery and cor pulmonale in chronic obstructive pulmonary disease. N Engl J Med. 1983;308:1092–4. doi: 10.1056/NEJM198305053081809. [DOI] [PubMed] [Google Scholar]
- Braghiroli A, Zaccaria S, Ioli F, et al. Pulmonary failure as a cause of death in COPD. Monaldi Arch Chest Dis. 1997;52:170–5. [PubMed] [Google Scholar]
- Buist AS. The US Lung Health Study. Respirology. 1997;2:303–7. doi: 10.1111/j.1440-1843.1997.tb00094.x. [DOI] [PubMed] [Google Scholar]
- Burge PS, Calverley PM, Jones PW, et al. Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ. 2000;320:1297–303. doi: 10.1136/bmj.320.7245.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celli BR, MacNee W ATS/ERS committee members. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932–46. doi: 10.1183/09031936.04.00014304. [DOI] [PubMed] [Google Scholar]
- Chaouat A, Weitzenblum E, Kessler R, et al. A randomized trial of nocturnal oxygen therapy in chronic obstructive pulmonary disease patients. Eur Respir J. 1999;14:1002–8. doi: 10.1183/09031936.99.14510029. [DOI] [PubMed] [Google Scholar]
- COMBIVENT Inhalation Aerosol Study Group. In chronic obstructive pulmonary disease, a combination of ipratropium and albuterol is more effective than either agent alone. An 85-day multicenter trial. Chest. 1994;105:1411–9. doi: 10.1378/chest.105.5.1411. [DOI] [PubMed] [Google Scholar]
- COMBIVENT Inhalation Solution Study Group. Routine nebulized ipratropium and albuterol together are better than either alone in COPD. Chest. 1997;112:1514–21. doi: 10.1378/chest.112.6.1514. [DOI] [PubMed] [Google Scholar]
- Confalonieri M, Potena A, Carbone G, et al. Acute respiratory failure in patients with severe community-acquired pneumonia. A prospective randomized evaluation of noninvasive ventilation. Am J Respir Crit Care Med. 1999;160:1585–91. doi: 10.1164/ajrccm.160.5.9903015. [DOI] [PubMed] [Google Scholar]
- Crapo RO, Morris AH. Pulmonary function testing: sources of error in measurement and interpretation. South Med J. 1989;82:875–9. [PubMed] [Google Scholar]
- Crockett AJ, Cranston JM, Moss JR, et al. Trends in chronic obstructive pulmonary disease mortality in Australia. Med J Aust. 1994;161:600–3. doi: 10.5694/j.1326-5377.1994.tb127638.x. [DOI] [PubMed] [Google Scholar]
- Curkendall SM, Jones JK, Goehring E, et al. Cardiovascular morbidity and mortality among patients with chronic obstructive pulmonary disease (COPD) [abstract] Am J Respir Crit Care Med. 2004;169:A220. [Google Scholar]
- Decramer M, Celli B, Tashkin DP, et al. Clinical trial design considerations in assessing long-term functional impacts of tiotropium in COPD: The Uplift trial. COPD. 2004;1:303–12. doi: 10.1081/copd-200026934. [DOI] [PubMed] [Google Scholar]
- Decramer M, Gosselink R, Bartsch P, et al. Effect of treatments on the progression of COPD: report of a workshop held in Leuven, 11–12 March 2004. Thorax. 2005;60:343–9. doi: 10.1136/thx.2004.028720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [ERS] European Respiratory Society and European Lung Foundation. European Lung White Book. Sheffield: European Respiratory Society; 2003. Section 3: Chronic obstructive pulmonary disease; pp. 34–43. [Google Scholar]
- Fan VS, Bryson CL, Curtis JR, et al. Inhaled corticosteroids in chronic obstructive pulmonary disease and risk of death and hospitalization: time-dependent analysis. Am J Respir Crit Care Med. 2003;168:1488–94. doi: 10.1164/rccm.200301-019OC. [DOI] [PubMed] [Google Scholar]
- Ferreira IM, Brooks D, Lacasse Y, et al. Nutritional supplementation for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;2 doi: 10.1002/14651858.CD000998.pub2. article nr CD000998. [DOI] [PubMed] [Google Scholar]
- Fishman A, Martinez F, Naunheim K, et al. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med. 2003;348:2059–73. doi: 10.1056/NEJMoa030287. [DOI] [PubMed] [Google Scholar]
- Gan WQ, Man SF, Senthilselvan A, et al. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax. 2004;59:574–80. doi: 10.1136/thx.2003.019588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOLD. [Accessed 9 November 2005];Global Initiative for Chronic Obstructive Lung Disease [online] 2005 URL: www.goldcopd.com.
- Górecka D, Gorzelak K, Sliwinski P, et al. Effect of long-term oxygen therapy on survival in patients with chronic obstructive pulmonary disease with moderate hypoxaemia. Thorax. 1997;52:674–9. doi: 10.1136/thx.52.8.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greten FR, Eckmann L, Greten TF, et al. IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell. 2004;118:285–96. doi: 10.1016/j.cell.2004.07.013. [DOI] [PubMed] [Google Scholar]
- Hansell A, Hollowell J, McNiece R, et al. Validity and interpretation of mortality, health service and survey data on COPD and asthma in England. Eur Respir J. 2003a;21:279–86. doi: 10.1183/09031936.03.00006102. [DOI] [PubMed] [Google Scholar]
- Hansell AL, Walk JA, Soriano JB. What do chronic obstructive pulmonary disease patients die from? A multiple cause coding analysis. Eur Respir J. 2003b;22:809–14. doi: 10.1183/09031936.03.00031403. [DOI] [PubMed] [Google Scholar]
- Hardie JA, Buist AS, Vollmer WM, et al. Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Eur Respir J. 2002;20:1117–22. doi: 10.1183/09031936.02.00023202. [DOI] [PubMed] [Google Scholar]
- Hogg JC, Chu F, Utokaparch S, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:2645–53. doi: 10.1056/NEJMoa032158. [DOI] [PubMed] [Google Scholar]
- Hosenpud JD, Bennett LE, Keck BM, et al. Effect of diagnosis on survival benefit of lung transplantation for end-stage lung disease. Lancet. 1998;351:24–7. doi: 10.1016/S0140-6736(97)06405-2. [DOI] [PubMed] [Google Scholar]
- Hurd SS. International efforts directed at attacking the problem of COPD. Chest. 2000;117:S336–8. doi: 10.1378/chest.117.5_suppl_2.336s. [DOI] [PubMed] [Google Scholar]
- Jenkins MA, Rubinfield ARR, Robertson CF, et al. Accuracy of asthma death statistics in Australia. Austral J Pub Health. 1992;16:427–9. doi: 10.1111/j.1753-6405.1992.tb00091.x. [DOI] [PubMed] [Google Scholar]
- Jones SE, Packham S, Hebden M, et al. Domiciliary nocturnal intermittent positive pressure ventilation in patients with respiratory failure due to severe COPD: long-term follow up and effect on survival. Thorax. 1998;53:495–8. doi: 10.1136/thx.53.6.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawakami Y, Kishi F, Yamamoto H, et al. Relation of oxygen delivery, mixed venous oxygenation, and pulmonary hemodynamics to prognosis in chronic obstructive pulmonary disease. N Engl J Med. 1983;308:1045–9. doi: 10.1056/NEJM198305053081801. [DOI] [PubMed] [Google Scholar]
- Kazerouni N, Alverson CJ, Redd SC, et al. Sex differences in COPD and lung cancer mortality trends: United States, 1968–1999. J Womens Health. 2004;13:17–23. doi: 10.1089/154099904322836410. [DOI] [PubMed] [Google Scholar]
- Keistinen T, Tuuponen T, Kivela SL. Survival experience of the population needing hospital treatment for asthma or COPD at age 50–54 years. Respir Med. 1998;92:568–72. doi: 10.1016/s0954-6111(98)90310-9. [DOI] [PubMed] [Google Scholar]
- Kiri VA, Bettoncelli G, Testi R, et al. Inhaled corticosteroids are more effective in COPD patients when used with LABA than with SABA. Respir Med. 2005a;99:1115–24. doi: 10.1016/j.rmed.2005.02.018. [DOI] [PubMed] [Google Scholar]
- Kiri VA, Pride NB, Soriano JB, et al. Inhaled corticosteroids in chronic obstructive pulmonary disease: results from two observational designs free of immortal time bias. Am J Respir Crit Care Med. 2005b;172:460–4. doi: 10.1164/rccm.200502-210OC. [DOI] [PubMed] [Google Scholar]
- Laden F, Schwartz J, Speizer FE, et al. Reduction in fine particulate air pollution and mortality: extended follow-up of the Harvard Six Cities Study. Am J Respir Crit Care Med. 2006;173:667–72. doi: 10.1164/rccm.200503-443OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesauskaite V. Age-related trends in mortality from COPD in Lithuania, 1989 to 1998. Chest. 2003;124:90–3. doi: 10.1378/chest.124.1.90. [DOI] [PubMed] [Google Scholar]
- Lightowler JV, Wedzicha JA, Elliott MW, et al. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ. 2003;326:185. doi: 10.1136/bmj.326.7382.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loddenkemper R, Gibson GJ, Sibille Y. European White Lung Book: The First Comprehensive Survey on Respiratory Health in Europe. Sheffield: European Respiratory Society; 2003. [Google Scholar]
- Lopez AD, Shibuya K, Rao C, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27:397–412. doi: 10.1183/09031936.06.00025805. [DOI] [PubMed] [Google Scholar]
- [LHSRG] Lung Health Study Research Group. Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary disease. N Engl J Med. 2000;343:1902–9. doi: 10.1056/NEJM200012283432601. [DOI] [PubMed] [Google Scholar]
- Mahler DA, Wire P, Horstman D, et al. Effectiveness of fluticasone propionate and salmeterol combination delivered via the Diskus device in the treatment of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166:1084–91. doi: 10.1164/rccm.2112055. [DOI] [PubMed] [Google Scholar]
- Mannino DM, Brown C, Giovino GA. Obstructive lung disease deaths in the United States from 1979 through 1993. An analysis using multiple-cause mortality data. Am J Respir Crit Care Med. 1997;156:814–8. doi: 10.1164/ajrccm.156.3.9702026. [DOI] [PubMed] [Google Scholar]
- Mannino DM, Gagnon RC, Petty TL, et al. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2000;160:1683–9. doi: 10.1001/archinte.160.11.1683. [DOI] [PubMed] [Google Scholar]
- Mannino DM, Homa DM, Akinbami LJ, et al. Chronic obstructive pulmonary disease surveillance: United States, 1971–2000. MMWR Surveillance Summaries. 2002;51:1–16. [PubMed] [Google Scholar]
- Mannino DM, Buist AS, Petty TL, et al. Lung function and mortality in the United States: data from the First National Health and Nutrition Examination Survey follow up study. Thorax. 2003;58:388–93. doi: 10.1136/thorax.58.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquis K, Debigare R, Lacasse Y, et al. Midthigh muscle cross-sectional area is a better predictor of mortality than body mass index in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166:809–13. doi: 10.1164/rccm.2107031. [DOI] [PubMed] [Google Scholar]
- Matsuba K, Wright JL, Wiggs BR, et al. The changes in airways structure associated with reduced forced expiratory volume in one second. Eur Respir J. 1989;2:834–9. [PubMed] [Google Scholar]
- [MRCWP] Medical Research Council Working Party. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet. 1981;1:681–6. [PubMed] [Google Scholar]
- Menezes AM, Perez-Padilla R, Jardim JB, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet. 2005;366:1875–81. doi: 10.1016/S0140-6736(05)67632-5. [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay T, Roth JA, Maxwell SA. Altered expression of the p50 subunit of the NF-kappa B transcription factor complex in non-small cell lung carcinoma. Oncogene. 1995;11:999–1003. [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997a;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997b;349:1436–42. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997c;349:1269–76. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- [NHLBI] National Institutes of Health, National Heart Lung and Blood Institute. Morbidity & mortality: 2004 chart book on cardiovascular, lung, and blood diseases. 2004:1–90. [Google Scholar]
- Nichol KL, Nordin J, Mullooly J, et al. Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med. 2003;348:1322–32. doi: 10.1056/NEJMoa025028. [DOI] [PubMed] [Google Scholar]
- [NOTTG] Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Ann Intern Med. 1980;93:391–8. doi: 10.7326/0003-4819-93-3-391. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, Revill SM, Webb KA. Dynamic hyperinflation and exercise intolerance in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164:770–7. doi: 10.1164/ajrccm.164.5.2012122. [DOI] [PubMed] [Google Scholar]
- Pauwels RA, Lofdahl CG, Laitinen LA, et al. Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. European Respiratory Society Study on Chronic Obstructive Pulmonary Disease. N Engl J Med. 1999;340:1948–53. doi: 10.1056/NEJM199906243402503. [DOI] [PubMed] [Google Scholar]
- Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD) Lancet. 2004;364:613–20. doi: 10.1016/S0140-6736(04)16855-4. [DOI] [PubMed] [Google Scholar]
- Petty TL, Bliss PL. Ambulatory oxygen therapy, exercise, and survival with advanced chronic obstructive pulmonary disease (the Nocturnal Oxygen Therapy Trial revisited) Respir Care. 2000;45:204–11. [PubMed] [Google Scholar]
- Pikarsky E, Porat RM, Stein I, et al. NF-kappaB functions as a tumour promoter in inflammation-associated cancer. Nature. 2004;431:461–6. doi: 10.1038/nature02924. [DOI] [PubMed] [Google Scholar]
- Reid DW, Hendrick VJ, Aitken TC, et al. Age-dependent inaccuracy of asthma death certification in Northern England, 1991–1992. Eur Respir J. 1998;12:1079–83. doi: 10.1183/09031936.98.12051079. [DOI] [PubMed] [Google Scholar]
- Repine JE, Bast A, Lankhorst I, et al. Oxidative stress in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997;156:341–57. doi: 10.1164/ajrccm.156.2.9611013. [DOI] [PubMed] [Google Scholar]
- Scalvini S, Porta R, Zanelli E, et al. Effects of oxygen on autonomic nervous system dysfunction in patients with chronic obstructive pulmonary disease. Eur Respir J. 1999;13:119–24. doi: 10.1183/09031936.99.13111999. [DOI] [PubMed] [Google Scholar]
- Scanlon PD, Connett JE, Waller LA, et al. Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease. The Lung Health Study. Am J Respir Crit Care Med. 2000;161:381–90. doi: 10.1164/ajrccm.161.2.9901044. [DOI] [PubMed] [Google Scholar]
- Schols AM, Slangen J, Volovics L, et al. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157:1791–7. doi: 10.1164/ajrccm.157.6.9705017. [DOI] [PubMed] [Google Scholar]
- Schols A. Nutritional modulation as part of the integrated management of chronic obstructive pulmonary disease. Proc Nutr Soc. 2003;62:783–91. doi: 10.1079/PNS2003303. [DOI] [PubMed] [Google Scholar]
- Schols AM, Wesseling G, Kester AD, et al. Dose dependent increased mortality risk in COPD patients treated with oral glucocorticoids. Eur Respir J. 2001;17:337–42. doi: 10.1183/09031936.01.17303370. [DOI] [PubMed] [Google Scholar]
- Sekine Y, Behnia M, Fujisawa T. Impact of COPD on pulmonary complications and on long-term survival of patients undergoing surgery for NSCLC. Lung Cancer. 2002;37:95–101. doi: 10.1016/s0169-5002(02)00014-4. [DOI] [PubMed] [Google Scholar]
- Sin DD, Tu JV. Lack of association between ipratropium bromide and mortality in elderly patients with chronic obstructive airway disease. Thorax. 2000a;55:194–7. doi: 10.1136/thorax.55.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin DD, Tu JV. Outpatient antibiotic therapy and short term mortality in elderly patients with chronic obstructive pulmonary disease. Can Respir J. 2000b;7:466–71. doi: 10.1155/2000/417298. [DOI] [PubMed] [Google Scholar]
- Sin DD, Tu JV. Inhaled corticosteroids and the risk of mortality and readmission in elderly patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164:580–4. doi: 10.1164/ajrccm.164.4.2009033. [DOI] [PubMed] [Google Scholar]
- Sin DD, Man SF. Inhaled corticosteroids and survival in chronic obstructive pulmonary disease: does the dose matter? Eur Respir J. 2003a;21:260–6. doi: 10.1183/09031936.03.00040803. [DOI] [PubMed] [Google Scholar]
- Sin DD, Man SF. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. 2003b;107:1514–9. doi: 10.1161/01.cir.0000056767.69054.b3. [DOI] [PubMed] [Google Scholar]
- Sin DD, McAlister FA, Man SF, et al. Contemporary management of chronic obstructive pulmonary disease: scientific review. JAMA. 2003;290:2301–12. doi: 10.1001/jama.290.17.2301. [DOI] [PubMed] [Google Scholar]
- Sin DD, Wu L, Anderson JA, et al. Inhaled corticosteroids and mortality in chronic obstructive pulmonary disease. Thorax. 2005;60:992–7. doi: 10.1136/thx.2005.045385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth ET, Wright SC, Evans AE, et al. Death from airways obstruction: accuracy of certification in Northern Ireland. Thorax. 1986;51:293–7. doi: 10.1136/thx.51.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soriano JB, Vestbo J, Pride NB, et al. Survival in COPD patients after regular use of fluticasone propionate and salmeterol in general practice. Eur Respir J. 2002;20:819–25. doi: 10.1183/09031936.02.00301302. [DOI] [PubMed] [Google Scholar]
- Soriano JB, Kiri VA, Pride NB, et al. Inhaled corticosteroids with/without long-acting beta-agonists reduce the risk of rehospitalization and death in COPD patients. Am J Respir Med. 2003;2:67–74. doi: 10.1007/BF03256640. [DOI] [PubMed] [Google Scholar]
- Ström K. Oral corticosteroid treatment during long-term oxygen therapy in chronic obstructive pulmonary disease: a risk factor for hospitalization and mortality in women. Respir Med. 1998;92:50–6. doi: 10.1016/s0954-6111(98)90032-4. [DOI] [PubMed] [Google Scholar]
- Suissa S. Effectiveness of inhaled corticosteroids in chronic obstructive pulmonary disease: immortal time bias in observational studies. Am J Respir Crit Care Med. 2003;168:49–53. doi: 10.1164/rccm.200210-1231OC. [DOI] [PubMed] [Google Scholar]
- Suissa S. Inhaled steroids and mortality in COPD: bias from unaccounted immortal time. Eur Respir J. 2004;23:391–5. doi: 10.1183/09031936.04.00062504. [DOI] [PubMed] [Google Scholar]
- Sunyer J, Anto JM, McFarlane D, et al. Sex differences in mortality of people who visited emergency rooms for asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158:851–6. doi: 10.1164/ajrccm.158.3.9801093. [DOI] [PubMed] [Google Scholar]
- Sutherland ER, Cherniack RM. Management of chronic obstructive pulmonary disease. N Engl J Med. 2004;350:2689–97. doi: 10.1056/NEJMra030415. [DOI] [PubMed] [Google Scholar]
- Szafranski W, Cukier A, Ramirez A, et al. Efficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary disease. Eur Respir J. 2003;21:74–81. doi: 10.1183/09031936.03.00031402. [DOI] [PubMed] [Google Scholar]
- Tan WC. The global initiative for chronic obstructive lung disease: Gold standards and the Asia-Pacific perspective. Respirology. 2002;7:1–2. doi: 10.1046/j.1440-1843.2002.00371.x. [DOI] [PubMed] [Google Scholar]
- Tashkin DP, Ashutosh K, Bleecker ER, et al. Comparison of the anticholinergic bronchodilator ipratropium bromide with metaproterenol in chronic obstructive pulmonary disease. A 90-day multi-center study. Am J Med. 1986;81:81–90. doi: 10.1016/0002-9343(86)90468-7. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Chronic obstructive pulmonary disease. Washington, DC: USDHHS; 2003. Data fact sheet. [Google Scholar]
- van der Valk P, Monninkhof E, van der Palen J, et al. Effect of discontinuation of inhaled corticosteroids in patients with chronic obstructive pulmonary disease: the COPE study. Am J Respir Crit Care Med. 2002;166:1358–63. doi: 10.1164/rccm.200206-512OC. [DOI] [PubMed] [Google Scholar]
- Vestbo J, Sorensen T, Lange P, et al. Long-term effect of inhaled budesonide in mild and moderate chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 1999;353:1819–23. doi: 10.1016/s0140-6736(98)10019-3. [DOI] [PubMed] [Google Scholar]
- Vestbo J The TORCH Study Group. The TORCH (TOwards a Revolution in COPD Health) survival study protocol. Eur Respir J. 2004;24:206–10. doi: 10.1183/09031936.04.00120603. [DOI] [PubMed] [Google Scholar]
- Vilkman S, Keistinen T, Tuuponen T, et al. Survival and cause of death among elderly chronic obstructive pulmonary disease patients after first admission to hospital. Respiration. 1997;64:281–4. doi: 10.1159/000196687. [DOI] [PubMed] [Google Scholar]
- Waterhouse JC, Fishwick D, Anderson JA, et al. What caused death in the inhaled steroids in obstructive lung disease in Europe (ISOLDE) study? [abstract] Eur Respir J. 1999;14(Suppl 30):387s. [Google Scholar]
- Wedzicha JA, Seemungal TA, MacCallum PK, et al. Acute exacerbations of chronic obstructive pulmonary disease are accompanied by elevations of plasma fibrinogen and serum IL-6 levels. Thromb Haemost. 2000;84:210–5. [PubMed] [Google Scholar]
- Weir E. COPD death rates: projecting a female trajectory. CMAJ. 2004;170:334. [PMC free article] [PubMed] [Google Scholar]
- Wilson DO, Rogers RM, Wright EC, et al. Body weight in chronic obstructive pulmonary disease. The National Institutes of Health Intermittent Positive-Pressure Breathing Trial. Am Rev Respir Dis. 1989;139:1435–8. doi: 10.1164/ajrccm/139.6.1435. [DOI] [PubMed] [Google Scholar]
- [WHO] World Health Organization. The World Health Report 2002: Reducing the Risks, Promoting Healthy Life. Geneva: WHO; 2002. [Google Scholar]
- [WHO] World Health Organization. The World Health Report 2004: Changing History. Geneva: WHO; 2004. [Google Scholar]
- Wright JG, Christman JW. The role of nuclear factor kappa B in the pathogenesis of pulmonary diseases: implications for therapy. Am J Respir Med. 2003;2:211–9. doi: 10.1007/BF03256650. [DOI] [PubMed] [Google Scholar]
- Zielinski J, MacNee W, Wedzicha J, et al. Causes of death in patients with COPD and chronic respiratory failure. Monaldi Arch Chest Dis. 1997;52:43–7. [PubMed] [Google Scholar]