Abstract
The plaque reduction neutralization test (PRNT) is a specific serological test used to identify and confirm arbovirus infection in diagnostic laboratories and monitor immunological protection in vaccine recipients. Wild-type (wt) viruses used in the PRNT may be difficult to grow and plaque titrate, such as the dengue viruses (DENV), and/or may require biosafety level 3 (BSL3) containment, such as West Nile virus (WNV), St. Louis encephalitis virus (SLEV), and Japanese encephalitis virus (JEV). These requirements preclude their use in diagnostic laboratories with only BSL2 capacity. In addition, wt JEV falls under the jurisdiction of the select-agent program and can be used only in approved laboratories. The chimeric vaccine viruses ChimeriVax-WNV and -SLEV have previously been shown to elicit antibody reactivity comparable to that of parental wt WNV and SLEV. ChimeriVax viruses provide advantages for PRNT, as follows: they grow more rapidly than most wt flaviviruses, produce large plaques, require BSL2 conditions, and are not under select-agent restrictions. We evaluated the ChimeriVax-DENV serotype 1 (DENV1), -DENV2, -DENV3, -DENV4, and -JEV for use in PRNT on sera from DENV- and JEV-infected patients and from JEV vaccine recipients. Serostatus agreement was 100% between the ChimeriVax-DENV serotypes and wt prototype DENV and 97% overall with ChimeriVax-JEV compared to prototype Nakayama JEV, 92% in a subgroup of JEV vaccine recipients, and 100% in serum from encephalitis patients naturally infected with JEV. ChimeriVax-DENV and -JEV plaque phenotype and BSL2 requirements, combined with sensitive and specific reactivity, make them good substitutes for wt DENV and JEV in PRNT in public health diagnostic laboratories.
Flaviviruses are medically important pathogens that are significant causes of disease throughout the temperate and tropical regions of the world. In Asia, over 3 billion people live in areas where they are at risk of being infected with Japanese encephalitis virus (JEV), and JEV infections have become the leading cause of pediatric encephalitis in Asia, with as many as 50,000 cases and 15,000 deaths per year (49, 50). The four serotypes of dengue virus (DENV) have emerged in recent years to reach pandistribution throughout the tropics and subtropics of the Americas, Asia, and Africa, resulting in over 100 million dengue fever cases and hundreds of thousands of cases of the more severe dengue hemorrhagic fever/dengue shock syndrome (14-17, 37).
Laboratory diagnosis of flavivirus infection is primarily serological, using detection of virus-specific immunoglobulin M (IgM) in an IgM antibody-capture enzyme-linked immunosorbent assay (MAC ELISA), ideally from paired acute and convalescent specimens but in practice from a single acute-phase serum specimen or cerebrospinal fluid specimen (6, 35, 36, 54). This method is sensitive and relatively specific. However, there is considerable cross-reactivity of antibodies elicited in the immune response to conserved regions of the flavivirus envelope (E) protein, which may cause false-positive results in the MAC ELISA and confound diagnosis in areas where multiple flaviviruses cocirculate (45). Specificity can be improved somewhat through differential diagnosis by cross-testing specimens against multiple flaviviruses simultaneously in a standardized MAC ELISA format, but it may be difficult to distinguish among flaviviruses by MAC ELISA alone, even those from different antigenic complexes such as JEV and DENV (7, 24, 35, 42).
The plaque reduction neutralization test (PRNT) is a specific serological assay that is used at the CDC/Division of Vector-Borne Infectious Diseases (DVBID) diagnostic laboratory to confirm infection and differentiate among flaviviruses in primary flavivirus infections (4, 11, 46-48). Neutralization assays are also used to monitor protective immunity in vaccinees (26, 38). In the PRNT procedure, the serological specimen (generally serum) is mixed with live virus, and if virus-specific neutralizing antibodies are present in the serum, they bind to the virus to form a complex. The mixture is then inoculated onto a monolayer of cells. Virus bound up in an antibody-virus complex is inhibited from infecting the cells; i.e., it is neutralized. Consequently, laboratories conducting these assays must have tissue culture capability, considerable technical expertise in growing and plaque titrating the flaviviruses, which have a wide range of growth rates, and appropriate biosafety level laboratory conditions in which to grow the virus. JEV, West Nile virus (WNV), and St. Louis encephalitis virus (SLEV) require biosafety level 3 (BSL3) containment, which precludes their use in many public health diagnostic laboratories with only BSL2 capacity. In addition, JEV falls under the jurisdiction of the select-agent program and can be used only in select-agent-registered laboratories (8).
Acambis, Inc. (now a part of Sanofi Pasteur), has developed chimeric vaccine viruses for JEV, WNV, SLEV, and the four serotypes of DENV, based on the attenuated yellow fever (YF) vaccine virus 17D (YF-VAX), with the genes encoding the premembrane (prM) and E proteins of the YF 17D virus replaced with those of heterologous flaviviruses, i.e., JEV, WNV, SLEV, and DENV (3, 9, 19, 20, 39). Previously, the ChimeriVax-WNV and -SLEV were shown to be functionally comparable to prototype WNV and SLEV in the PRNT (44). The ChimeriVax viruses have many advantages over the prototype wild-type (wt) viruses in the PRNT; most importantly for this application, they can be used under BSL2 containment. They are plaque purified and produce large-sized, relatively uniform plaques which are phenotypically similar to those of the YF 17D virus but with specific reactivity to the heterologous prM-E protein insert. They grow at relatively the same rate, which has allowed the procedure to be standardized at the CDC/DVBID so that when using multiple flaviviruses in differential diagnosis, the second overlay can be applied to all the PRNT plates on the same day (Table 1). This generally shortens the test duration compared to that of the wt flaviviruses.
TABLE 1.
PRNT90 double agarose overlay procedure, showing the number of days following application of first overlay until application of second overlay
| Virus | Prototype virus overlay
|
ChimeriVax overlay
|
ChimeriVax parental overlay
|
|||
|---|---|---|---|---|---|---|
| Strain | No. of days until second overlay | Virus | No. of days until second overlay | Strain | No. of days until second overlay | |
| DENV1 | Hawaii44 | 7 | ChimeriVax-DENV1 | 4 | PUO359 | 7 |
| DENV2 | NGC | 6 | ChimeriVax-DENV2 | 4 | PUO218 | 6 |
| DENV3 | H-87 | 7 | ChimeriVax-DENV3 | 4 | PaH881/88 | 7 |
| DENV4 | H-241 | 4 | ChimeriVax-DENV4 | 4 | 1228 | 7 |
| JEV | Nakayama | 4 | ChimeriVax-JEV | 4 | SA-14-14-2 | NDa |
ND, not done.
We compared serostatuses and neutralizing antibody titers of the ChimeriVax-DENV serotype 1 (DENV1), -DENV2, -DENV3, -DENV4, and -JEV to those of their counterpart prototype viruses used in the PRNT at the CDC/DVBID. The performance of the ChimeriVax viruses was comparable to that of the prototype viruses in the PRNT, which combined with their facility of use and BSL2 classification, make them advantageous to use in diagnostic laboratories which otherwise would be unable to perform this specific confirmatory diagnostic assay.
MATERIALS AND METHODS
Serum specimens.
A panel of serum specimens without personal identifiers was selected from the CDC/DVBID collection of archived samples, which had been submitted for JEV or DENV diagnostic testing or to monitor protective immunity following JEV or YF virus (YFV) vaccination. In addition, serum specimens from JEV-infected patients were provided by Phan Thi Nga, Department of Virology, National Institute of Hygiene and Epidemiology, Hanoi, Vietnam. Diagnostic specimens had been previously characterized by MAC ELISA and confirmed by PRNT using the prototype DENV and JEV or by virus isolation. Neutralizing antibody titer had been determined previously in the serum specimens from vaccine recipients by PRNT, using the prototype viruses.
Viruses.
The following prototype viruses used in the PRNTs were obtained from the CDC/DVBID virus reference collection: DENV1 (Hawaii, 1944 [Hawaii44]), DENV2 (New Guinea C, 1944 [NCG]), DENV3 (Philippines, 1956 [H-87]), DENV4 (Philippines, 1956 [H-241]), and JEV (Nakayama, Japan, 1935 [Nakayama]) (53). The ChimeriVax-DENV1, -2, -3, and -4 and the parental wt DENV strains on which the ChimeriVax-DENV are based (DENV1 PUO359, DENV2 PUO218, DENV3 PaH881/88, and DENV4 1228) were supplied by Acambis, Inc. (Cambridge, MA) (18-21, 40). The ChimeriVax-JEV, constructed to contain the prM-E genes from JEV SA14-14-2, the live-virus vaccine strain developed in China, was also supplied by Acambis (20, 57).
The prototype DENV were grown in 25-cm2 flasks with Dulbecco modified Eagle medium (for a closed system) on C6/36 cells at 33°C. The supernatant was harvested on the fifth day; no cytopathic effect was observed. Cellular debris was removed from the supernatant by centrifugation at 3,500 × g for 30 min. Fetal bovine albumin was added to the clarified supernatant to a final concentration of 20%. The seeds were aliquoted and stored at −70°C.
The ChimeriVax virus seeds were prepared in Vero cells in Dulbecco modified Eagle medium with 2% fetal bovine serum. The supernatant was harvested on day 3 or 4, and cellular debris was removed by centrifugation at 3,000 × g for 30 min. The working stock ChimeriVax virus was stored with 20% fetal bovine serum at −70°C. ChimeriVax-JEV was passaged once in Vero cells from lyophilized JEV vaccine manufactured by Acambis; the ChimeriVax-DENV working stock was passaged twice in Vero cells. YFV was not used in the PRNT reported here because we have repeatedly shown that the ChimeriVax viruses with heterologous (e.g., DENV, JEV) prM-E genes are not neutralized by YF-specific antibodies and do not induce neutralizing antibodies to YFV (39).
PRNT.
All the PRNTs were completed by one Clinical Laboratory Improvement Amendments-certified technician, who routinely performs neutralization assays in the CDC/DVBID arbovirus diagnostic laboratory. Each sample was tested simultaneously with the prototype and ChimeriVax viruses. Each test run was validated with a standardized virus-specific mouse hyperimmune ascitic fluid (MHIAF)-positive control and compared against the virus back titration. Because the evaluation was designed to simulate diagnostic testing conditions and protocol in which the specimens would normally be tested once, replicate testing was not done unless noted.
Virus-specific neutralizing antibody titers were determined by 90% endpoint PRNT (PRNT90) in 6-well plates with Vero cells, using a 0.5% agarose double overlay and visualized with neutral red staining in the second overlay (4). Samples were first heat inactivated at 56°C for 30 min to destroy the complement and to inactivate adventitious viruses, so as to make a fair comparison between paired samples; non-heat-inactivated normal human sera added to the serum-virus mixture at a concentration of 4% provided a source of labile serum factor. Second overlays were applied on days 4 to 7 (Table 1).
Neutralizing antibody titer is expressed as the reciprocal of the endpoint serum dilution that reduced the challenge virus plaque count by 90%, based on the back titration. In differential PRNT, in which specimens were tested simultaneously for two or more viruses, a neutralizing titer of fourfold or higher for one virus compared to those of the others was considered virus specific, except in tests in which the neutralizing antibodies reacted to all the flaviviruses tested (7). Extensive antibody cross-reactivity among challenge viruses in the PRNT is an indication of a secondary flavivirus infection, and identification of the infecting flavivirus could not be made with these specimens.
Statistical analyses.
Of primary importance was the serostatus of the sample under testing, using the prototype viruses and using the ChimeriVax viruses. Because the serostatus outcome is binary, agreement between the prototype virus and the ChimeriVax virus was assessed using the kappa statistic for intraclass correlation (13). Antibody cross-reactivity to the prototype DENV was compared to that of the ChimeriVax-DENV by comparing how frequently a heterologous (cross-reactive) titer indicated positivity (even if the homologous titer was fourfold greater, indicating a correct diagnosis). A noninferiority test for proportions (34) was then used to determine whether the ChimeriVax-DENV produced more cross-reactive results than the prototype DENV. A secondary question asked how similar the neutralizing antibody titers were against the prototype viruses and the ChimeriVax viruses. For comparing antibody titers in the DENV PRNT evaluation, titers were modeled as a function of strain, test serotype, and whether the test was homologous or heterologous using generalized estimating equations (GEEs). We chose to use GEEs because the titers against DENV had a complex covariance structure that could be made explicit in the GEE framework. In the JEV PRNT comparison, the titers were modeled using a linear model. A linear model not only estimates the strength of the relationship between the chimeric and wt titers but, unlike a simple correlation, also can identify a scaling factor between the titers.
RESULTS
DENV PRNT.
The sample set used in the DENV PRNT evaluation consisted of 48 serum specimens from 33 primary DENV infections (15 DENV1, 12 DENV2, 3 DENV3, and 3 DENV4); 3 secondary DENV infections; 6 other flavivirus infections (3 WNV, 3 YFV vaccinated), and 6 flavivirus-negative controls. These specimens had been characterized previously by MAC ELISA and PRNT and/or virus isolation or viral RNA detection (4, 10, 30, 35, 36).
Initially, each specimen was tested simultaneously against the four prototype DENV serotypes, the four ChimeriVax-DENV serotypes, and the four ChimeriVax parental DENV strains (Table 2). Because each specimen was tested in 12 six-well plates at a time, the samples were tested in five batches, with standardized positive and negative controls. The positive specimens were retested with the homologous prototype DENV, ChimeriVax DENV, and ChimeriVax parental DENV together in one replicate to confirm uniformity of the five tests (data not shown). Because of the limited sample volume available and the number of different viruses against which each sample was tested, initial serum dilutions of 1:10 and working serum dilutions of 1:20 were used for the dengue test specimens. Therefore, the lower limit of quantification (LLOQ) for this group was a neutralizing antibody titer of 20.
TABLE 2.
Comparison of neutralizing antibody titers using prototype DENV, ChimeriVax-DENV, and ChimeriVax-DENV parental strains in PRNT90
| Specimen type (no. of samples) | Specimen no. | Neutralizing antibody titers in PRNT90a
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prototype DENV
|
ChimeriVax-DENV
|
ChimeriVax-DENV parental strains
|
|||||||||||
| DENV1 | DENV2 | DENV3 | DENV4 | DENV1 | DENV2 | DENV3 | DENV4 | DENV1 | DENV2 | DENV3 | DENV4 | ||
| DENV1 infection (15) | 1 | 1,280 | — | — | — | 5,120 | 40 | — | — | 160 | — | — | — |
| 2 | 1,280 | 40 | — | — | 640 | 40 | 20 | — | 160 | — | 20 | — | |
| 3 | 640 | — | — | — | 80 | 20 | — | — | 160 | — | — | — | |
| 4 | 160 | — | — | — | 320 | — | — | — | 20 | — | — | — | |
| 5 | 160 | — | — | — | 160 | — | — | — | 160 | — | — | — | |
| 6 | 160 | — | — | — | 80 | — | — | — | 80 | — | — | — | |
| 7 | 320 | — | — | — | 2,560 | 40 | 40 | 20 | 320 | — | — | — | |
| 8 | 1,280 | — | 40 | 20 | 320 | 80 | 80 | 20 | 640 | — | 40 | — | |
| 9 | 40 | — | — | — | 40 | — | — | — | 40 | — | — | — | |
| 10 | 320 | — | — | — | 640 | — | — | — | 160 | — | — | — | |
| 11 | 320 | — | — | 20 | 640 | 20 | 20 | — | 320 | — | 20 | — | |
| 12 | 640 | 40 | 20 | 20 | 1,280 | 80 | 40 | — | 640 | — | 20 | — | |
| 13 | 80 | ND | ND | ND | 160 | ND | ND | ND | 160 | ND | ND | ND | |
| 14 | 40 | — | — | — | 640 | 20 | — | — | 160 | — | — | — | |
| 15 | 20 | — | — | — | 80 | 20 | — | — | 40 | — | — | — | |
| DENV2 infection (12) | 16 | 20 | 320 | — | — | — | 640 | — | — | — | 160 | — | — |
| 17 | 40 | 160 | — | — | — | 320 | — | — | — | 80 | — | — | |
| 18 | 40 | 640 | — | — | — | 640 | 20 | — | — | 320 | — | — | |
| 19 | 160 | 640 | 20 | — | 40 | 640 | 40 | 40 | 20 | 320 | 20 | — | |
| 20 | 40 | 320 | — | — | — | 320 | — | — | — | 80 | — | — | |
| 21 | — | 80 | — | — | — | 160 | — | — | — | 80 | — | — | |
| 22 | — | 160 | — | — | — | 320 | — | — | — | 320 | — | — | |
| 23 | 20 | 320 | — | 20 | — | 320 | 20 | — | — | 160 | 20 | — | |
| 24 | 20 | 320 | — | — | — | 1,280 | — | — | 20 | 160 | — | — | |
| 25 | — | 160 | — | — | — | 640 | — | — | — | 40 | — | — | |
| 26 | — | 320 | — | — | — | 1,280 | — | — | — | 320 | — | — | |
| 27 | — | 640 | — | — | — | 1,280 | — | — | — | 320 | — | — | |
| DENV3 infection (3) | 28 | — | — | — | — | — | — | — | — | — | — | — | — |
| 29 | — | — | 40 | — | — | — | 40 | — | — | — | 80 | — | |
| 30 | 20 | — | 160 | — | 20 | — | 320 | — | — | — | 160 | — | |
| DENV4 infection (3) | 31 | — | — | — | 1,280 | — | — | — | 160 | — | — | — | 320 |
| 32 | — | 20 | — | 320 | — | 20 | — | 160 | — | — | — | 320 | |
| 33 | — | 40 | — | 5,120 | — | 20 | — | 2,560 | — | — | — | 5,120 | |
| Secondary DENV infection (3) | 34 | 1,280 | 640 | 640 | 640 | 640 | 1,280 | 320 | 640 | 1,280 | 320 | 640 | 80 |
| 35 | 5,120 | 2,560 | 5,120 | 5,120 | 5,120 | 10,240 | 2,560 | 5,120 | 5,120 | 1,280 | 10,240 | 1,280 | |
| 36 | 10,240 | 5,120 | 10,240 | 40,960 | 5,120 | 20,480 | 5,120 | 40,960 | 10,240 | 2,560 | 20,480 | 10,240 | |
| WNV infection (3) | 37-39 | — | — | — | — | — | — | — | — | — | — | — | — |
| YFV vaccinated (3) | 40-42 | — | — | — | — | — | — | — | — | — | — | — | — |
| All flavivirus negative (6) | 43-48 | — | — | — | — | — | — | — | — | — | — | — | — |
| Positive controlsb | |||||||||||||
| DENV1 | 640 (5,120) | (80) | (160) | (80) | 2,560 (2,560) | (80) | (320) | (160) | 1,280 (320) | (20) | (40) | (—) | |
| DENV2 | (320) | 1,280 (1,280) | (80) | (160) | (160) | 2,560 (2,560) | (160) | (80) | (—) | 640 (80) | (—) | (—) | |
| DENV3 | (320) | (160) | 1,280 (1,280) | (160) | (320) | (160) | 640 (2,560) | (80) | (80) | (40) | 1,280 (320) | (—) | |
| DENV4 | (160) | (80) | (80) | 5,120 (5,120) | (160) | (80) | (80) | 2,560 (2,560) | (—) | (—) | (—) | 1,280 (80) | |
| Negative controlc | — | — | — | — | — | — | — | — | — | — | — | — | |
The neutralizing antibody titer is expressed as the reciprocal of the endpoint serum dilution that neutralized the challenge virus plaque count by 90%. LLOQ has a neutralizing antibody titer of 20; only positive titers (≥20) are shown. Dash = no detectable titer (<20). A neutralizing titer difference of more than fourfold between antibody to the homologous DENV serotype and antibodies to the other DENV serotypes indicates a DENV serotype-specific antibody response. The neutralizing antibody titers in parentheses are the results of the initial evaluations of the MHIAF samples using each of the four DENV serotypes as challenge viruses. These titers are shown to illustrate the level of cross-reactivity of the MHIAF samples to the other DENV serotypes. ND, not done due to insufficient sample volume.
MHIAF produced against a single DENV serotype.
Normal human control serum.
Overall serostatus agreement of each of the ChimeriVax-DENV serotypes compared to those of the prototype wt DENV serotypes and ChimeriVax parental wt DENV was 100% (Table 2). The kappa statistic for intraclass correlation was 1, with a P value of <0.01 and a lower 95% confidence bound of 0.89, showing a strong, positive correlation. The noninferiority test from Liu et al. (34) indicated that the antibody cross-reactivity of the DENV serotypes observed with the ChimeriVax-DENV was not greater than the cross-reactivity observed with the prototype DENV (P = 0.02). It should be noted that one of the specimens originally classified as a DENV3 infection showed no neutralizing titer with either the chimeric or the prototype DENV3.
GEE results failed to show a statistically significant difference in neutralizing antibody titers among the ChimeriVax-DENV, the prototype DENV, or the ChimeriVax-DENV parental strains (P = 0.12). However, this statistical test is designed to detect a difference in titers, and therefore, caution must be exercised with interpreting this finding. The fact that no statistically significant difference was found may suggest that, after adjusting for other effects, the two strains produce the same mean neutralizing antibody titers. However, on its own, it is not conclusive. We include this result not only to illustrate that the ChimeriVax-DENV and prototype DENV have similar agreement in the final diagnosis but also to show that there is some evidence that the resultant antibody titers are similar on a log scale.
In the three secondary DENV infections (specimens 34 to 36) (Table 2), the infecting DENV serotype could not be differentiated by either the ChimeriVax-DENV or prototype DENV, as the neutralizing antibody was highly reactive to all ChimeriVax-DENV and prototype DENV serotypes.
JEV PRNT.
A total of 100 serum specimens were used in the side-by-side PRNT comparison of ChimeriVax-JEV and JEV Nakayama (Table 3). Fifty-five serum specimens were banked specimens collected from individuals that had received JEV (Biken) or YFV vaccines, and these sera had been screened previously by PRNT with JEV Nakayama to monitor protective immunity (Table 3). Twenty-six specimens had JEV-specific neutralizing titers; 29 did not have detectable JEV-specific titers. Fourteen specimens were from encephalitis patients from Vietnam, which had been previously classified as recent JEV infections by JEV MAC ELISA and PRNT (Table 3). Serum specimens from persons with heterologous flavivirus infections included nine DENV, three WNV, three YFV (one natural infection and two vaccine recipients), and eight specimens that were classified as secondary flavivirus infections in which the infecting virus could not be determined (Table 3). Ten specimens had been submitted as suspected JEV infections based on travel to countries where JEV is endemic. In the initial diagnostic testing, these specimens had JEV-positive or equivocal MAC ELISA results but were JEV negative by PRNT against JEV Nakayama (Table 3). Each specimen was tested simultaneously against JEV Nakayama and ChimeriVax-JEV in three groups (Table 3), and each group included standardized positive and negative controls. The initial serum dilution was 1:5, and the LLOQ was 10.
TABLE 3.
Comparison of neutralizing antibody titers using prototype JEV (Nakayama) and ChimeriVax-JEV in PRNT90
| Specimen type (no. of samples) | Specimen no. | Neutralizing antibody titers in PRNT90a
|
|
|---|---|---|---|
| Prototype JEV Nakayama | ChimeriVax-JEV | ||
| JEV vaccinated (55) | 1 | 1,280 | 1,280 |
| 2 | 640 | 320 | |
| 3 | 640 | 1,280 | |
| 4 and 5 | 160 | 160 | |
| 6 | 160 | 320 | |
| 7 | 160 | 80 | |
| 8 and 9 | 160 | 40 | |
| 10 and 11 | 80 | 40 | |
| 12 | 40 | 40 | |
| 13 | 40 | 20 | |
| 14 | 20 | 20 | |
| 15 and 16 | 20 | — | |
| 17-20 | 40 | 10 | |
| 21-26 | 10 | 10 | |
| 27-55 | — | — | |
| JEV infection (14) | 56 | 2,560 | 20,480 |
| 57 | 5,120 | 10,240 | |
| 58 | 1,280 | 10,240 | |
| 59 | 2,560 | 5,120 | |
| 60 | 640 | 5,120 | |
| 61 | 640 | 2,560 | |
| 62 | 640 | 1,280 | |
| 63 and 64 | 320 | 1,280 | |
| 65 and 66 | 160 | 1,280 | |
| 67 and 68 | 640 | 640 | |
| 69 | 320 | 320 | |
| Other flavivirus infections (21) | |||
| DENV infection (9) | 70-78 | — | — |
| WNV infection (1) | 79 | — | — |
| YFV infection (3) | 80-82 | — | — |
| Past or secondary flavivirus infection (8) | 83 | 320 | 640 |
| 84 | — | 10 | |
| 85-90 | — | — | |
| All flavivirus negative (10) | 91-99 | — | — |
| 100 | — | 20 | |
| Positive control—JEV vaccine serumb | 1,280 | 320 | |
| Negative controlc | — | — | |
The neutralizing antibody titer is expressed as the reciprocal of the endpoint serum dilution that neutralized the challenge virus plaque count by 90%. LLOQ has a neutralizing antibody titer of 10; only positive titers (≥10) are shown. Dash = no detectable titer (<10).
MHIAF produced against JEV Nakayama strain.
Normal human control serum.
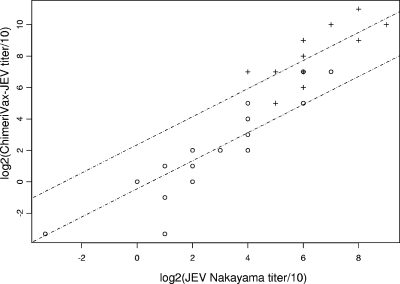
With respect to indicating a positive or negative result, agreement between the prototype JEV Nakayama and ChimeriVax-JEV was high, at 96% (96/100). The kappa statistic for intraclass correlation was 0.92 (P < 0.01), with a lower 95% confidence bound of 0.76. In the vaccinated subgroup (n = 55), serostatus agreement between JEV Nakayama and ChimeriVax-JEV was 92% (Table 3). Of those with a detectable neutralizing antibody titer against JEV Nakayama (n = 26), 50% (13/26) had a higher titer against JEV Nakayama, 7.6% (2/26) had a higher titer against ChimeriVax-JEV, and 42.3% (11/26) had equivalent titers. Serostatus agreement between JEV Nakayama and ChimeriVax-JEV was 100% within the subgroup of persons with naturally acquired JEV infections from Vietnam (Table 3). Of these, 78.6% (11/14) had higher titers against ChimeriVax-JEV, none had a higher titer against JEV Nakayama, and 21.4% (3/14) had equivalent titers. When the ChimeriVax-JEV log2 (ChimeriVax-JEV titer/10) is regressed on the prototype JEV log2 (prototype JEV titer/10) and strain, the titer with ChimeriVax-JEV is, on average, approximately 2 logs higher than the titer with JEV Nakayama for the JEV-infected group (P < 0.01; 95% confidence interval [CI] of 1.69 to 3.03). Additionally, in the JEV-vaccinated group, the ChimeriVax-JEV log2 (ChimeriVax-JEV titer/10) is slightly less than the prototype JEV log2 (prototype JEV titer/10) (the 95% CI for their ratio is 0.82 to 0.97) (Fig. 1).
FIG. 1.
Linear regression of log2 of ChimeriVax-JEV titer/10 (y axis) on log2 of prototype JEV titer/10 (x axis). JEV-vaccinated samples are represented by circles; samples with natural JEV infections are represented by plus signs. The slopes of the regression lines through the two groups are slightly less than 1 (95% CI is 0.82 to 0.97). There is no statistical difference between the two slopes (P = 0.89). However, the difference between the regression lines is statistically significant (P < 0.01; 95% CI for difference on the log scale is 1.69 to 3.03). Together, these results suggest that, on average, titers against ChimeriVax-JEV and JEV Nakayama are approximately equal in the vaccinated group, but in the naturally infected group, the titers against ChimeriVax-JEV are about 2 logs greater than those against JEV Nakayama.
DISCUSSION
Diagnostic testing for arbovirus infections has increased in the United States since the introduction of WNV in 1999 and globally through laboratory-based surveillance projects designed to aid countries with making decisions on implementation of vaccine and/or arbovirus control programs. Combined with the increase in the number of tests, laboratories are also expanding the repertoire of diagnostic assays that they routinely carry out in order to improve detection. Virus-specific MAC ELISA has been the primary serological test for detecting arbovirus infection when a single acute serological specimen is obtained. The MAC ELISA is sensitive, as IgM antibody is produced early in infection and is detectable within a few days from illness onset, and is more virus specific than IgG antibody (27, 28, 36, 54-56). However, in flavivirus infections, antibodies elicited against conserved epitopes on the immunogenic envelope protein may cross-react with other flaviviral antigens in the MAC ELISA, which can cause false-positive results (45). PRNT is a specific, quantitative assay which measures the amount of virus-specific neutralizing antibody present in the serum and is used to confirm infection and differentiate cross-reactive MAC ELISA results.
Acute serological specimens received by the CDC/DVBID arbovirus diagnostic laboratory are initially tested by MAC ELISA against selected arboviruses circulating in a geographical area to which the patient may have been exposed (4, 32, 35, 36, 46). Positive or equivocal MAC ELISA results are confirmed by PRNT. (An equivocal MAC ELISA result with a negative PRNT titer is considered negative.) In differential diagnosis, in which the specimens are tested for multiple flaviviruses, cross-reactive results in the MAC ELISA are resolved by PRNT.
Neutralization assays are also used to monitor protective immunity in JEV vaccine recipients. WHO vaccine guidelines consider a neutralizing antibody titer of 10 in a PRNT50 to be protective (26, 53). The more stringent PRNT90 is used in the CDC/DVBID diagnostic laboratory for both monitoring immune protection and confirmatory testing of clinical specimens, as low-level cross-reactivity may result in false positives in the PRNT50. This is especially important for making a differential diagnosis between closely related, cocirculating flaviviruses, such as between WNV and SLEV or JEV and WNV.
PRNT using wt flaviviruses can be technically difficult, as many flaviviruses grow slowly and have pinpoint-sized plaque phenotypes. Prototype viruses may be comprised of mixed populations, or quasispecies, which grow at different rates and produce plaques of various sizes. The difficulties are compounded in differential PRNT when specimens are tested against multiple flaviviruses simultaneously, such as with the four DENV serotypes reported here. The prototype DENV2 NCG and DENV4 H-241 produce medium-sized plaques and grow relatively quickly, with second overlays applied on days 6 and 4, respectively. However, DENV1 Hawaii44 and DENV3 H-87 grow more slowly and produce diffuse plaques of various sizes, which are difficult to visualize even 2 days after the second overlay application at day 7. Thus, using the four prototype DENV in the PRNT requires application of the second agarose overlay on three different days (Table 1). The ChimeriVax-DENV grow at relatively the same rate, generally more rapidly than the prototypes, so that in differential PRNT using multiple ChimeriVax viruses, the second overlays can all be applied on the same day, which simplifies the overlay procedure and shortens the test (Table 1). They also produce larger, more-uniform plaques which are more readily visualized soon after neutral red staining compared to the prototype DENV.
JEV prototype Nakayama strain produces medium-sized, easy-to-read plaques, following application of the second agarose overlay on day 4. However, the American Committee on Arthropod-Borne Viruses has classified wt JEV as a BSL3 agent which must be used under BSL3 containment (23). In addition, wt JEV is under U.S. Department of Agriculture select-agent restrictions and can be used only in registered laboratories (8). The ChimeriVax viruses require only BSL2 containment, are not under select-agent restrictions, and can be used in most public health laboratories with tissue culture capabilities. For these reasons, we evaluated the ChimeriVax-JEV and -DENV to determine if they could replace the prototype JEV and DENV in routine diagnostic neutralization assays.
Prototype DENV and ChimeriVax-DENV were compared in differential PRNTs, in which the specimens were tested against all four DENV serotypes simultaneously in a panel of 48 serum specimens from primary and secondary DENV infections and suspected flavivirus infection cases (Table 2). The parental strains of DENV from which the ChimeriVax-DENV viruses were constructed were also included in the evaluation to control for any DENV strain differences. Although neutralizing antibody reactivities to the parental DENV strains have been characterized in ChimeriVax-DENV vaccine trials, they have not been used as challenge viruses in PRNT with diagnostic specimens. Isolated from human classical dengue fever cases in Thailand (DENV1 PUO359, DENV2 PUO218, and DENV3 PaH881/88) and Indonesia (DENV4 1228), these parental DENV strains were difficult to plaque titrate (18, 21). They grew slowly, with the second agarose overlay applied on day 6 or 7, and produced very small plaques. The lower neutralizing antibody titers using DENV1 PUO359 and DENV2 PUO218 compared to those of ChimeriVax-DENV1 and -2 may have been due to the unfamiliarity of using these strains in PRNT. However, serostatus agreement among the ChimeriVax-DENV parental strain, ChimeriVax-DENV, and the prototype DENV was 100%, indicating that the anti-DENV neutralizing antibodies in the test specimens effectively reacted with ChimeriVax-DENV parental strains and therefore with the ChimeriVax-DENV.
ChimeriVax-JEV was compared to the prototype JEV Nakayama strain in a group of 100 serum specimens from JEV or YFV vaccinees, a JEV outbreak in Vietnam, and suspected JEV or other flavivirus infection cases. Serostatus agreement between ChimeriVax-JEV and JEV Nakayama was 92% among the 55 JEV vaccine recipients (Table 3). In this subset, there were 26 specimens with neutralizing antibody titers against JEV Nakayama. ChimeriVax-JEV failed to detect neutralizing antibody in two of these specimens, although the titers were also low in both of the specimens against JEV Nakayama. Generally, the neutralizing antibody titers were higher against JEV Nakayama than ChimeriVax-JEV in the vaccine recipient subset (Table 3 and Fig. 1). This was not unexpected, as studies monitoring immunological protection by PRNT in JEV vaccine trials have shown that using JEV strains homologous to the JEV vaccine result in higher titers than using heterologous JEV strains (12, 26, 39). Furthermore, cross-neutralization studies have demonstrated that there are significant differences in neutralization titers between strains within a flavivirus species, based on the degree of homology between the strain used to produce polyclonal antibody and the reference strain used as the challenge virus in the PRNT (1, 2, 7). Serum specimens in this subset were from individuals that had been vaccinated with the Biken JEV vaccine, which is an inactivated vaccine prepared from the Nakayama strain. Therefore, it would be expected that serum from the vaccine recipients would be more reactive to the homologous JEV Nakayama strain than to the ChimeriVax-JEV, which contains the prM-E genes from a different strain (SA14-14-2) (12, 25, 33, 39, 51).
In general, the neutralizing antibody titers in the vaccinee subset were low with both JEV Nakayama and ChimeriVax-JEV, and no neutralizing antibody titer was detected with either the JEV Nakayama or ChimeriVax-JEV in 29 of 55 of the vaccinees in that subset (specimens 27 to 55) (Table 3). Annual monitoring of the protective immunity among vaccine recipients who are otherwise seldom exposed to flaviviruses, such as residents of the United States, has shown that neutralizing antibody titers may be very low to undetectable, although the person may still be protected (26, 53). ChimeriVax-JEV may be less sensitive for detecting neutralizing antibody titer in JEV Biken vaccinees in which the titer is close to the detection threshold. However, it is notable how little difference there was between the titers measured with JEV Nakayama and those with ChimeriVax-JEV. ChimeriVax-JEV has been optimized at the CDC/DVBID for use in neutralization assays to monitor immune protection in JEV vaccinees by lowering the LLOQ, which increased serostatus agreement to 100% compared to that of JEV Nakayama (data not shown).
In the subset of specimens from the JEV outbreak in Vietnam (n = 14), other flavivirus primary (n = 13) and secondary (n = 8) infections and suspected flavivirus infections (n = 10) of ChimeriVax-JEV showed high serostatus agreement with JEV Nakayama. In these groups of specimens, the neutralizing titers were significantly higher against ChimeriVax-JEV than against JEV Nakayama (Table 3 and Fig. 1). JEV Nakayama, isolated in Japan in 1935, and SA14-14-2, an attenuated strain of SA-14 which was isolated in China in 1954, are both grouped in JEV genotype III based on phylogenetic analysis (1, 2, 12, 22, 38, 39, 51, 52). Historically, isolates from Vietnam have also clustered into genotype III, with slightly higher homology to SA-14 than to Nakayama. However, JEV isolates from JEV outbreaks in Vietnam in 2001 and 2002 showed a shift to genotype I (41). The specimens from Vietnam used in this evaluation were obtained from JEV outbreaks in 2004 and 2005. Whether the difference between antibody reactivity in these sera to ChimeriVax-JEV and JEV Nakayama was due to greater nucleotide sequence homology of the parental ChimeriVax-JEV strain (SA14-14-2) to the JEV strains circulating in Vietnam than to JEV Nakayama cannot be determined, as a JEV isolate was not obtained from these specimens (40).
Infection with one flavivirus does not necessarily confer protective immunity against infection by a heterologous flavivirus (43). Consequently, secondary flavivirus infections are common in individuals who live in areas where multiple flaviviruses cocirculate. PRNT may not be a virus-specific diagnostic assay in sera from patients with secondary flavivirus infections, as antibodies from the primary and secondary infection may both react to the challenge flavivirus, whether it is the infecting virus or not. This antibody cross-reactivity results in high titers to all the flaviviruses used in the differential PRNT or in a titer which is higher to the primary flavivirus infection than to the infecting flavivirus, indicating the phenomenon of “original antigenic sin” (29, 43). A differential diagnosis cannot be made by PRNT in these cases, even if there is a difference of fourfold between titers. However, these results are diagnostically informative to indicate evidence of a secondary flavivirus infection (7). The four DENV serotypes are considered four separate flavivirus species, and consistent with the secondary flavivirus infection PRNT profile, the neutralizing antibody titers were high against all the prototype DENV and ChimeriVax-DENV serotypes in sera from secondary dengue infections (samples 34 to 26) (Table 2) (5, 31). In these types of specimens, identification of the infecting DENV serotype would not be possible by using PRNT with either the prototype DENV or ChimeriVax-DENV.
ChimeriVax-WNV and -SLEV are powerful diagnostic tools which have proved useful in resolving cross-reactive results between WNV and SLEV in the MAC ELISA. As reported here, the ChimeriVax-DENV and -JEV have also been shown to have comparable performance with the prototype DENV and JEV currently in use in the PRNT. The BSL2 classification, uniform growth rates, and easy-to-read plaque phenotypes of the ChimeriVax viruses facilitate performing PRNT in public health diagnostic laboratories, particularly for differential diagnosis. The addition of ChimeriVax-DENV and -JEV to the reagent repertoire for use in the PRNT and distribution by the CDC to public health laboratories will further enhance diagnostic laboratory capacity.
Acknowledgments
We thank Phan Thi Nga from the Department of Virology at the National Institute of Hygiene and Epidemiology in Hanoi, Vietnam, for providing the specimens used in the JEV PRNT.
Footnotes
Published ahead of print on 20 May 2009.
REFERENCES
- 1.Ali, A., and A. Igarashi. 1997. Antigenic and genetic variations among Japanese encephalitis virus strains belonging to genotype 1. Microbiol. Immunol. 41241-252. [DOI] [PubMed] [Google Scholar]
- 2.Ali, A., A. Igarashi, L. R. Paneru, F. Hasebe, K. Morita, M. Takagi, W. Suwonkerd, Y. Tsuda, and Y. Wada. 1995. Characterization of two Japanese encephalitis virus strains isolated in Thailand. Arch. Virol. 1401557-1575. [DOI] [PubMed] [Google Scholar]
- 3.Arroyo, J., C. A. Miller, J. Catalan, and T. P. Monath. 2001. Yellow fever vector live-virus vaccines: West Nile virus vaccine development. Trends Mol. Med. 7350-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beaty, B., C. Calisher, and R. Shope. 1995. Arboviruses, p. 189-212. In E. Lennette, D. Lennette, and E. Lennette (ed.), Diagnostic procedures for viral, rickettsial, and chlamydial infections, 7th ed. American Public Health Association, Washington, DC.
- 5.Burke, D., and T. P. Monath. 2001. Flaviviruses, p. 1043-1125. In D. Knipe and P. Howley (ed.), Fields virology, 4th ed., vol. 1. Lippincott Williams and Wilkins, Philadelphia, PA. [Google Scholar]
- 6.Burke, D. S., A. Nisalak, and M. A. Ussery. 1982. Antibody capture immunoassay detection of Japanese encephalitis virus immunoglobulin M and G antibodies in cerebrospinal fluid. J. Clin. Microbiol. 161034-1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calisher, C. H., N. Karabatsos, J. M. Dalrymple, R. E. Shope, J. S. Porterfield, E. G. Westaway, and W. E. Brandt. 1989. Antigenic relationships between flaviviruses as determined by cross-neutralization tests with polyclonal antisera. J. Gen. Virol. 7037-43. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention, Department of Health and Human Services. 2001. Requirements for facilities transferring or receiving select agents. Final rule. Fed. Regist. 6645944-45945. [PubMed] [Google Scholar]
- 9.Chambers, T. J., A. Nestorowicz, P. W. Mason, and C. M. Rice. 1999. Yellow fever/Japanese encephalitis chimeric viruses: construction and biological properties. J. Virol. 733095-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chao, D.-Y., B. S. Davis, and G.-J. Chang. 2007. Development of multiplex real-time reverse transcriptase PCR assays for detecting eight medically important flaviviruses in mosquitoes. J. Clin. Microbiol. 45584-589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dulbecco, R., M. Vogt, and A. G. Strickland. 1956. A study of the basic aspects of neutralization of two animal viruses, western equine encephalitis virus and poliomyelitis virus. Virology 2162-205. [DOI] [PubMed] [Google Scholar]
- 12.Ferguson, M., S. Johnes, L. Li, A. Heath, and A. Barrett. 2008. Effect of genomic variation in the challenge virus on the neutralization titres of recipients of inactivated JE vaccines—report of a collaborative study on PRNT50 assays for Japanese encephalitis virus (JE) antibodies. Biologicals 36111-116. [DOI] [PubMed] [Google Scholar]
- 13.Fleiss, J. L. 1981. Statistical methods for rates and proportions, 2nd ed. John Wiley & Sons, New York, NY.
- 14.Gubler, D. J. 2006. Dengue/dengue haemorrhagic fever: history and current status. Novartis Found. Symp. 2773-16; discussion, 16-22, 71-73, 251-253. [DOI] [PubMed] [Google Scholar]
- 15.Gubler, D. J. 1998. Epidemic dengue and dengue hemorrhagic fever: a global public health problem in the 21st century, p. 1-14. In W. Scheld, D. Armstrong, and J. Hughes (ed.), Emerging infections, vol. 1. ASM Press, Washington, DC. [Google Scholar]
- 16.Gubler, D. J. 2002. The global emergence/resurgence of arboviral diseases as public health problems. Arch. Med. Res. 33330-342. [DOI] [PubMed] [Google Scholar]
- 17.Gubler, D. J. 1998. The global pandemic of dengue/dengue haemorrhagic fever: current status and prospects for the future. Ann. Acad. Med. Singapore 27227-234. [PubMed] [Google Scholar]
- 18.Guirakhoo, F., J. Arroyo, K. V. Pugachev, C. Miller, Z. X. Zhang, R. Weltzin, K. Georgakopoulos, J. Catalan, S. Ocran, K. Soike, M. Ratterree, and T. P. Monath. 2001. Construction, safety, and immunogenicity in nonhuman primates of a chimeric yellow fever-dengue virus tetravalent vaccine. J. Virol. 757290-7304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guirakhoo, F., K. Pugachev, J. Arroyo, C. Miller, Z. X. Zhang, R. Weltzin, K. Georgakopoulos, J. Catalan, S. Ocran, K. Draper, and T. P. Monath. 2002. Viremia and immunogenicity in nonhuman primates of a tetravalent yellow fever-dengue chimeric vaccine: genetic reconstructions, dose adjustment, and antibody responses against wild-type dengue virus isolates. Virology 298146-159. [DOI] [PubMed] [Google Scholar]
- 20.Guirakhoo, F., Z. X. Zhang, T. J. Chambers, S. Delagrave, J. Arroyo, A. D. Barrett, and T. P. Monath. 1999. Immunogenicity, genetic stability, and protective efficacy of a recombinant, chimeric yellow fever-Japanese encephalitis virus (ChimeriVax-JE) as a live, attenuated vaccine candidate against Japanese encephalitis. Virology 257363-372. [DOI] [PubMed] [Google Scholar]
- 21.Guirakhoo, R., R. Weltzin, T. Chambers, Z.-X. Zhang, K. Soike, M. Ratterree, J. Arroyo, K. Georgakopoulos, J. Catalan, and T. Monath. 2000. Recombinant chimeric yellow fever-dengue type 2 virus is immunogenic and protective in nonhuman primates. J. Virol. 745477-5485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Halstead, S. B., and J. Jacobson. 2003. Japanese encephalitis. Adv. Virus Res. 61103-138. [DOI] [PubMed] [Google Scholar]
- 23.HHS. 2007. Biosafety in microbiological and biomedical laboratories, 5th ed. U.S. Government Printing Office, Washington, DC.
- 24.Hogrefe, W. R., R. Moore, M. Lape-Nixon, M. Wagner, and H. E. Prince. 2004. Performance of immunoglobulin G (IgG) and IgM enzyme-linked immunosorbent assays using a West Nile virus recombinant antigen (preM/E) for detection of West Nile virus- and other flavivirus-specific antibodies. J. Clin. Microbiol. 424641-4648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holbrook, M. R., and A. D. Barrett. 2002. Molecular epidemiology of Japanese encephalitis virus. Curr. Top. Microbiol. Immunol. 26775-90. [DOI] [PubMed] [Google Scholar]
- 26.Hombach, J., T. Solomon, I. Kurane, J. Jacobson, and D. Wood. 2005. Report on a WHO consultation on immunological endpoints for evaluation of new Japanese encephalitis vaccines, WHO, Geneva, 2-3 September, 2004. Vaccine 235205-5211. [DOI] [PubMed] [Google Scholar]
- 27.Johnson, A. J., D. A. Martin, N. Karabatsos, and J. T. Roehrig. 2000. Detection of anti-arboviral immunoglobulin G by using a monoclonal antibody-based capture enzyme-linked immunosorbent assay. J. Clin. Microbiol. 381827-1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson, A. J., A. J. Noga, O. Kosoy, R. S. Lanciotti, A. A. Johnson, and B. J. Biggerstaff. 2005. Duplex microsphere-based immunoassay for detection of anti-West Nile virus and anti-St. Louis encephalitis virus immunoglobulin M antibodies. Clin. Diagn. Lab. Immunol. 12566-574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson, B. W., O. Kosoy, D. A. Martin, A. J. Noga, B. J. Russell, A. A. Johnson, and L. R. Petersen. 2005. West Nile virus infection and serologic response among persons previously vaccinated against yellow fever and Japanese encephalitis viruses. Vector Borne Zoonotic Dis. 5137-145. [DOI] [PubMed] [Google Scholar]
- 30.Johnson, B. W., B. J. Russell, and R. S. Lanciotti. 2005. Serotype-specific detection of dengue viruses in a fourplex real-time reverse transcriptase PCR assay. J. Clin. Microbiol. 434977-4983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuno, G., G. J. Chang, K. R. Tsuchiya, N. Karabatsos, and C. B. Cropp. 1998. Phylogeny of the genus Flavivirus. J. Virol. 7273-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lanciotti, R. S., and T. F. Tsai. 2007. Arboviruses, p. 1486-1500. In P. R. Murray, E. J. Baron, J. H. Jorgensen, M. L. Landry, and M. A. Pfaller (ed.), Manual of clinical microbiology, 9th ed., vol. 2. ASM Press, Washington, DC. [Google Scholar]
- 33.Lindsey, H. S., C. H. Calisher, and J. H. Mathews. 1976. Serum dilution neutralization test for California group virus identification and serology. J. Clin. Microbiol. 4503-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu, J. P., H. M. Hsueh, E. Hsieh, and J. J. Chen. 2002. Tests for equivalence or non-inferiority for paired binary data. Stat. Med. 21231-245. [DOI] [PubMed] [Google Scholar]
- 35.Martin, D. A., B. J. Biggerstaff, B. Allen, A. J. Johnson, R. S. Lanciotti, and J. T. Roehrig. 2002. Use of immunoglobulin M cross-reactions in differential diagnosis of human flaviviral encephalitis infections in the United States. Clin. Diagn. Lab. Immunol. 9544-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martin, D. A., D. A. Muth, T. Brown, A. J. Johnson, N. Karabatsos, and J. T. Roehrig. 2000. Standardization of immunoglobulin M capture enzyme-linked immunosorbent assays for routine diagnosis of arboviral infections. J. Clin. Microbiol. 381823-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Monath, T. P. 1994. Dengue: the risk to developed and developing countries. Proc. Natl. Acad. Sci. USA 912395-2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Monath, T. P. 2002. Japanese encephalitis vaccines: current vaccines and future prospects. Curr. Top. Microbiol. Immunol. 267105-138. [DOI] [PubMed] [Google Scholar]
- 39.Monath, T. P., K. McCarthy, P. Bedford, C. T. Johnson, R. Nichols, S. Yoksan, R. Marchesani, M. Knauber, K. H. Wells, J. Arroyo, and F. Guirakhoo. 2002. Clinical proof of principle for ChimeriVax: recombinant live, attenuated vaccines against flavivirus infections. Vaccine 201004-1018. [DOI] [PubMed] [Google Scholar]
- 40.Monath, T. P., K. Soike, I. Levenbook, Z. X. Zhang, J. Arroyo, S. Delagrave, G. Myers, A. D. Barrett, R. E. Shope, M. Ratterree, T. J. Chambers, and F. Guirakhoo. 1999. Recombinant, chimaeric live, attenuated vaccine (ChimeriVax) incorporating the envelope genes of Japanese encephalitis (SA14-14-2) virus and the capsid and nonstructural genes of yellow fever (17D) virus is safe, immunogenic and protective in non-human primates. Vaccine 171869-1882. [DOI] [PubMed] [Google Scholar]
- 41.Nga, P. T., M. del Carmen Parquet, V. D. Cuong, S. P. Ma, F. Hasebe, S. Inoue, Y. Makino, M. Takagi, V. S. Nam, and K. Morita. 2004. Shift in Japanese encephalitis virus (JEV) genotype circulating in northern Vietnam: implications for frequent introductions of JEV from Southeast Asia to East Asia. J. Gen. Virol. 851625-1631. [DOI] [PubMed] [Google Scholar]
- 42.Niedrig, M., K. Sonnenberg, K. Steinhagen, and J. T. Paweska. 2007. Comparison of ELISA and immunoassays for measurement of IgG and IgM antibody to West Nile virus in human sera against virus neutralisation. J. Virol. Methods 139103-105. [DOI] [PubMed] [Google Scholar]
- 43.Porterfield, J. S. 1986. Antibody-dependent enhancement of viral infectivity. Adv. Virus Res. 31335-355. [DOI] [PubMed] [Google Scholar]
- 44.Pugachev, K. V., F. Guirakhoo, F. Mitchell, S. W. Ocran, M. Parsons, B. W. Johnson, O. L. Kosoy, R. S. Lanciotti, J. T. Roehrig, D. W. Trent, and T. P. Monath. 2004. Construction of yellow fever/St. Louis encephalitis chimeric virus and the use of chimeras as a diagnostic tool. Am. J. Trop. Med. Hyg. 71639-645. [PubMed] [Google Scholar]
- 45.Roehrig, J. T. 2003. Antigenic structure of flavivirus proteins. Adv. Virus Res. 59141-175. [DOI] [PubMed] [Google Scholar]
- 46.Roehrig, J. T. 2000. Arboviruses, p. 356-373. In S. Spector, R. Hodinka, and S. Young (ed.), Clinical virology manual, 3rd ed. ASM Press, Washington, DC.
- 47.Roehrig, J. T., J. Hombach, and A. D. Barrett. 2008. Guidelines for plaque-reduction neutralization testing of human antibodies to dengue viruses. Viral Immunol. 21123-132. [DOI] [PubMed] [Google Scholar]
- 48.Russell, P. K., A. Nisalak, P. Sukhavachana, and S. Vivona. 1967. A plaque reduction test for dengue virus neutralizing antibodies. J. Immunol. 99285-290. [PubMed] [Google Scholar]
- 49.Solomon, T. 2006. Control of Japanese encephalitis—within our grasp? N. Engl. J. Med. 355869-871. [DOI] [PubMed] [Google Scholar]
- 50.Solomon, T., N. M. Dung, R. Kneen, M. Gainsborough, D. W. Vaughn, and V. T. Khanh. 2000. Japanese encephalitis. J. Neurol. Neurosurg. Psychiatry 68405-415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Solomon, T., H. Ni, D. W. Beasley, M. Ekkelenkamp, M. J. Cardosa, and A. D. Barrett. 2003. Origin and evolution of Japanese encephalitis virus in southeast Asia. J. Virol. 773091-3098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tsai, T. F., Y. X. Yu, L. L. Jia, R. Putvatana, R. Zhang, S. Wang, and S. B. Halstead. 1998. Immunogenicity of live attenuated SA14-14-2 Japanese encephalitis vaccine—a comparison of 1- and 3-month immunization schedules. J. Infect. Dis. 177221-223. [DOI] [PubMed] [Google Scholar]
- 53.WHO. 2007. Guidelines for plaque reduction neutralizing testing of human antibodies to dengue viruses. WHO, Geneva, Switzerland. [DOI] [PubMed]
- 54.WHO. 2003. WHO-recommended standards for surveillance of selected vaccine-preventable diseases. WHO, Geneva, Switzerland.
- 55.Wong, S. J., R. H. Boyle, V. L. Demarest, A. N. Woodmansee, L. D. Kramer, H. Li, M. Drebot, R. A. Koski, E. Fikrig, D. A. Martin, and P. Y. Shi. 2003. Immunoassay targeting nonstructural protein 5 to differentiate West Nile virus infection from dengue and St. Louis encephalitis virus infections and from flavivirus vaccination. J. Clin. Microbiol. 414217-4223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wong, S. J., V. L. Demarest, R. H. Boyle, T. Wang, M. Ledizet, K. Kar, L. D. Kramer, E. Fikrig, and R. A. Koski. 2004. Detection of human anti-flavivirus antibodies with a West Nile virus recombinant antigen microsphere immunoassay. J. Clin. Microbiol. 4265-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yu, Y.-X., P. F. Wu, J. Ao, L. H. Liu, and H. M. Lim. 1981. Selection of a better immunogenic and highly attenuated live vaccine virus strain of JE. I. Some biological characteristics of SA14-14-2 mutant. Chin. J. Microbiol. Immunol. 177-84. [Google Scholar]