Abstract
Insulin resistance and type 2 diabetes (T2D) are closely linked to obesity. Numerous prospective studies have reported on weight gain, insulin resistance, and insulin signaling in experimental animals, but not in humans. We examined insulin signaling in adipocytes from lean volunteers, before and at the end of a 4-wk period of consuming a fast-food, high-calorie diet that led to weight gain. We also examined adipocytes from patients with T2D. During the high-calorie diet, subjects gained 10% body weight and 19% total body fat, but stayed lean (body mass index = 24.3 kg/m2) and developed moderate systemic insulin resistance. Similarly to the situation in T2D subjects, in subjects on the high-calorie diet, the amount of insulin receptors was reduced and phosphorylation of IRS1 at tyrosine and at serine-307 (human sequence, corresponding to murine serine-302) were impaired. The amount of insulin receptor substrate protein-1 (IRS1) and the phosphorylation of IRS1 at serine-312 (human sequence, corresponding to murine serine-307) were unaffected by the diet. Unlike the T2D subjects, in subjects on the high-calorie diet, likely owing to the ongoing weight-gain, phosphorylation of MAP-kinases ERK1/2 became hyperresponsive to insulin. To our knowledge this study is the first to investigate insulin signaling during overeating in humans, and it demonstrates that T2D effects on intracellular insulin signaling already occur after 4 wks of a high-calorie diet and that the effects in humans differ from those in laboratory animals.
INTRODUCTION
Type 2 diabetes (T2D) is closely linked to obesity (1) and is attributable to reduced sensitivity to insulin in the main target tissues of this hormone, and failure of the insulin-producing β-cells of the pancreas to increase the release of insulin to compensate for the reduced insulin sensitivity. Control of target cells by insulin involves binding to and activating cell-surface receptors via autophosphorylation of tyrosine residues. These are recognized by a set of signal transducers, particularly the insulin receptor substrate protein-1 (IRS1), which in turn is phosphorylated on tyrosine residues. Thus, phosphorylated IRS1 can bind and activate phosphatidylinositol 3′-kinase, which activates downstream signaling to metabolic controls. Tyrosine-phosphorylated IRS1 can also bind Grb2, which initiates a Ras-mediated activation of MAP-kinases ERK1/2 for mitogenic control via phosphorylation of transcription factors. In contrast, the molecular mechanisms behind insulin resistance in humans are poorly understood (2,3). In T2D, insulin-induced phosphorylation of IRS1 on tyrosine residues has been shown to be impaired in both human skeletal muscle (4–7) and adipose tissue (8,9). In adipocytes from patients with T2D we have found that a positive feedback control loop, involving phosphorylation of IRS1 at serine-307 (human sequence, corresponding to serine-302 in the murine sequence) is not fully functional (10,11). On the other hand, other studies have reported increased phosphorylation of IRS1 at serine-312 (human sequence, corresponding to serine-307 in the murine sequence), which is part of a negative feedback loop (reviewed in 12–16).
Many studies have investigated obesity in humans, and some have prospectively evaluated effects of weight reduction in obese subjects (17), but very few modern studies have examined lean human subjects during weight gain (18,19). Many animal studies, however, have been performed to investigate the influence of obesity, weight gain, and high-fat feeding on metabolic control and insulin sensitivity (reviewed in 12–16). We present the first reported study of insulin signaling in adipocytes from healthy human beings subjected to high-calorie overeating.
MATERIALS AND METHODS
Subjects and Study Description
Informed consent was obtained from all participating individuals, and the study procedures were approved by the ethics committee at Linköping University and were performed in accordance with the Declaration of Helsinki.
This study originally included 18 young volunteers (20). Participants agreed to increase their body weight by 5%–15% by eating two fast-food meals a day and restricting their physical activity to 5000 steps a day during a 4-wk period (20). Adipose tissue biopsies were obtained from each participant at the start and end of the study period. Because of the leanness of the subjects at the start of the study (Table 1), we could not get enough adipose tissue from several subjects. The small biopsy volumes of tissue also restricted the type and number of analyses. From a subgroup of six subjects (four females and two males) who exhibited increased insulin levels, we obtained enough material to analyze selected aspects of insulin signaling.
Table 1.
Characteristics of subjects participating in the high-calorie diet.a
| BMI, kg/m2 |
Total body fat, kg
|
Insulin, pmol/L
|
HOMA
|
QUICKI
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age, years | Baseline | End | Baseline | End | Baseline | End | Baseline | End | Baseline | End |
| 27.3 ± 3.2 | 22.4 ± 1.8 | 24.3 ± 2.2 | 17.6 ± 6.0 | 21.0 ± 6.7 | 36.7 ± 15.9 | 50.3 ± 17.9 | 1.1 ± 0.5 | 1.6 ± 0.6 | 0.385 ± 0.056 | 0.356 ± 0.038 |
| P = 0.002 | P = 0.006 | P = 0.030 | P = 0.036 | P = 0.029 | ||||||
Values are the average for the participating subjects at the start of the study (baseline) and at the end, or the ratio of the averages for the values at the end and at baseline, means ± SD (n = 6), P from paired Student t test. Body composition was determined by dual energy x-ray absorptiometry (Hologic 4500, Hologic). BMI, body mass index; HOMA, homeostasis model assessment (30); QUICKI, quantitative insulin sensitivity check index (31).
The study participants were subjected to dual-energy x-ray absorptiometry (Hologic 4500; Hologic, Waltham, MA, USA) for analysis of body composition. During the study period the average energy intake of the six participants approximately doubled compared with intake before the intervention (Table 2). During intervention, on average, 37% of the dietary energy was from fat, 47% from carbohydrates, (43% mono- and disaccharides [Table 2]), and 15% from protein. The detailed composition of the diet was based on reports obtained 3 d before the study (baseline) and another 3-d period at the end of the first (period 1) and third (period 2) wk of the study. In most cases the exact food composition given by the corresponding fast-food restaurant could be used as a source of information, but when such information was incomplete we used food composition charts. For food bought at grocery stores, manufacturer information was used. If no such information was available, the item was substituted with a similar item in the database of the Swedish National Food Administration. Total caloric intake and intake of macronutrients were also determined for the whole study period, and these determinations were based on all food receipts and on interviews performed after the intervention period.
Table 2.
Characteristics of food intake.a
| Intake | Baseline | Period 1 | Period 2 |
|---|---|---|---|
| Mono- and disaccharides, g/day | 102 ± 35 | 270 ± 52 | 244 ± 45 |
| Total carbohydrates, g/day | 243 ± 49 | 600 ± 108 | 566 ± 112 |
| Total energy, MJ/day | 8.54 ± 1.37 | 23.69 ± 2.77 | 23.14 ± 4.24 |
Values are the averages for the participating subjects 3 d before the study (baseline) and during two 3-d periods, at the end of the first week (period 1) and at the end of the third week (period 2) of the study, means ± SD (n = 6).
Subcutaneous adipose tissue was excised by needle aspiration after study participants received local anesthesia with mepivacain (Carbocain®, AstraZeneca AB, Södertälje, Sweden). Approximately 10 mL of tissue was aspirated in a fanlike area unilaterally in the umbilical region. On the second occasion fat was from the contralateral umbilical region. For determination of insulin concentrations blood was drawn while study participants were in a fasting state.
For a comparison with the diabetic state, subjects with or without T2D were recruited consecutively as they were scheduled for elective surgery at the department of Obstetrics and Gynecology at the University Hospital in Linköping. Subcutaneous fat was obtained during abdominal surgery (laparotomy) while patients were under general anesthesia. A 1.5-cm broad slice of subcutaneous tissue from the skin to the muscle fascia was excised. The only selection criterion for nondiabetic subjects was that they did not have a diabetes diagnosis. Patients with diagnosed T2D were included if they conformed to criteria for the metabolic syndrome: obesity/ overweight (body mass index [BMI] > 28) and dyslipidemia and/or hypertension. We did not match control subjects for obesity or BMI. Therefore both our non-diabetic subjects and patients with diabetes were not selected for anything but the absence or presence of the disease, respectively.
Materials
Mouse antiphosphotyrosine (PY20) monoclonal antibodies were from Transduction Laboratories (Lexington, KY, USA). Rabbit phosphothreonine(308)-protein kinase B and anti-IRS1 polyclonal antibodies were from Upstate Biotech (Charlottesville, VA, USA). Anti–phosphoserine(307)-IRS1, anti–phosphoserine(312)-IRS, and phospho-ERK1/2 polyclonal antibodies were from Cell Signaling Technologies (Beverly, MA, USA). Rabbit polyclonal anti–insulin receptor β-subunit and antiactin antibodies were from Santa Cruz Biotechnology (Santa Cruz, CA, USA).
Isolation and Incubation of Adipocytes
Adipose tissue samples, obtained by needle aspiration or by surgical excision, were cut into small pieces, and adipocytes were isolated after digestion by collagenase (Type 1, Worthington Biochemical Corporation, Lakewood, NJ, USA) as described (21). Cells were treated and incubated with the indicated concentration of insulin in supplemented Krebs-Ringer solution as described previously (9).
SDS-PAGE and Immunoblotting
Cell incubations were terminated by separating cells from medium using centrifugation through dinonylphtalate. To minimize postincubation signaling modifications in the cells and protein modifications, which can occur during immunoprecipitation, the cells were immediately dissolved in SDS and β-mercaptoethanol with protease and protein phosphatase inhibitors, frozen within 10 s, and thawed in boiling water for further processing (21). Total cell number, cell surface, or cell volume of the adipocytes can be compared. Adipocytes consist of a central lipid droplet occupying >95% of the cell volume, and the cytosol is a 200–500-nm thin film beneath the plasma membrane. We therefore compared total volumes of cells as a good approximation to a comparison based on cytosolic volume or cell surface area. Equal amounts of cells, as determined by lipocrit (that is, total cell volume) were subjected to SDS-PAGE and immunoblotting (8) and evaluated by use of chemiluminescence imaging (Las 1000; Image-Gauge, Fuji, Tokyo, Japan). The amount of actin protein was the same in the adipocytes obtained at baseline and at the end of the high-calorie intervention (not shown), and also in adipocytes from nondiabetic controls compared with patients with T2D. Moreover, the amount of insulin receptor and IRS1, and the phosphorylation of IRS1 at tyrosine, protein kinase B, and ERK1/2 were normalized to the amount of actin in each sample; the phosphorylation of IRS1 at serine 307 or serine 312 was normalized to the amount of IRS1 in each sample.
Dose-response data were normalized to percentage of maximal effect, and the effect of insulin was fitted to experimental data by using the sigmoidal dose-response algorithm of GraphPad Prism 4 (GraphPad Software, San Diego, CA, USA). Curves were compared statistically by use of the F-test with the sigmoidal curve-fitting algorithm in Graph-Pad Prism 4. When indicated, Student t test was used to compare control and intervention groups. The null hypothesis was rejected if P was <0.05.
RESULTS
Whole-Body Effects
Subjects increased their BMI from the low baseline value of 22.4 kg/m2 to a moderate 24.3 kg/m2, which corresponded to a total body fat increase of 19%, or 3.4 kg, on average, as determined by dual-energy x-ray absorptiometry (Table 1). The fat deposition was paralleled by development of a moderate, but significant, systemic insulin resistance measured both as increased insulin resistance (homeostasis model assessment) and as decreased insulin sensitivity (quantitative insulin sensitivity check index), and also as increased fasting concentrations of circulating insulin (Table 1).
Insulin Signaling in Isolated Adipocytes
Insulin binding sites have been found to be reduced on adipocytes from obese and insulin-resistant subjects (22). We therefore examined the effect of the high-calorie diet on the amount of insulin receptors in the isolated adipocytes. The concentration of insulin receptors was significantly reduced by about 40% at the end of the diet compared with baseline levels (Table 3), such as could result from reduced FOXO1 activation of insulin receptor transcription (23). A similar reduction of the amount of receptors was found in cells from patients with T2D, compared with nondiabetic subjects (Table 3). The cellular concentration of IRS1 was found to be reduced in adipocytes from patients with T2D (24). In our subjects, however, we observed no significant effect of the high-calorie diet on the concentration of IRS1 protein (Table 3), nor did we detect any difference in the concentration of IRS1 in adipocytes from patients with T2D compared with the group of nondiabetic subjects (Table 3).
Table 3.
Cellular concentration of insulin receptor and IRS1.a
| Diet, % of baseline | T2D, % of controls | |
|---|---|---|
| Insulin receptor | 57 ± 7, P = 0.001 | 55 ± 12, P = 0.035 |
| IRS1 | 103 ± 21 | 98 ± 30 |
The amounts of insulin receptor or IRS1 in adipocytes were compared at baseline and after 4 wks on the high-calorie diet. Samples from the same subjects were analyzed on the same gel by SDS-PAGE and immunoblotting. Results are expressed as percentage of the amount of protein at the start (baseline) of the high-energy diet, mean ± SE (n = 6). The amounts of insulin receptor or IRS1 were also compared in adipocytes from subjects with T2D (age 33–72 years, average 53 years; BMI 28–48 kg/m2, average 36 kg/m2 [n = 16]), with cells from nondiabetic controls (age 34–80 years, average 62 years; BMI 20–39 kg/m2, average 28 kg/m2 [n = 17]). Samples from subjects with and without T2D were analyzed on the same gels, by SDS-PAGE and immunoblotting. Results are expressed as a percentage of nondiabetic controls, mean ± SE. P, paired Student t test.
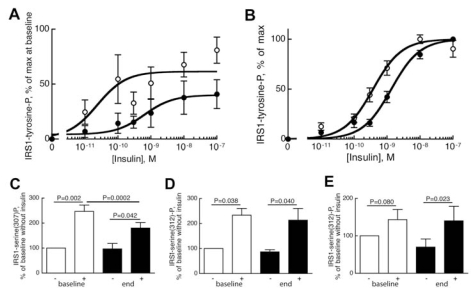
The concentration of insulin needed for the insulin receptor to phosphorylate IRS1 at tyrosine was low at the start of the high-calorie diet, but the cells required several-fold higher concentrations of insulin at the end of the intervention (Figure 1A). The maximal effect of insulin on phosphorylation of IRS1 at tyrosine was also reduced (Figure 1A). A similarly reduced sensitivity to insulin was seen in cells from patients with T2D compared with nondiabetic controls (Figure 1B). Because of technical limitations we could not compare the maximal effect of insulin on this number of subjects, but we have previously reported a tendency toward lower maximal effects of insulin in diabetic adipocytes (8).
Figure 1.
Phosphorylation of IRS1 at tyrosine (A,B) at serine-307 (C) and serine-312 (D,E). (A,B) Adipocytes obtained at baseline (open circles) and at the end (closed circles) of the high-calorie overeating period (A) or from patients with type 2 diabetes (closed circles), age 35–74 years, average 57 years; BMI 28–43 kg/m2, average 35 kg/m2 (n = 15) compared with nondiabetic controls (open circles), age 31–82 years, average 55 years; BMI 23-33 kg/m2, average 26 kg/m2 (n = 16) (B), were incubated with the indicated concentration of insulin for 10 min, when incubations were terminated and equal volumes of whole cells were subjected to SDS-PAGE and immunoblotting for phosphotyrosine. The phosphorylation of IRS1 is expressed as a percentage of maximal insulin effect at the start (baseline) of the high-calorie diet, mean ± SE (n = 6) (A), or as a percentage of maximal insulin effect in control cells and in diabetic cells, respectively, mean ± SE (B). Samples from the same subject were analyzed on the same gel. The curves were statistically different: P = 0.0009 (A); P < 0.0001 (B), F-test. (C–E) Adipocytes obtained at baseline (open bars) and at the end (closed bars) of the high-calorie overeating period were incubated with (+) or without (−) 100 nmol/L insulin, as indicated. After 10 min (C,E) or 30 min (D) incubations were terminated and equal volumes of whole cells were subjected to SDS-PAGE and immunoblotting for phosphorylation of IRS1 at serine-307 (C) or serine-312 (D,E). Whereas insulin-stimulated phosphorylation of IRS1 at serine-307 is maximal after 10 min, the phosphorylation at serine-312 requires 30 min (10); we therefore incubated for 10 or 30 min, as indicated. The phosphorylation of IRS1 in response to insulin is expressed as a percentage of baseline phosphorylation without insulin; mean ± SE (C, n = 6; D, n = 3; E, n = 6). Samples from the same subject were analyzed on the same gel. Paired Student t test was used for statistical analysis.
We have previously reported that in obese patients with T2D, a positive feedback control loop, to phosphorylation of IRS1 at serine-307 (human sequence, corresponding to serine-302 in the murine sequence), is attenuated (10,11). Interestingly, at the end of the high-calorie feeding period, insulin-induced phosphorylation at serine 307 was attenuated (Figure 1C), which was similar to our earlier observation in adipocytes from diabetic patients (11). In contrast, neither the basal level of phosphorylation at serine-312 (corresponding to serine-307 in the murine sequence) nor the effect of insulin on inducement of phosphorylation at this serine was affected by the high-calorie diet (Figure 1D and E). This result was again similar to the situation in T2D (9).
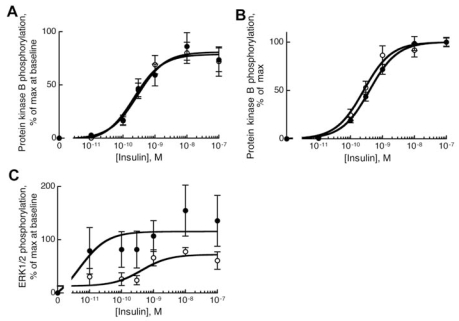
The high-calorie diet had no significant effect on the downstream phosphorylation of protein kinase B at threonine-308 in response to insulin (Figure 2A). Likewise, in adipocytes from patients with T2D the sensitivity to insulin for phosphorylation of protein kinase B was similar to that in cells from nondiabetic controls (Figure 2B).
Figure 2.
Insulin sensitivity for phosphorylation of protein kinase B (A,B) and MAP-kinases ERK1/2 (C). (A,C) Adipocytes obtained at baseline (open circles) and at the end (closed circles) of the high-calorie overeating period were incubated with the indicated concentration of insulin for 10 min, when incubations were terminated and equal volumes of whole cells were subjected to SDS-PAGE and immunoblotting for phosphorylation of protein kinase B at threonine-308 (A) or phosphorylation of MAP-kinases ERK1/2 (C). Phosphorylation is expressed as a percentage of maximal insulin effect at the start (baseline) of the high-fat diet, mean ± SE (n = 6). Samples from the same subject were analyzed on the same gel. The two curves in (C) were statistically different (P = 0.006, F-test). (B) Adipocytes from patients with T2D (closed circles), age 35–74 years, average 57 years; BMI 28–43 kg/m2, average 34 kg/m2 (n = 16); and from nondiabetic controls (open circles), age 31-94 years, average 58 years; BMI 17–33 kg/m2, average 25 kg/m2 (n = 17), were incubated with the indicated concentration of insulin for 10 min, when incubations were terminated and equal volumes of whole cells were subjected to SDS-PAGE and immunoblotting for phosphorylation of protein kinase B at threonine-308. The phosphorylation is expressed as a percentage of maximal insulin effect in control cells and diabetic cells, respectively, mean ± SE.
The downstream effect of insulin to phosphorylate MAP-kinases ERK1/2 was enhanced at the end of the high-calorie diet, and both the sensitivity to insulin and the maximal response were affected (Figure 2C).
DISCUSSION
Several conclusions can tentatively be drawn from this study of high-calorie diet and rapid weight gain in lean human subjects, in comparison with T2D and the metabolic syndrome. First, in the study participants a significant, albeit moderate, systemic insulin resistance had already developed after 4 weeks on a high-calorie diet. Second, this effect was reflected in altered insulin signal transduction in adipocytes, which in several aspects approached the situation in cells from patients with T2D. Third, insulin downstream mitogenic signaling to phosphorylation and activation of MAP-kinases ERK1/2 was enhanced, in sharp contrast to the situation in T2D. Fourth, these changes in insulin signaling occurred in lean and healthy young people with a very low degree of adiposity. Even after diet and weight gain the study subjects were not obese or overweight, hence our findings suggest that, at least within the time scale of this study, weight gain caused the lowering of insulin sensitivity. This conclusion is a mirror image of clinical observations that obese and insulin-resistant people improve their insulin sensitivity by weight reduction and increased physical activity, even if these individuals remain obese or overweight (17,25).
Although it was not possible to match T2D patients to our young and lean overeating study group, it is very interesting to compare the effects of overeating on insulin signaling with the situation in adipocytes from patients with T2D. The effects of overeating on the amount of insulin receptor, and on phosphorylation of IRS1 at tyrosine and at serine-307, were similar to the situation in adipocytes from patients with T2D (herein and [11]), as was the lack of effect on the amount of IRS1 protein and phosphorylation of IRS1 at serine-312 (herein and [9]). These effects were, moreover, also found in adipocytes made insulin resistant by incubation with the diabetogenic adipokine RBP4 (9). The normal state of phosphorylation of IRS1 at serine-312 was reflected in the unperturbed levels of IRS1 protein at the end of the diet or in the diabetic state, because phosphorylation of this serine residue in H4IIE rat hepatoma cells has been linked to increased degradation of IRS1 (26). The insulin-stimulated phosphorylation of protein kinase B was not affected by the diet in study participants, nor in individuals with T2D (herein), or in response to RBP4 (9). These findings are similar to what has been observed in skeletal muscle of obese and diabetic patients, in whom muted association of IRS1 (or IRS2) with PI3-kinase does not affect the phosphorylation of protein kinase B in response to insulin (4).
The hyperresponsive effects of high-calorie overeating on insulin control of ERK1/2 and mitogenic signaling were the opposite of the situations in both T2D and after induction of insulin resistance by RBP4, where the sensitivity to insulin is reduced (9). This observation is interesting because cells from diabetic patients reflect a steady-state situation, whereas we examined adipocytes obtained at the end of 4 weeks of a high-calorie diet while the subjects were still on the diet. Hence, at this time point weight gain had not stabilized. The adipose tissues of these subjects should therefore have been in a hypertrophic mode to accommodate the increasing storage of triacylglycerol. This situation is likely reflected in the insulin-hyperresponsive ERK1/2, which are part of the major insulin-regulated cell growth–controlling signaling pathway. The MAP-kinase signaling pathway has been shown to be critical for proliferative effects of insulin in H4IIE hepatoma cells (27), and ERK1−/− mice do indeed have reduced adiposity and are resistant to obesity induced by high fat intake, and ERK1 is required for adipogenesis in embryo fibroblasts from these mice (28). In a follow-up to this study it will be important to analyze to what extent overeating affects the number versus size of the adipocytes, as well as to examine how ERK1/2 respond to insulin in subjects who have attained a new steady-state energy balance and stabilized higher body weight. Studies of animal cells (3T3-L1 adipocytes) have demonstrated that increased activity of ERK1/2 causes a dramatic downregulation of IRS1 protein in the cells (29), a situation that was obviously not the case with human adipocytes.
This feasibility study produced statistically significant results despite a small number of subjects. The study subjects acted as their own controls, with their baseline data compared with their data at the end of the diet. There were more female than male subjects (2:1), a situation that may have confounded the results. Thus in the future it will be important to address possible sex differences in isolated adipocytes during overeating. We have, however, previously found no difference in insulin signaling when we examined adipocytes from male and female patients with T2D (8). The small biopsy volumes of tissue that could be obtained from lean subjects restricted the type and number of analyses that could be done. Nevertheless the results demonstrate that such studies of humans are feasible and, indeed, necessary to advance understanding of the effects of overeating on human fat cells. This study was restricted to examination of abdominal subcutaneous fat, because open surgery is required to obtain visceral fat. Visceral fat is often considered to be more associated with disease than subcutaneous fat. We nevertheless did record substantial effects on insulin signaling in the subcutaneous fat. It remains to be determined if these results reflect similar effects in the visceral fat or if visceral fat has a qualitatively different response to overeating.
Much is known about effects of high-fat feeding and adiposity in experimental animals, especially in transgenic mice that overexpress or are deficient in an array of various proteins, which in many cases have been found to protect the animals from or make the animals more susceptible to obesity, insulin resistance, and diabetes (reviewed in 12–16). One finding in studies with animals is that metabolic overload from high-calorie overeating inhibits insulin signaling via increased phosphorylation of IRS1 at serine residues, especially serine-307 (murine sequence, corresponding to serine-312 in the human sequence) (reviewed in 12–16). In the fat cells of our study participants at the end of the high-calorie overeating period, the phosphorylation of serine-312 was not affected, whereas phosphorylation of serine-307 (corresponding to serine-302 in the murine sequence) was attenuated. This result compares well with that found in human T2D. One should bear in mind that most experimental animals have been bred for generations with unlimited food availability and little opportunity for physical activity and have thus been genetically selected to the conditions being studied, characteristics that are not present in human beings.
Our study of weight gain induced by a high-calorie, high-fat diet raises many questions that should be approached in a larger follow-up to this first study. Topics requiring further investigation include effects on insulin control of glucose uptake, other aspects of insulin signaling such as insulin signaling in skeletal muscle and when body weight is at a steady state after weight gain, hypertrophia versus hyperplasia of the adipocytes, sex differences, and the extent of differing responses of visceral and subcutaneous adipocytes. An important further objective would be to quantify and characterize any adipose tissue macrophage infiltration during weight gain. Compared with studies of animals, the study of humans involves severe limitations to what can be done. To study weight gain in lean humans, moreover, means that the small biopsy volumes of adipose tissue that can be obtained restrict the type and number of analyses. This study demonstrates that studies of humans are required and that in spite of many limitations such studies yield important insight and understanding.
ACKNOWLEDGMENTS
Financial support was obtained from Östergötland County Council, Medical Research Council of Southeast Sweden, European Commission Network of Excellence Biosim, Novo Nordisk Foundation, Swedish Diabetes Association, and Swedish Research Council.
Footnotes
Online address: http://www.molmed.org
DISCLOSURE
We declare that the authors have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
REFERENCES
- 1.Colditz GA, et al. Weight as risk factor for clinical diabetes in women. Am J Epidemiol. 1990;132:501–13. doi: 10.1093/oxfordjournals.aje.a115686. [DOI] [PubMed] [Google Scholar]
- 2.Biddinger SB, Kahn CR. From mice to men: insights into the insulin resistance syndromes. Ann. Rev. Physiol. 2006;68:20.21–36. doi: 10.1146/annurev.physiol.68.040104.124723. [DOI] [PubMed] [Google Scholar]
- 3.Muoio DM, Newgard CB. Molecular and metabolic mechanisms of insulin resistance and beta-cell failure in type 2 diabetes. Nature Rev Mol Cell Biol. 2008;9:193–205. doi: 10.1038/nrm2327. [DOI] [PubMed] [Google Scholar]
- 4.Kim Y-B, Nikoulina SE, Ciaraldi TP, Henry RR, Kahn BB. Normal insulin-dependent activation of Akt/protein kinase B, with diminished activation of phosphoinositide 3-kinase, in muscle in type 2 diabetes. J Clin Inv. 1999;104:733–41. doi: 10.1172/JCI6928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goodyear L, et al. Insulin receptor phosphorylation, insulin receptor substrate-1 phosphorylation and phosphatidylinositol 3-kinase activity are decreased in intact skeletal muscle strips from obese subjects. J Clin Inv. 1995;95:2195–204. doi: 10.1172/JCI117909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cusi K, et al. Insulin resistance differentially affects the PI 3-kinase and MAP kinase-mediated signaling in human muscle. J Clin Inv. 2000;105:311–20. doi: 10.1172/JCI7535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Björnholm M, Kawano Y, Lehtihet M, Zierath J. Insulin receptor substrate-1 phosphorylation and phosphatidylinositol 3-kinase acitivity in skeletal muscle from NIDDM subjects after in vivo insulin stimulation. Diabetes. 1997;46:524–7. doi: 10.2337/diab.46.3.524. [DOI] [PubMed] [Google Scholar]
- 8.Danielsson A, et al. Insulin resistance in human adipocytes downstream of IRS1 after surgical cell isolation, but at the level of phosphorylation of IRS1 in type 2 diabetes. FEBS J. 2005;272:141–51. doi: 10.1111/j.1432-1033.2004.04396.x. [DOI] [PubMed] [Google Scholar]
- 9.Öst A, et al. Retinol-binding protein-4 attenuates insulin-induced phosphorylation of IRS1 and ERK1/2 in primary human adipocytes. FASEB J. 2007;21:3696–704. doi: 10.1096/fj.07-8173com. [DOI] [PubMed] [Google Scholar]
- 10.Danielsson A, Nystrom FH, Strålfors P. Phosphorylation of IRS1 at serine 307 and serine 312 in response to insulin in human adipocytes. Biochem Biophys Res Commun. 2006;342:1183–87. doi: 10.1016/j.bbrc.2006.02.075. [DOI] [PubMed] [Google Scholar]
- 11.Danielsson A, Öst A, Nystrom FH, Strålfors P. Attenuation of insulin-stimulated insulin receptor substrate-1 serine 307 phosphorylation in insulin resistance of type 2 diabetes. J Biol Chem. 2005;280:34389–92. doi: 10.1074/jbc.C500230200. [DOI] [PubMed] [Google Scholar]
- 12.Gual P, LeMarchand-Brustel Y, Tanti J-F. Positive and negative regulation of insulin signaling through IRS-1 phosphorylation. Biochemie. 2005;87:99–109. doi: 10.1016/j.biochi.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 13.Um SH, D’Alessio D, Thomas G. Nutrient overload, insulin resistance, and ribosomal protein S6 kinase 1, S6K1. Cell Metab. 2006;3:393–402. doi: 10.1016/j.cmet.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–7. doi: 10.1038/nature05485. [DOI] [PubMed] [Google Scholar]
- 15.Luca Cd, Olefsky JM. Inflammation and insulin resistance. FEBS Lett. 2008;582:97–105. doi: 10.1016/j.febslet.2007.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guilherme A, Virbasius JV, Puri V, Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nature Rev Mol Cell Biol. 2008;9:367–77. doi: 10.1038/nrm2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petersen KF, et al. Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes. 2005;54:603–8. doi: 10.2337/diabetes.54.3.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salans LB, Horton ES, Sims EAH. Experimental obesity in man: cellular character of the adipose tissue. J Clin Inv. 1971;50:1005–11. doi: 10.1172/JCI106570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lammert O, et al. Effects of isoenergetic overfeeding of either carbohydrate or fat in young men. Br J Nutrition. 2000;84:233–45. [PubMed] [Google Scholar]
- 20.Kechagias S, et al. Fast food based hyper-alimentation can induce rapid and profound elevation of serum alanine aminotransferase in healthy subjects. Gut. 2008;57:649–54. doi: 10.1136/gut.2007.131797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strålfors P, Honnor RC. Insulin-induced dephosphorylation of hormone-sensitive lipase: correlation with lipolysis and cAMP-dependent protein kinase activity. Eur J Biochem. 1989;182:379–85. doi: 10.1111/j.1432-1033.1989.tb14842.x. [DOI] [PubMed] [Google Scholar]
- 22.Olefsky JM. Decreased insulin binding to adipocytes and circulating monocytes from obese subjects. J Clin Inv. 1976;57:1165–72. doi: 10.1172/JCI108384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Puig O, Tjian R. Transcriptional feedback control of insulin receptor by dFOXO/FOXO1. Genes Dev. 2006;19:2435–46. doi: 10.1101/gad.1340505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rondinone CM, et al. Insulin receptor substrate (IRS) 1 is reduced and IRS2 is the main docking protein for phosphatidylinositol 3-kinase in adipocytes from subjects with non-insulin dependent diabetes mellitus. Proc Natl Acad Sci U S A. 1997;94:4171–5. doi: 10.1073/pnas.94.8.4171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dixon JB, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes. J Am Med Assoc. 2008;23:316–23. doi: 10.1001/jama.299.3.316. [DOI] [PubMed] [Google Scholar]
- 26.Greene MW, Sakaue H, Wang L, Alessi DR, Roth RA. Modulation of insulin-stimulated degradation of human insulin receptor substrate-1 by serine 312 phosphorylation. J Biol Chem. 2003;278:8199–211. doi: 10.1074/jbc.M209153200. [DOI] [PubMed] [Google Scholar]
- 27.Törnkvist Å, Parpal S, Gustavsson J, Strålfors P. Inhibition of raf-1 kinase expression abolishes insulin stimulation of DNA synthesis in H4IIE hepatoma cells. J Biol Chem. 1994;269:13919–21. [PubMed] [Google Scholar]
- 28.Bost F, et al. The extracellular signal-regulated kinase isoform ERK1 is specifically required for in vitro and in vivo adipogenesis. Diabetes. 2005;54:402–11. doi: 10.2337/diabetes.54.2.402. [DOI] [PubMed] [Google Scholar]
- 29.Jager J, Gremeaux T, Cormont M, Marchand-Brustel YL. Interleukin-1 beta-induced insulin resistance in adipocytes through down-regulation of insulin receptor substrate-1 expression. Endocrinology. 2007;148:241–51. doi: 10.1210/en.2006-0692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matthews DR, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 31.Katz A, et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000;85:2402–10. doi: 10.1210/jcem.85.7.6661. [DOI] [PubMed] [Google Scholar]