Abstract
Gastrointestinal stromal tumor (GIST) of the stomach was treated by endoscopic enucleation in five patients. They were three men and two woman, aged 36-56 years. Tumors located in the cardia were completely enucleated endoscopically without any serious complication. The largest diameter of removed tumors ranged from 1.2 to 2.5 cm. Histopathological diagnosis was GIST with low risk of malignancy (mitotic index < 5/50 high power field) in all cases. The patients were disease-free for 10.5-42.2 mo after endoscopic enucleation.
Keywords: Gastrointestinal stromal tumor, Endoscopic enucleation, Stomach
INTRODUCTION
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal subepithelial tumors of the gastrointestinal tract. Immunohistochemical studies have indicated their relationship to the interstitial cells of Cajal, with which they share differentiation markers such as CD-117 (c-kit) and CD34[1]. They are tumors with uncertain malignant potential, the risk of which is predicted by tumor size and mitotic index[1].
Large GISTs of the stomach carry a high risk of malignancy, and surgical resection is the gold standard for treatment of these tumors. On the other hand, small GISTs (< 3 cm in diameter) are usually benign and there is no consensus about treatment recommendations for such tumors; surgery or observation with regular follow-up[2]. In several recent studies, laparoscopic[3,4] or endoscopic resection[2,5,6] has emerged as minimally invasive treatment for small GISTs of the stomach. However, most of these studies have been in single or a small number of cases, and the safety and efficacy of these novel treatments has not been established.
In this brief communication, we report the results of endoscopic enucleation of GISTs of the stomach in five patients. Endoscopic enucleation appears to be a safe and effective method of treatment of small GISTs of the stomach, if the tumor tissue does not adhere to the muscularis propria.
CASE REPORT
The patients were three men and two women, aged 36-56 years (median, 50 years). None of them complained of abdominal symptoms. Submucosal tumor of the stomach was found by endoscopy performed as a part of a medical check-up. The tumors were located in the stomach fundus in all cases, and their diameter ranged from 1.1 to 2.5 cm (median, 1.8 cm). They were diagnosed as GIST from the endoscopic appearance shown in Figure 1. Ultrasonography showed the origin of the tumor was in the submucosa, leaving the muscularis propria free from the tumor (Figure 2). Endoscopic enucleation was indicated and written informed consent to the procedure was obtained from all the patients.
Figure 1.
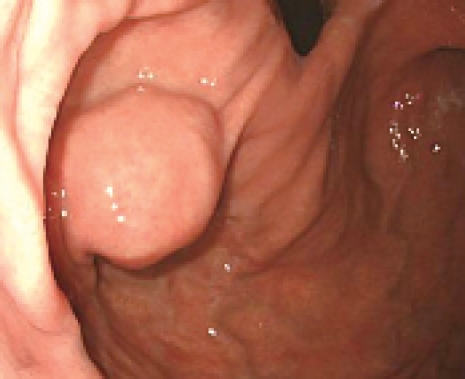
Endoscopic appearance of a subepithelial tumor in the cardia of the stomach.
Figure 2.

Ultrasonography indicated the tumor was confined within the submucosa.
Endoscopic enucleation was carried out as follows: 5-10 ml physiological saline was injected into the submucosa, and the mucosa covering the tumor was removed using a snare or a cutting knife. Then the tumor was dissected from the surrounding tissues (Figure 3A). The tumor was removed completely by snaring its base (Figure 3B). The enucleated lesion was shown in Figure 3C.
Figure 3.
A: Dissection of submucosal tumor after removing the covering mucosa; B: Snaring of the base of the tumor; C: Specimens of the enucleated tumor and its covering mucosa.
Duration of the operation was 18-45 min. (median, 25 min) and no serious complications were encountered. Several days after endoscopic removal of the tumor, oral intake was started without any trouble. Follow-up examinations at 6-8 wk after endoscopic surgery disclosed that the ulcer at the site of the enucleation had healed completely.
Histopathology of the tumor tissue was KIT-positive GISTs with low risk for malignancy (mitotic index, < 5 per 50 high power field) in all of the patients. The patients were disease-free at 10.5-42.5 mo (median, 26.6 mo) after the operation.
DISCUSSION
Reports on endoscopic removal of small GISTs of the stomach have been increasing, but they are mostly documentation of single or a small number of cases[2,5,6]. Park et al[7] have recently reported the experience of endoscopic enucleation of submucosal tumors of the esophagus and the stomach in 15 patients. There were four patients with GISTs of the stomach. Tumor tissue was removed completely in these patients but a small perforation occurred in one patient, in whom the tumor involved the muscularis propria and had grown outward to the serosa. Roesch et al[8] have treated 14 patients with submucosal tumors of the esophagus and the stomach by endoscopic surgery. In their series, there were five patients with GIST of the stomach. No serious complications were encountered in these patients but complete removal was uncertain in two patients with gastric GISTs that originated in the muscularis propria.
These reports, together with our experiences reported here, indicate endoscopic enucleation is a safe and effective method of treatment for most patients with gastric GISTs. Endoscopic enucleation, however, is not indicated if the tumor is > 3 cm in diameter or if involvement of the muscularis propria is suspected from preoperative ultrasonography.
If GIST is completely removed by endoscopic resection and histopathological examination discloses that the risk for malignancy is low, then no further treatment is necessary. However, if resection is incomplete and/or the tumor tissue has a high risk of malignancy, additional wide resection is indicated. At present, whether postoperative imatinib can improve disease-free survival in high-risk patients is still uncertain[9].
Peer reviewer: Rene Lambert, Professor, International Agency for Research on Cancer, 150 Cours Albert Thomas, Lyon 69372 cedex 8, France
S- Editor Liu JN L- Editor Kerr C E- Editor Ma WH
References
- 1.Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O'Leary TJ, Remotti H, Rubin BP, et al. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol. 2002;33:459–465. doi: 10.1053/hupa.2002.123545. [DOI] [PubMed] [Google Scholar]
- 2.Ponsaing LG, Hansen MB. Therapeutic procedures for submucosal tumors in the gastrointestinal tract. World J Gastroenterol. 2007;13:3316–3322. doi: 10.3748/wjg.v13.i24.3316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choi SM, Kim MC, Jung GJ, Kim HH, Kwon HC, Choi SR, Jang JS, Jeong JS. Laparoscopic wedge resection for gastric GIST: long-term follow-up results. Eur J Surg Oncol. 2007;33:444–447. doi: 10.1016/j.ejso.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Iwahashi M, Takifuji K, Ojima T, Nakamura M, Nakamori M, Nakatani Y, Ueda K, Ishida K, Naka T, Ono K, et al. Surgical management of small gastrointestinal stromal tumors of the stomach. World J Surg. 2006;30:28–35. doi: 10.1007/s00268-005-7944-4. [DOI] [PubMed] [Google Scholar]
- 5.Piccinni G, Marzullo A, Angrisano A, Iacobone D, Nacchiero M. Endoscopic resection of benign very low-risk gastric gastrointestinal stromal tumors. Is it enough? Eur J Gastroenterol Hepatol. 2007;19:177–179. doi: 10.1097/01.meg.0000252632.80796.24. [DOI] [PubMed] [Google Scholar]
- 6.Saftoiu A, Ciurea T, Georgescu CV, Comanescu V, Popescu C. Curative endoscopic ultrasound-assisted submucosal resection of a gastric stromal tumor. Rom J Gastroenterol. 2005;14:177–182. [PubMed] [Google Scholar]
- 7.Park YS, Park SW, Kim TI, Song SY, Choi EH, Chung JB, Kang JK. Endoscopic enucleation of upper-GI submucosal tumors by using an insulated-tip electrosurgical knife. Gastrointest Endosc. 2004;59:409–415. doi: 10.1016/s0016-5107(03)02717-2. [DOI] [PubMed] [Google Scholar]
- 8.Rosch T, Sarbia M, Schumacher B, Deinert K, Frimberger E, Toermer T, Stolte M, Neuhaus H. Attempted endoscopic en bloc resection of mucosal and submucosal tumors using insulated-tip knives: a pilot series. Endoscopy. 2004;36:788–801. doi: 10.1055/s-2004-825838. [DOI] [PubMed] [Google Scholar]
- 9.D’Amato G, Steinert DM, McAuliffe JC, Trent JC. Update on the biology and therapy of gastrointestinal stromal tumors. Cancer Control. 2005;12:44–56. doi: 10.1177/107327480501200106. [DOI] [PubMed] [Google Scholar]



