Abstract
Background
The incidence and significance of gasping after cardiac arrest in humans are controversial.
Methods and Results
Two approaches were used. The first was a retrospective analysis of consecutive confirmed out-of-hospital cardiac arrests from the Phoenix Fire Department Regional Dispatch Center text files to determine the presence of gasping soon after collapse. The second was a retrospective analysis of 1218 patients with out-of-hospital cardiac arrests in Arizona documented by emergency medical system (EMS) first-care reports to determine the incidence of gasping after arrest in relation to the various EMS arrival times. The primary outcome measure was survival to hospital discharge. An analysis of the Phoenix Fire Department Regional Dispatch Center records of witnessed and unwitnessed out-of-hospital cardiac arrests with attempted resuscitation found that 44 of 113 (39%) of all arrested patients had gasping. An analysis of 1218 EMS-attended, witnessed, out-of-hospital cardiac arrests demonstrated that the presence or absence of gasping correlated with EMS arrival time. Gasping was present in 39 of 119 patients (33%) who arrested after EMS arrival, in 73 of 363 (20%) when EMS arrival was <7 minutes, in 50 of 360 (14%) when EMS arrival time was 7 to 9 minutes, and in 25 of 338 (7%) when EMS arrival time was >9 minutes. Survival to hospital discharge occurred in 54 of 191 patients (28%) who gasped and in 80 of 1027 (8%) who did not (adjusted odds ratio, 3.4; 95% confidence interval, 2.2 to 5.2). Among the 481 patients who received bystander cardiopulmonary resuscitation, survival to hospital discharge occurred among 30 of 77 patients who gasped (39%) versus only 38 of 404 among those who did not gasp (9%) (adjusted odds ratio, 5.1; 95% confidence interval, 2.7 to 9.4).
Conclusions
Gasping or abnormal breathing is common after cardiac arrest but decreases rapidly with time. Gasping is associated with increased survival. These results suggest that the recognition and importance of gasping should be taught to bystanders and emergency medical dispatchers so as not to dissuade them from initiating prompt resuscitation efforts when appropriate.
Keywords: breathing, cardiopulmonary resuscitation, heart arrest, resuscitation
Out-of-hospital cardiac arrest (OHCA) is a common cause of death in the United States and is therefore a major public health problem.1 It has long been known that the early initiation of bystander cardiopulmonary resuscitation (CPR) efforts, when followed by early defibrillation or advanced cardiac life support, significantly improves survival of individuals with OHCA.2 Nevertheless, the incidence of bystander-initiated CPR remains unacceptably low.3–5 Several possible deterrents to the early initiation of bystander resuscitation efforts exist. One is the bystanders’ or emergency medical dispatchers’ delay in recognizing cardiac arrest because of the presence of gasping or other forms of abnormal breathing in the early stage of the arrest.6–9
The 2005 American Heart Association Basic Life Support Guidelines state under Treatment Recommendations, “Rescuers should start CPR if the victim is unconscious (unresponsive), not moving and not breathing. Even if the victim takes occasional gasps, rescuers should suspect that cardiac arrest has occurred and should start CPR.”10 Despite written recommendations, all too often bystanders (even physicians) who were “willing and able” to do CPR delayed because the victim was gasping. The question is, how frequent is gasping in victims of OHCA? Is gasping or agonal breathing rare, as some have stated,11 or common? Our goal was to determine the incidence of gasping in victims of OHCA in Arizona and the relationship of gasping to survival.
Methods
The presence and significance of abnormal breathing or gasping in humans were determined retrospectively by 2 approaches. The first was an analysis of the Phoenix Fire Department Regional Dispatch Center (PFDRDC) text files from January 1, 2008, to February 29, 2008. These data reflect the incidence of gasping in patients as found by bystanders of both witnessed and unwitnessed OHCA. Because the PFDRDC text files did not differentiate between witnessed and unwitnessed arrest, both were included in this analysis. The PFDRDC provides fire and emergency medical dispatching services that cover >2000 sq miles within Maricopa County. The PFDRDC dispatches ≈327 000 annual calls for service. The second part of our report included a retrospective analysis of emergency medical system (EMS) first-care reports of patients with OHCA from July 2004 through December 2007 to determine the incidence of gasping on or after arrival at the scene. The arrival times were divided into 4 groups; the first was made up of those who arrested after the arrival of EMS. Patients who arrested before the arrival on EMS were divided into 3 time intervals so that approximately one third of the patients were in each arrival time period. Dispatch-to-EMS-arrival time intervals, initial rhythm, age, sex, location of the cardiac arrest, bystander CPR, and survival to hospital discharge were recorded for each arrest. The data were from fire departments that have emergency medical technician-paramedics on first-response vehicles for high-priority level 9–1–1 calls. These providers have the ability to deliver advanced cardiac life support. Prehospital providers are specifically instructed to document gasping as “any abnormal breathing pattern,” if present, during OHCA events.
A statewide Utstein-style database for OHCA, as previously reported, was used.12,13 The Arizona Bureau of Emergency Medical Services and Trauma System established the Save Hearts in Arizona Registry and Education (SHARE) program as a means to address the public health problem of OHCA. Because OHCA has been identified as a public health issue in Arizona and the goal of the SHARE program is quality improvement, the data collected are exempt from the Health Insurance Portability and Accountability Act. Permission to publish deidentified SHARE program data was obtained from the Arizona Department of Health Services Human Subjects Review Committee as well as the University of Arizona Institutional Review Board. Survival data were obtained through local hospitals and the Bureau of Public Health Statistics in the Arizona Department of Health Services.12,13
Cardiac arrest was defined as the absence of arterial pulsations and normal breathing. Patients included were adults with cardiac arrest that occurred before and after the arrival of the EMS providers. Cardiac arrest rhythms included asystole, pulseless electrical activity, and shockable rhythms of ventricular fibrillation (VF) or ventricular tachycardia. Victims with obvious signs of death (eg, rigor mortis, lividity) or with do-not-resuscitate documentation on EMS arrival were excluded because resuscitation efforts were not initiated per standard protocol. Other exclusion criteria were age <18 years and cardiac arrest secondary to trauma, drowning, or other noncardiac causes.
Statistical Analysis
The data were entered into Microsoft Access for Windows (Microsoft Office, Microsoft Corp, Redmond, Wash) and transported into SPSS 16.0 for Windows for statistical analysis (SPSS, Inc, Chicago, Ill). A logistic regression analysis was used to determine the relationship between EMS arrival times and the incidence of gasping. EMS arrival time was divided into 4 categories. Patients whose collapse occurred after EMS arrival were put in 1 category, and patients who arrested before EMS arrival were divided equally into 3 categories by EMS arrival time. The models were adjusted for age, sex, location of cardiac arrest, bystander CPR, VF, and method of professional resuscitation. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for gasping were determined. The proportion of patients who survived among those who had abnormal breathing (gaspers) was compared with those who did not gasp (nongaspers) by collapse-to–EMS-arrival times and by bystander-performed CPR through the use of χ2 analysis and by logistic regression analysis. Analyses of differences in dichotomous outcomes between groups were made with the χ2 test. Continuous variables were analyzed by Student t test or the nonparametric Wilcoxon tests. All statistical tests were 2 sided and evaluated at α=0.05. The sample size was not planned.
The authors had full access to and take full responsibility for the integrity of the data. All authors have read and agree to the manuscript as written.
Results
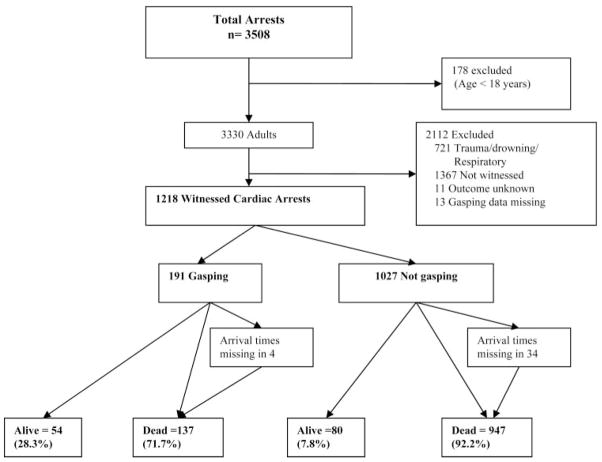
Of the 269 documents of recorded PFDRDC conversations, 116 were excluded because the patients had “unconfirmed codes,” trauma, or obvious drug overdose; had do-not-resuscitate documents; met prehospital criteria for hospice patients; or were obviously dead. Of 113 OHCAs, both witnessed and unwitnessed, analysis of dispatch text files found that 44 of 113 (39%) had abnormal breathing. First-care reports from 3508 total EMS-attended arrests were entered into the statewide Utstein-style EMS database, of which 1218 were witnessed arrests of presumed cardiac origin and entered into the analysis (the Figure). No difference was found in the median age, gender, home location of the cardiac arrest, or bystander-performed CPR among patients who gasped compared with those who did not gasp (Table 1).
Figure.
Out-of-hospital EMS-attended arrests. Shown are the presence or absence of gasping as documented by EMS personnel and the resultant survival to hospital discharge (alive).
Table 1.
Demographics of Study Participants and Event Characteristics
| Gasping |
|||
|---|---|---|---|
| Yes (n=1027) | No (n=191) | P | |
| Male, % (n) | 69.6 (133) | 71.1 (730) | 0.68 |
| Home location, % (n) | 61.8 (118) | 67.7 (695) | 0.11 |
| Bystander CPR performed, % (n) | 40.3 (77) | 39.3 (404) | 0.80 |
| VF, % (n) | 50.8 (97) | 41.9 (430) | 0.02 |
| EMS collapse to arrival time, median (IQR), min | 6.0 (5) | 8.0 (5) | <0.001 |
IQR indicates interquartile range. n=1218.
Gasping was present in 39 of 119 patients (32.8%) who arrested after EMS arrival, in 73 of 363 (20.1%) when EMS arrival was <7 minutes, in 50 of 360 (13.9%) when EMS arrival time was 7 to 9 minutes, and in 25 of 338 (7.4%) when EMS arrival time was >9 minutes (Table 2). The adjusted odds of gasping decreased as collapse-to–EMS-arrival time increased. Complete time interval data were not available for 38 of 1218 (3.1%) cases (Table 2). Gasping was significantly higher in the witnessed VF group (18.4%) compared with the witnessed non-VF group (13.6%) (adjusted OR, 1.7; 95% CI, 1.2 to 2.4; Table 2).
Table 2.
Relation of Collapse of Witnessed VF to Observation of Gasping
| Gasping (Yes) (n=191) |
||
|---|---|---|
| % (n) | OR (95% CI)* | |
| Collapse after EMS arrival (n=119) | 32.8 (39) | 2.7 (1.6–4.7)¶ |
| Collapse before EMS arrival, min (n) | ||
| <7 (363) | 20.1 (73) | 1.00 (Ref) |
| 7–9 (360) | 13.9 (50) | 0.6 (0.4–1.0) |
| >9 (338) | 7.4 (25) | 0.3 (0.2–0.5)¶ |
| Missing data (38)† | 10.5 (4) | … |
| Witnessed VF (n)‡ | ||
| No (690) | 13.6 (94) | 1.00 |
| Yes (527) | 18.4 (97) | 1.7 (1.2–2.4)§ |
The model was adjusted for age, gender, bystander CPR performed, location of cardiac arrest, and VF. Negelkerke R2=0.086; Cox and Snell R2=0.05. Model χ2 (8) =60.55; P<0.001.
Thirty-eight cases were missing either collapse time or EMS arrival time and were excluded from analysis.
One case excluded because of missing initial rhythm analysis.
P<0.01;
P<0.001.
The relationship of gasping to bystander CPR is provided in Table 3. The proportion of patients who received bystander CPR was not different between gaspers and nongaspers (Table 3). The relationship of survival to observations of gasping by bystander CPR and by collapse-to-arrival time is shown in Table 4. Fifty-four of 191 gaspers (28.3%) and 80 of 1027 nongaspers (7.8%) survived (OR, 3.4; 95% CI, 2.2 to 5.2; Table 4).
Table 3.
Relationship of Gasping to Bystander CPR by Collapse-to-Arrival Time
| Collapse-to–EMS-arrival time, min (n/N)* | Received Bystander CPR and Gasping, % (n/N) | Received Bystander CPR and Not Gasping, % (n/N) | P, χ2 |
|---|---|---|---|
| <7 (363) | 57.5 (42/73) | 50.7 (147/290) | 1.09 (0.29) |
| 7–9 (360) | 44.0 (22/50) | 46.5 (144/310) | 0.10 (0.74) |
| >9 (338) | 36.0 (9/25) | 31.9 (100/310) | 0.17 (0.67) |
Thirty-eight cases were missing either collapse time or EMS arrival time. The group of patients who collapsed after EMS arrival (n=119) was not included in the table because only 1 patient received bystander CPR.
Table 4.
Relationship of Survival to Observation of Gasping by Bystander CPR and Collapse-to-Arrival Time
| Survival |
|||
|---|---|---|---|
| Gasping (n) | % (n) | OR (95% CI) | |
| All cardiac arrest (n=1218) | |||
| No (1027) | 7.8 (80) | 1.00 | |
| Yes (191) | 28.3 (54) | 3.4 (2.2–5.2)† | |
| Bystander CPR performed (n) | |||
| Yes (481) | No (404) | 9.4 (38) | 1.00 |
| Yes (77) | 39.0 (30) | 5.1 (2.7–9.4)† | |
| No (737) | No (623) | 6.7 (42) | 1.00 |
| Yes (114) | 21.1 (24) | 2.4 (1.2–4.3)* | |
| Collapse-to-arrival time, min (n) | |||
| <7 (363) | No (290) | 12.8 (37) | 1.00 |
| Yes (73) | 46.6 (34) | 6.0 (3.2–11.1)† | |
| 7–9 (360) | No (310) | 5.8 (18) | 1.00 |
| Yes (50) | 18.0 (9) | 3.8 (1.5–9.9)* | |
| >9 (338) | No (313) | 2.9 (9) | 1.00 |
| Yes (25) | 16.0 (4) | 5.7 (1.4–22.0)* | |
| Collapse after EMS arrival (n=119) | |||
| No (80) | 20.0 (16) | 1.00 | |
| Yes (39) | 17.9 (7) | 1.02 (0.3–2.9) | |
Model is adjusted for age, gender, location of cardiac arrest, bystander CPR performed, collapse-to–EMS-arrival time, VF, and method of professional resuscitation (CPR vs CCR).
P<0.01;
P<0.001.
Bystander CPR was provided for 77 of 191 gaspers (40%) and for 404 of 1027 nongaspers (39%; P>0.05). Among the 481 patients who received bystander CPR, 30 of 77 patients who gasped (39%) survived, whereas only 38 of 404 nongaspers (9.4%) survived (OR, 5.1; 95% CI, 2.7 to 9.4; Table 4). Similar results were found among the 737 patients who did not receive bystander CPR; gaspers had a higher survival (21.1%) compared with nongaspers (6.7%) (adjusted OR, 2.4; 95% CI, 1.2 to 4.3; Table 4).
Discussion
These data confirm that gasping is common after an OHCA of presumed cardiac origin in adults and is associated with increased survival to hospital discharge. In addition, this study establishes that gasping is most frequent soon after the collapse and decreases with time. The importance and incidence of gasping with cardiac arrest (often referred to as snoring, snorting, gurgling, or moaning or as agonal, barely, labored, noisy, or heavy breathing)14,15 after cardiac arrest are not generally appreciated. This may be unfortunate because this knowledge gap may delay the recognition of cardiac arrest and thus delay the prompt recognition of cardiac arrest. It is not uncommon to hear anecdotal reports that bystanders (even medical professionals) failed to initiate CPR because they concluded that the patient was still breathing and therefore did not have a cardiac arrest.
Abnormal breathing is a common and important phenomenon in cardiac arrest and resuscitation.14,15 Gasping indicates markedly decreased but marginally adequate cerebral perfusion. This conclusion is based on observations after cardiac arrest in studies that showed that if gasping is present when advanced cardiac life support is provided, survival is markedly improved.14 The overall survival to hospital discharge in our study was 54 of 191 patients (28%) who gasped but only 80 of 1027 patients (8%) who did not (P<0.0001). This is remarkably similar to the 27% OHCA survival rate among patients who gasped and 9% among those without agonal respiration reported by Clark and associates14 >15 years ago.
Our analysis of the PFDRDC data revealed that 39% of consecutive patients with confirmed witnessed or unwitnessed OHCA gasped, a frequency similar to that in 2 previous reports. Clark and associates14 reported that gasping was present in 40% of all arrests, and Bang and associates15 reported that gasping was present in 40% of 100 dispatcher calls for cardiac arrest. Although similar, our data may actually underestimate the incidence of gasping because our PFDRDC text files included both witnessed and unwitnessed cardiac arrests. Clark et al14 reviewed taped recordings from dispatch centers and reported agonal respiration or gasping activity in 55% of 445 out-of-hospital patients with a witnessed (seen or heard) arrest.
The incidence of gasping decreases rapidly with time. Gasping was present in 39 of 119 patients (33%) who arrested after EMS arrival, in 73 of 363 patients (20%) when EMS arrival was <7 minutes, in 50 of 360 patients (14%) when EMS arrival time was 7 to 9 minutes, and in 25 of 338 patients (7%) when EMS arrival time was >9 minutes.
Among the 481 patients who were receiving bystander CPR, 30 of 77 gaspers (39%) and only 38 of 404 nongaspers (9.4%) survived (adjusted OR, 5.1; 95% CI, 2.7 to 9.4; Table 4).
The presence or absence of gasping in patients immediately after cardiac arrest has taken on increasing importance because of the national and international debate over continuous-chest-compression CPR versus the necessity for assisted mouth-to-mouth ventilation for bystander CPR. If gasping is present, one could question whether assisted ventilation is required.
Some have suggested that gasping indicates early arrest; thus, if a defibrillator is available, gasping is an indication that the person is in the electric phase and should respond to defibrillation.8 Unfortunately, no published data support that contention. We found gasping in 12% of patients with EMS arrival times >9 minutes, long after the so-called electric phase of fibrillations described by Weisfeldt and Becker.16 Others have suggested that if a defibrillator is not available, the bystander might initiate CPR in the patient with agonal respirations by chest compression alone and later integrate ventilations as the agonal breaths dissipate.17
If gasping were rare in humans, the results of nonparalyzed swine models of OHCA in which gasping is common would be less important. Because gasping is common in humans, these studies are clinically relevant. Such studies have shown that continuous-chest-compression CPR without provision of mouth-to-mouth ventilation has resulted in improved survival.18
If gasping is initially present in almost half of humans in cardiac arrest, as this and other studies indicate, the necessity for early mouth-to mouth ventilation, so-called rescue breathing, may be questioned. Multiple studies in humans have shown no improvement in survival when rescue breathing is added to chest compressions.19,20 Interruptions for rescue breathing make CPR efforts more complicated and result in fewer compressions during this crucial period when perfusion is key to successful resuscitation.20
The presence of gasping has the potential to delay the recognition of cardiac arrest by both bystanders and emergency medical dispatchers and thereby delay the initiation of the critical first link in the chain of survival. However, we were unable to confirm this assumption in this report.
In a recent science advisory, the Emergency Cardiovascular Care Committee of the American Heart Association advocated “hands-only CPR” for lay bystanders of witnessed cardiac arrest.19 This advisory statement did not address the implications of gasping.
This study has several limitations. These findings were based on prehospital documentation in numerous EMS systems in Arizona. Although the EMS personnel whose data collection was critical to this report have repeatedly been admonished to watch for and record abnormal breathing, they may not have accurately identified or recorded gasping in each case. The determination of gasping from written EMS records may have overestimated or underestimated its occurrence. Data on the quality of bystander CPR were not available. Finally, gasping is not diagnostic of VF arrest and could be present in the early minutes of asystolic or pulseless electrical activity arrest.
Conclusions
These data confirm that gasping occurs commonly soon after an OHCA. Furthermore, gasping is most frequent soon after collapse and decreases with time. These data also confirm that bystander resuscitation efforts markedly improve survival in patients who are gasping from cardiac arrest.
CLINICAL PERSPECTIVE
The incidence and significance of gasping after primary cardiac arrest are controversial. This study confirms that gasping is common in the early minutes after cardiac arrest, but in untreated patients its incidence decreases rapidly with time. Gasping was present in 33% of patients who arrested after emergency medical system arrival, in 20% when emergency medical system arrival was <7 minutes, in 14% when arrival time was 7 to 9 minutes, and in 7% when arrival time was >9 minutes. Among the patients who received bystander cardiopulmonary resuscitation, survival to hospital discharge occurred among 39% of patients who gasped versus only 9% who did not gasp. Thus, resuscitation efforts are most effective in patients who gasp. Gasping often delays the recognition of cardiac arrest in patients with witness collapse and thereby may delay prompt initiation of bystander resuscitation efforts. During resuscitation efforts, the return of gasping may be interpreted as a sign of recovery, so resuscitation efforts are often interrupted. Gasping is not a sign of recovery but a sign that resuscitation efforts are effective and should be continued because the chance of survival in such patients is greater. When gasping is present, assisted ventilation during resuscitation efforts might not be necessary. Recognition of gasping and its significance in patients with primary cardiac arrest is important to successful resuscitation efforts.
Acknowledgments
We would like to thank the emergency medical dispatchers at the PFDRDC. Their work is invaluable, is greatly appreciated, and has saved thousands of lives. We also thank the thousands of EMS personnel in Arizona whose dedication and daily sacrifice in the line of duty have resulted in numerous lives saved. Thanks also go to Paula R. Brazil, MA, Arizona Department of Health Services, Bureau of Emergency Medical Services and Trauma System, for her assistance in the preparation of this manuscript.
Footnotes
Disclosures
Dr Ewy is a coinvestigator on an unrestricted grant from the Laerdal Foundation of Stavanger, Norway, and on unrestricted grants to the University of Arizona Foundation, both significant. Dr Berg is a coinvestigator on an unrestricted grant from the Laerdal Foundation of Stavanger, Norway, and has grants from the National Institutes of Health, National Heart, Lung, and Blood Institute, Bethesda, Md, and from Medtronic Inc, all significant, and is on the Scientific Advisory Board of the AHA National Registry of CPR. Dr Kern is the principal investigator of an unrestricted grant from the Laerdal Foundation of Stavanger, Norway, and is on the Scientific Advisory Committee of Zoll Inc and PhysioControl Inc, both not significant. The other authors report no conflicts.
References
- 1.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac arrest in the United States. Circulation. 2001;104:2158–2163. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 2.Becker LB, Berg RA, Pepe PE, Idris AH, Aufderheide TP, Barnes TA, Stratton SJ, Chandra NC. A reappraisal of mouth-to-mouth ventilation during bystander-initiated cardiopulmonary resuscitation: a statement for healthcare professionals from the Ventilation Working Group of the Basic Life Support and Pediatric Life Support Subcommittees, American Heart Association. Ann Emerg Med. 1997;30:654–666. doi: 10.1016/s0196-0644(97)70085-4. [DOI] [PubMed] [Google Scholar]
- 3.Holmberg M, Holmberg S, Herlitz J, Gardelov B. Survival after cardiac arrest outside hospital in Sweden: Swedish Cardiac Arrest Registry. Resuscitation. 1998;36:29–36. doi: 10.1016/s0300-9572(97)00089-0. [DOI] [PubMed] [Google Scholar]
- 4.Holmberg M, Holmberg S, Herlitz J. Effect of bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest patients in Sweden. Resuscitation. 2000;47:59–70. doi: 10.1016/s0300-9572(00)00199-4. [DOI] [PubMed] [Google Scholar]
- 5.Vadeboncoeur T, Bobrow BJ, Clark L, Kern KB, Sanders AB, Berg RA, Ewy GA. The Save Hearts in Arizona Registry and Education (SHARE) program: who is performing CPR and where are they doing it? Resuscitation. 2007;75:68–75. doi: 10.1016/j.resuscitation.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Hauff SR, Rea TD, Culley LL, Kerry F, Becker L, Eisenberg MS. Factors impeding dispatcher-assisted telephone cardiopulmonary resuscitation. Ann Emerg Med. 2003;42:731–737. doi: 10.1016/s0196-0644(03)00423-2. [DOI] [PubMed] [Google Scholar]
- 7.Zabala Arguelles JI, Maranon Pardillo R, Gonzalez Serrano P, Serina Ramirez C. Main vascular access in situations of extreme urgency: intra-osseous infusion [in Spanish] An Esp Pediatr. 1992;37:489–492. [PubMed] [Google Scholar]
- 8.Rea TD. Agonal respirations during cardiac arrest. Curr Opin Crit Care. 2005;11:188–191. doi: 10.1097/01.ccx.0000162095.08148.64. [DOI] [PubMed] [Google Scholar]
- 9.Eisenberg MS. Incidence and significance of gasping or agonal respirations in cardiac arrest patients. Curr Opin Crit Care. 2006;12:204–206. doi: 10.1097/01.ccx.0000224862.48087.66. [DOI] [PubMed] [Google Scholar]
- 10.2005 international consensus on cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) science with treatment recommendations, part 2: adult basic life support. Circulation. 2005;112(suppl):III-5–III-16. doi: 10.1016/j.resuscitation.2005.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soar J, Nolan JP. Cardiopulmonary resuscitation for out of hospital cardiac arrest: American Heart Association advocates chest compression without ventilation. Br Med J. 2008;336:782–783. doi: 10.1136/bmj.39541.489699.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bobrow BJ, Clark LL, Ewy GA, Chikani V, Sanders AB, Berg RA, Richman PB, Kern KB. Minimally interrupted cardiac resuscitation by emergency medical services providers for out-of-hospital cardiac arrest. JAMA. 2008;229:1158–1165. doi: 10.1001/jama.299.10.1158. [DOI] [PubMed] [Google Scholar]
- 13.Bobrow BJ, Vadeboncoeur T, Clark L, Chikani V. Establishing Arizona’s statewide cardiac arrest reporting and educational network. Prehosp Emerg Care. 2008;12:381–387. doi: 10.1080/10903120802100670. [DOI] [PubMed] [Google Scholar]
- 14.Clark JJ, Larsen MP, Culley LL, Graves JR, Eisenberg MS. Incidence of agonal respirations in sudden cardiac arrest. Ann Emerg Med. 1992;21:1464–1467. doi: 10.1016/s0196-0644(05)80062-9. [DOI] [PubMed] [Google Scholar]
- 15.Bang A, Herlitz J, Martinell S. Interaction between emergency medical dispatcher and caller in suspected out-of-hospital cardiac arrest calls with focus on agonal breathing: a review of 100 tape recordings of true cardiac arrest cases. Resuscitation. 2003;56:25–34. doi: 10.1016/s0300-9572(02)00278-2. [DOI] [PubMed] [Google Scholar]
- 16.Weisfeldt ML, Becker LB. Resuscitation after cardiac arrest: a 3-phase time-sensitive model. JAMA. 2002;288:3035–3038. doi: 10.1001/jama.288.23.3035. [DOI] [PubMed] [Google Scholar]
- 17.Idris AH. Reassessing the need for ventilation during CPR. Ann Emerg Med. 1996;27:569–575. doi: 10.1016/s0196-0644(96)70159-2. [DOI] [PubMed] [Google Scholar]
- 18.Ewy GA, Zuercher M, Hilwig RW, Sanders AB, Berg RA, Otto CW, Hayes MM, Kern KB. Improved neurological outcome with continuous chest compressions compared with 30:2 compressions-to-ventilations cardiopulmonary resuscitation in a realistic swine model of out-of-hospital cardiac arrest. Circulation. 2007;116:2525–2530. doi: 10.1161/CIRCULATIONAHA.107.711820. [DOI] [PubMed] [Google Scholar]
- 19.Sayre MR, Berg RA, Cave DM, Page RL, Potts J, White RD. Hands-only (compression-only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation. 2008;117:2162–2167. doi: 10.1161/CIRCULATIONAHA.107.189380. [DOI] [PubMed] [Google Scholar]
- 20.SOS-KANTO Study Group. Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. Lancet. 2007;369:920–926. doi: 10.1016/S0140-6736(07)60451-6. [DOI] [PubMed] [Google Scholar]