Abstract
Chronic obstructive pulmonary disease (COPD) is characterized by poorly reversible airflow limitation. The pathological hallmarks of COPD are inflammation of the peripheral airways and destruction of lung parenchyma or emphysema. The functional consequences of these abnormalities are expiratory airflow limitation and dynamic hyperinflation, which then increase the elastic load of the respiratory system and decrease the performance of the respiratory muscles. These pathophysiologic features contribute significantly to the development of dyspnea, exercise intolerance and ventilatory failure. Several treatments may palliate flow limitation, including interventions that modify the respiratory pattern (deeper, slower) such as pursed lip breathing, exercise training, oxygen, and some drugs. Other therapies are aimed at its amelioration, such as bronchodilators, lung volume reduction surgery or breathing mixtures of helium and oxygen. Finally some interventions, such as inspiratory pressure support, alleviate the threshold load associated to flow limitation. The degree of flow limitation can be assessed by certain spirometry indexes, such as vital capacity and inspiratory capacity, or by other more complexes indexes such as residual volume/total lung capacity or functional residual capacity/total lung capacity. Two of the best methods to measure flow limitation are to superimpose a flow–volume loop of a tidal breath within a maximum flow–volume curve, or to use negative expiratory pressure technique. Likely this method is more accurate and can be used during spontaneous breathing. A definitive definition of dynamic hyperinflation is lacking in the literature, but serial measurements of inspiratory capacity during exercise will document the trend of end-expiratory lung volume and allow establishing relationships with other measurements such as dyspnea, respiratory pattern, exercise tolerance, and gas exchange.
Keywords: COPD, flow limitation, dynamic hyperinflation, treatment, exercise
Introduction
Chronic obstructive pulmonary disease (COPD) is defined as a disease state characterized by poorly reversible airflow limitation and loss of pulmonary capillary bed. It is usually progressive and associated with abnormal inflammatory responses in the lung (Pauwels et al 2001). Chronic inflammation is a predominant feature of COPD and involves the airways (Saetta et al 2001), lung parenchyma (Saetta et al 1999), and pulmonary vasculature (Peinado et al 1999). It is caused by exposure to inhaled noxious particles and gases present in tobacco smoke (Von Essen et al 1995; Salvi et al 1999) and likely in other air pollutants that may be inhaled during breathing. Macrophages, T lymphocytes (predominately CD8+), and neutrophils are increased numerically as well as activated (Pesci et al 1998), this results in the release of a variety of mediators (Keatings et al 1996; Mueller et al 1996; Yamamoto et al 1997; Beeh et al 2003) that are believed to be capable of unbalance the protease-antiprotease equilibrium (Gottlieb et al 1996; Stockley et al 1999) and damage lung structures (Liu et al 1999; Shapiro and Senior 1999).
The pathological hallmarks of COPD are inflammation of the peripheral airways and destruction of lung parenchyma or emphysema (Thurlbeck 1991). The functional consequence of these abnormalities is expiratory airflow limitation. Since the determinants of expiratory flow through the airways are both the driving alveolar pressure that promotes flow (elastic recoil of the lung) and the opposing resistance of the airways, the reduction in flow occurring in COPD is defined more accurately as airflow limitation rather than airflow obstruction, since both loss of elastic recoil and increase in airway resistance play an important role (Pride and Green 1997). Emphysema will contribute to the airflow limitation by reducing the elastic recoil of the lung through parenchymal destruction, as well as by reducing the elastic load applied to the airways through destruction of alveolar attachments. On the other hand, inflammation of the peripheral airways will contribute to the airflow limitation by increasing the thickness of the airway wall which, together with fibrosis and smooth muscle hypertrophy, may cause airway narrowing (Thurlbeck 1985). The role of mucus hypersecretion in the development of chronic airflow limitation is still controversial (Peto et al 1983; Vestbo et al 1996).
Expiratory flow limitation and dynamic hyperinflation (DH) are clinical and pathologic concepts that have been present for well over 100 years. Recent developments have revitalized the interest on this crucial psychopathological consequence of obstructive disease. In accordance with this renewed interest, a provocative hypothesis has been put forward recently that proposes that the transition from peripheral airways disease to COPD follows three pathophysiological stages defined by the severity of expiratory flow limitation: In Stage I, closing volume eventually exceeds the functional residual capacity (FRC); in Stage II tidal volume expiratory flow limitation (EFL) develops; and in Stage III, DH increases to a point that produces dyspnea and exercise limitation. The presence of airway closure (Stage I) and EFL (Stage II) may promote peripheral airway injury and accelerate the abnormalities of lung function (Milic-Emili 2004).
Pathophysiology of dynamic hyperinflation
Nonmuscular factors
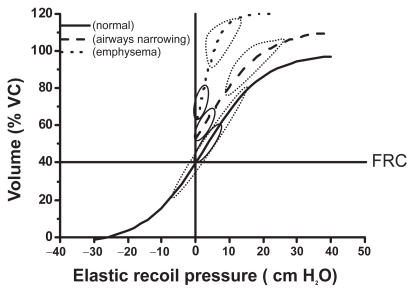
The respiratory system (ie, the combined elastic recoil of the lung and chest wall) is an elastic structure able to change its shape and volume in order to breathe the necessary air in, and the alveolar gas out, to sustain the amount of gas exchange needed to match metabolic needs. Under normal physiological conditions the respiratory muscles provide the power to produce such changes in volume. For a given change in pleural pressure generated by the respiratory muscles, the attainable end-inspiratory and end-expiratory volumes are determined by the passive pressure–volume (P–V) relationship of the respiratory system (Figure 1) (Mead et al 1967; Agostoni and Hyatt 1986). The P–V behavior of the respiratory system is distinctly sigmoid (Figure 1) since the respiratory system is most compliant between 20% to 80% of the vital capacity (VC) (Mead et al 1967; Agostoni and Hyatt 1986). To state this in a clearer way, the elastic work of breathing is minimized by maintaining tidal volume within the 20%–80% of the VC range. In COPD there are different forms and degrees of damage to the alveolar wall resulting in pathophysiological changes in the lung elastic recoil. These changes might reduce the amount of pressure required to achieve a specific change in volume (Cherniack et al 1963; Saksena and Burrows 1966), or simply shift the normal relationship upwards near passive FRC (Figure 1) (Sharp et al 1968). There is limited information about passive elastic recoil characteristics of the lung and chest wall during exercise, but at least in healthy subjects, they remain essentially unchanged, or decrease slightly (Stubbing et al 1980; Younes and Kivinen 1984). Therefore total lung capacity (TLC) does not change significantly during physical activity either in normal subjects or in COPD patients (Stubbing et al 1980).
Figure 1.
Pressure volume relationship of the passive respiratory system. Lower and upper boundaries of the elastic recoil pressure–volume relationship of the respiratory system in healthy subjects (---), in patients with narrowed airways (—), and in patients with loss of lung elastic recoil (·····). The loops represent tidal breathing at rest (—) and during exercise (·····).
Abbreviations: FRC, functional residual capacity; VC, vital capacity.
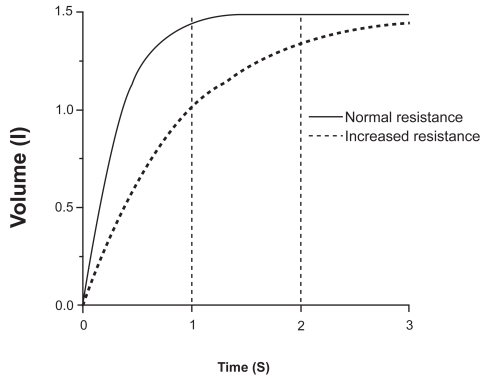
While the P–V relationship determines the attainable volume extremes for a given muscular pressure, the actual volume change in a given amount of inspiratory or expiratory time depends on the pressure–flow (P–F) relationship, which is highly dependent on the airways resistance (in a linear system, the volume at the time tx [Vtx] is given by the expression
where P is the pressure applied, C the compliance of the system, tx the time elapsed, and R the resistance. The product RC is the time constant, which determines the speed of the change), as can be seen in Figure 2. During inspiration, even when inspiratory resistances are high, flow down the airways can be increased by increasing the force of inspiratory muscle contraction up to its maximum capacity (Younes and Riddle 1981). The same is true during expiration at relative low pressures, but during forced expiration in both normal and COPD, increments in alveolar pressure (generated by increasing muscle effort) produce progressively smaller increments in expiratory flow, until flow ultimately reaches a plateau (Figure 3) where it is independent of any increase of driving pressure (Hyatt and Wilcox 1963). This phenomenon is called flow limitation and it seems to be related to the dynamic compression of the intra-thoracic airways at a segment progressively distal as lung volume decreases (Green and Pride 1997). The resulting increase in airways resistance offsets the pressure generated by the additional increase in muscular effort, and therefore expiratory flow is actually largely independent of muscle effort and is determined by the respiratory system elastic recoil. Elastic recoil of the system is proportional to lung volume and the expiratory airways conductance (ie, the inverse of resistance) (Hyatt 1983). Respiratory mechanics in COPD are characterized by both elevated inspiratory and expiratory resistance to airflow (McGregor and Becklake 1961; Citterio 1981; Aldrich et al 1989). An increased inspiratory airflow resistance can be compensated by augmenting the activation of the inspiratory muscles (Im Hof et al 1986), but the increased expiratory resistance, together with the reduced lung elastic recoil present in these patients, further limits expiratory flow (Hyatt 1961). This is physiologically much more deleterious because expiration is primarily effort independent (Figure 3), and cannot be compensated by increasing expiratory muscle effort (Poon et al 1987). The consequence in COPD is that the time needed for lung units to empty their volume and achieve their passive equilibrium point is significantly increased and many of them do not reach their relaxation volume before a new inspiration is initiated. As a result, part of the gas that would have been expired in a normal lung remains “trapped” (ie, more gas remains inside that what would be if those units were not altered) and the alveolar pressure at the end of the expiration is higher than the atmospheric pressure (intrinsic PEEP) (Pride and Macklem 1986; Younes 1991). In young healthy subjects RV is about 25% of the TLC, and FRC is about 50% of the TLC (Stocks and Quanjer 1995). In older healthy subjects, RV and FRC are about 30% and 55% of TLC respectively (Stocks and Quanjer 1995). In COPD, values of RV and FRC are increased to values as high as 70% and 85% of the TLC, respectively (Fishman et al 2003). Since tidal breathing is performed at FRC, COPD must breathe at volumes that are very close to TLC where the system is much less distensible (Figure 1).
Figure 2.
Effects of time and resistance on the change in expiratory volume. Rates of changes of volume after a similar given change of alveolar pressure in a subject with normal respiratory system resistance (—) and a resistance 3 times greater (---) such as in COPD, assuming a constant compliance. Note the marked effect of resistance on the volume change, particularly when the available time is shortened.
Abbreviations: COPD, chronic obstructive pulmonary disease.
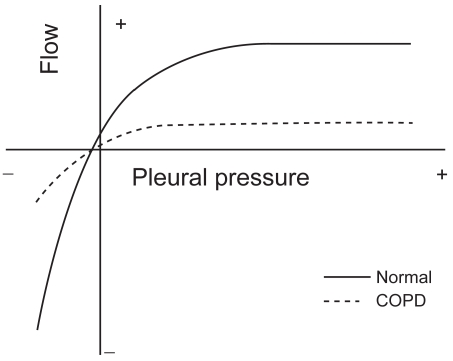
Figure 3.
Iso-volume pressure-flow relationship. Schematic representation of the pressure-flow relationship in a healthy (normal) subject and a patient with COPD, showing the effect of the increased expiratory resistance upon the maximum expiratory flow and in both cases the independence of the maximum flow from the pleural pressure. Copyright © 1986. Modified with permission from Pride NB, Macklem PT. 1986. Lung mechanics in disease. In: Fishman AP (ed). Handbook of physiology, Section 3, Volume III, Part 2: The respiratory system. Bethesda MD: American Physiological Society, pp 659–92.
Abbreviations: COPD, chronic obstructive pulmonary disease.
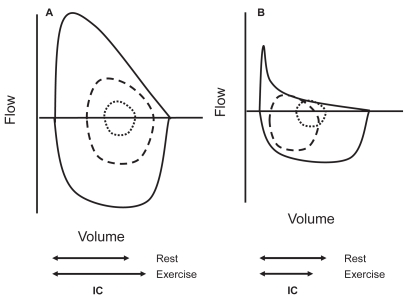
During exercise minute ventilation must increase to meet the increased metabolic demands. This is achieved by increasing both the tidal volume (VT) and the respiratory frequency (fR), what means that the expiratory time necessary to reach passive FRC or below is reduced. In normal young subjects expiratory flow is fast enough to decrease end-expiratory lung volume (EELV) up to 0.5–1L below the resting FRC with increasing work. This is due to the activation of expiratory muscles (Pride and Macklem 1986; Henke et al 1988). The decreased EELV not only allows increasing VT within the most compliant part of the P–V relationship, but also has a beneficial inspiratory effect because, as the expiratory muscles relax, the passive tendency of the respiratory system below FRC is towards inspiration. In older subjects, EELV also decreases during moderate exercise, but thereafter, tends to increase back to near resting levels (Johnson et al 1991). In COPD, due to the increased flow limitation, more and more units are unable to empty their gas as expiratory time decreases when the respiratory rate increases, and EELV typically rises (Figures 1 and 4) (Hyatt 1961; Grimby et al 1968; Potter et al 1971; Dodd et al 1984; Pride and Macklem 1986; Babb et al 1991; Younes 1991; Yan et al 1997; Diaz et al 2000; O’Donell et al 2001; Oga et al 2002, 2003; O’Donnell and Webb 2003; Puente-Maestu et al 2005) in spite of expiratory muscles activity (Dodd et al 1984; Younes 1991). This temporary increase in EELV in COPD above its baseline (admittedly already elevated) value is termed DH. The extent of DH depends on the degree of expiratory flow limitation, the prevailing ventilation, the breathing pattern for a given ventilation, and is inversely related to the level of resting lung hyperinflation (O’Donnell et al 2001; Puente-Maestu et al 2005).
Figure 4.
Maximum and tidal flow-volume curves in subjects with and without flow limitation. In this figure it can be seen an schematic representation of the spontaneous flow-volume curves generated at tidal volume at rest (inner dotted line ····) and peak exercise (dashed line ----) compared with the maximum flow volume curve in a subject without flow limitation able to reduce its end-expiratory lung volume (Panel A) and a flow-limited COPD patient with dynamic hyperinflation (Panel B).
Abbreviations: COPD, chronic obstructive pulmonary disease; IC, inspiratory capacity.
Muscle function
To move the air into the alveoli, sufficient force must be exerted by the respiratory muscles to expand the lungs and the chest wall. In addition, respiratory muscles must overcome the resistance and inertia in the system so that air will flow into the airways. This force is provided by the respiratory muscles and, thus, breathing is the results of their cyclic activation. Whether the net force is inspiratory or expiratory will depend on the balance between the pressure generated by the muscles and the elastic recoil of the respiratory system. The maximum inspiratory and expiratory pressures that the respiratory muscles are able to generate are related to several factors such as age (Black and Hyatt 1969), muscle training (Leith and Bradley 1976), the integrity of the inervation (Gross et al 1980) and, more important for the present discussion, of the length and shape (usually termed as “configuration”) of the respiratory muscles, and particularly of the diaphragm (Marshall 1962). According to the Laplace’s relationship (the Laplace relationship establishes the relationship between the pressure generated across a curved surface “P”, the tension of the surface “T” and its radius “r”: P=T/r), the less curved a surface is, the lower the pressure difference created across it. Thus at high lung volumes, a given neural output would be likely to cause less change in trans-diaphragmatic pressure than at low lung volumes. Furthermore, inspiratory muscles are able to generate less pressure for a given neural input because of their length–tension relationship (Kim et al 1976; Similowski et al 1991; Polkey et al 1998). The ability of the respiratory muscles to sustain a given level of pressure output (endurance) is defined by its pressure time index (PTI) (McGregor and Becklake 1961; Bellee and Grassino 1982, 1983)
Where “Pimus” is the inspiratory muscular pressure needed to achieve a certain displacement of the respiratory system, “MIP” is the maximum inspiratory pressure, “Ti” the inspiratory time and “Ttot” the total respiratory time. Thus the PTI is determined to a considerable degree by how high MIP is, and the fraction of MIP required to sustaining a given VT. MIP decreases as lung volume increases, while maximum expiratory pressure changes in the opposite direction (Agostoni and Hyatt 1986), therefore at high volumes a greater fraction of maximum effort is required to generate the same pressure. Paradoxically, thus, while flow limitation is primarily an expiratory phenomenon, its consequences are mainly suffered by the inspiratory muscles because expiratory muscles cannot appreciably increase flow (Figures 3) (Hyatt 1961, 1983; Hyatt and Wilcox 1963; Pride and Macklem 1986; Green and Pride 1997) to force the emptying of the lungs. In consequence the volume at which the respiratory system has to operate is increased (Hyatt 1961; Grimby et al 1968; Potter et al 1971; Dodd et al 1984; Pride and Macklem 1986; Babb et al 1991; Younes 1991; Yan et al 1997; Diaz et al 2000; O’Donnell et al 2001; Oga et al 2002, 2003; O’Donnell and Webb 2003; Puente-Maestu et al 2005) and hence the elastic work needed for a given displacement of the thorax (Figure 1 and 4) (Cherniack et al 1963; Saksena and Burrows 1966; Mead et al 1967; Sharp et al 1968; Younes and Kivinen 1984; Agostoni and Hyatt 1986). Second inspiratory muscles have to generate a substantial inspiratory pressure (intrinsic PEEP) before inspiratory airflow can occur. PEEP behaves actually as an inspiratory threshold load (Pepe and Marini 1982; Pride and Macklem 1986; Haluszka et al 1990; Younes 1991), and finally, as we have seen above, at high lung volume efficacy of respiratory muscles as pressure generators is greatly reduced (Marshall 1962; Kim et al 1976; Similowski et al 1991; Polkey et al 1998).
Clinical consequences of dynamic hyperinflation
Exercise limitation
Patients with COPD characteristically show a poor exercise performance which is manifested as marked reduction in peak oxygen uptake and decreased endurance to submaximal levels of exercise (Table 1) (Gallagher 1994; Casaburi et al 1999; O’Donnell and Webb 2003). The origin of this poor exercise tolerance is multifactorial and includes abnormal lung mechanics, impaired pulmonary gas exchange, destruction of the pulmonary vascular bed, impaired cardiac function and peripheral muscle dysfunction (Gallagher 1994; Casaburi et al 1999; O’Donnell and Webb 2003). Dynamic hyperinflation has a detrimental impact on exercise tolerance via three important physiopathological mechanisms. The relatively rapid shallow breathing pattern in COPD compared with healthy subjects, reflects the mechanical constraints on tidal volume expansion, which has an exaggerated frequency-dependency in COPD, fR increases with exercise in COPD up to a maximum of about 25–35min−1 (Diaz et al 2000; Nield et al 2003; Puente-Maestu et al 2005). At increased respiratory rates, the inversely proportional decrease in expiratory time, even though there is a slight reduction of Ti/Ttot to 0.40–0.45 (Diaz et al 2000; Puente-Maestu et al 2005), and as result of the decreased expiratory time further DH ensues. When EELV reaches approximately 0.5L tidal volume, ventilation reaches a plateau (or even a slight decreases), exercise soon stops (Figure 5) (O’Donnell et al 2001; Puente-Maestu et al 2005). This encroachment of tidal volume not only hampers the ventilatory response to the metabolic load of exercise, it contributes to reducing the efficiency of ventilation (ie, increases the dead space) as well (Gallagher 1994). This effect, together with the augmented mechanical impedance of the respiratory system results in an increased work and O2 cost of breathing at any given metabolic load compared with age-matched healthy controls, (Roussos et al 1982; Donahoe et al 1989; Shindoh et al 1994; Mannix et al 1999; Takayama et al 2003). In one study this additional oxygen cost has been found to be as much as 40% of the total oxygen uptake (Levison and Cherniack 1968).
Table 1.
Main clinical consequences of dynamic hyperinflation
| Exercise limitation and dyspnea |
| Hypoventilation during exercise |
| Hypercarbic respiratory failure during exacerbations |
| Hypercapnia during exercise |
| Cardiac dysfunction during exercise |
| Weaning failure |
| Hypotension and barotraumas during mechanical ventilation |
| Independent risk factor for survival in COPD subjects |
| Reduced improvement with exercise training |
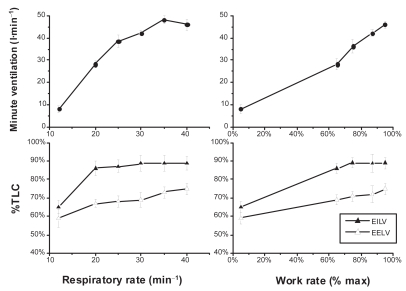
Figure 5.
Tidal volume encroachment by dynamic hyperinflation in COPD. In this figure the effects of respiratory rate and work rate on the end-inspiratory (EILV), end-expiratory lung volume (EELV), tidal volume (ie, EILV–EELV) and minute ventilation in subjects with severe COPD is displayed. While EILV increases with increasing respiratory rate from 20 to 30min−1 (lower left panel), so does EELV resulting in an almost constant (encroached) tidal volume. At respiratory rates higher than 30, though, EILV does not increase any more, however, EELV further increases resulting in a reduced tidal volume and even a drop in ventilation (left upper panel) at respiratory rates higher than 35min−1. In the right lower panel we can see how during progressive exercise tidal volume also decreases at high intensity due again to increase in EELV without parallel increase in EILV (Constructed with data from Puente-Maestu et al 2005).
Abbreviation: COPD, chronic obstructive pulmonary disease; EELV, end-expiratory lung volume; EILV, end-inspiratory lung volume; TLC, total lung capacity.
Dyspnea
Dyspnea is believed to be the unpleasant awareness of the respiratory muscle effort. As it was discussed above DH both increases the pressure changes needed to achieve a given tidal volume and decreases the ability of the respiratory muscles to generate this pressure (Marshall 1962; Kim et al 1976; Similowski et al 1991; Polkey et al 1998). This then increases the amount of pressure needed to achieve a certain tidal volume with respect to the maximum pressure (Killian et al 1992). The change in lung mechanics during exacerbation of COPD has been show to be directly related to dyspnea during spontaneously breathing. The improvement in operating lung volumes (ie, increase in inspiratory capacity [IC]) as the exacerbation resolves is correlated to symptomatic improvement and reductions in dyspnea (Parker et al 2005; Stevenson et al 2005). While COPD patients do not usually stop exercise at higher rates of perceived dyspnea than normal subjects, the ratio of symptoms to the metabolic load and minute ventilation are usually increased (Killian and Jones 1994; Hamilton et al 1996). In these patients there exists a close correlation between breathlessness during exercise and DH (O’Donnell et al 1993; Eltayara et al 1996; Puente-Maestu et al 2005; Vogiatzis et al 2005). In a recent study, arm exercise in COPD has been found to produce DH as well (Gigliotti et al 2005).
Hypoventilation/hypercapnia
The increase in inspiratory and expiratory airway resistance characteristic of COPD would cause only minor problems in ventilatory function (ie, for the respiratory muscles) if the disease, through expiratory flow limitation did not cause dynamic hyperventilation, and its corollaries that include increased elastic recoil, encroached tidal volume, the threshold load imposed by intrinsic PEEP, and the changes in the configuration of the thorax that greatly reduce their ability to generate pressure. When COPD patients with expiratory flow-limitation need to increase their respiratory rate to increase minute ventilation, there is potential for inspiratory muscle failure due to DH (Table 1). During exacerbations, the inflammatory process, the ventilation/perfusion (V′A/Q′) mismatching, increased airflow resistance, and DH, expose the respiratory muscles to the risk of fatigue, eventually leading to ventilatory pump failure and hypercapnia (Rossi et al 1997). DH is one of the major mechanisms involved in the development of hypercapnia and (secondarily hypoxemia) during exercise in COPD patients (Diaz et al 2000; O’Donnell et al 2002).
Cardiac dysfunction
Lung hyperinflation and excessive expiratory muscle recruitment can impair venous return and reduce right ventricular preload in COPD (Mahler et al 1984; Miller, Pegelow, et al 2005). Moreover, large intrathoracic pressure swings generated during exercise to overcome the increased elastic and resistive loads may result in left ventricular dysfunction (increased left ventricular afterload) (Oswald-Mammosser et al 1991; Montes de Oca et al 1996). Right ventricular afterload during exercise is also increased because of the increased pulmonary vascular resistance associated with breathing at lung volumes close to TLC (Ranieri et al 1996; Oswald-Mammosser et al 1998).
Weaning failure
The incidence of EFL was very high in a small sample of patients with COPD receiving invasive mechanical ventilation for acute respiratory failure. In this series IC was lower in patients who failed weaning than those who were successfully weaned (Alvisi et al 2003).
Hypotension and barotrauma in the mechanical ventilated patient
Dynamic hyperinflation is a potential cause of hypotension and barotrauma in mechanically ventilated patients with EFLs (Table 1). DH should be minimized by the use of bronchodilators and appropriately setting minute ventilation (higher tidal volumes, slower respiratory rate, higher I:E ratio) to maximize expiratory time (Schumaker et al 2004).
Exercise training
Most rehabilitation programs are based on constant-load exercise (CLE) training, consisting of sustained exercise for 30–40min (ACCP/AACVPR 1997). Generally, high-intensity training is argued to be needed for the improvement of exercise capacity (Casaburi et al 2001). Although patients with moderately severe COPD (mean forced expiratory volume in one second [FEV1] >45% predicted) can tolerate high levels (80%) of their peak tolerance for several minutes (Neder et al 2000), more severe disease (FEV1 <45% predicted) are unable to tolerate such high exercise intensities for long periods of time (Maltais et al 1997). Together with peripheral muscle dysfunction, the major factor that limit exercise tolerance in these patients is the development of DH, and the concurrent mechanical constraints on ventilation that contribute importantly to perceived respiratory discomfort (Diaz et al 2000; Puente-Maestu et al 2005). Dynamic hyperventilation is evident even with short exercise bouts in interval training (Vogiatzis et al 2004). In one study, a correlation was found between resting hyperinflation (measured as RV/TLC%) and the increase in endurance time after 8 weeks of leg muscle rehabilitation (Puente-Maestu et al 2003). In another study, IC was found as a significant predictor of the long term effects after a rehabilitation program, but in a multiple logistic regression model, only pressure of carbon dioxide (PaCO2) was identified as predictor for the maintenance of improvement in health-related quality of life over one year (Nishiyama et al 2005).
Survival
Certain variables closely linked to DH (O’Donnell et al 1993, 2001, 2002; Diaz et al 2000; Marin et al 2001) such as exercise capacity (maximal oxygen uptake) (Gerardi et al 1996; Bowen et al 2000; Myers et al 2002; Hiraga et al 2003; Oga et al 2003) or 6 minute walking distance (Pinto-Plata et al 2004), dyspnea (Celli et al 2004), and oxygen desaturation (Nishimura et al 2002; Hiraga et al 2003; Tojo et al 2005) during exercise have been show to be powerful predictors of survival in COPD patients (Table 1). A recent study of 689 COPD patients, with a mean follow up of 34 month, showed that the IC/TLC was an independent risk factor for mortality in subjects with COPD (Casanova et al 2005). Using the criterion of IC/TLC <25% with a mean follow up period of 34 months, the adjusted hazard ratio for death of any cause was 1.97 and 2.04 for death caused by acute respiratory failure (Casanova et al 2005). In another study RV/TLC was also a prognostic factor for survival at 5 years but not independent of age, FEV1, and arterial oxygen pressure at maximal exercise (Tojo et al 2005).
Therapeutic interventions directed to ameliorate dynamic hyperinflation
The treatment of flow limitation and DH has a long history that goes back as far as the 19th century, but the recent recognition of the importance of DH has modified the target physiological variables that we use to evaluate the therapeutic interventions, such as bronchodilators or rehabilitation, and has led to a renewed interest in specific treatments such as the lung volume reduction surgery (LVRS). In this section we will discuss those therapies grouped according their target physiological variable.
Treatments that primarily decrease respiratory rate and increase VT
Pursed-lip breathing
Pursed-lip breathing (PLB) (Barach et al 1995) is aimed to reduce breathing frequency and to diminish the impact of intrinsic PEEP on respiratory muscles. PLB produces a substantial increase in VT along with a reduced ventilatory rate and minute ventilation (Thoman et al 1966; Mueller et al 1970; Bianchi et al 2004). There is a direct relationship between the efficacy of PLB in reducing dyspnea and the effect on respiratory rate (Mueller et al 1970). This technique is able to increase expiratory airways pressure thus inhibiting expiratory airways collapse (Ingram et al 1967). It appears that patients that do not adopt PLB instinctively did not assume it naturally for long periods of time even when properly taught (Tiep et al 1986). In a recent study imposed PLB did not improved 6 minute-walking distance, but improved the rate of dyspnea recovery to basal levels (Garrod et al 2005). In another study, PLB reduced respiratory rate in patients with COPD during exercise on a cycle-ergometer, but the effect of imposed PLB on dyspnea were variable and related to the change that it promoted in the tidal volume and EELV (Spahija et al 2005).
Peripheral muscle training
A number of studies have shown that leg training decreases respiratory rate during exercise (Cassaburi et al 1997; Puente-Maestu et al 2000; Vogiatzis et al 2002; Gigliotti et al 2003; Ruiz de Oña et al 2004), and three previous studies have directly analyzed the impact of leg training on DH at high intensity exercise. In two uncontrolled studies, a reduction of respiratory rate and an increase in IC was seen (Gigliotti et al 2003; Porszasz et al 2005). In another controlled study, the same effect was seen after 8 weeks of leg training on a bike compared with no training in moderate to severe COPD (Puente-Maestu et al 2006). In another study the opposite was observed (Pellegrino 1999). However, this latter study included eight quite unusual COPD subjects (ie, 38 [11] years, FEV1 3.5 (0.5) L and V O2 2.86 (0.6) L min−1) that can not be regarded as a typical population of COPD patients. Arm training also reduced DH during arm exercise in a small uncontrolled study of COPD subjects (Gigliotti et al 2005).
Oxygen
Several observations in nonhypoxemic COPD patients demonstrate the favorable effect of oxygen supplementation during exercise in COPD patients without clinically significant hypoxemia (Woodcock, Gross, Geddes, et al 1981; Dean et al 1992; O’Donnell, Bain, et al 1997). Endurance time increased with supplemental oxygen at several different inhaled concentrations of oxygen both in a small group (10) of severe mildly hypoxemic COPD patients and 7 healthy controls. In both groups oxygen reduced fR, dyspnea, and increased VT, and endurance time in a dose-dependent fashion, but the effects were relatively larger in the COPD patients. In the healthy subjects, differences were only appreciable with FIO2 > 0.5 or more. The improvement in endurance time was correlated with a decrease in EELV (Somfay et al 2001). In a group of 18 severe COPD patients, oxygen reduced the degree of DH during recovery from exercise but did not reduce breathlessness compared with air, which suggests that lung mechanics may play a different role in the genesis of dyspnea during recovery from exercise (Stevenson et al 2004).
Opioids
Opioids have been show to decrease dyspnea during exercise (Woodcock, Gross, Gellert, et al 1981; Light et al 1989), but to our knowledge no study has addressed their effect on DH. One study reported a decrease in fR for a given work-rate, and increases in VT and ventilation were found (Light et al 1996). The reported side-effects of opioids and their tendency to lead to tolerance and addiction preclude their use except in highly specific cases and end-of-life situations. Benzodiazepines do not seem to improve exercise capacity or dyspnea (Haas et al 1993) and have a deleterious effect on inspiratory muscle function, reducing both VT and minute ventilation (Jolly et al 1996).
Treatments that primarily reduce flow limitation
One of the most exciting aspects of the renewed interest in DH is the realization that bronchodilator drugs may significantly improve DH, and thus exercise tolerance (Belman et al 1996; O’Donnell et al 1998), and that these changes may not be detectable by isolated resting pulmonary function test (PFT) measurements like the FEV1 (Hadcroft and Calverley 2001).
Bronchodilators
Several studies have addressed the effect of bronchodilators on lung hyperinflation (Table 2). In 13 COPD patients randomly assigned to receive either inhaled placebo or salbutamol, the bronchodilator caused significant increase in both FEV1 and forced vital capacity (FVC). There was also a significant reduction in the peak exercise EELV/TLC and esophageal inspiratory pressure/peak inspiratory esophageal pressure. Moreover a significant reduction in breathlessness that correlated with changes in end-inspiratory lung volume/TLC was also seen (Belman et al 1996). In a retrospective review of 281 patients with TLC >133% predicted and 676 with TLC between 115% to 133% predicted, 200μg of salbutamol produced a significant reduction of FRC, RV, and increased the IC and FVC. The FEV1 improved in only a minority (around 30%). If lung volume measurements are also considered, the overall bronchodilator response may improve up to 76% of the severely hyperinflated group and up to 62% of the moderately hyperinflated ones. Changes in volumes correlated poorly with changes in maximal airflows. Surprisingly TLC was also slightly reduced (about 2.5%) by bronchodilators suggesting that the changes in airways resistance or the familiarity with the method may have affected the constant volume plethysmographic technique used to measure volumes (Newton et al 2002). Unless salbutamol had produced changes in the ability to generate force by the respiratory muscles, or the elastic properties of the lung, both of which it are unlikely. Ramirez-Venegas and colleagues (1997) found that the use of salmeterol reduced not only dyspnea but improved lung function in patients with COPD. Patients showed an increase in FVC, a reduction in RV and FRC, and no changes in TLC following inhalation of salmeterol. Boni and colleagues (2002) studied 20 COPD, 11 with flow limitation using the negative expiratory pressure before and after the inhalation of 400μg salbutamol. Following salbutamol, IC did not change in non-flow limited patients but increased significantly in the flow-limited ones. Dyspnea decreased in relation to IC at rest even in the absence of a significant improvement in FEV1. Di Marco and colleagues (1993) found that in patients with decreased baseline inspiratory capacities; there was a much greater increase of IC after administration of bronchodilators such as salbutamol, formoterol, salmeterol, and oxitropium. This increase correlated closely with improvement in a sensation of dyspnea. Celli and colleagues (2003) evaluated the long-term effects (4 weeks) of 18 μg/day of tiotropium. Significant similar improvements in the area under the curve of FEV1 and IC and over the curve in FRC were observed, reflecting sustained improvements in hyperinflation. O’Donnell, Fluge, and colleagues (2004) and Maltais and colleagues (2005) conducted a multicentric study on the long-term effects (6 weeks) of 18μg/day of tiotropium. Tiotropium reduced lung hyperinflation indices at rest and during exercise, and improved exercise tolerance 8 h after the inhalation of the drug. Finally O’Donnell, Voduc, and colleagues (2004) studied the effects of 50μg of inhaled salmeterol. After salmeterol versus placebo at rest, IC increased and FRC decreased at a standardized time during exercise. In addition, IC and VT increased and dyspnea decreased. Significant increments in peak ventilation, oxygen uptake, and the duration of the incremental test were also seen. Man and colleagues (2004) studied 16 patients with “irreversible” severe COPD after two weeks of treatment with 50μg of salmeterol twice a day. Salmeterol significantly reduced the transdiaphragmatic pressure-time product, DH, and Borg scores during endurance treadmill walk, however there was no significant change in exercise endurance time.
Table 2.
Summary of trials on BD measuring resting or dynamic hyperinflations an outcome
| Ref | FEV1 (%) | “n”/design | Intervention | Duration | Resting PFT | Resting hyperinflation | Exercise hyperinflation | Exercise dyspnea | Endurance time CLE | Comment |
|---|---|---|---|---|---|---|---|---|---|---|
| Single dose | ||||||||||
| (Belman et al 1996) | 40 (3) | 13 cross-over against placebo | 200μg of salbutamol | Improvement in FEV1 and FVC | Improved | Improved | ||||
| (Newton et al 2002) | 52 (1)//78(1)* | 281 TLC>133% and 676 TLC 113%–133%)//retrospective | 200μg of salbutamol | ~30% improved FEV1 | Reduced FRC RV// | TLC was also reduced by BD. overall sensitivity may improve up to ~66% by measuring changes in lung volumes. | ||||
| (Ramirez-Venegas et al 1997) | 52 (13) | 16 with positive BD test//cross-over against placebo | 50μg of salmeterol | Improvement in FEV1 and FVC | Reduced FRC | lower dyspnea during resistive breathing | ||||
| (Boni et al 2002) | 47 (18) | 20//11 with FL | 400μg of salbutamol | No changes in FEV1 | Improvement in IC only in FL | Improved | Changes in dyspnea correlated with improvements in resting IC | |||
| (Di Marco et al 2993) | 52 (3)* | 20//cross-over against placebo | 200μg of salbutamol//12μg of formoterol//50μg of salmeterol//200μg of oxytropium | Improvement in FEV1 | Increased IC | Fomoterol better than salmeterol and than oxytropium//Those with decrease IC achieved a larger effect | ||||
| Long-term | ||||||||||
| (Celli et al 2003) | 43 (12) | 40/41//placebo controlled | Tiotropium 18μg/d | 4 weeks | Improvement in FEV1, FVC, SVC, | Increased IC and decreased FRC | ||||
| (O’Donnell et al 2004a) | 44 (13) | 96/91//placebo controlled | Tiotropium 18μg/d | 6 weeks | Improvement VC, but not FEV1, | Increased IC and decreased FRC | Improved | Improved | 105 (40)s (21%) >than | |
| (Maltais et al 2005) | 43 (13) | 131/117//placebo controlled | Tiotropium 18μg/d | 6 weeks | Improvement VC, but not FEV1, | Increased IC and decreased FRC | Improved | Improved | 171 (58) s> than placebo | Effects seen at 2.5h still at 8h |
| (O’Donnell2004c) | 42 (3)* | 23//cross-over against placebo | Salmeterol (50μg bid) added to the daily drug regimen. | 2 weeks | Increased FEV1, Improved | Increased IC | Improved | Improved | Increased In peak oxygen uptake and VT at 10w incremental test. | |
| (Man et al 2004) | 32 (4) | 16 “no reversible”//cross-over against placebo | Salmeterol (50μg bid) added to the daily drug regimen. | 2 weeks | No effect on FEV1, FVC, SVC, | Decreased RV/TLC | Improved | Improved | No improvement | Changes in dyspnea correlated with improvements DH and esophageal pressure |
Note: Values are men with standard deviation within parenthesis; except *SEM.
In contrast with the results of Table 2, bronchodilators have shown wide variations in regards to changes in exercise capacity (Liesker et al 2002). Earlier negative studies may have included subjects whose exercise capacity was not ventilatory-limited. In fact, several studies in Table 2 demonstrate that the effects of bronchodilators are larger in those with flow limitation than in those without flow limitation. Flow limitations are a major determinant of exercise capacity (Diaz et al 2000). Alternatively, they may have included a great proportion of patients that were not responsive to bronchodilators (about 1/3 of COPD patients do not improve either FEV1 or IC with bronchodilators) (Newton et al 2002). Third, some of those studies may have used insufficient doses and only a few included long-acting bronchodilators, and in particular, none included tiotropium (Liesker et al 2002). Fourth, most studies included 6 minute walking tests to measure exercise capacity; however, 6 minute walking distance is sensitive to a learning effect. Two training sessions are necessary to eliminate a learning effect in walking tests (Kervio et al 2003; Knox et al 1988). Constant work load tests appears to be more appropriate than other tests, as they allow for placebo-controlled comparisons of symptoms and physiological parameters, including exercise endurance time at a standardized work rate or power output (O’Donnell, Fluge, et al 2004). Cycle exercise endurance testing, combined with measurements of exertional dyspnea, ventilation, and dynamic operating lung volumes, has been shown to be reliable, reproducible, and responsive to the intervention (Oga et al 2000; Puente-Maestu et al 2003; O’Donnell, Fluge, et al 2004).
Heliox
Helium is gas that is less dense and more viscous than air. Its lower density can decrease airway resistance in the absence of any anatomical change. Therefore, the greatest theoretical benefit of heliox would be achieved by decreasing turbulent flow in large airways and at branch points in the tracheobronchial tree.
Heliox is unlikely to be of substantial benefit in adults with asthma. A systematic analysis pooled results from seven trials enrolling nearly 400 patients and found no significant improvement in recovery of pulmonary function in patients with acute asthma who were treated with heliox (Rodrigo et al 2001, 2003). One study examined the effects of heliox (80:20) on gas exchange, breathing pattern, respiratory mechanics, and gas distribution in patients with stable, but severe, COPD (Swidwa et al 1985). Heliox was not associated with significant changes in minute ventilation or breathing pattern, however a 15% reduction in FRC which increased back to baseline after a return to air breathing was observed. On the other hand another small trial found no change in DH among COPD patients (Pecchiari et al 2004). In addition, the high cost and limited availability of heliox make its clinical use more difficult. In another study, researchers used an esophageal balloon in recently extubated patients without significant lung disease to quantify intrathoracic pressure swings and estimate the work of breathing (Jaber et al 2001). Fifteen of 18 patients exhibited a drop in their work of breathing, although gas exchange parameters were unchanged. The patients also reported decreased dyspnea while breathing heliox.
The clinical effects of heliox in the absence of positive pressure ventilation have not been well studied. Fifty normoxic COPD with an acute exacerbations were prospectively randomized in the emergency room to receive either heliox (70:30), or air as the driving gas for updraft nebulization of a mixture of salbutamol and ipratropium bromide The base-line FEV1 was 44% There were no significant differences in the change of FEV1 between the two groups by either the 1 h or 2 h time point. Lung volume measurements were not made, but the improvement in forced expiratory flow over the middle half of the FVC (FEF25%–75%) was significantly greater in the heliox group, the authors considered that this improvement had no clinical significance, but measures of dyspnea or recovery were not provided (deBoisblanc et al 2000). A retrospective review of 81 patients presenting to the emergency department with COPD and hypercarbic respiratory insufficiency found a significant reduction in the rates of intubation (8% vs 50%) and in-hospital mortality (3% vs 24%) in the patients who received heliox as compared with control patients (Gerbeaux et al 2001).
Several trials have compared noninvasive positive pressure ventilation (NPPV) combined with either air or heliox in patients with exacerbations of COPD. In one well-designed trial, patients with acute exacerbations of COPD were treated with low or high pressure NPPV in combination with heliox or oxygen-supplemented air (Jaber et al 2000). Differences in breathing pattern, work of breathing, and gas exchange were measured in nine patients using an esophageal balloon technique. Heliox was not associated with changes in breathing pattern, whereas high pressure NPPV produced significant increases in tidal volume and minute ventilation. Heliox was associated with a reduction in PaCO2 and improvement in all measured indices of respiratory effort and work. The beneficial effects on the measured variables were further increased when high pressure NPPV was combined with heliox, compared with the low pressure/air group. The authors suggest that the addition of heliox to NPPV may allow a larger number of patients to benefit from NPPV. In addition, heliox may allow the use of lower levels of pressure support, which could reduce complications and patient discomfort resulting from high pressures and flow rates (Jaber et al 2000). A crossover study monitored the effects of NPPV plus either heliox (70:30) or oxygen (FiO2 0.30) on gas exchange and dyspnea in 19 patients with severe COPD (Jolliet et al 1999). The use of heliox decreased PaCO2, reduced dyspnea, and favorably changed the breathing pattern of patients. Peak inspiratory flow rates were higher, while inspiratory time and the ratio of inspiratory time to respiratory cycle length were both decreased. All of these findings suggest a reduced work of breathing. A third series of 23 intubated patients with COPD and respiratory failure found that the administration of heliox significantly reduced intrinsic PEEP, trapped lung volume, and peak and mean airway pressures (Tassaux et al 2000). Similar findings were noted in a second small study of 12 patients recovering from acute exacerbations of COPD. In this randomized prospective crossover trial, heliox decreased the resistive work of breathing and intrinsic positive end-expiratory pressure (auto-PEEP) without changing the breathing pattern (Diehl et al 2003).
One study examined the impact of heliox on pulmonary function in ten aging runners with very mild COPD during cardiopulmonary exercise testing. Heliox was associated with an increase in minute ventilation, in the absence of any change in the metabolic cost of breathing (Babb et al 2003). Another work studied 12 patients with severe COPD (FEV1 38[10]% of predicted) comparing heliox (79:21) with air. Exercise endurance increased significantly and peak ventilation time with heliox. This was associated with a significant reduction in lung DH and dyspnea at isotime. The reduction in dyspnea correlated significantly with the increase in IC induced by heliox (Palange et al 2004).
Increasing elastic recoil
Although there are no currently available treatments to return the lung to its normal structure once it has been damaged by the inflammatory process (like COPD), this may indeed be possible in the future using stem cells (Ortiz et al 2003; Suratt et al 2003). Stem cells may indeed improve the compliance characteristics of the lung. However, at this time lung volume-reduction surgery (LVRS; a surgical or bronchoscopic procedure that involves resection or exclusion of the most severely affected regions of diseased lung tissue) in patients with diffuse emphysema, may improve lung function by increasing elastic recoil of the lung, the effective pressure driving maximal expiratory flow airway, and the conductance of the airways by augmenting the radial traction of their alveolar attachments. Hence it may improve flow proportionately at all areas of the lung and secondarily reduce hyperinflation (Brantigan et al 1959; Rogers et al 1968; Fessler and Permutt 1998; Ingenito et al 2001). This surgery was initially described in the late 1950s (Brantigan et al 1959). The persistent air leaks that limited early success have been diminished considerably by the recent surgical advances, which has increased interest in this procedure and led to its greater availability (Wakabayashi et al 1991; Cooper et al 1995; Keenan et al 1996; Hazelrigg et al 1997; Brenner et al 2004).
Several randomized trials have compared LVRS with optimal medical treatment (Geddes et al 2000; Fishman et al 2003; Miller, Berger, et al 2005) and by far the largest of these was the National Emphysema Treatment Trial (NETT) (Fishman et al 2003). NETT enrolled over 1200 patients with severe emphysema who underwent baseline assessment followed by six months of mandatory pulmonary rehabilitation. The patients were then randomly assigned to surgical or continued medical therapy, with plans for three-year follow-up. In this study high risk patients were defined as having: FEV1 < 20% and either diffusing capacity of the lung for carbon monoxide (DLCO) < 20% predicted or homogeneous changes on chest computer tomography (Table 3). The 30-day mortality was 16% in the surgical group compared with no deaths in the medically managed group (NETT 2001). In the remainder of the study, while there was a significant improvement in exercise capacity in the surgical group (the same has been found in another study [Dolmage et al 2004]), there was no difference in the total mortality rate at the end of follow-up with surgical or medical therapy (9% vs 10% per year with medical therapy), however, the 90-day mortality was significantly higher with surgery (5.2% vs 1.5%) (Fishman et al 2003). Only the subset of patients with upper lobe predominant emphysema and low exercise capacity (24%) had a significant reduction in total mortality with surgery (7% vs 15% per year, risk ratio 0.47). In this study, low exercise capacity was defined as less than 40% of the gender–specific predicted work rate (40 W in men and 25 W in women) (Fishman et al 2003).
Table 3.
Subjects likely to benefit for lung volume surgery
| Marked disability after rehabilitation (peak work rate <40% predicted) |
| Quit from smoking at least 6 month before |
| Understanding of risks and benefits |
| Heterogeneous enphysiema |
| Marked hyperinflation |
| DLCO <50% >20% as percent of predicted |
| FEV1 < 35% >20% as percent of predicted |
| Normal ejection fraction |
Abbreviations: DLCO, diffusing capacity of the lung for carbon monoxide; FEV, forced expiratory volume in one second
Recently LVRS has been attempted by bronchoscopically placing one-way valves in airways associated with areas of severe emphysema and hyperexpansion. These valves allow air and secretions to move from alveoli to the central airways, but prevent air from entering the distal airspaces. Over time, this results in collapse of the affected regions. Experience in humans is limited, but one series of 19 patients who underwent unilateral valve placement noted decreased air-trapping and improvement in exercise tolerance one month after the procedure (Hopkinson et al 2005).
LVRS produces less functional improvement than lung transplant (Gaissert et al 1996), but since patients who undergo LVRS are not automatically excluded from receiving a subsequent lung transplant both treatments might be sequentially applied (Nathan et al 2004).
Large bullae which can potentially benefit from surgical resection are uncommon clinically. An important challenge for the clinician is to select the patient for bullectomy who can have the greatest benefit with the lowest morbidity and mortality. The most common indication for bullectomy is severe dyspnea in the setting of a large bulla occupying at least 30%–50% of the hemithorax. Another indication is history of a pneumothorax. The physiologic outcome after surgery is determined largely by the size of the bulla and the severity of the underlying emphysema, and patients with severe generalized emphysema tend to do poorly (Nickoladze 1992). The surgical risk is increased when the FEV1 is less than 40% of predicted, and the presence of severe dyspnea, a markedly reduced FEV1, hypercapnia, or cor pulmonale makes the risk of surgery almost prohibitive (Gunstensen and McCormack 1973).
Relieving the inspiratory threshold load
Pursed-lip breathing
We have reviewed the effects of PLB above. In addition to reducing respiratory rate, it likely reduces dynamic airways compression by generating an extratoracic resistance and thus creates PEEP.
Positive end-expiratory pressure
Intrinsic PEEP is frequent in mechanically ventilated patients with obstructive airways disease. Several studies indicate that in patients with flow limitation by dynamic airway collapse, the application of small amounts of external PEEP can be beneficial since intrinsic PEEP can account for about one-third of the total work of breathing (Coussa et al 1993). Hyperinflation may not be affected when applied PEEP is below 85% of the measured auto-PEEP (Ranieri et al 1993), however not all patients with auto-PEEP and DH have expiratory flow limitation (Armaganidis et al 2000) and care has to be taken to reduce the impact of a narrow diameter or kinked endotracheal tube, inspisated secretions, exhalation/PEEP valves, and asynchrony due to pain or agitation. The incidence of expiratory flow limitation has been reported to be as high as 93% upon initiation of mechanical ventilation, but it is reduced by half over time with therapy (Alvisi et al 2003). It seems to be more likely when patients are supine instead of semirecumbent (Valta et al 1994).
A recent meta-analysis of 7 studies including a total of 65 patients with COPD shows a modest beneficial effect of ventilatory support on exercise tolerance as well (van ‘t Hul et al 2002), probably in part because continuous positive airway pressure (CPAP) unloads inspiratory muscles from the inspiratory threshold load imposed by intrinsic PEEP (Pepe and Marini 1982; Haluszka et al 1990; Petrof et al 1990; Lougheed et al 1995). In severe COPD patients CPAP of 0.5kPa resulted in a significant reduction in dyspnea and an increase in exercise endurance time (O’Donnell, Sanii, Giesbrecht, et al 1988; O’Donnell, Sanii, Younes, et al 1988), however excessive CPAP increases the perception of breathing effort (O’Donnell, Sanii, Giesbrecht, et al 1988) and hence it should be titrated individually. Inspiratory pressure support (IPS) a form of pressure-targeted mechanical ventilation which each breath is patient triggered and supported has been shown to improve exercise tolerance (Keilty et al 1994; Maltais et al 1995; Kyroussis et al 2000; Polkey et al 2000; van’t Hul et al 2004) and reduce lactate production (Polkey et al 2000). Proportional assisted ventilation, a mode of partial ventilatory assistance adapted to the intensity and timing of spontaneous ventilatory pattern by providing inspiratory pressure in proportion to a patient’s spontaneous effort, has been shown also to increase exercise tolerance (Dolmage and Goldstein 1997; Bianchi et al 1998). The role of pressure support in severely limited COPD patients is not yet clear. In a recent double-blind controlled study of 29 patients with moderate-severe COPD and ventilatory limitation during an incremental exercise test, 37 patients were exercised with either IPS 1kPa (19 subjects) versus 0.5kPa (18 subjects) in the control group. Statistically significant differences were found in favor of the IPS in shuttle walking distance, cycle endurance, and reduction in minute ventilation during exercise (van’t Hul et al 2004).
Measuring flow limitation and dynamic hyperinflation
Spirometry
Spirometry is a central parameter in the diagnosis and staging of COPD, yet it is poorly correlated with dyspnea and exercise capacity (Hay et al 1992; Bauerle et al 1998) and has limited individual value to predict the increase in exercise tolerance in patients with severe COPD (Tobin et al 1984; O’Donnell et al 1998), however resting IC seems to be better index of exercise capacity (Diaz et al 2000) and changes in IC are better indicator of the reduction of dyspnea and exercise tolerance (Ramirez-Venegas et al 1997; Hadcroft and Calverley 2001; Boni et al 2002; Celli et al 2003; O’Donnell, Fluge, et al 2004; Stevenson et al 2005), furthermore the use of IC as an adjunct criterion for a bronchodilator test apparently increases the sensitivity to detect functional changes clinically relevant (Newton et al 2002; Parker et al 2005). Although there is no defined criterion to evaluate changes in IC (Pellegrino et al 2005), changes after bronchodilators have been usually larger than 15% (Ramirez-Venegas et al 1997; Hadcroft and Calverley 2001; Boni et al 2002; Celli et al 2003; O’Donnell, Fluge, et al 2004). Other useful indexes of air trapping are FRC, RV, and their relationship with TLC (Diez Herranz 1995), although they are more complex to obtain and not as widely available as spirometry.
Flow volume loops
The conventional method used to detect expiratory flow limitation using tidal breathing was one proposed by Hyatt and Wilcox (1963). It consists of superimposing a flow–volume loop of a tidal breath within a maximum flow–volume curve. Expiratory flow limitation is not present when the patient breathes below the maximal expiratory flow–volume curve (Pride 1999). This method to detect expiratory flow limitation has several methodological deficiencies such as intrathoracic gas compression artefacts (which only can be detected with a constant pressure body plethysmograph (Ingram and Schilder 1966), incorrect alignment of tidal with maximal expiratory flow–volume curve considering the TLC as a fixed reference point, which is not always valid (Younes and Kivinen 1984; D’Angelo et al 1993). Respiratory mechanics and the intrathoracic pressure swinging are different during the tidal and maximal expiratory efforts and exercise may result in changes in airways tone (Beck et al 1994). Another important limitation of the conventional method is that it requires patient cooperation.
The negative expiratory pressure technique
The negative expiratory pressure technique (NEP) method is based on the principle that the increase in pressure caused by NEP should result in increased expiratory flow. By contrast, in flow-limited subjects, application of NEP should not change the expiratory flow (Koulouris et al 1995). For technical details we refer the reader elsewhere. This method does not require FVC maneuvers, collaboration on the part of the patient, or use of a body plethysmograph, and can be used during spontaneously breathing subjects during exercise (Calverley and Koulouris 2005).
Measurement of dynamic hyperinflation
Since TLC remains essentially unaltered during exercise (Stubbing et al 1980; Younes and Kivinen 1984) changes in EELV during exercise can be reliably tracked by serial IC measurements (Figure 5). Exercise IC measurements are reproducible, provided care is taken with their measurement. In one study of 29 patients the variability coefficient was 17% at rest and approximately 20% during exercise with intra-class correlation coefficients of 0.77 and 0.73 respectively (O’Donnell et al 1998). In another study of 15 patient esophageal pressures were found reproducible during IC maneuvers during exercise at different work-rates, the reduction in IC during exercise correlates well with esophageal balloon-derived measurements of dynamic compliance (O’Donnell, Chau, et al 1997). In another study, three methods of measuring IC were tested in 10 severe COPD subjects. IC calculated, after correction of the expiratory part of the signal, as the difference between the mean EELV of the six breaths that preceded the IC prompt and the peak inspiratory volume was found to be the most reproducible method (Dolmage and Goldstein 2002). In an unpublished multicentric study of 463 patients with moderate to severe COPD, the intra-class correlation of exercise IC measurements during serial exercise tests exceeded 0.85 (O’Donnell, He, et al 2004). The extent of the reduction in IC with exercise in COPD is variable. In a population of 105 patients with moderate to severe COPD, IC at end-exercise was reduced by 20% of its already-reduced resting value (O’Donell et al 2001). In another smaller group of 27 severe COPD patients a similar reduction was found at maximum ventilation at the end of high intensity exercise (Puente-Maestu et al 2005). Similar changes were found in severe COPD in 15 severe COPD (Yan et al 1997). However, guidelines for standardization of IC measurement have not yet been issued. Recently a new complex method called optoelectronic plethysmography has been developed for research purposes (Aliverti et al 2004)
Conclusion
Flow limitation and DH are crucial pathophysiological mechanisms in the development of exercise intolerance, dyspnea, and respiratory failure in COPD patients. As the disease advances with progression of symptoms and impairment, the flow limitation and DH proportionally worsens. Several methods of treatment may palliate its impact of flow limitation and DH on the patient, including physical therapy, bronchodilators, ventilatory support, oxygen, heliox, or surgery. Measurement of DH may be done indirectly by spirometry or by more direct approaches that have known limitations or are not widely available. Clinical use is limited by the lack of a standard method to measure DH or flow limitation during exercise.
References
- [ACCP/AACVPR] Pulmonary Rehabilitation Guidelines Panel, American College of Chest Physicians, American Association of Cardiovascular and Pulmonary Rehabilitation. Pulmonary rehabilitation: joint ACCP/AACVRR evidence based guidelines. Chest. 1997;112:1363–96. [PubMed] [Google Scholar]
- Agostoni E, Hyatt RE. Handbook of physiology The respiratory system, sect 3. 1. III. Bethesda, MD: American Physiological Society; 1986. Static behaviour of the respiratory system; pp. 113–130. [Google Scholar]
- Aldrich TK, Shapiro SM, Sherman MS, et al. Alveolar pressure and airway resistance during maximal and submaximal respiratory efforts. Am Rev Respir Dis. 1989;140:899–906. doi: 10.1164/ajrccm/140.4.899. [DOI] [PubMed] [Google Scholar]
- Aliverti A, Stevenson N, Dellaca RL, et al. Regional chest wall volumes during exercise in chronic obstructive pulmonary disease. Thorax. 2004;59:210–16. doi: 10.1136/thorax.2003.011494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvisi V, Romanello A, Badet M, et al. Time course of expiratory flow limitation in COPD patients during acute respiratory failure requiring mechanical ventilation. Chest. 2003;123:1625–32. doi: 10.1378/chest.123.5.1625. [DOI] [PubMed] [Google Scholar]
- Armaganidis A, Stavrakaki-Kallergi K, Koutsoukou A, et al. Intrinsic positive end-expiratory pressure in mechanically ventilated patients with and without tidal expiratory flow limitation. Crit Care Med. 2000;28:3837–42. doi: 10.1097/00003246-200012000-00015. [DOI] [PubMed] [Google Scholar]
- Babb TG, DeLorey DS, Wyrick BL. Ventilatory response to exercise in aged runners breathing He-O2 or inspired CO2. J Appl Physiol. 2003;94:685–93. doi: 10.1152/japplphysiol.00214.2002. [DOI] [PubMed] [Google Scholar]
- Babb TG, Viggiano R, Hurley B, et al. Effect of mild-to-moderate airflow limitation on exercise capacity. J Appl Physiol. 1991;70:223–30. doi: 10.1152/jappl.1991.70.1.223. [DOI] [PubMed] [Google Scholar]
- Barach AL. Breathing exercises in pulmonary emphysema and alied chronic respiratory disease. Arch Phys Med Reahab. 1955;36:379–90. [PubMed] [Google Scholar]
- Bauerle O, Chrusch CA, Younes M. Mechanisms by which COPD affects exercise tolerance. Am J Respir Crit Care Med. 1998;157:57–68. doi: 10.1164/ajrccm.157.1.9609126. [DOI] [PubMed] [Google Scholar]
- Beck KC, Offord KP, Scanlon PD. Bronchoconstriction occurring during exercise in asthmatic patients. Am J Respir Crit Care Med. 1994;149:352–7. doi: 10.1164/ajrccm.149.2.8306029. [DOI] [PubMed] [Google Scholar]
- Beeh KM, Beier J, Kornmann O, et al. Long-term repeatability of induced sputum cells and inflammatory kers in stable, moderately severe COPD. Chest. 2003;123:778–83. doi: 10.1378/chest.123.3.778. [DOI] [PubMed] [Google Scholar]
- Bellee F, Grassino A. Effect of pressure and timing of contraction on human diaphragm fatigue. J Appl Physiol. 1982;53:1190–5. doi: 10.1152/jappl.1982.53.5.1190. [DOI] [PubMed] [Google Scholar]
- Bellee F, Grassino A Force reserve of the diaphragm in patients with chronic obstructive pulmonary disease. J Appl Physiol. 1983;55:8–15. doi: 10.1152/jappl.1983.55.1.8. [DOI] [PubMed] [Google Scholar]
- Belman MJ, Botnick WC, Shin JW. Inhaled bronchodilators reduce dynamic hyperinflation during exercise in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996;153:967–75. doi: 10.1164/ajrccm.153.3.8630581. [DOI] [PubMed] [Google Scholar]
- Bianchi L, Foglio K, Pagani M, et al. Effects of proportional assist ventilation on exercise tolerance in COPD patients with chronic hypercapnia. Eur Resp J. 1998;11:422–7. doi: 10.1183/09031936.98.11020422. [DOI] [PubMed] [Google Scholar]
- Bianchi R, Gigliotti F, Romagnoli I, et al. Chest wall kinematics and breathlessness during pursed-lip breathing in patients with COPD. Chest. 2004;125:459–65. doi: 10.1378/chest.125.2.459. [DOI] [PubMed] [Google Scholar]
- Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis. 1969;99:696–702. doi: 10.1164/arrd.1969.99.5.696. [DOI] [PubMed] [Google Scholar]
- Boni E, Corda L, Franchini D, et al. Volume effect and exertional dyspnoea after bronchodilator in patients with COPD with and without expiratory flow limitation at rest. Thorax. 2002;57:528–32. doi: 10.1136/thorax.57.6.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen JB, Votto JJ, Thrall RS, et al. Functional Status and Survival Following Pulmonary Rehabilitation. Chest. 2000;118:697–703. doi: 10.1378/chest.118.3.697. [DOI] [PubMed] [Google Scholar]
- Brantigan OC, Mueller E, Kress MB. A surgical approach to pulmonary emphysema. Am Rev Respir Dis. 1959;80:194–202. doi: 10.1164/arrd.1959.80.1P2.194. [DOI] [PubMed] [Google Scholar]
- Brenner M, Hanna NM, Mina-Araghi R, et al. Innovative approaches to lung volume reduction for emphysema. Chest. 2004;126:238–48. doi: 10.1378/chest.126.1.238. [DOI] [PubMed] [Google Scholar]
- Calverley PMA, Koulouris NG. Flow limitation and dynamic hyperinflation: key concepts in modern respiratory physiology. Eur Respir J. 2005;25:186–99. doi: 10.1183/09031936.04.00113204. [DOI] [PubMed] [Google Scholar]
- Casaburi R, Gosselink R, Ramer M, et al. American Thoracic Society/European Respiratory Society skeletal muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;159:S1–S40. doi: 10.1164/ajrccm.159.supplement_1.99titlepage. [DOI] [PubMed] [Google Scholar]
- Casaburi R, Porszasz J, Burns MR, et al. Am J Respir Crit Care Med. 1997;155:1541–51. doi: 10.1164/ajrccm.155.5.9154855. [DOI] [PubMed] [Google Scholar]
- Casaburi R. ACSM resource manual for guidelines for exercise testing and prescription. 4th ed. ACSM; 2001. Special considerations for exercise training; pp. 346–52. [Google Scholar]
- Casanova C, Cote C, de Torres JP, et al. Inspiratory-to-total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171:591–7. doi: 10.1164/rccm.200407-867OC. [DOI] [PubMed] [Google Scholar]
- Celli B, ZuWallack R, Wang S, et al. Improvement in resting inspiratory capacity and hyperinflation with tiotropium in COPD patients with increased static lung volumes. Chest. 2003;124:1743–8. doi: 10.1378/chest.124.5.1743. [DOI] [PubMed] [Google Scholar]
- Celli BR, Cote CG, Marin JM, et al. The body mass index, airflow obstruction, dyspnoea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:1005–12. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- Cherniack RM, Hodson A. Compliance of the Chest wall in chronic bronchitis and emphysema. J Appl Physiol. 1963;18:707–11. doi: 10.1152/jappl.1963.18.4.707. [DOI] [PubMed] [Google Scholar]
- Citterio G, Agostoni E, Del Santo A, et al. Decay of inspiratory muscle activity in chronic airway obstruction. J Appl Physiol. 1981;51:1388–97. doi: 10.1152/jappl.1981.51.6.1388. [DOI] [PubMed] [Google Scholar]
- Cooper JD, Trulock EP, Triantafillou AN, et al. Bilateral pneumectomy (volume reduction) for chronic obstructive pulmonary disease. J Thorac Cardiovasc Surg. 1995;109:106–16. doi: 10.1016/S0022-5223(95)70426-4. [DOI] [PubMed] [Google Scholar]
- Cosio MG, Hale KA, Niewoehner DE. Morphologic and morphometric effects of prolonged cigarette smoking on the small airways. Am Rev Respir Dis. 1980;122:265–21. doi: 10.1164/arrd.1980.122.2.265. [DOI] [PubMed] [Google Scholar]
- Coussa ML, Guerin C, Eissa NT, et al. Partitioning of work of breathing in mechanically ventilated COPD patients. J Appl Physiol. 1993;75:1711–19. doi: 10.1152/jappl.1993.75.4.1711. [DOI] [PubMed] [Google Scholar]
- D’Angelo E, Prandi E, Milic-Emili J. Dependence of maximal flow-volume curves on time-course of preceding inspiration. J Appl Physiol. 1993;75:1155–9. doi: 10.1152/jappl.1993.75.3.1155. [DOI] [PubMed] [Google Scholar]
- Dean NC, Brown JK, Himelman RB, et al. Oxygen may improve dyspnoea and endurance in patients with chronic obstructive pulmonary disease and only mild hypoxemia. Am Rev Respir Dis. 1992;146:941–5. doi: 10.1164/ajrccm/146.4.941. [DOI] [PubMed] [Google Scholar]
- deBoisblanc BP, DeBleiux P, Resweber S, et al. Randomized trial of the use of heliox as a driving gas for updraft nebulization of bronchodilators in the emergent treatment of acute exacerbations of chronic obstructive pulmonary disease. Crit Care Med. 2000;28:3177–80. doi: 10.1097/00003246-200009000-00009. [DOI] [PubMed] [Google Scholar]
- Di Marco J, Milic-Emili J, Boveri P, et al. Effect of inhaled bronchodilators on inspiratory capacity and dyspnoea at rest in COPD. Eur Respir J. 2003;21:86–94. doi: 10.1183/09031936.03.00020102. [DOI] [PubMed] [Google Scholar]
- Diaz O, Villafranca C, Ghezzo H, et al. Exercise tolerance in COPD patients with and without tidal expiratory flow limitation at rest. Eur Respir J. 2000;16:269–75. doi: 10.1034/j.1399-3003.2000.16b14.x. [DOI] [PubMed] [Google Scholar]
- Diehl JL, Mercat A, Guerot E, et al. Helium/oxygen mixture reduces the work of breathing at the end of the weaning process in patients with severe chronic obstructive pulmonary disease. Crit Care Med. 2003;31:1415–20. doi: 10.1097/01.CCM.0000059720.79876.B5. [DOI] [PubMed] [Google Scholar]
- Diez Herranz A. RV/TLC% ratio: alternative criteria of normality. Eur Respir J. 1995;8:1812–13. doi: 10.1183/09031936.95.08101812. [DOI] [PubMed] [Google Scholar]
- Dodd DS, Brancatisano T, Engel LA. Chest wall mechanics during exercise in patients with severe chronic air-flow obstruction. Am Rev Respir Dis. 1984;129:33–8. doi: 10.1164/arrd.1984.129.1.33. [DOI] [PubMed] [Google Scholar]
- Dolmage TE, Goldstein RS. Proportional assist ventilation and exercise tolerance in subjects with COPD. Chest. 1997;111:948–54. doi: 10.1378/chest.111.4.948. [DOI] [PubMed] [Google Scholar]
- Dolmage TE, Goldstein RS. Repeatability of inspiratory capacity during incremental exercise in patients with severe COPD. Chest. 2002;121:708–14. doi: 10.1378/chest.121.3.708. [DOI] [PubMed] [Google Scholar]
- Dolmage TE, Waddell TK, Maltais F, et al. The influence of lung volume reduction surgery on exercise in patients with COPD. Eur Respir J. 2004;23:269–74. doi: 10.1183/09031936.03.00068503. [DOI] [PubMed] [Google Scholar]
- Donahoe M, Rogers RM, Wilson DO, et al. Oxygen consumption of the respiratory muscles in normal and in malnourished patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1989;140:385–91. doi: 10.1164/ajrccm/140.2.385. [DOI] [PubMed] [Google Scholar]
- Eltayara L, Becklake MR, Volta CA, et al. Relationship between chronic dyspnoea and expiratory flow limitation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996;154:1726–34. doi: 10.1164/ajrccm.154.6.8970362. [DOI] [PubMed] [Google Scholar]
- Fessler HE, Permutt S. Lung volume reduction surgery and airflow limitation. Am J Respir Crit Care Med. 1998;157:715–22. doi: 10.1164/ajrccm.157.3.9608004. [DOI] [PubMed] [Google Scholar]
- Fishman A, Martinez F, Naunheim K, et al. National Emphysema Treatment Trial Research Group. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med. 2003;348:2059–73. doi: 10.1056/NEJMoa030287. [DOI] [PubMed] [Google Scholar]
- Gaissert HA, Trulock EP, Cooper JD, et al. Comparison of early functional results after volume reduction or lung transplantation for chronic obstructive pulmonary disease. J Thorac Cardiovasc Surg. 1996;111:296–306. doi: 10.1016/s0022-5223(96)70438-5. [DOI] [PubMed] [Google Scholar]
- Gallagher CG. Exercise limitation and clinical exercise testing in chronic obstructive pulmonary disease. Clin Chest Med. 1994;15:305–26. [PubMed] [Google Scholar]
- Garrod R, Dallimore K, Cook J, et al. An evaluation of the acute impact of pursed lips breathing on walking distance in nonspontaneous pursed lips breathing chronic obstructive pulmonary disease patients. Chron Respir Dis. 2005;2:67–72. doi: 10.1191/1479972305cd068oa. [DOI] [PubMed] [Google Scholar]
- Geddes D, Davies M, Koyama H, et al. Effect of lung-volume-reduction surgery in patients with severe emphysema. N Engl J Med. 2000;343:239–45. doi: 10.1056/NEJM200007273430402. [DOI] [PubMed] [Google Scholar]
- Gerardi DA, Lovett L, Benoit-Connors ML, et al. Variables related to increased mortality following out-patient pulmonary rehabilitation. Eur Respir J. 1996;9:431–5. doi: 10.1183/09031936.96.09030431. [DOI] [PubMed] [Google Scholar]
- Gerbeaux P, Gainnier M, Boussuges A, et al. Use of heliox in patients with severe exacerbation of chronic obstructive pulmonary disease. Crit Care Med. 2001;29:2322–4. doi: 10.1097/00003246-200112000-00015. [DOI] [PubMed] [Google Scholar]
- Gigliotti F, Coli C, Bianchi R, et al. Exercise training improves exertional dyspnoea in patients with COPD: evidence of the role of mechanical factors. Chest. 2003;123:1794–802. doi: 10.1378/chest.123.6.1794. [DOI] [PubMed] [Google Scholar]
- Gigliotti F, Coli C, Bianchi R, et al. Arm exercise and hyperinflation in patients with COPD: effect of arm training. Chest. 2005;128:1225–32. doi: 10.1378/chest.128.3.1225. [DOI] [PubMed] [Google Scholar]
- Gottlieb DJ, Stone PJ, Sparrow D, et al. Urinary desmosine excretion in smokers with and without rapid line of lung function: the Normative Aging Study. Am J Respir Crit Care Med. 1996;154:1290–5. doi: 10.1164/ajrccm.154.5.8912738. [DOI] [PubMed] [Google Scholar]
- Green M, Pride MB. Normal respiratory mechanics. In: Scadding JG, Cumming G, Thrubeck WM, editors. Scientific foundations of respiratory medicine. London: William Heinemann Medical books; 1997. pp. 113–29. [Google Scholar]
- Grimby G, Bunn J, Mead J. Relative contribution of rib cage and abdomen to ventilation during exercise. J Appl Physiol. 1968;24:159–66. doi: 10.1152/jappl.1968.24.2.159. [DOI] [PubMed] [Google Scholar]
- Gross D, Ladd HW, Riley EJ, et al. The effect of training on strength and endurance of the diaphragm in quadriplegia. Am J Med. 1980;68:27–35. doi: 10.1016/0002-9343(80)90157-6. [DOI] [PubMed] [Google Scholar]
- Gunstensen J, McCormack RJ. The surgical management of bullous emphysema. J Thorac Cardiovasc Surg. 1973;65:920–5. [PubMed] [Google Scholar]
- Haas F, Salazar-Schichi J, Axen K. Desensitization to dyspnoea in chronc obstructive pulmonary disease. In: Casaburi R, Petty TL, editors. Principles and practice of pulmonary rehabilitation. Philadelphia: WB Saunders Company; 1993. pp. 241–51. [Google Scholar]
- Hadcroft J, Calverley PM. Alternative methods for assessing bronchodilator reversibility in chronic obstructive pulmonary disease. Thorax. 2001;56:713–20. doi: 10.1136/thorax.56.9.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haluszka J, Chartrand DA, Grassino AE, et al. Intrinsic PEEP and arterial PCO2 in stable patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1990;141:1194–7. doi: 10.1164/ajrccm/141.5_Pt_1.1194. [DOI] [PubMed] [Google Scholar]
- Hamilton AL, Killian KJ, Summers E, et al. Symptom intensity and subjective limitation to exercise in patients with cardiorespiratory disorders. Chest. 1996;110:1255–63. doi: 10.1378/chest.110.5.1255. [DOI] [PubMed] [Google Scholar]
- Hay JG, Stone P, Carter J, et al. Bronchodilator reversibility, exercise performance and breathlessness in stable chronic obstructive pulmonary disease. Eur Respir J. 1992;5:659–64. [PubMed] [Google Scholar]
- Hazelrigg SR, Boley TM, Naunheim KS, et al. Effect of bovine pericardial strips on air leak after stapled pulmonary resection. Ann Thorac Surg. 1997;63:1573–5. doi: 10.1016/s0003-4975(97)00126-4. [DOI] [PubMed] [Google Scholar]
- Henke KG, Sharratt M, Pegelow D, et al. Regulation of end-expiratory lung volume during exercise. J Appl Physiol. 1988;64:135–46. doi: 10.1152/jappl.1988.64.1.135. [DOI] [PubMed] [Google Scholar]
- Hiraga T, Maekura R, Okuda Y, et al. Prognostic predictors for survival in patients with COPD using cardiopulmonary exercise testing. Clin Physiol Funct Imaging. 2003;23:324–9. doi: 10.1046/j.1475-0961.2003.00514.x. [DOI] [PubMed] [Google Scholar]
- Hopkinson NS, Toma TP, Hansell DM, et al. Effect of bronchoscopic lung volume reduction on dynamic hyperinflation and exercise in emphysema. Am J Respir Crit Care Med. 2005;171:453–60. doi: 10.1164/rccm.200407-961OC. [DOI] [PubMed] [Google Scholar]
- Hyatt RE, Wilcox RE. The pressure-flow relationships of the intrathoracic airway in man. J Clin Invest. 1963;42:29–39. doi: 10.1172/JCI104693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyatt RE. The interrelationships of pressure, flow, and volume during various respiratory maneuvers in normal and emphysematous subjects. Am Rev Respir Dis. 1961;83:676–83. doi: 10.1164/arrd.1961.83.5.676. [DOI] [PubMed] [Google Scholar]
- Hyatt RE. Expiratory flow limitation. J Appl Physiol. 1983;55:1–8. doi: 10.1152/jappl.1983.55.1.1. [DOI] [PubMed] [Google Scholar]
- Im Hof V, West P, Younes M. Steady-state response of normal subjects to inspiratory resistive load. J Appl Physiol. 1986;60:1471–81. doi: 10.1152/jappl.1986.60.5.1471. [DOI] [PubMed] [Google Scholar]
- Ingenito EP, Loring SH, Moy ML, et al. Interpreting improvement in expiratory flows after lung volume reduction surgery in terms of flow limitation theory. Am J Respir Crit Care Med. 2001;163:1074–80. doi: 10.1164/ajrccm.163.5.2001121. [DOI] [PubMed] [Google Scholar]
- Ingram RH, Jr, Schilder DP. Effect of gas compression on pulmonary pressure, flow, and volume relationship. J Appl Physiol. 1966;21:1821–6. doi: 10.1152/jappl.1966.21.6.1821. [DOI] [PubMed] [Google Scholar]
- Ingram RH, Jr, Schilder DP. Effect of pursed lips expiration on the pulmonary pressure-flow relationship in obstructive lung disease. Am Rev Respir Dis. 1967;96:381–8. doi: 10.1164/arrd.1967.96.3.381. [DOI] [PubMed] [Google Scholar]
- Jaber S, Carlucci A, Boussarsar M, et al. Helium-oxygen in the postextubation period decreases inspiratory effort. Am J Respir Crit Care Med. 2001;164:633–7. doi: 10.1164/ajrccm.164.4.2008027. [DOI] [PubMed] [Google Scholar]
- Jaber S, Fodil R, Carlucci A, et al. Noninvasive ventilation with helium-oxygen in acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161:1191–200. doi: 10.1164/ajrccm.161.4.9904065. [DOI] [PubMed] [Google Scholar]
- Johnson BD, Reddan WG, Seow KC, et al. Mechanical constraints on exercise hyperpnea in a fit aging population. Am Rev Respir Dis. 1991;143:968–77. doi: 10.1164/ajrccm/143.5_Pt_1.968. [DOI] [PubMed] [Google Scholar]
- Jolliet P, Tassaux D, Thouret JM, et al. Beneficial effects of helium: oxygen versus air: oxygen noninvasive pressure support in patients with descompensated chronic obstructive pulmonary disease. Crit Care Med. 1999;27:2422–9. doi: 10.1097/00003246-199911000-00017. [DOI] [PubMed] [Google Scholar]
- Jolly E, Aguirre L, Jorge E, et al. Acute effect of lorazepam on respiratory muscles in stable patients with chronic obstructive pulmonary disease. Medicina (B Aires) 1996;56:472–8. [PubMed] [Google Scholar]
- Keatings VM, Collins PD, Scott DM, et al. Differences in interleukin-8 and tumor necrosis factor-alpha in induced sputum from patients with chronic obstructive pulmonary disease or asthma. Am J Respir Crit Care Med. 1996;153:530–4. doi: 10.1164/ajrccm.153.2.8564092. [DOI] [PubMed] [Google Scholar]
- Keenan RJ, Landreneau RJ, Sciurba FC, et al. Unilateral thoracoscopic surgical approach for diffuse emphysema. J Thorac Cardiovasc Surg. 1996;111:308–15. doi: 10.1016/s0022-5223(96)70439-7. [DOI] [PubMed] [Google Scholar]
- Keilty SE, Ponte J, Fleming TA, et al. Effect of inspiratory pressure support on exercise tolerance and breathlessness in patients with severe stable chronic obstructive pulmonary disease. Thorax. 1994;49:990–6. doi: 10.1136/thx.49.10.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kervio G, Carre F, Ville NS. Reliability and intensity of the six-minute walk test in healthy elderly subjects. Med Sci Sports Exerc. 2003;35:169–74. doi: 10.1097/00005768-200301000-00025. [DOI] [PubMed] [Google Scholar]
- Killian KJ, Jones NL. Mechanisms of exertional dyspnoea. Clin Chest Med. 1994;15:247–57. [PubMed] [Google Scholar]
- Killian KJ, Leblanc P, Tin DH, et al. Exercise capacity and ventilatory, circulatory, and symptom limitation in patients with chronic airflow limitation. Am Rev Respir Dis. 1992;146:935–40. doi: 10.1164/ajrccm/146.4.935. [DOI] [PubMed] [Google Scholar]
- Kim MJ, Druz WS, Danon J, et al. Mechanics of the canine diaphragm. J Appl Physiol. 1976;41:369–82. doi: 10.1152/jappl.1976.41.3.369. [DOI] [PubMed] [Google Scholar]
- Knox AJ, Morrison JF, Muers MF. Reproducibility of walking test results in chronic obstructive airways disease. Thorax. 1998;43:388–92. doi: 10.1136/thx.43.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koulouris NG, Valta P, Lavoie A, et al. A simple method to detect expiratory flow limitation during spontaneous breathing. Eur Respir J. 1995;8:306–13. doi: 10.1183/09031936.95.08020306. [DOI] [PubMed] [Google Scholar]
- Kyroussis D, Polkey MI, Hamnegard CH, et al. Respiratory muscle activity in patients with COPD walking to exhaustion with and without pressure support. Eur Respir J. 2000;15:649–55. doi: 10.1034/j.1399-3003.2000.15d05.x. [DOI] [PubMed] [Google Scholar]
- Leith DE, Bradley M. Ventilatory muscle strength and endurance training. J Appl Physiol. 1976;41:508–16. doi: 10.1152/jappl.1976.41.4.508. [DOI] [PubMed] [Google Scholar]
- Levison H, Cherniack RM. Ventilatory cost of exercise in chronic obstructive pulmonary disease. J Appl Physiol. 1968;25:21–7. doi: 10.1152/jappl.1968.25.1.21. [DOI] [PubMed] [Google Scholar]
- Liesker JJ, Wijkstra PJ, Ten Hacken NH. A systematic review of the effects of bronchodilators on exercise capacity in patients with COPD. Chest. 2002;121:597–608. doi: 10.1378/chest.121.2.597. [DOI] [PubMed] [Google Scholar]
- Light RW, Muro JR, Sato RI, et al. Effects of oral morphine on breathlessness and exercise tolerance in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1989;139:126–33. doi: 10.1164/ajrccm/139.1.126. [DOI] [PubMed] [Google Scholar]
- Light RW, Stansbury DW, Webster JS. Effect of 30 mg of morphine alone or with promethazine or prochlorperazine on the exercise capacity of patients with COPD. Chest. 1996;109:975–81. doi: 10.1378/chest.109.4.975. [DOI] [PubMed] [Google Scholar]
- Liu AN, Mohammed AZ, Rice WR, et al. Perforin-independent CD8(+) T-cell-mediated cytotoxicity of alveolar epithelial cells is preferentially mediated by tumor necrosis factor-alpha: relative insensitivity to Fas ligand. Am J Respir Cell Mol Biol. 1999;20:849–58. doi: 10.1165/ajrcmb.20.5.3585. [DOI] [PubMed] [Google Scholar]
- Lougheed MD, Webb KA, O’Donnell DE. Breathlessness during induced hyperinflation in asthma: role of the inspiratory threshold load. Am J Respir Crit Care Med. 1995;152:911–20. doi: 10.1164/ajrccm.152.3.7663804. [DOI] [PubMed] [Google Scholar]
- Mahler DA, Brent BN, Loke J, et al. Right ventricular performance and central circulatory hemodynamics during upright exercise in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1984;130:722–9. doi: 10.1164/arrd.1984.130.5.722. [DOI] [PubMed] [Google Scholar]
- Maltais F, Hamilton A, Marciniuk D, et al. Improvements in symptom-limited exercise performance over 8 h with once-daily tiotropium in patients with COPD. Chest. 2005;128:1168–78. doi: 10.1378/chest.128.3.1168. [DOI] [PubMed] [Google Scholar]
- Maltais F, LeBlanc P, Jobin J, et al. Intensity of training and physiologic adaptation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997;155:555–61. doi: 10.1164/ajrccm.155.2.9032194. [DOI] [PubMed] [Google Scholar]
- Maltais F, Reissmann H, Gottfried SB. Pressure support reduces inspiratory effort and dyspnoea during exercise in chronic airflow obstruction. Am J Respir Crit Care Med. 1995;151:1027–33. doi: 10.1164/ajrccm/151.4.1027. [DOI] [PubMed] [Google Scholar]
- Man WD, Mustfa N, Nikoletou D, et al. Effect of salmeterol on respiratory muscle activity during exercise in poorly reversible COPD. Thorax. 2005;59:471–6. doi: 10.1136/thx.2003.019620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannix ET, Manfredi F, Farber MO. Elevated O2 cost of ventilation contributes to tissue wasting in COPD. Chest. 1999;115:708–13. doi: 10.1378/chest.115.3.708. [DOI] [PubMed] [Google Scholar]
- Marhsall R. Relationships between stimulus and work of breathing at different lung volumes. J Appl Physiol. 1962;17:917–21. [Google Scholar]
- Marin JM, Carrizo SJ, Gascon M, et al. Inspiratory capacity, dynamic hyperinflation, breathlessness, and exercise performance during the 6-minute-walk test in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163:1395–9. doi: 10.1164/ajrccm.163.6.2003172. [DOI] [PubMed] [Google Scholar]
- McGregor M, Becklake MR. The relationship of oxygen cost of breathing to respiratory mechanical work and respiratory force. J Clin Invest. 1961;40:971–80. doi: 10.1172/JCI104336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead J, Turner JM, Macklem PT, et al. Significance of the relationship between lung recoil and maximum expiratory flow. J Appl Physiol. 1967;22:95–108. doi: 10.1152/jappl.1967.22.1.95. [DOI] [PubMed] [Google Scholar]
- Milic-Emili J. Provocative hypothesis: does mechanical injury the peripheral airways play a role in the genesis of COPD in smokers? J Chron Obstruc Pulm Dis. 2004;1:1–8. doi: 10.1081/COPD-120028700. [DOI] [PubMed] [Google Scholar]
- Miller JD, Berger RL, Malthaner RA, et al. Lung volume reduction surgery vs medical treatment: for patients with advanced emphysema. Chest. 2005;127:1166–77. doi: 10.1378/chest.127.4.1166. [DOI] [PubMed] [Google Scholar]
- Miller JD, Pegelow DF, Jacques AJ, et al. Effects of augmented respiratory muscle pressure production on locomotor limb venous return during calf contraction exercise. J Appl Physiol. 2005;99:1802–15. doi: 10.1152/japplphysiol.00278.2005. [DOI] [PubMed] [Google Scholar]
- Montes de Oca M, Rassulo J, Celli BR. Respiratory muscle and cardiopulmonary function during exercise in very severe COPD. Am J Respir Crit Care Med. 1996;154:1284–9. doi: 10.1164/ajrccm.154.5.8912737. [DOI] [PubMed] [Google Scholar]
- Mueller R, Chanez P, Campbell AM, et al. Different cytokine patterns in bronchial biopsies in asthma and chronic bronchitis. Respir Med. 1996;90:79–85. doi: 10.1016/s0954-6111(96)90202-4. [DOI] [PubMed] [Google Scholar]
- Mueller RE, Petty TL, Filley GF. Ventilation and arterial blood gas changes induced by pursed lips breathing. J Appl Physiol. 1970;28:784–9. doi: 10.1152/jappl.1970.28.6.784. [DOI] [PubMed] [Google Scholar]
- Myers J, Prakash M, Froelicher V, et al. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- Nathan SD, Edwards LB, Barnett SD, et al. Outcomes of COPD lung transplant recipients after lung volume reduction surgery. Chest. 2004;126:1569–74. doi: 10.1378/chest.126.5.1569. [DOI] [PubMed] [Google Scholar]
- Neder A, Jones PW, Nery LE, et al. Determinants of the exercise endurance capacity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;162:497–504. doi: 10.1164/ajrccm.162.2.9907122. [DOI] [PubMed] [Google Scholar]
- [NETT] National Emphysema Treatment Trial Research Group. Patients at high risk of death after lung-volume-reduction surgery. N Engl J Med. 2001;345:1075–83. doi: 10.1056/NEJMoa11798. [DOI] [PubMed] [Google Scholar]
- Newton MF, O’Donnell DE, Forkert L. Response of lung volumes to inhaled salbutamol in a large population of patients with severe hyperinflation. Chest. 2002;121:1042–50. doi: 10.1378/chest.121.4.1042. [DOI] [PubMed] [Google Scholar]
- Nickoladze GD. Functional results of surgery for bullous emphysema. Chest. 1992;101:119–22. doi: 10.1378/chest.101.1.119. [DOI] [PubMed] [Google Scholar]
- Nield M, Arora A, Dracup K, et al. Comparison of breathing patterns during exercise in patients with obstructive and restrictive ventilatory abnormalities. J Rehabil Res Dev. 2003;40:407–14. doi: 10.1682/jrrd.2003.09.0407. [DOI] [PubMed] [Google Scholar]
- Niewoehner DE, Kleinerman J, Rice DB. Pathologic changes in the peripheral airways of young cigarette smokers. N Engl J Med. 1974;291:755–8. doi: 10.1056/NEJM197410102911503. [DOI] [PubMed] [Google Scholar]
- Nishimura K, Izumi T, Tsukino M, et al. Dyspnoea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002;121:1434–40. doi: 10.1378/chest.121.5.1434. [DOI] [PubMed] [Google Scholar]
- Nishiyama O, Taniguchi H, Kondoh Y, et al. Factors in maintaining long-term improvements in health-related quality of life after pulmonary rehabilitation for COPD. Qual Life Res. 2005;14:2315–21. doi: 10.1007/s11136-005-7710-y. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, Chau LKL, Bertley JC, et al. Qualitative aspects of exertional breathlessness in chronic airflow limitation: pathophysiologic mechanisms. Am J Respir Crit Care Med. 1997;155:109–15. doi: 10.1164/ajrccm.155.1.9001298. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, He Z, Lam M, et al. Reproducibility of measurements of inspiratory capacity, dyspnoea intensity and exercise endurance in multicentre trials in COPD. Eur Respir J. 2004;24:323s. [Google Scholar]
- O’Donnell DE, Revill S, Webb KA. Dynamic hyperinflation and exercise intolerance in COPD. Am J Respir Crit Care Med. 2001;164:770–7. doi: 10.1164/ajrccm.164.5.2012122. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, Webb KA. Chapter 18: Exercise. In: Calverley P, MacNee W, Rennard S, et al., editors. Chronic obstructive lung disease. 2nd ed. London: Edward Arnold Ltd; 2003. pp. 243–65. [Google Scholar]
- O’Donnell CE, Fluge T, Gerken F, et al. Effects of tiotropium on lung hyperinflation, dyspnoea and exercise tolerance in COPD. Eur Respir J. 2004;23:832–40. doi: 10.1183/09031936.04.00116004. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, Bain DJ, Webb KA. Factors contributing to relief of exertional breathlessness during hyperoxia in chronic airflow limitation. Am J Respir Crit Care Med. 1997;155:530–5. doi: 10.1164/ajrccm.155.2.9032190. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, D’Arsigny C, Fitzpatrick M, et al. Exercise hypercapnia in advanced chronic obstructive pulmonary disease. The role of lung hyperinflation. Am J Respir Crit Care Med. 2002;166:663–8. doi: 10.1164/rccm.2201003. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, Lam M, Webb KA. Measurement of symptoms, lung hyperinflation, and endurance during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158:1557–65. doi: 10.1164/ajrccm.158.5.9804004. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, Sanii R, Giesbrecht G, et al. Effect of continuous positive airway pressure on respiratory sensation in patients with chronic obstructive pulmonary disease during submaximal exercise. Am Rev Respir Dis. 1988;138:1185–91. doi: 10.1164/ajrccm/138.5.1185. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, Sanii R, Younes M. Improvement in exercise endurance in patients with chronic airflow. Limitation using continuous positive airway pressure. Am Rev Respir Dis. 1988;138:1510–14. doi: 10.1164/ajrccm/138.6.1510. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, Voduc N, Fitzpatrick M, et al. Effect of salmeterol on the ventilatory response to exercise in chronic obstructive pulmonary disease. Eur Respir J. 2004;24:86–94. doi: 10.1183/09031936.04.00072703. [DOI] [PubMed] [Google Scholar]
- O’Donnell DE, Webb KA. Exertional breathlessness in patients with chronic airflow limitation. The role of lung hyperinflation. Am Rev Respir Dis. 1993;148:1351–7. doi: 10.1164/ajrccm/148.5.1351. [DOI] [PubMed] [Google Scholar]
- Oga K, Nishimura K, Tsukino M, et al. The effects of oxitropium bromide on exercise performance in patients with stable chronic obstructive pulmonary disease. a comparison of three different exercise tests. Am J Respir Crit Care Med. 2000;161:1897–901. doi: 10.1164/ajrccm.161.6.9905045. [DOI] [PubMed] [Google Scholar]
- Oga T, Nishimura K, Tsukino M, et al. Relationship between different indices of exercise capacity and clinical measures in patients with chronic obstructive pulmonary disease. Heart Lung. 2002;31:374–81. doi: 10.1067/mhl.2002.127941. [DOI] [PubMed] [Google Scholar]
- Oga T, Nishimura K, Tsukino M, et al. Analysis of factors related to mortality in chronic obstructive pulmonary disease: role of exercise capacity and health status. Am J Respir Crit Care Med. 2003;167:544–49. doi: 10.1164/rccm.200206-583OC. [DOI] [PubMed] [Google Scholar]
- Ortiz LA, Gambelli F, McBride C, et al. Mesenchymal stem cell engraftment in lung is enhanced in response to bleomycin exposure and ameliorates its fibrotic effects. Proc Natl Acad Sci U S A. 2003;100:8407–11. doi: 10.1073/pnas.1432929100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oswald-Mammosser M, Apprill M, Bachez P, et al. Pulmonary hemodynamics in chronic obstructive pulmonary disease of the emphysematous type. Respiration. 1991;58:304–10. doi: 10.1159/000195950. [DOI] [PubMed] [Google Scholar]
- Oswald-Mammosser M, Kessler R, Massard G, et al. Effect of lung volume reduction surgery on gas exchange and pulmonary hemodynamics at rest and during exercise. Am J Respir Crit Care Med. 1998;158:1020–5. doi: 10.1164/ajrccm.158.4.9710057. [DOI] [PubMed] [Google Scholar]
- Palange P, Valli G, Onorati P, et al. Effect of heliox on lung dynamic hyperinflation, dyspnea, and exercise endurance capacity in COPD patients. J Appl Physiol. 2004;97:1637. doi: 10.1152/japplphysiol.01207.2003. [DOI] [PubMed] [Google Scholar]
- Parker M, Voduc N, Aaron SD, et al. Physiological changes during symptom recovery from moderate exacerbations of COPD. Eur Respir J. 2005;26:420–8. doi: 10.1183/09031936.05.00136304. [DOI] [PubMed] [Google Scholar]
- Pauwels RA, Buist AS, Calverley PMA, et al. Am J Respir Crit Care Med. 2001;163:1256–76. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- Pecchiari M, Pelucchi A, D’Angelo E, et al. Effect of heliox breathing on dynamic hyperinflation in COPD patients. Chest. 2004;125:2075–82. doi: 10.1378/chest.125.6.2075. [DOI] [PubMed] [Google Scholar]
- Peinado VI, Barbera JA, Abate P, et al. Inflammatory reaction in pulmonary muscular arteries of patients with mild chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;159:1605–11. doi: 10.1164/ajrccm.159.5.9807059. [DOI] [PubMed] [Google Scholar]
- Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–68. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- Pellegrino R, Villosio C, Milanese U, et al. Breathing during exercise in subjects mild-to-moderate airflow obstruction: effects of physical training. J Appl Physiol. 1999:1697–704. doi: 10.1152/jappl.1999.87.5.1697. [DOI] [PubMed] [Google Scholar]
- Pepe PE, Marini JJ. Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction: the auto-PEEP effect. Am Rev Respir Dis. 1982;126:166–70. doi: 10.1164/arrd.1982.126.1.166. [DOI] [PubMed] [Google Scholar]
- Pesci A, Balbi B, Majori M, et al. Inflammatory cells and mediators in bronchial lavage of patients with chronic obstructive pulmonary disease. Eur Respir J. 1998;12:380–6. doi: 10.1183/09031936.98.12020380. [DOI] [PubMed] [Google Scholar]
- Peto R, Speizer FE, Cochrane AL, et al. The relevance in adults of airflow obstruction, but not of mucous hypersecretion, to mortality from chronic lung disease. Am Rev Respir Dis. 1983;128:491–500. doi: 10.1164/arrd.1983.128.3.491. [DOI] [PubMed] [Google Scholar]
- Petrof BJ, Calderini E, Gottfried SB. Effect of CPAP on respiratory effort and dyspnoea during exercise in severe COPD. J Appl Physiol. 1990;69:179–88. doi: 10.1152/jappl.1990.69.1.179. [DOI] [PubMed] [Google Scholar]
- Pinto-Plata VM, Cote C, Cabral H, et al. The 6-min walk distance: change over time and value as a predictor of survival in severe COPD. Eur Respir J. 2004;23:28–33. doi: 10.1183/09031936.03.00034603. [DOI] [PubMed] [Google Scholar]
- Polkey MI, Hamnegard CH, Hughes PD. Influence of acute lung volume change on contractile properties of human diaphragm. J Appl Physiol. 1998;85:1322–8. doi: 10.1152/jappl.1998.85.4.1322. [DOI] [PubMed] [Google Scholar]
- Polkey MI, Hawkins P, Kyroussis D, et al. Inspiratory pressure support prolongs exercise induced lactataemia in severe COPD. Thorax. 2000;55:547–9. doi: 10.1136/thorax.55.7.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poon CS, Younes M, Gallagher CG. Effects of expiratory resistive load on respiratory motor output in conscious humans. J Appl Physiol. 1987;63:1837–45. doi: 10.1152/jappl.1987.63.5.1837. [DOI] [PubMed] [Google Scholar]
- Porszasz J, Emtner M, Goto S, et al. Exercise training decreases ventilatory requirements and exercise-induced hyperinflation at sub-maximal intensities in patients with COPD. Chest. 2005;128:2025–34. doi: 10.1378/chest.128.4.2025. [DOI] [PubMed] [Google Scholar]
- Potter WA, Olafsson S, Hyatt RE. Ventilatory mechanics and expiratory flow limitation during exercise in patients with obstructive lung disease. J Clin Invest. 1971;50:910–19. doi: 10.1172/JCI106563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pride NB, Green M. Abnormalities of respiratory mechanics. In: Scadding JG, Cumming G, Thrubeck WM, editors. Scientific foundations of respiratory medicine. London: William Heinemann Medical Bks; 1997. pp. 669–88. [Google Scholar]
- Pride NB, Macklem PT. Lung mechanics in disease. In: Fishman AP, editor. Handbook of physiology, Section 3, Volume III, Part 2: The respiratory system. Bethesda MD: American Physiological Society; 1986. pp. 659–92. [Google Scholar]
- Pride NB. Tests of forced expiration and inspiration. In: Hughes JMB, Pride NB, editors. Lung function tests: physiological principles and clinical applications. London: WB Saunders; 1999. pp. 3–25. [Google Scholar]
- Puente-Maestu L, García J, Martínez-Abad Y, et al. Dyspnoea, ventilatory pattern, and changes in dynamic hyperinflation related to the intensity of constant work rate exercise in COPD. Chest. 2005;128:651–56. doi: 10.1378/chest.128.2.651. [DOI] [PubMed] [Google Scholar]
- Puente-Maestu L, Martínez Y, Pedraza F, et al. A controlled trial of the effects of leg training on breathing pattern and dynamic hyperinflation in severe COPD. Lung. 2006;184:159–67. doi: 10.1007/s00408-005-2576-x. [DOI] [PubMed] [Google Scholar]
- Puente-Maestu L, SantaCruz A, Vargas T, et al. Effects of training on the tolerance to high-intensity exercise in patients with severe COPD. Respiration. 2003;70:367–70. doi: 10.1159/000072899. [DOI] [PubMed] [Google Scholar]
- Puente-Maestu L, Sánz ML, Sánz P, et al. Comparison of effects of supervised versus self-monitored training programs in patients with chronic obstructive pulmonary disease. Eur Respir J. 2000;15:517–25. doi: 10.1034/j.1399-3003.2000.15.15.x. [DOI] [PubMed] [Google Scholar]
- Ramirez-Venegas A, Ward J, Lentine T, et al. Salmeterol reduces dyspnoea and improves lung function in patients with COPD. Chest. 1997;112:336–40. doi: 10.1378/chest.112.2.336. [DOI] [PubMed] [Google Scholar]
- Ranieri VM, Dambrosio M, Brienza N. Intrinsic PEEP and cardiopulmonary interaction in patients with COPD and acute ventilatory failure. Eur Respir J. 1996;9:1283–92. doi: 10.1183/09031936.96.09061283. [DOI] [PubMed] [Google Scholar]
- Ranieri VM, Giuliani R, Cinnella G, et al. Physiologic effects of positive end-expiratory pressure in patients with chronic obstructive pulmonary disease during acute ventilatory failure and controlled mechanical ventilation. Am Rev Respir Dis. 1993;147:5–13. doi: 10.1164/ajrccm/147.1.5. [DOI] [PubMed] [Google Scholar]
- Rodrigo G, Rodrigo C, Pollack C, et al. Helium-oxygen mixture for nonintubated acute asthma patients (Cochrane Review) Cochrane Database Syst Rev. 2001;1:CD002884. doi: 10.1002/14651858.CD002884. [DOI] [PubMed] [Google Scholar]
- Rodrigo GJ, Rodrigo C, Pollack CV, et al. Use of helium-oxygen mixtures in the treatment of acute asthma: a systematic review. Chest. 2003;123:891–6. doi: 10.1378/chest.123.3.891. [DOI] [PubMed] [Google Scholar]
- Rogers RM, DuBois AB, Blakemore WS. Effect of removal of bullae on airway conductance and conductance volume ratios. J Clin Invest. 1968;47:2569–79. doi: 10.1172/JCI105939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi A, Ganassini A, Polese G, et al. Pulmonary hyperinflation and ventilator-dependent patients. Eur Respir J. 1997;10:1663–74. doi: 10.1183/09031936.97.10071663. [DOI] [PubMed] [Google Scholar]
- Roussos C, Macklem PT. The respiratory muscles. N Engl J Med. 1982;307:786–97. doi: 10.1056/NEJM198209233071304. [DOI] [PubMed] [Google Scholar]
- Ruiz de Oña Lacasta JM, Garcia de Pedro J, Puente-Maestu L, et al. Effects of muscle training on breathing pattern in patients with severe chronic obstructive pulmonary disease. Arch Bronconeumol. 2004;40:20–3. [PubMed] [Google Scholar]
- Saetta M, Baraldo S, Corbino L, et al. Am J Respir Crit Care Med. 1999;160:711–17. doi: 10.1164/ajrccm.160.2.9812020. [DOI] [PubMed] [Google Scholar]
- Saetta M, Turato G, Maestrelli P, et al. Cellular and structural bases of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163:1304–9. doi: 10.1164/ajrccm.163.6.2009116. [DOI] [PubMed] [Google Scholar]
- Saksena FB, Burrows B. Thoracic compliance in chronic obstructive lung disease. J Lab Clin Med. 1966;68:427–32. [PubMed] [Google Scholar]
- Salvi S, Blomberg A, Rudell B, et al. Acute inflammatory responses in the airways and peripheral blood after short-term exposure to diesel exhaust in healthy human volunteers. Am J Respir Crit Care Med. 1999;159:702–9. doi: 10.1164/ajrccm.159.3.9709083. [DOI] [PubMed] [Google Scholar]
- Schumaker GL, Epstein SK. Managing acute respiratory failure during exacerbation of chronic obstructive pulmonary disease. Respir Care. 2004;49:766–82. [PubMed] [Google Scholar]
- Shapiro SD, Senior RM. Matrix metalloproteinases: matrix degradation and more. Am J Respir Cell Mol Biol. 1999;20:1100–2. doi: 10.1165/ajrcmb.20.6.f151. [DOI] [PubMed] [Google Scholar]
- Sharp JT, Van Lith P, Vej Nughprayoon C, et al. The thorax in chronic obstructive lung disease. Am J Med. 1968;44:39–46. [Google Scholar]
- Shindoh C, Hida W, Kikuchi Y, et al. Oxygen consumption of respiratory muscles in patients with COPD. Chest. 1994;105:790–7. doi: 10.1378/chest.105.3.790. [DOI] [PubMed] [Google Scholar]
- Similowski T, Yan S, Gauthier AP, et al. Contractile properties of the human diaphragm during chronic hyperinflation. N Engl J Med. 1991;325:917–23. doi: 10.1056/NEJM199109263251304. [DOI] [PubMed] [Google Scholar]
- Somfay A, Porszasz J, Lee SM, et al. Dose-response effect of oxygen on hyperinflation and exercise endurance in nonhypoxaemic COPD patients. Eur Respir J. 2001;18:77–84. doi: 10.1183/09031936.01.00082201. [DOI] [PubMed] [Google Scholar]
- Spahija J, de Marchie M, Grassino A. Effects of imposed pursed-lips breathing on respiratory mechanics and dyspnoea at rest and during exercise in COPD. Chest. 2005;128:640–50. doi: 10.1378/chest.128.2.640. [DOI] [PubMed] [Google Scholar]
- Stevenson NJ, Calverley PM. Effect of oxygen on recovery from maximal exercise in patients with chronic obstructive pulmonary disease. Thorax. 2004;59:668–72. doi: 10.1136/thx.2003.014209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson NJ, Walker PP, Costello RW, et al. Lung mechanics and dyspnoea during exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;172:1510–16. doi: 10.1164/rccm.200504-595OC. [DOI] [PubMed] [Google Scholar]
- Stockley RA. Neutrophils and protease/antiprotease imbalance. Am J Respir Crit Care Med. 1999;160:S49–S52. doi: 10.1164/ajrccm.160.supplement_1.13. [DOI] [PubMed] [Google Scholar]
- Stocks J, Quanjer PH. Reference values for residual volume, functional residual capacity and total lung capacity. ATS Workshop on Lung Volume Measurements. Official Statement of the European Respiratory Society. Eur Respir J. 1995;8:492–506. doi: 10.1183/09031936.95.08030492. [DOI] [PubMed] [Google Scholar]
- Stubbing DG, Pengelly LD, Morse JL, et al. Pulmonary mechanics during exercise in normal males. J Appl Physiol. 1980;49:506–10. doi: 10.1152/jappl.1980.49.3.506. [DOI] [PubMed] [Google Scholar]
- Suratt BT, Cool CD, Serls AE, et al. Human pulmonary chimerism after hematopoietic stem cell transplantation. Am J Respir Crit Care Med. 2003;168:318–22. doi: 10.1164/rccm.200301-145OC. [DOI] [PubMed] [Google Scholar]
- Swidwa DM, Montenegro HD, Goldman MD, et al. Helium-oxygen breathing in severe chronic obstructive pulmonary disease. Chest. 1985;87:790–5. doi: 10.1378/chest.87.6.790. [DOI] [PubMed] [Google Scholar]
- Takayama T, Shindoh C, Kurokawa Y, et al. Effects of lung volume reduction surgery for emphysema on oxygen cost of breathing. Chest. 2003;123:1847–52. doi: 10.1378/chest.123.6.1847. [DOI] [PubMed] [Google Scholar]
- Tassaux D, Jolliet P, Roeseler J, et al. Effects of helium-oxygen on intrinsic positive end-expiratory pressure in intubated and mechanically ventilated patients with severe chronic obstructive pulmonary disease. Crit Care Med. 2000;28:2721–8. doi: 10.1097/00003246-200008000-00006. [DOI] [PubMed] [Google Scholar]
- Thoman RL, Stoker GL, Ross JC. The efficacy of pursed-lips breathing in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1966;93:100–6. doi: 10.1164/arrd.1966.93.1.100. [DOI] [PubMed] [Google Scholar]
- Thurlbeck W. Pathology of chronic airflow obstruction. In: Cherniack N, editor. Chronic obstructive pulmonary disease. Philadelphia: WB Saunders; 1991. pp. 3–20. [Google Scholar]
- Thurlbeck WM. Chronic airflow obstruction. Correlation of structure and function. In: Petty TL, editor. Chronic obstructive pulmonary disease. New York: Marcel Dekker; 1985. pp. 129–204. [Google Scholar]
- Tiep BL, Burns M, Kao D, et al. Pursed lips breathing training using ear oximetry. Chest. 1986;90:218–21. doi: 10.1378/chest.90.2.218. [DOI] [PubMed] [Google Scholar]
- Tobin MJ, Hughes JA, Hutchison DC. Effects of ipratropium bromide and fenoterol aerosols on exercise tolerance. Eur J Respir Dis. 1984;65:441–6. [PubMed] [Google Scholar]
- Tojo N, Ichioka M, Chida M, et al. Pulmonary exercise testing predicts prognosis in patients with chronic obstructive pulmonary disease. Intern Med. 2005;44:20–5. doi: 10.2169/internalmedicine.44.20. [DOI] [PubMed] [Google Scholar]
- Valta P, Corbeil C, Lavoie A, et al. Detection of expiratory flow limitation during mechanical ventilation. Am J Respir Crit Care Med. 1994;150:1311–17. doi: 10.1164/ajrccm.150.5.7952558. [DOI] [PubMed] [Google Scholar]
- van’t Hul AJ, Kwakkel G, Gosselink R. The acute effects of non-invasive ventilatory support during exercise on exercise endurance and dyspnoea in patients with COPD: a systematic review. J Cardiopulm Rehabil. 2002;22:290–7. doi: 10.1097/00008483-200207000-00013. [DOI] [PubMed] [Google Scholar]
- van’t Hul A, Gosselink R, Hollander P, et al. Acute effects of inspiratory pressure support during exercise in patients with COPD. Eur Respir J. 2004;23:34–40. doi: 10.1183/09031936.03.00016903. [DOI] [PubMed] [Google Scholar]
- Vestbo J, Prescott E, Lange Pl the Copenhagen City Heart Study Group. Association of chronic mucus hypersecretion with FEV1 line and chronic obstructive pulmonary disease morbidity. Am J Respir Crit Care Med. 1996;153:1530–5. doi: 10.1164/ajrccm.153.5.8630597. [DOI] [PubMed] [Google Scholar]
- Vogiatzis I, Georgiadou O, Golemati S, et al. Patterns of dynamic hyperinflation during exercise and recovery in patients with severe chronic obstructive pulmonary disease. Thorax. 2005;60:723–9. doi: 10.1136/thx.2004.039115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogiatzis I, Nanas S, Kastanakis E, et al. Dynamic hyperinflation and tolerance to interval exercise in patients with advanced COPD. Eur Respir J. 2004;24:385–90. doi: 10.1183/09031936.04.00128903. [DOI] [PubMed] [Google Scholar]
- Vogiatzis I, Nanas S, Roussos C. Interval training as an alternative modality to continuous exercise in patients with COPD. Eur Respir J. 2002;20:12–19. doi: 10.1183/09031936.02.01152001. [DOI] [PubMed] [Google Scholar]
- Von Essen SG, O’Neill DP, McGranaghan S, et al. Neutrophilic respiratory tract inflammation and peripheral blood neutrophilia after grain sorghum dust extract challenge. Chest. 1995;108:1425–33. doi: 10.1378/chest.108.5.1425. [DOI] [PubMed] [Google Scholar]
- Wakabayashi A, Brenner M, Kayaleh RA, et al. Thoracoscopic carbon dioxide laser treatment of bullous emphysema. Lancet. 1991;337:881–3. doi: 10.1016/0140-6736(91)90206-5. [DOI] [PubMed] [Google Scholar]
- Woodcock AA, Gross ER, Geddes DM. Oxygen relieves breathlessness in “pink puffers”. Lancet. 1981;i:907–9. doi: 10.1016/s0140-6736(81)91612-3. [DOI] [PubMed] [Google Scholar]
- Woodcock AA, Gross ER, Gellert A, et al. Effects of dihydrocodeine, alcohol, and caffeine on breathlessness and exercise tolerance in patients with chronic obstructive lung disease and normal blood gases. N Engl J Med. 1981;305:1611–16. doi: 10.1056/NEJM198112313052703. [DOI] [PubMed] [Google Scholar]
- Yamamoto C, Yoneda T, Yoshikawa M, et al. Airway inflammation in COPD assessed by sputum levels of interleukin-8. Chest. 1997;112:505–10. doi: 10.1378/chest.112.2.505. [DOI] [PubMed] [Google Scholar]
- Yan S, Kaminski D, Sliwinski P. Reliability of inspiratory capacity for estimating end-expiratory lung volume changes during exercise in patients with chronic obstructive pulmonary disease. Am J Resp Crit Care Med. 1997;156:55–9. doi: 10.1164/ajrccm.156.1.9608113. [DOI] [PubMed] [Google Scholar]
- Younes M, Kivinen G. Respiratory mechanics and breathing pattern during and following maximal exercise. J Appl Physiol. 1984;57:1773–82. doi: 10.1152/jappl.1984.57.6.1773. [DOI] [PubMed] [Google Scholar]
- Younes M, Riddle W. A model for the relation between respiratory neural and mechanical outputs. I. Theory. J Appl Physiol. 1981;51:963–78. doi: 10.1152/jappl.1981.51.4.963. [DOI] [PubMed] [Google Scholar]
- Younes M. Determinants of thoracic excursion during exercise. In: Whipp BJ, Wasserman K, editors. Exercise pulmonary physiology and physiopathology. New York: Marcel Dekker; 1991. pp. 1–65. [Google Scholar]