Abstract
Background
The majority of Americans die in institutions although most prefer to die at home. States vary greatly in their proportion of home deaths. Although individuals’ circumstances largely determine where they die, health policies may affect the range of options available to them.
Objective
To examine whether states’ spending on home- and community-based services (HCBS) affects place of death, taking into consideration county health care resources and individuals’ family, sociodemographic, and health factors.
Methods
Using exit interview data from respondents in the Health and Retirement Study born in 1923 or earlier who died between 1993 and 2002 (N = 3362), we conducted discrete-time survival analysis of the risk of end-of-life nursing home relocation to examine whether states’ HCBS spending would delay or prevent end-of-life nursing home admission. Then we ran logistic regression analysis to investigate the HCBS effects on place of death separately for those who relocated to a nursing home and those who remained in the community.
Results
Living in a state with higher HCBS spending was associated with lower risk of end-of-life nursing home relocation, especially among people who had Medicaid. However, state HCBS support was not directly associated with place of death.
Conclusions
States’ generosity for HCBS increases the chance of dying at home via lowering the risk of end-of-life nursing home relocation. State-to-state variation in HCBS spending may partly explain variation in home deaths. Our findings add to the emerging encouraging evidence for continued efforts to enhance support for HCBS.
Keywords: long-term care, elderly, state policy, nursing home admission, end-of-life
Most Americans prefer to die at home,1,2 but less than a quarter actually do.3 The majority die in hospitals or nursing homes. The proportion of hospital deaths declined from approximately 54% to 41% during the 1990s, but the proportion of nursing home deaths increased as much as that of home deaths.1 Nursing home deaths are particularly common among the oldest old: one-third of decedents aged 75 and older died in a nursing home in 2001.4 Where elderly persons spend their last stage of life has important implications for their own well-being and that of their family5 as well as the level and distribution of health care expenditures across various sources. People aged 65 and older consume more than one-third of personal health care spending, largely for inpatient services primarily funded by Medicare and for nursing home facility services, the largest portion of which is financed by Medicaid.6,7 Close to a quarter of medical expenditures for the elderly occur in the last year of life in the United States.8
Although individuals’ circumstances such as their health, family, social, and economic factors may largely determine where they die, health policies may affect the range of options available to individuals. Indeed, the proportion of home deaths varied more than 3-fold across states in 2001.3 Such large state-to-state variation is not likely to be explained away by between-state variation in residents’ characteristics. We suspect state-level factors play a role, but previous studies provide little information on this issue. Studies of place of death typically use clinical or population-based samples from local areas, which are inappropriate for cross-state investigation. Even with the use of a national sample, confidentiality concerns have hindered access to data on respondents’ addresses, hampering research on statelevel factors.9,10
As major players in long-term care (LTC) policies, states vary greatly in their support of home- and community-based services (HCBS).11,12 These services including personal assistance with activities of daily living, day care, transportation, and meals-on-wheels, help seniors avoid institutionalization and remain in the community. If those services function as intended, we expect that living in a state with more HCBS enhances the chance of living in the community at the end of life and eventually dying at home. However, HCBS, consisting mostly of nonmedical custodial care, may not be effective in preventing end-of-life hospitalization triggered by medical needs. Furthermore, recent state-level efforts to enhance HCBS, funded mainly by Medicaid, do not support palliative care that would prevent institutional deaths.13 Thus we hypothesize that living in a state with higher HCBS support would delay or prevent entering a nursing home as one’s end-of-life residence, especially among seniors with Medicaid, but it may have limited or no impact on whether one dies in a hospital or in one’s residence.
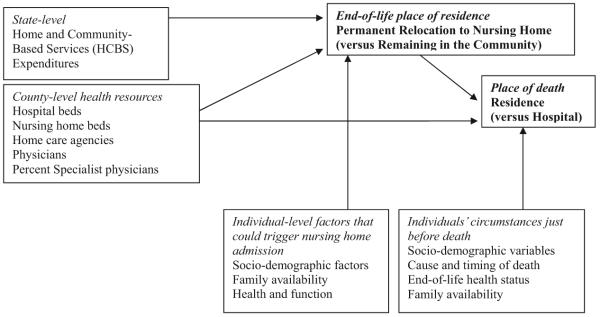
To test this hypothesis, we propose a multilevel conceptual framework involving 2 end-of-life transitions (relocation to a nursing home and death) (Fig. 1). Unlike previous studies that assume that place of death is determined at the time of death, we assume that where people die involves 2 independent decisions, first whether to relocate to a nursing home as one’s end-of-life “permanent” residence, and second where to die. In addition to person-level determinants of place of death examined in previous studies, we considered multilevel factors (eg, family care availability, local LTC resource availability, and states’ HCBS support). To capture the 2 transitions and the effect of changing characteristics of states and individuals that may prompt those 2 transitions, which may be days or years apart, we used 10-year longitudinal data. As described below, we conducted 2 separate sets of multivariate analysis, one for “permanent” nursing home admission and the other for “place of death.” The second “place of death” decision, in many practical respects, is contingent on the first “place of residence” decision,8,14 and thus we examined “place of death” separately for those who relocated to a nursing home and those who remained in the community. Because social factors are likely to exert stronger influences in the case of expected deaths than for unexpected deaths, where chance elements may play a large role, we examined place of death for expected deaths as well as for total deaths.
FIGURE 1.
Multilevel conceptual framework of place of death involving 2 end-of-life transitions.
METHODS
Data
Data came from the Health and Retirement Study (HRS), a national longitudinal study of health, family support, and economic circumstances of older adults.15 We focused on respondents born in 1923 or earlier (a national representative sample of noninstitutionalized seniors 70 years and older at the 1993 baseline survey conducted) who died between 1993 and 2002. HRS tracks all the respondents every 2 years (3 years between 1992 and 1995), including those who moved to nursing homes. For deceased participants, exit interviews are attempted with “proxy” informants knowledgeable about the respondents. As of the 2002 wave, 3563 of the 7443 people in the original cohort were known dead, of whom 3349 completed exit interviews in 1995, 1998, 2000, or 2002. Our sample consists of 3320, excluding 28 cases with missing death or end-of-life nursing home admission timing data. We supplemented person-level data drawn from files produced by the Rand Center for the Study of Aging (Version E), which include data from the panel surveys conducted in 1993, 1995, 1998, 2000, and 2002, with other public data files such as “exit interview” and “tracker” files.15 A restricted data file containing state and county identifiers permitted us to link state- and county-level data to the person-level data.
To identify “permanent” nursing home relocation, we relied on a proxy informant’s response to the following question: “Was (the respondent) living in a nursing home or other health care facility at the time (he/she) died?” HRS defines a nursing home or other facility as any institution that provides 24-hour care, dispenses medication, and offers personal assistance and room and meals. This question captures the place of residence at the time of death, which may be the same as, or different from, the place of death. The length of “permanent” nursing home stays varied: the median was approximately 4 months, whereas a quarter of our sample stayed for less than 1 month and the upper 5% for more than 3.5 years up to 7.8 years. The timing of relocation and the place of death were determined by the questions, “In what month and year did (he/she) move to the facility where (he/she) was a resident just before (his/her) death?” and “At the time of death, was (the respondent) in a hospital, in a nursing home, at home, in a hospice, or what?,” respectively.
Independent Variables
State HCBS expenditures were measured by 2 alternative variables, total HCBS expenditures per 65+ population, and percentage of LTC expenditures going to HCBS rather than nursing homes.16-18 The former indicates the absolute amount of money spent on HCBS adjusted for the state population size, whereas the latter indicates the extent of state LTC system’s orientation toward HCBS as opposed to institutional services. These variables were created for 1993-2002 from state-level data on HCBS and LTC expenditures compiled from various sources. We captured HCBS funds not only from Medicaid (home health and personal care19,20 and waiver programs21-23) but also from non-Medicaid funds (Older Americans Act,24-26 Social Services Block Grant,27-29 and state-funded programs16,30,31) that provided HCBS to older adults, given the substantial role played by non-Medicaid programs in some states. For multivariate analysis, we used the natural logarithm of the per-capita HCBS expenditures to capture the effect of proportional changes. To identify the state of residence, we used administrative records of place of residence (1993) or the location of interviews (subsequent HRS panel surveys), which were matched with respondents’ self-reported state of residence. County-level measures of LTC availability (nursing home beds and certified home health agencies)32 adjusted for the number of 65+ residents33 and medical resources (hospital beds and physicians, and the percentage of specialists among physicians33) were also included. As shown in Table 1, state-level HCBS expenditures significantly increased both in their percentage of LTC expenditures and per-capita amount between 1993 and 2000.
TABLE 1.
Characteristics of States and Counties Represented in the Sample of Health and Retirement Study Respondents Born 1923 or Earlier and Deceased as of 2002, 1993-2000
| Variables | 1993 (201 Counties, 36 States)* Median (25, 75 Percentile) |
1995 (255 Counties, 41 States) Median (25, 75 Percentile) |
1998 (309 Counties, 41 States) Median (25, 75 Percentile) |
2000 (342 Counties, 44 States) Median (25, 75 Percentile) |
|---|---|---|---|---|
| State-level | ||||
| HCBS expenditures per 65+ persons ($)† | 161 (107, 257) | 214 (157, 318) | 308 (183, 438) | 354 (195, 533) |
| Total LTC expenditure per 65+ persons ($)‡ | 911 (728, 1199) | 1071 (875, 1272) | 1244 (1072, 1598) | 1402 (1189, 1802) |
| Percentage of total long-term care expenditures spent on HCBS (%) | 18.86 (14.13, 25.34) | 21.00 (15.58, 27.99) | 24.84 (16.39, 32.38) | 25.94 (16.94, 33.05) |
| County-level | ||||
| No. nursing home beds per 1000 65+ persons§ | 48.14 (37.20, 62.57) | 48.66 (37.53, 65.26) | 48.58 (38.41, 65.55) | 48.20 (38.25, 63.37) |
| No. home health agencies per 10,000 65+ persons | 1.64 (0.96, 2.68) | 1.83 (1.05, 3.22) | 2.05 (1.13, 3.49) | 1.48 (0.90, 2.67) |
| No. hospital beds per 1000 persons¶ | 3.42 (2.10, 5.14) | 3.15 (1.78, 4.79) | 2.91 (1.74, 4.35) | 2.76 (1.61, 4.05) |
| No. physicians per 1000 persons∥ | 1.28 (0.73, 69.68) | 1.34 (0.81, 1.92) | 1.39 (0.89, 2.02) | 1.41 (0.91, 2.02) |
| Percentage of specialists among physicians∥ | 65.00 (56.40, 69.68) | 63.77 (54.65, 69.19) | 63.17 (53.21, 68.21) | 62.38 (53.96, 68.06) |
Change in the number of states and counties resulted from residential mobility and mortality of the sample.
Home and community-based services (HCBS) include expenditures on Medicaid home health, personal care,19,20 and 1915 (c) waiver programs for the aged/disabled21-23], Older Americans Act,24-26 Social Services Block Grant,27-29 and state source programs.16,30,31 The sum was divided by the size of 65+ population for each state.
Total LTC (long-term care) expenditures = Total HCBS expenditures plus Medicaid nursing home expenditures.19,20
Nursing home beds include both certified and uncertified beds in certified nursing homes.32
Short-term general and long-term hospital beds.33
Active, office-based physicians. Specialists include all specialist physicians except for those in general internal medicine, general pediatrics, and family practice subspecialties.33
Each set of analysis (nursing home relocation and place of death) involves the same state-level and county-level factors and a similar, but somewhat different set of person-level factors assessed at different points in the respondents’ life course. For example, causes of death and end-of-life circumstances can determine place of death, while they are irrelevant for the majority of nursing home relocations that may occur before terminal illnesses. Person-level factors included in both sets of analysis are: sociodemographic variables (age, gender, race/ethnicity, years of education, household income and nonhousing wealth, Medicaid coverage), physical/mental health and function, and family availability. Most of these person-level variables were compiled from the Rand data unless noted otherwise. More detailed description of variables unique to each analysis is provided below.
Analysis
After describing where people died, we conducted discrete-time survival analysis of the risk of permanent nursing home relocation to examine how it is associated with states’ support for HCBS, taking into consideration the timing of relocation and state, county, and person-level characteristics that change over time. Then we ran logistic regression analysis of place of death, separately for community and nursing home residents, to examine how the chance of dying in the residence (vs. in the hospital) was associated with state LTC contexts and individuals’ end-of-life circumstances.
RESULTS
Where Do People Die?
Of the total sample of N = 3320, approximately one-quarter died at home, another quarter in a nursing home, and the rest in hospitals, hospice, and other locations. Description of place of death by end-of-life residence (Table 2) is consistent with the view that place of death is contingent on whether one relocated to a nursing home or remained in the community: among community residents, 40.9% died at home and 1.5% in a nursing home; among nursing home residents, 68.7% died in the nursing home and only 0.8% at home.
TABLE 2.
End-of-Life Characteristics: Health and Retirement Study Respondents Born in 1923 or Earlier and Deceased as of 2002*
| Total Sample N = 3320 |
Those Who Died at the Residence or in the Hospital N = 2528 |
|||
|---|---|---|---|---|
| Variables | Community Residents N = 2125 % |
Nursing Home Residents N = 1195 % |
Community Residents N = 1615 % or Mean (SD) |
Nursing Home Residents N = 913 % or Mean (SD) |
| Place of death | ||||
| Home | 40.9 | 0.8 | 45.3 | |
| Nursing home | 1.5 | 68.7 | 74.5 | |
| Hospital | 49.5 | 23.1 | 55.7 | 25.5 |
| Hospice | 3.1 | 3.3 | ||
| Other | 5.0 | 4.2 | ||
| Sociodemographic characteristics | ||||
| Age at death (yrs) | 83.2 (6.2) | 87.1 (6.3) | ||
| Female gender (%)* | 52.4 | 63.8 | ||
| Race (%)* | ||||
| White non-Hispanic (ref) | 76.4 | 83.1 | ||
| Black non-Hispanic | 16.2 | 14.4 | ||
| Hispanic | 7.4 | 2.5 | ||
| Education (yrs)* | 10.1 (4.0) | 10.0 (3.7) | ||
| Household income ($)* | 26,989 (44,289) | 18,842 (27,627) | ||
| Total nonhousing wealth ($)* | 156,463 (909,350) | 81,962 (279,053) | ||
| Medicaid at death (%) | 18.0 | 41.1 | ||
| Cause of death (%) | ||||
| Cancer (ref) | 23.9 | 13.0 | ||
| Cardiovascular disease | 44.1 | 44.5 | ||
| Other chronic conditions | 9.0 | 11.5 | ||
| Acute conditions | 6.8 | 9.1 | ||
| Unknown | 3.1 | 3.6 | ||
| Other | 13.5 | 18.5 | ||
| Timing of death | ||||
| Death expected (%) | 52.9 | 68.9 | ||
| Duration of final illness (%) | ||||
| <1 d | 19.1 | 11.8 | ||
| <1 mo | 36.9 | 39.7 | ||
| ≥1 mo (ref) | 44.0 | 48.5 | ||
| End of life health status | ||||
| No. ADL† limitations in the last 3 mo (range, 0-6) | 2.8 (2.6) | 4.7 (2.0) | ||
| Any ADL limitation lasting >1 yr | 10.1 | 18.8 | ||
| Temper (%) | 12.0 | 20.5 | ||
| Confused (%) | 32.3 | 54.8 | ||
| Severe pain (%) | 18.6 | 18.0 | ||
| No. diseases: (range, 0-5)‡ | 1.6 (1.0) | 1.6 (1.0) | ||
| Cognitive impairment§ | 9.13 (3.8) | 12.0 (3.5) | ||
| Family availability | ||||
| Married (%) | 47.2 | 27.8 | ||
| No. children* | 2.9 (2.4) | 2.374 (2.0) | ||
| Live alone (%)* | 66.6 | 80.8 | ||
| Control variables | ||||
| Year of death | 1997.5 (2.4) | 1998.5 (2.3) | ||
| Years since last core interview | 1.1 (0.7) | 1.3 (0.8) | ||
Obtained from the data of the last core survey that the respondent participated in when alive. All the other variables were obtained from exit interviews.
Activities of daily living.
Number of diagnosed health conditions that have ever been reported (heart, stroke, lung, cancer, and other).
Sum of 3 cognition variables assessing memory, judgment, and organization [each assessed on a scale of 1-5 (ie, excellent to poor; range, 3-15)].
Does State Support for HCBS Reduce the Risk of End-of-life Relocation to a Nursing Home?
For discrete time survival analysis of permanent nursing home relocation, we constructed a file of person-months for each observation beginning with the month of the 1993 interview and continuing until admission to a nursing home where the person resided at death. We chose the month of 1993 interview as the starting point, because our focus was on state-specific “period” or “history” effects of HCBS. We controlled for birth cohorts by including age at the 1993 survey. Those who died without permanent nursing home relocation were considered censored. For each month of observation, we constructed time-varying covariates, drawn from the most recent interview (for person-level variables) and the most recent annual data (for state and county-level variables) before the month in question.
After excluding 55 respondents with missing data, the analysis file consisted of 155,108 person-month records, each coded to indicate whether permanent relocation to a nursing home had taken place. Of the 3265 respondents represented in those records, 1082 persons resided in nursing homes at the time of death.
The effects of state- and county-level factors presented in Table 3 are based on the complementary log-log model34 with standard errors adjusted for individuals clustered within states.35 We examined the main state HCBS effects (including or excluding county factors) and the interaction between state HCBS and person-level Medicaid status for 2 alternative measures of HCBS. Higher state HCBS was associated with lower risk of nursing home relocation, regardless of state HCBS measures and county-level controls. When measured in HCBS expenditures per 65+, state HCBS had significant main effects (not shown) and interaction with Medicaid (models 1 and 2). The significant interaction indicated differential HCBS effects: for those with Medicaid, the HCBS coefficient is the sum of the HCBS main effect and the interaction coefficients [(-0.0191) + (-0.2309) = 0.25; P < 0.02], suggesting that doubling per-capita HCBS expenditures (a 100% increase) would result in a 25% reduction in the risk of nursing home relocation. For those without Medicaid, the effect (-0.0191) was not statistically significant. When measured in the percentage of LTC expenditures, state HCBS had significant main effects (models 3 and 4), but there was no statistically significant interaction (not shown). The HCBS coefficient in model 3 (-0.0068; P ≤ 0.01) indicates that a 10% increase in the percent of LTC expenditures spent on HCBS would reduce the risk of relocation by 6.8%. Adding county-level controls reduces the effect to -0.0036 (P < 0.10), indicating that some of the HCBS effect is mediated by county-level variables. All models controlled for numerous person level variables as shown in the footnote to Table 3.
TABLE 3.
State- and County-Level Correlates of Permanent Nursing Home Admission: Discrete Time Survival Analysis Results‡
| Variables | Model 1 Coefficients (Exponentiated) | Model 2 Coefficients (Exponentiated) | Model 3 Coefficients (Exponentiated) | Model 4 Coefficients (Exponentiated) |
|---|---|---|---|---|
| Person-level factors§ | ||||
| Medicaid coverage (1 = yes, 0 = no) | 0.0363 (1.0370) | 0.0227 (1.0230) | 0.0139 (1.0140) | 0.00136 (1.0014) |
| State-level health system factors | ||||
| Total HCBS∥ expenditures per 65+ (logged) | -0.0191 (0.9810) | -0.0121 (0.9880) | ||
| Percentage of LTC¶ expenditures spent on HCBS∥ | -0.0068 (0.9932)† | -0.0036 (0.9964)* | ||
| LTC¶ expenditures per 65+ persons (logged) | -0.0264 (0.9739) | -0.0497 (0.9515) | ||
| Interaction between state-level HCBS and person-level Medicaid status** | -0.2309 (0.7938)* | -0.2153 (0.8063)* | ||
| County-level health system factors | ||||
| Nursing home beds per 1000 65+ at county | 0.0055 (1.0055)† | 0.0001 (1.0001)† | ||
| Hospital beds per 1000 persons at county | 0.0098 (1.0099) | 0.0088 (1.0088) | ||
| Home health agencies per 10,000 65+ at county | -0.0016 (0.9984) | -0.0013 (0.9987) | ||
| Generalist physicians per 1000 persons at county | -0.1657 (0.8473) | -0.1682 (0.8452) | ||
| Percentage of specialist physicians at county | 0.1886 (1.2076) | 0.1724 (1.1882) | ||
P ≤ 0.10.
P ≤ 0.01.
Models 1 and 2 use total HCBS expenditures per 65+ person as a measure of state HCBS expenditures, whereas models 3 and 4 use percentage of LTC expenditures spent on HCBS rather than nursing homes and include total per-capita long-term care expenditures as a control variable. Models 1 and 3 include state-level factors, and models 2 and 4 include state and county-level factors.
Other person-level variables included in the models are age, gender, race, years of education, household wealth, household income, nursing home coverage, physical functioning, self-rated health, severity of dementia (1 = no dementia, 2 = mild dementia, 3 = moderate dementia, 4 = severe dementia), number of medical conditions, marital status (currently married or not), child availability (3 categories: coresidence or child living ≤10 miles, child living >10 miles, and no living child), number of living siblings, spouse age, spouse physical functioning, spouse self-rated health, spouse’s number of medical conditions, whether own residential house, whether proxy interview, time since the month of 1993 survey, and time squared, square of time, and cubic of time.
Home- and community-based services.
Long-term care.
The interaction between state-level HCBS and person-level Medicaid status was significant when state HCBS was measured in HCBS expenditures per 65+ (models 1 and 2). This result indicates that the effects of state HCBS expenditures depend on the person’s Medicaid status. For those with Medicaid, the HCBS coefficient was -0.25 (-0.0191 plus -0.2309; P = 0.02), suggesting that doubling per-capita HCBS expenditures (100% increase) would result in a 25% reduction in the risk of nursing home relocation. For those without Medicaid, the coefficient was -0.0191 (statistically insignificant). On the other hand, when state HCBS expenditures were measured in the percentage of LTC expenditures spent on HCBS, the interaction term involving state HCBS and Medicaid status was not significant (results not shown). Thus, Table 3 reports the main effects models that do not include the interaction term (models 3 and 4).
End-of-Life Circumstances and State HCBS Spending: Association With Place of Death
We examined factors associated with place of death separately for community residents and nursing home residents, as we argued that place of death is contingent on the decision to relocate to a nursing home. Given the small number of people who died in settings other than residence or hospital (Table 2, columns 1 and 2), we restricted our analysis to those who died in the end-of-life residence or in a hospital. We excluded hospice from our dependent and independent variables, because the number of hospice deaths was too small to constitute a separate category, and we could not ascertain the actual place of death, given that hospice services can be provided in a home, hospital, or nursing home setting. Sensitivity analysis including hospice deaths as deaths in the residence or hospital deaths, indicated that our findings were robust. The analytic sample consisted of 2528 (1615 community and 913 nursing home) residents from 36 states, after excluding those who died in hospice or other unspecified places (n = 301), cases with missing or inconsistent state identifiers (n = 272), those who moved out of the area since the interview before death (n = 124), and those with missing data for specific variables (n = 95). Data from each wave of exit interviews were combined with state and county-level data from the year in which a respondent died.
The independent variables represent end-of-life circumstances. Age at death was calculated based on birth months (Rand data) and death months (exit interview data). For 17 cases with no death month information, we used the National Death Index (NDI) data available from HRS as a restricted dataset. If the month of birth or death was unavailable, only the year was used for computation. Household income and nonhousing wealth, assessed at the last interview before death and inflation adjusted using the 2000 consumer price index, involved 3 categories (high, middle, low) using the 33.3 and 66.6 percentile values of the 1993 full sample to adjust for potentially high mortality of people with lower income. Medicaid status was assessed at the time of death. Underlying causes of death came from the NDI data. HRS collapsed cause-of-death categories comparable in ICD9 and ICD1036 at their highest levels. We grouped the HRS codes into cancer (reference category), cardiovascular diseases, other chronic diseases, acute diseases, other causes, and unknown. Timing of death was indicated by whether or not the death was expected at the time it occurred, and duration of the final illness that led to death. End-of-life health status included the number of activities of daily living (ADL) limitations during the last 3 months of life, and whether the duration of any ADL limitation lasted longer than a year. Those respondents who spent the last 3 months in bed were coded as limited in all ADL items. Also included were variables indicating whether there was a period of at least 1 month during the last year when the respondent had “uncontrolled outbursts of temper” or “periodic confusion,” whether the respondent experienced severe pain most of the time since the last interview, the number of diagnosed health conditions, and cognitive impairment. Family availability involves marital status, living alone at death, and the number of living children assessed at the most recent panel survey. Calendar years of death was included to examine the time trend of place of death. Time between the most recent panel interview month and the death month varied from person to person and thus was controlled for. Table 2 presents sample characteristics.
Preliminary multilevel analysis results (not shown; “empty” model with no independent variables; individuals nested in counties nested in states) indicated that the variance was mainly at the individual level with negligible variance at the state- and county-levels (0.22% and 0.32%, respectively among community residents; 0.65% and 5.74% among nursing home residents). Thus, rather than using random effect models, we present conventional logistic regression analysis with standard errors adjusted for clustering in states35 for community and nursing home samples (Table 4). For each sample, we ran parallel models including and excluding unexpected deaths.
TABLE 4.
Logistic Regression Analysis of Dying in the Residence (vs. Hospital) by End-of-Life Residence
| Community Residents |
Nursing Home Residents |
|||||||
|---|---|---|---|---|---|---|---|---|
| Full Sample N = 1615 |
Expected Deaths§ N = 855 |
Full Sample N = 913 |
Expected Deaths§ N = 628 |
|||||
| Odds | (SE) | Odds | (SE) | Odds | (SE) | Odds | (SE) | |
| Sociodemographic characteristics | ||||||||
| Age (yrs) | 1.032† | (0.010) | 1.068‡ | (0.014) | 1.023 | (0.017) | 1.024 | (0.022) |
| Female | 0.936 | (0.105) | 1.323 | (0.220) | 1.065 | (0.217) | 0.972 | (0.201) |
| Black | 0.785 | (0.133) | 0.436† | (0.120) | 0.623* | (0.138) | 0.360‡ | (0.087) |
| Hispanic | 1.014 | (0.198) | 1.077 | (0.290) | 0.385‡ | (0.090) | 0.347* | (0.163) |
| Education (yrs) | 1.002 | (0.018) | 0.986 | (0.024) | 1.015 | (0.029) | 1.011 | (0.033) |
| Income (low = reference) | ||||||||
| Middle | 1.092 | (0.186) | 1.493 | (0.355) | 0.769 | (0.166) | 0.996 | (0.260) |
| High | 1.056 | (0.236) | 2.151* | (0.687) | 0.629 | (0.164) | 0.779 | (0.335) |
| Wealth (low = reference) | ||||||||
| Middle | 1.128 | (0.173) | 1.150 | (0.190) | 1.111 | (0.332) | 1.062 | (0.375) |
| High | 1.177 | (0.194) | 0.832 | (0.168) | 1.614 | (0.498) | 1.155 | (0.516) |
| Medicaid | 0.897 | (0.219) | 0.893 | (0.271) | 0.989 | (0.190) | 0.795 | (0.237) |
| Underlying cause of death | ||||||||
| Cardiovascular disease | 0.737* | (0.101) | 0.365‡ | (0.087) | 0.350† | (0.122) | 0.324* | (0.147) |
| Other chronic conditions | 0.211‡ | (0.062) | 0.135‡ | (0.052) | 0.242† | (0.116) | 0.241* | (0.153) |
| Acute conditions | 0.573† | (0.114) | 0.355‡ | (0.082) | 0.205‡ | (0.093) | 0.212† | (0.122) |
| Unknown | 0.542‡ | (0.123) | 0.503‡ | (0.204) | 0.625† | (0.316) | 0.990* | (0.699) |
| Other | 0.424† | (0.083) | 0.276 | (0.076) | 0.311 | (0.119) | 0.342 | (0.159) |
| Timing of death | ||||||||
| Death expected | 1.290* | (0.167) | 1.734* | (0.376) | ||||
| Final illness (>1 mo = reference) | ||||||||
| <1 d | 2.019‡ | (0.326) | 0.760 | (0.264) | 0.631 | (0.152) | 0.500 | (0.243) |
| <1 mo | 0.236‡ | (0.032) | 0.374‡ | (0.063) | 0.296‡ | (0.042) | 0.305‡ | (0.051) |
| End-of-life health status | ||||||||
| No. ADL∥ limitations in the last 3 mo | 1.082‡ | (0.021) | 1.178‡ | (0.048) | 1.088 | (0.048) | 1.180‡ | (0.059) |
| Any ADL∥ lasting >1 yr | 1.074 | (0.248) | 1.414 | (0.411) | 1.275 | (0.313) | 1.446 | (0.383) |
| Temper | 0.976 | (0.146) | 1.315 | (0.193) | 1.621* | (0.383) | 1.199 | (0.395) |
| Confused | 1.274 | (0.227) | 1.118 | (0.217) | 0.787 | (0.186) | 0.906 | (0.239) |
| Severe pain | 0.946 | (0.136) | 1.043 | (0.240) | 0.687 | (0.139) | 0.696 | (0.142) |
| No. diseases | 0.820‡ | (0.046) | 0.851 | (0.085) | 0.839 | (0.078) | 0.817 | (0.102) |
| Cognitive impairment¶ | 1.016 | (0.019) | 1.017 | (0.022) | 1.063* | (0.026) | 1.024 | (0.038) |
| Family availability | ||||||||
| Married | 1.098 | (0.136) | 1.145 | (0.284) | 1.347 | (0.320) | 1.127 | (0.371) |
| No. children | 1.037 | (0.030) | 1.064 | (0.037) | 1.021 | (0.058) | 1.039 | (0.067) |
| Live alone | 0.885 | (0.091) | 0.813 | (0.152) | 0.848 | (0.190) | 0.849 | (0.283) |
| Control variables | ||||||||
| Year of death | 0.982 | (0.033) | 1.023 | (0.049) | 1.051 | (0.042) | 1.047 | (0.043) |
| Years since previous survey | 1.042 | (0.081) | 0.994 | (0.101) | 0.985 | (0.109) | 0.940 | (0.130) |
| County-level resources | ||||||||
| Nursing home beds/1000 65+ | 1.000 | (0.003) | 0.997 | (0.004) | 1.006 | (0.005) | 1.001 | (0.006) |
| Home health agencies/10,000 65+ | 0.995 | (0.020) | 0.987 | (0.030) | 0.986 | (0.026) | 1.014 | (0.031) |
| Hospital beds/1000 65+ | 0.972 | (0.025) | 0.942 | (0.034) | 0.998 | (0.052) | 1.004 | (0.048) |
| Physicians/1000 65+ | 1.032 | (0.113) | 1.187 | (0.193) | 0.832 | (0.108) | 0.759 | (0.147) |
| % Specialist physicians | 0.997 | (0.006) | 0.989 | (0.010) | 1.014 | (0.008) | 1.023 | (0.010) |
| State-level HCBS | ||||||||
| HCBS** $/65+ (logged) | 1.057 | (0.089) | 0.970 | (0.098) | 0.907 | (0.095) | 0.982 | (0.167) |
P ≤ 0.05.
P ≤ 0.01.
P ≤ 0.001.
Based on the proxy informant’s response to the question, “Was the death expected at about the time it occurred, or was it unexpected?”
Activities of daily living.
Sum of 3 cognition variables assessing memory, judgment, and organization (each assessed on a scale of 1-5; ie, excellent to poor; range, 3-15).
Home- and community-based services.
Cause of death, medical needs, and timing of death were consistently associated with death in the residence (vs. hospital death). Both in the community and nursing home samples, cancer deaths (vs. dying of other causes), less medical needs (ie, less comorbidities), and more ADL limitations in the last 3 months of life were associated with death in the residence. The final illness lasting less than a month increased the chance of hospital death in both samples, whereas the duration of final illness was negatively associated with hospital death in the community sample but positively associated with hospital death in the nursing home sample.
Among community residents, dying at an older age was associated with home death. Community residents with final illness lasting more than a month were more likely to die in the home. Home death was also associated with higher income and nonethnic minority status, and marginally with the number of living children. Among nursing home residents, nursing home death (vs. hospital death) was associated with nonminority status. African Americans’ reduced chance of dying at a residence was especially salient when death was expected. Contrary to our initial expectation, availability of specialist physicians was associated with a higher chance of dying in a nursing home among nursing home residents whose death was expected. We speculate that hospitals in areas with higher medical specialization may be more reluctant to care for dying elderly patients. Or it could be that nursing home residents in such areas have more access to outpatient specialists, reducing the need for hospitalization.
As expected, state HCBS expenditures were not significantly associated with place of death, regardless of the use of an alternative HCBS measure (percentage of LTC expenditures).
DISCUSSION
States vary greatly in LTC policies and their efforts to convert a traditionally institution-based LTC system into a more balanced one that would help people with disabilities access community-based services and remain in the community.18 We examined whether such variation contributes to the large state-to-state variation in location of death using a conceptual model involving 2 end-of-life transitions (nursing home relocation and death) and their relationships with multilevel factors (state HCBS support, county health resources, and person-level characteristics). A major strength of this study lies in the use of a 10-year longitudinal multilevel dataset, which allowed examination of state HCBS effects on older persons’ end-of-life transitions that occurred over years. We found that living in a state with high HCBS expenditures would reduce the risk of end-of-life relocation to a nursing home, especially among those with Medicaid, and thus indirectly increase the chance of dying at home. State commitment to HCBS did not have a direct effect on the chance of dying in the residence (vs. hospital), whether one lived in the community or in a nursing home. This lack of effect was not surprising, given that HCBS are not designed to address end-of-life medical needs. Minorities and individuals with fewer resources (income and time to prepare for death during one’s final illness) were less likely to die in the residence. This finding is consistent with previous studies that indicate racial and socioeconomic disparities in end-of-life transitions.37
Our findings add to the emerging evidence from recent observational studies that states’ increased spending on HCBS may reduce nursing home utilization among seniors.18,38 Based on the HRS data, Muramatsu et al18 reported that living in a state with higher HCBS expenditures reduced first life-time nursing home admission lasting 90+ days among childless seniors.18 Our current study extended these findings to show that state HCBS may exert statistically significant effects on permanent nursing home relocation regardless of child availability. Those findings of state HCBS effects are in contrast with studies of the late 1970s and early 1980s based mainly on experimental designs, which provided little support for HCBS’s effects on preventing nursing home admissions.39-42
The United States has made a significant progress towards expanding HCBS, mainly through Medicaid HCBS waiver programs. Most public LTC services are funded for those with limited economic resources. Our study indicated that per-capita state HCBS expenditures lowers the risk for nursing home relocation among those with Medicaid, but not among those without, suggesting that the US efforts to enhance HCBS do not significantly benefit Medicaid-ineligible Americans. On the other hand, a higher percentage of LTC expenditures spent on HCBS, which was also associated with reduced risk of nursing home relocation, did not have differential effects on those with or without Medicaid, indicating that state efforts to shift their LTC services from nursing homes to HCBS may have exerted spill-over effects on people who are not poor enough to be eligible for public HCBS, perhaps by changing societal caregiving norms to promote HCBS. Given that LTC needs are universal regardless of one’s socioeconomic status, the United States should look toward other countries already committed to universal and equitable access to LTC.43
States’ adoption of enhanced HCBS programs may not be independent of nursing home utilization. States with higher nursing home utilization might be more motivated to adopt HCBS initiatives, while states without strong nursing home industries or those with strong home care labor unions may be better positioned to lower nursing home utilization and enhance HCBS. Complex political factors and processes that may facilitate or inhibit HCBS support are beyond the scope of this study and should be examined in future research.
Our study, due to data limitations, could not incorporate additional determinants of place of death, including nursing home characteristics44-46 and end-of-life needs.47 Preference may be expressed in the form of advanced directives to limit health care, an item included in the HRS exit interviews except for 1998. Our analysis excluding the 1998 data indicated that advanced directives significantly reduced hospital deaths in the nursing home sample (not shown), supporting previous findings.48 Access to hospice, known to facilitate home deaths, is another missing factor.
Due to the HRS complex sampling design, our sample did not include all 50 states. Side analyses indicated that states included in the sample had higher HCBS expenditures. The implications of this are difficult to assess, and caution is needed to generalize our findings. Our use of the sample restricted to noninstitutionalized persons aged 70+ as of 1993 may be justified, because states’ support for HCBS is mainly targeted to noninstitutionalized seniors.
Our findings support states’ increased efforts to expand HCBS programs, which would reduce the risk of moving into a nursing home and thus increase the chance of spending end-of-life at home. However, we should pay attention to evidence that people facing death sometimes prefer to die in an institution because the home setting may not accommodate difficult end-of-life situations.49,50 Promoting a LTC system that would help seniors deal with end-of-life medical emergencies and reduce family burden could not only enhance people’s quality of life but also help lower inpatient hospital expenditures that constitute a large portion of older adults’ end-of life health care expenses. States’ support for HCBS should involve end-of-life care, for example, greater integration of social and medical services, improved access to medical care for the homebound, and greater access to end-of-life care for people dying of noncancer diseases as well as cancer.
ACKNOWLEDGMENTS
The authors thank Robert L. Kane and Marshall H. Chin for their insightful comments on earlier versions of this paper; Paul D. Allison for his assistance on statistical issues; Brian Burwell, Charlene Harrington, and other people at various agencies and organizations for their help in our state data compilation process; and John Klemm of the Centers for Medicare and Medicaid Services, who provided the Medicaid expenditure data of 1992 and 1993 from Form CMS-64.
This work was supported by the National Institute on Aging (R01 AG021648).
Footnotes
An earlier version of this article was presented at the 50th Annual Scientific Meeting of the Gerontological Society of America, November 18, 2006, Dallas, TX.
REFERENCES
- 1.Flory J, Yinong YX, Gurol I, et al. Place of death: US. trends since 1980. Health Aff. 2004;23:194–200. doi: 10.1377/hlthaff.23.3.194. [DOI] [PubMed] [Google Scholar]
- 2.Pritchard RS, Fisher ES, Teno JM, et al. Influence of patient preferences and local health system characteristics on the place of death. J Am Geriatr Soc. 1998;46:1242–1250. doi: 10.1111/j.1532-5415.1998.tb04540.x. [DOI] [PubMed] [Google Scholar]
- 3.Center for Gerontology and Health Care Research [Accessed July 23, 2005];Facts on dying: policy relevant data on care at the end of life. 2005 Available at: http://www.chcr.brown.edu/dying/2001DATA.HTM.
- 4.National Center for Health Statistics [Accessed February 26, 2007];Deaths by place of death, age, race, and sex: United States, 2001. 2004 Work Table 309. Available at: http://www.cdc.gov/nchs/data/statab/mortfinal2001_work309.pdf.
- 5.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 6.Hoover DR, Crystal S, Kumar R, et al. Medical expenditures during the last year of life: findings from the 1992-1996 Medicare Current Beneficiary Survey. Health Serv Res. 2002;37:1625–1642. doi: 10.1111/1475-6773.01113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keehan SP, Lazenby HC, Zezza MA, et al. [Accessed February 8, 2007];Age estimates in the national health accounts. 2004 Available at: http://www.cms.hhs.gov/HealthCareFinancingReview/Downloads/Keehan.pdf. [PMC free article] [PubMed]
- 8.Hogan C, Lunney J, Gabel J, et al. Medicare beneficiaries’ costs of care in the last year of life. Health Aff. 2001;20:188–195. doi: 10.1377/hlthaff.20.4.188. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell SL, Teno JM, Miller SC, et al. A national study of the location of death for older persons with dementia. J Am Geriatr Soc. 2005;53:299–305. doi: 10.1111/j.1532-5415.2005.53118.x. [DOI] [PubMed] [Google Scholar]
- 10.Weitzen S, Teno JM, Fennell M, et al. Factors associated with site of death: a national study of where people die. Med Care. 2003;41:323–335. doi: 10.1097/01.MLR.0000044913.37084.27. [DOI] [PubMed] [Google Scholar]
- 11.Kane RL, Kane RA, Ladd RC, et al. Variation in state spending for long-term care: factors associated with more balanced systems. J Health Polit Policy Law. 1998;23:364–390. doi: 10.1215/03616878-23-2-363. [DOI] [PubMed] [Google Scholar]
- 12.Kitchener M, Carrillo H, Harrington C. Medicaid community-based programs: a longitudinal analysis of state variation in expenditures and utilization. Inquiry. 2003;40:375–389. doi: 10.5034/inquiryjrnl_40.4.375. [DOI] [PubMed] [Google Scholar]
- 13.Miller SC, Shield R. [Accessed September 7, 2007];Palliative care/hospice for persons with terminal and/or chronic progressive illness: the role of state and federal policies in shaping access and quality for persons receiving long-term care. 2007 Available at: http://www.chcr.brown.edu/PDFS/JEHT_4_FINALREPORT07.pdf.
- 14.Merrill DM, Mor V. Pathways to hospital death among the oldest old. J Aging Health. 1993;5:516–535. doi: 10.1177/089826439300500406. [DOI] [PubMed] [Google Scholar]
- 15. [Accessed September 7, 2007];The Health and Retirement Study. Available at: http://hrsonline.isr.umich.edu/
- 16.Administration on Aging . Infrastructure of Home and Community Based Services for the Functionally Impaired Elderly—State Source Book. Administration on Aging, U.S. Department of Health and Human Services; Washington, DC: 1995. [Google Scholar]
- 17.Ladd RC, Kane RL, Kane RA, et al. State long term care profiles report. National LTC Mentoring Program, Institute for Health Services Research, School of Public Health, University of Minnesota; 1995. [Google Scholar]
- 18.Muramatsu N, Yin H, Campbell RT, et al. Risk of nursing home admission among older Americans: does states’ spending on home and community-based services matter? J Gerontol B Psychol Sci Soc Sci. 2007;62:S169–S178. doi: 10.1093/geronb/62.3.s169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burwell B. [Accessed February 13, 2004];Medicaid long term care expenditures in FY 2000. 2001 doi: 10.1093/geront/41.5.687. Available at: http://www.hcbs.org/htmlFile.php/fid/280/did/127/ [DOI] [PubMed]
- 20.Burwell B. [Accessed February 13, 2004];Medicaid long term care expenditures, FY2002. 2003 doi: 10.1093/geront/41.5.687. Available at: http://www.hcbs.org/files/5/248/2002LTCExpenditures.xls. [DOI] [PubMed]
- 21.Burwell B. [Accessed February 13, 2004];Medicaid HCBS waiver expenditures, FY1995-2000. 2001 Available at: http://www.hcbs.org/moreInfo.php/type_tool/129/ofs/10/doc/127/Medicaid_HCBS_Waiver_Expenditures,_FY1995-2000.
- 22.Burwell B. [Accessed February 13, 2004];Medicaid HCBS waiver expenditures, FY1997-2002. 2003 Available at: http://www.hcbs.org/files/6/252/HCBSwaivers-Table2.xls.
- 23.Harrington C, Carillo HM, Wellin V, et al. © Medicaid home and community based waiver participants, services, and expenditures, 1992-1997. University of California, Department of Social and Behavioral Sciences; San Francisco, CA: 1915. 2000. [Google Scholar]
- 24.Administration on Aging . State Program Report for Titles III and VII of the Older Americans Act. Department of Health and Human Services; Washington, DC: 1995. 1995. [Google Scholar]
- 25.Administration on Aging . State Program Report for Titles III and VII of the Older Americans Act. Department of Health and Human Services; Washington, DC: 1996. 1996. [Google Scholar]
- 26.Administration on Aging [Accessed October 1, 2004];Titles III and VII State Program Reports. 2004 Available at: http://www.aoa.gov/prof/agingnet/NAPIS/SPR/spr_reports.asp.
- 27.U.S. Department of Health and Human Services. Office of Community Services . Social Services Block Grant Program Annual Report 2002. U.S. Government Printing Office; Washington, DC: 2004. [Google Scholar]
- 28.U.S. Department of Health and Human Services. Administration for Children and Families. Office of Community Services . Social Services Block Grant Program: Analysis of Expenditure and Recipient Data 1995-1997. U.S. Government Printing Office; Washington, DC: 1999. [Google Scholar]
- 29.U.S. Department of Health and Human Services. Administration for Children and Families. Office of Community Services . Social Services Block Grant Program Annual Report. U.S. Government Printing Office; Washington, DC: 20002004. [Google Scholar]
- 30.Kassner E, Williams L. Taking Care of Their Own: State-Funded Home and Community-Based Care Programs for Older Persons. The Public Policy Institute, American Association of Retired Persons; Washington, DC: 1997. [Google Scholar]
- 31.Summer LL, Ihara ES. State Funded Home and Community Based Service Programs for Older People. AARP Public Policy Institute; Washington, DC: 2004. [Google Scholar]
- 32.Provider of Services File 1992-2002. Centers for Medicare and Medicaid Services; Bethesda, MD: [PubMed] [Google Scholar]
- 33.Area Resource File. U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions; Rockville, MD: Feb, 2003. [Google Scholar]
- 34.Allison PD. Survival Analysis Using the SAS System: A Practical Guide. SAS Institute; Cary, NC: 1995. [Google Scholar]
- 35.Stata Corporation . Stata Statistical Software: Release 9.0. Stata Corporation; College Station, TX: 2005. [Google Scholar]
- 36.Anderson RN, Minino AM, Hoyert DL, et al. Comparability of Cause of Death Between ICD-9 and ICD 10: Preliminary Estimates. National Vital Statistics Reports National Center for Health Statistics. 2001:49. [PubMed] [Google Scholar]
- 37.Gruneir A, Mor V, Weitzen S, et al. Where people die: a multi-level approach to understanding influences on site of death in America. Med Care Res Rev. 2007;64:351–378. doi: 10.1177/1077558707301810. [DOI] [PubMed] [Google Scholar]
- 38.Alecxih LMB, Lutzky S, Corea J. Estimated cost savings from the use of home and community-based alternatives to nursing facility care in three states. The Public Policy Institute, American Association of Retired Persons; Washington, DC: 1996. [Google Scholar]
- 39.Doty P. Cost-Effectiveness of Home and Community-Based Long-Term Care Services. U.S. Department of Health and Human Services; Washington, DC: 2000. p. 18. [Google Scholar]
- 40.Kemper P. The evaluation of the national long term care demonstration: overview of findings. Health Serv Res. 1988;23:161–174. [PMC free article] [PubMed] [Google Scholar]
- 41.Weissert WG, Cready CM, Pawelak JE. The past and future of home and community-based long-term care. Milbank Q. 1988;66:309–388. [PubMed] [Google Scholar]
- 42.Wooldridge J, Schore J. The effect of channeling on the use of nursing homes, hospitals, and other medical services. Health Serv Res. 1988;23:119–127. [PMC free article] [PubMed] [Google Scholar]
- 43.Tsutsui T, Muramatsu N. Japan’s universal long-term care system reform of 2005: containing costs and realizing a vision. J Am Geriatr Soc. 2007;55:1458–1463. doi: 10.1111/j.1532-5415.2007.01281.x. [DOI] [PubMed] [Google Scholar]
- 44.Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially. Preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52:1730–1736. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- 45.Oliver DP, Porock D, Zweig S. End-of-life care in U.S. nursing homes: a review of the evidence. J Am Med Dir Assoc. 2004;5:147–155. doi: 10.1097/01.JAM.0000123063.79715.8E. [DOI] [PubMed] [Google Scholar]
- 46.Buchanan JL, Murkofsky RL, O’Malley AJ, et al. Nursing home capabilities and decisions to hospitalize: a survey of medical directors and directors of nursing. J Am Geriatr Soc. 2006;54:458–465. doi: 10.1111/j.1532-5415.2005.00620.x. [DOI] [PubMed] [Google Scholar]
- 47.Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ. 2006;332:515–521. doi: 10.1136/bmj.38740.614954.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Degenholtz HB, Rhee Y, Arnold RM. Brief communication: the relationship between having a living will and dying in place. Ann Intern Med. 2004;141:113–117. doi: 10.7326/0003-4819-141-2-200407200-00009. [DOI] [PubMed] [Google Scholar]
- 49.Fried TR, Pollack DM, Drickamer MA, et al. Who dies at home? Determinants of site of death for community-based long-term care patients. J Am Geriatr Soc. 1999;47:25–29. doi: 10.1111/j.1532-5415.1999.tb01897.x. [DOI] [PubMed] [Google Scholar]
- 50.Fried TR, van Doorn C, O’Leary JR, et al. Older persons’ preferences for site of terminal care. Ann Intern Med. 1999;131:109–112. doi: 10.7326/0003-4819-131-2-199907200-00006. [DOI] [PubMed] [Google Scholar]