SYNOPSIS
Musculoskeletal, cardiovascular, and mental health are all associated with the physical and psychosocial conditions of work, as well as with individual health behaviors. An integrated approach to workplace health-promotion programs should include attention to the work environment, especially in light of recent findings that work organization influences so-called lifestyle or health behaviors. Macroergonomics provides a framework to improve both physical and organizational features of work and, in the process, to empower individual workers. The Center for the Promotion of Health in the New England Workplace (CPH-NEW) is a research-to-practice effort examining the effectiveness of worksite programs that combine occupational safety and health—especially ergonomics—with health promotion, emphasizing the contribution of work organization to both. Two intervention studies are underway in three different sectors: health care, corrections, and manufacturing. Each study features participatory structures to facilitate employee input into health goal-setting, program design and development, and evaluation, with the goal of enhanced effectiveness and longer-term sustainability.
The National Institute for Occupational Safety and Health (NIOSH) WorkLife Initiative (http://www.cdc.gov/niosh/worklife) seeks to promote a coordinated or integrated approach to the control of occupational health hazards and health-risk reduction that targets individual health behaviors or hazards originating outside the workplace. The Center for the Promotion of Health in the New England Workplace (CPH-NEW) is a Center for Excellence funded in 2006 through the NIOSH WorkLife Initiative. The CPH-NEW research and translational projects share the objective of implementing and comparing several strategies for integrating occupational safety and health (OSH) with workplace health promotion (WHP). The OSH focus is on ergonomics because of the many influences of physical and work organization hazards on musculo-skeletal, cardiovascular, and mental health. These same conditions are also closely related to common health promotion (HP) targets such as smoking, exercise, diet, and obesity. Traditional HP programs often have low compliance from lower socioeconomic groups; participatory rather than top-down programs are favored as a means to ensure that worker priorities are addressed in a context-sensitive manner. In addition, the key factors of decision latitude and social support at work are enhanced more consistently through participatory programs, which have much in common with participatory ergonomics models.
OCCUPATIONAL ERGONOMICS AND HEALTH
Occupational ergonomics attempts to improve the fit between the workforce and the work environment through the optimized design of jobs and work systems. Ergonomics programs most often focus on physical job features, such as tool or workstation dimensions, heavy lifting, awkward postures, and repetitive tasks. The most common goal is avoidance of work-related musculoskeletal disorders (MSDs) such as low back pain and tendonitis, which represent a major cause of morbidity and absenteeism and generate high disability and medical care costs in the U.S. and other developed countries.1,2
Musculoskeletal health represents not only specific disorders, but also the continuum of normal and abnormal age-related physiological changes in muscle, bone, and joint function, as well as fitness-related performance capacity involving strength, mobility, and lean muscle mass. Declining musculoskeletal performance can be reversed into the seventh decade, thus supporting a comprehensive approach to risk identification and intervention.3,4 For example, a benchmark prospective study of 6,500 Finnish municipal employees found that loss of function after 45 years of age was clustered and conditional on physical work-demand profiles.5,6 Active jobs did not enhance musculoskeletal fitness later in life.7 Protective factors included a positive attitude toward aging and fitness, the presence of teamwork and coworker support, reductions in unabated repetitive work, lower management strain and noise at work, better work postures, satisfaction with supervisor's attitude, and leisure exercise.8 Two other cohort studies have similarly highlighted the qualitative difference in effects of occupational and voluntary physical activity on cardiovascular outcomes and all-cause mortality.9,10
Musculoskeletal, mental, and cardiovascular health all share several occupational risk factors, both physical and psychosocial. The proportion of musculoskeletal morbidity attributable to physical work demands is considerable.11–13 Psychosocial stressors, especially low decision latitude, are also linked, but the mechanism(s) may not be fully independent of physical factors.11,12,14–18 In contrast, key psychosocial factors such as quantitative demands (e.g., time pressure), supervisor and coworker support, and intrinsic and extrinsic rewards have well-documented effects for cardiovascular disease (CVD)19–25 and mental health.26–33
Shift work is another widespread organizational stressor with diverse direct and indirect health effects.34–36 Besides sleep disruption, night work is associated with redistributed eating, lower intake of dietary fiber,37 adverse serum lipid and cholesterol profiles,38 oxidative stress,39 and obesity.35,40 Consequent risks include higher incidence of heart disease, particularly from interactions with smoking and obesity.36,41,42 Night work, irregular schedules, and involuntary overtime increase absenteeism43 and work-family conflict with implications for mental health (notably in low-reward jobs45) and for women with primary family responsibilities.46,47
Workplace interventions to reduce MSDs tend to focus primarily on reduction of physical job demands, but sometimes interventions on physical workplace conditions require addressing upstream organizational factors that operate at the group or systems level and are influenced by work technology. This is the macroergonomic approach.48 Work organization represents a set of underlying determinants of both the physical job demands and the psychosocial work environment.49 An effective occupational ergonomics program must address work organization features such as task design, incentive pay, decision latitude, quality of supervision, work scheduling, understaffing, and division of labor among workers and between people and machines.50
When the explicit intervention goal is to improve mental or cardiovascular health through the psychosocial work environment, more complex, large-scale organizational change is usually required.51 A few studies have shown benefits ranging from reduced work-related disability to better work/family balance.52 Multiple health indicators improved following a health-motivated, multifaceted program to promote institutional change.53
HEALTH PROMOTION, SOCIOECONOMIC DISPARITIES IN HEALTH, AND THE WORK ENVIRONMENT
Undesirable physical and psychosocial job features are distributed differentially by gender, socioeconomic status, race/ethnicity, and national origin54–59 in many societies. These factors are thus part of the context of any attempt to improve the health of people in a low socioeconomic position, who are also more likely to experience poor diet, inadequate exercise, tobacco smoke and other environmental hazards, and lack of access to primary care and medical screening.60,61 Additive or even synergistic effects may result from hazardous workplace exposures, whether physical or organizational.
Traditionally, HP practice has focused on individual change in health behaviors such as exercise, diet, tobacco smoking, and stress management and coping skills, with these lifestyle risk factors being well-established contributors to chronic conditions such as obesity, hypertension, CVD, and diabetes. They have also been associated with MSD risk, albeit inconsistently.62–72
However, HP is a broader public health activity than the prevention of specific diseases at the individual level. More recent evolutions have addressed environmental influences on health behaviors in the community73,74 and in the work setting.75 Social HP76 involves activities conducted at the community or societal level, complementing the individual focus. The World Health Organization's Ottawa Charter for Health Promotion highlighted the impact of working and living conditions on socioeconomic health disparities:
Health promotion action aims at reducing differences in current health status and ensuring equal opportunities and resources.. .. People cannot achieve their fullest health potential unless they are able to take control of those things which determine their health.77
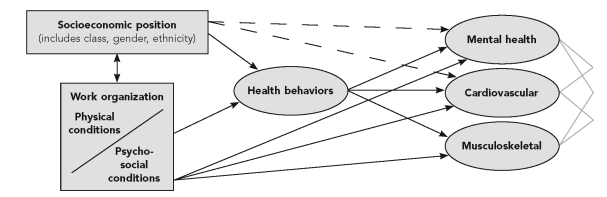
Health behaviors represent decisions based on intrinsic factors (knowledge, beliefs, motivation) and also in relation to factors in the physical and psychosocial environment. An emerging literature indicates the effect of working conditions on individual health behaviors such as smoking, diet, and exercise (Figure). For example, low decision latitude, low rewards relative to effort, and other psychosocial stressors at work have been associated with leisure time inactivity, obesity, and tobacco and alcohol consumption.78–90 In turn, such combinations of risk factors may challenge health even further; examples are the interaction of cigarette smoking with physically heavy jobs on the risk of vertebral pathology,91 and that of body mass index with physical workload on the risk of chronic shoulder disorders.92 Thus, to be effective, WHP programs should address organizational conditions93,94 in addition to individual behaviors. Healthy workplaces should involve employees in decisions about work processes, promote learning, reward appropriately, and attend to interpersonal relationships.
Figure.
Overview of associations among working conditions, socioeconomic position, health behaviors,a and selected health domainsb
aHealth behaviors include tobacco and alcohol consumption, aerobic exercise, nutrition, and sleep.
bNot shown in the diagram: mediators of other links from socioeconomic status to health or the reciprocal effects of health on socioeconomic position, working conditions, or health behaviors.
HEALTH DECISION-MAKING AND PARTICIPATORY PROGRAMS
Traditionally designed WHP programs show overall positive impact, albeit with variable study rigor.95–99 A review of 316 WHP programs reported positive results for weight control; borderline positive results for nutrition, exercise, and cholesterol management; and weak results for health-risk appraisals.98 However, detailed analyses of intervention components suggest equivocal success in changing lifestyle characteristics such as dietary habits or physical activity.96,97,99 These uncertainties are mirrored in workplace preventive lifting programs (as opposed to ergonomic interventions): evident short-term benefits but problematic long-term adherence and benefits.100–103 Program and behavioral sustainability are, therefore, major concerns.104
One potential indicator of durable effectiveness is health self-efficacy (HSE), the belief in one's own capacity to improve and maintain health. HSE, an important component of healthy decision-making, can be viewed as an intermediary variable on the path to good health, being associated with smoking cessation, increased exercise, improved diet,105–110 and reduced disability from musculoskeletal pain.111 HSE can change over time109,110 and is affected positively by successful health mastery experiences and the removal of barriers to healthy behaviors. If the goal is healthy decision-making by individuals, the work environment itself should reinforce employee competence in decision-making.112
Participatory programs that instill a sense of empowerment are likely to bolster program effectiveness,113 as HSE supports a range of healthy behaviors. The very act of participating in a team working toward a common goal can improve psychosocial aspects of the work environment.114,115 Thus, workplace programs empowering participant decision-making at the workplace could also directly reduce psychosocial strain and its negative health consequences.116 Michie et al. summarized the potential health benefits of increased worker participation in decision-making, including better communication, improved support, and feedback.29
Comprehensive employee health programs should identify potential obstacles and facilitators that operate at multiple levels.60,113,117–121 Workers are often best qualified to evaluate programmatic congruence with their own psychosocial and material needs, and can identify incumbent health barriers and opportunities from their experiential knowledge of the workplace culture and environment.118,122
Participatory approaches to organizational flexibility, cited as important ingredients in successful community health interventions,123 can apply in work settings. Semi-autonomous groups, such as workplace health and safety committees and apprenticeship training programs, can be modified as agents for individual health change, provided that parameters of action are predefined and acceptable to the workforce. In our own program experience, smoking cessation in an asbestos-exposed workforce, which had initiated its own health prevention programs, exceeded national norms by a large margin.124
Workplace participatory ergonomics programs can both remediate hazardous working conditions and engage workers in a process that is empowering.125 Worker expertise and confidence in applying knowledge are also critical to maintain improvements and avoid the introduction of new hazards as production technology changes over time. The iterative design approach that is central to participatory ergonomics provides ample opportunities for addressing health concerns during a workplace change process. Successful participatory ergonomics thus represents a form of HP112 and produces a strong sense of commitment to the broader program,126 thereby enhancing program sustainability.
RISK ASSESSMENT, INCENTIVIZATION, AND COST-EFFECTIVENESS
Many of the cost-effectiveness arguments for WHP seem to show a return on investment.127 Chapman reviewed 42 epidemiologic studies with a total of 537,319 employee participants followed for a mean of 3.6 years. In his meta-analysis, employee absenteeism decreased by a mean of 30.0% (range: 22.3–38.4), and health-care costs decreased by 21.8% (range: 12.7–31.0).128 Among the 16 studies with cost-benefit analyses, each dollar spent returned $5.67 to the company (range: $3.40–$7.88). There are, however, difficulties controlling for selection and short-term efficacy; when substantive economic metrics, such as reduced group health costs among participants, are weighed, positive effects may be more modest.129 Indirect benefits of WHP programs for employers have also been reported, such as improved morale, increased productivity, enhanced retention, and reduced health-care costs.113,130–133 These may extend to family members.131
One commonly used assessment instrument in WHP is the health risk appraisal (HRA), a standardized compilation of questionnaire and test results that often serves as a baseline for both risk attribution and incentivization. HRAs rarely assess occupational risk factors that may contribute to long-latency morbidity, either directly or through interaction with personal behaviors. Further, multifactorial health outcomes such as MSDs and CVD are disproportionately likely to be rejected as claims for workers' compensation.134–138 For both of these reasons, work-related components of multicausal morbidity are likely to be undervalued. This speaks to the importance of the combined assessment of workers' compensation and group health data.
One important distinction differentiates individual motivation and group behavior. There are sound reasons to base HP incentives on changes in individual behavior among individuals at highest risk.139,140 In the workplace, there is a potentially corresponding tradition of individual productivity incentives, such as overtime pay and bonuses. However, workplace culture also imposes a collective sensibility regarding group-insured benefits, union dues, seniority, and charitable contributions. For example, there is often unease about altering the benefit structure in ways that transfer risk to the employee. Although the moral hazard argument for transparent health-care costs has support in health policy debate, there is strong employee resistance to the concept that individuals must assume a larger portion of their costs.141
CPH-NEW: AN INTEGRATED APPROACH TO HEALTH PROMOTION AND PROTECTION
Following on these scientific and policy considerations, CPH-NEW promotes a combined approach to addressing risks arising from both personal behaviors and the work environment, with a focus on ergonomic hazards broadly defined.115 Previous studies have suggested that adding OSH interventions to WHP increases their effectiveness compared with traditional WHPs alone;60,113 those OSH programs primarily addressed chemical exposures rather than occupational ergonomics. There does not appear to be any reported evaluation of adding WHP to OSH interventions, compared with OSH alone.
There is a recognized disparity between the willingness of workers to accept health and safety activities directed at workplace hazards and their acceptance of employer-sponsored HP activities.95 Employees who feel that workplace hazards are ignored may be understandably unreceptive to employer advice about their activities during personal time. Conversely, managers have blamed MSDs and CVD on worker obesity, smoking, and other personal risk factors. Combining the two sets of concerns may offer an equitable solution to this impasse by facilitating the sharing of responsibility between workers and employers. Further, integrating ergonomics with HP, in both the needs assessment and program recommendations, is likely to produce more tailored interventions that take into account the full risk profile, rather than compartmentalized approaches. For example, WHP programs often emphasize walking programs for fitness, but these may have little perceived value to people who already spend the entire workday on their feet.
In two separate research projects with complementary study designs, CPH-NEW is comparing the health benefits and cost-effectiveness of an integrated approach vs. an OSH intervention alone, and of an ongoing participatory process vs. more conventional, expert-directed control measures. The economic analyses utilize a comprehensive net-cost approach142,143 to incorporate the costs of investment on equipment and labor (direct costs) plus the avoided costs of lost work time, medical care and turnover (indirect costs), and productivity improvements (spillover effects).
One of these projects evaluates the benefits of an ergonomics intervention in long-term-care centers (nursing homes) with and without wellness programs, followed by a second stage in which participatory health design teams have been initiated in three centers without existing wellness programs. The second project is implementing and comparing traditional best-practices programs with participatory programs in both public sector (department of corrections) and manufacturing environments. There will be multiple measures of effectiveness, evaluating both changes in exposures and in morbidity, with at least two years of follow-up for each project.
Some preliminary findings from the nursing home study illustrate the need for an integrated approach to employee health. Baseline questionnaire surveys were distributed to direct care personnel (primarily nurses and aides) in 12 centers in Maryland and Maine owned by a single company. A total of 920 surveys were returned (mean response was 70% of all eligible employees). Respondents were mostly female (92%), 47% were African American or African, and the mean age was 42 (±13) years.
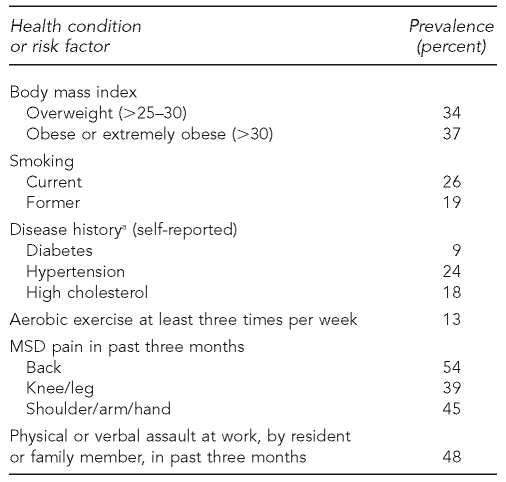
The study population was notable for a high prevalence of chronic health conditions and risk factors (Table 1). One-third (35%) reported diagnosis or treatment of a chronic health condition (diabetes, high blood pressure, high cholesterol, or low back disease), of which hypertension was the most common. More than 70% of respondents reported musculoskeletal symptoms during the previous three months, and 21% said that their pain interfered at least moderately with paid work or housework.
Table 1.
Baseline health characteristics of 920 clinical staff in 12 nursing homes, surveyed by self-administered questionnaire, 2006–2007
aMedical diagnosis and/or treatment
MSD = musculoskeletal disorder
Fewer than half of the respondents reported frequent exercising to work up a sweat. Six of 10 non-exercisers planned to begin exercising more, but only 39% were confident that they could do so for six months. In contrast, despite the high prevalence of overweight, only 30% reported that they planned to lose weight. Six respondents who indicated smoking “often” planned to quit within the next six months.
Preliminary analyses demonstrated several associations between features of the work environment and individual health behaviors. For example, current smokers were more likely than nonsmokers to be in jobs with psychosocial strain (high demands relative to decision latitude) and to have had at least one recent physical assault at work. Those who exercised at least three times per week experienced about a 10% higher degree of control over their work schedules than those who exercised less than once per week. Higher self-rated health (SF-12)144 was associated with lower job strain, better supervisor support and work-family balance, and no recent physical assault. Confidence in one's ability to get a full night's sleep was lowest among night (third-shift) workers and also slightly lower among those who had experienced three assaults at work in the past three months. Mental health (SF-12 Mental Components Summary)144 was lower with increasing age and body mass index, physically awkward work, and work interference with home life, while weekly aerobic exercise and coworker support had protective influences (model R2 = 0.152).
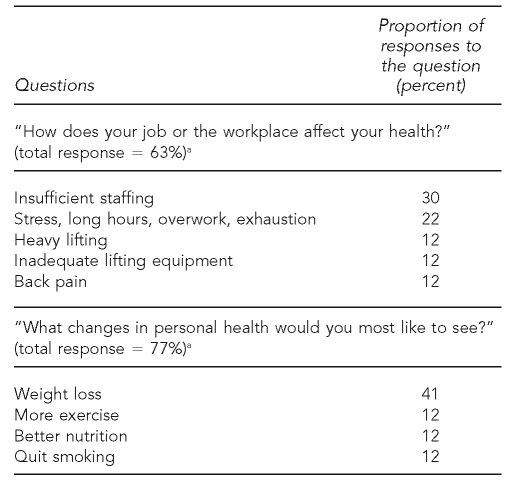
Concurrent with these findings were the replies to open-ended questions at the end of the survey, to which a large proportion of the participants provided responses (Table 2). Staffing, work hours, and general overload clearly represented a major challenge to the health of these employees, while resident handling and associated back pain was a secondary although important concern. Simultaneously, a large number also wanted to lose weight, improve their diets, and exercise more regularly.
Table 2.
Categorized responses to open-ended questions on self-administered survey of 658 nursing home employees, Maryland, 2006
aProportion of all participants who answered this question; answers were not mutually exclusive
The current intervention program in this sector involved employee-centered design teams145 in three centers; another three centers served as the control group. Initial focus groups of nursing aides in the intervention centers highlighted an overlapping set of health concerns with those noted in the survey responses. Stress at work was linked to staffing levels (e.g., effects of absenteeism on coworkers); quality of communication with and support from supervisors; having to handle combative residents; and general sensory overload at work.
These survey and focus group findings not only provided empirical support for the feasibility of the overall approach, but the availability of these findings was critical to launching the first phase of the participatory intervention. Regarding feasibility, the results indicated that these employees were able to articulate and prioritize their HP concerns, and they also reflected a general desire to improve their health. The interdependent nature of the identified concerns confirmed that an integrated OSH and WHP program employing macroergonomics would be necessary to fully address them. Availability and consistency in the findings was essential to successfully launching the activities of the participatory health design teams. The findings allowed team members to immediately begin focusing on the set of HP topics that mattered most to a large number of employees; in general, this also helped validate the approach to the organization.
For example, the design teams at all three centers prioritized activities to improve access to healthy food and to facilitate aerobic exercise during active rest breaks (also for stress reduction) during the workday, while issues of teamwork, communication, and supervision were identified for longer-term action. There has also been discussion of reducing back injury risk through stretching and strengthening exercises, as well as enhancing the effectiveness of the corporate program on safe resident handling (lifting reduction) already in place.
CONCLUSION
WHP programs can approach the workplace as more than a venue for delivering services, by addressing environmental obstacles to HP in the workplace and by accounting for the effects of working conditions, including whether employees are empowered as decision makers. Workers are more apt to accept HP programs if they are accompanied by workplace changes as well. Occupational ergonomics in its broadest sense provides a framework to address workplace preconditions for musculoskeletal, cardiovascular, and mental health. The principle of combining OSH and HP could readily be extended to other domains, such as respiratory health (with interventions on indoor air quality, smoking, and other asthma-control measures) and reproductive health (workplace chemical exposures and maternal nutrition). With employee input into program priorities and activities, improved HSE may help sustain behavioral change. Thus, there is a strong scientific justification for integrating WHP and ergonomics programs, although only modest empirical evidence is available to date on potential health effects. CPH-NEW is addressing these questions in two workplace intervention studies that emphasize macroergonomic issues (i.e., work organization and participatory programs) to the extent possible.
Acknowledgments
The authors thank Kimberly Rauscher and Helena Miranda, who assisted with literature searches; and Rebecca Gore, Helena Miranda, Suzanne Nobrega, Ameia Yen-Patton, David Reeves, II, and Michael Tuller, who assisted with data analyses.
Footnotes
This work was supported by grant #1U19-OH008857 from the National Institute for Occupational Safety and Health (NIOSH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH.
An earlier literature review on some of these topics is found in Conceptual Issues in Worksite Health Promotion, by Eberhard Wenzel, available from: URL: http://www.ldb.org/whpr.htm.
REFERENCES
- 1.Badley EM, Rasooly I, Webster GK. Relative importance of musculoskeletal disorders as a cause of chronic health problems, disability, and health care utilization: findings from the 1990 Ontario Health Survey. J Rheumatol. 1994;21:505–14. [PubMed] [Google Scholar]
- 2.Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–99. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 3.Fiatarone MA, O'Neill EF, Ryan ND, Clements KM, Solares GR, Nelson ME, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. 1994;330:1769–75. doi: 10.1056/NEJM199406233302501. [DOI] [PubMed] [Google Scholar]
- 4.Makrides L, Heigenhauser GJ, Jones NL. High-intensity endurance training in 20- to 30- and 60- to 70-yr-old healthy men. J Appl Physiol. 1990;69:1792–8. doi: 10.1152/jappl.1990.69.5.1792. [DOI] [PubMed] [Google Scholar]
- 5.Ilmarinen J, Tuomi K, Eskelinen L, Nygard CH, Huuhtanen P, Klockars M. Summary and recommendations of a project involving cross-sectional and follow-up studies on the aging worker in Finnish municipal occupations (1981–1985) Scand J Work Environ Health. 1991;17(Suppl 1):135–41. [PubMed] [Google Scholar]
- 6.Nygard CH, Pohjonen T, Ilmarinen J. FinnAge—respect for the ageing. Helsinki: Finnish Institute of Occupational Health; 1999. Muscular strength of ageing employees over an 11-year period. In: Ilmarinen J, Louhevaara V, editors; pp. p. 240–9. [Google Scholar]
- 7.Savinainen M, Nygard CH, Ilmarinen J. A 16-year follow-up study of physical capacity in relation to perceived workload among ageing employees. Ergonomics. 2004;47:1087–102. doi: 10.1080/00140130410001686357. [DOI] [PubMed] [Google Scholar]
- 8.Savinainen M, Nygard CH, Korhonen O, Ilmarinen J. Changes in physical capacity among middle-aged municipal employees over 16 years. Exp Aging Res. 2004;30:1–22. doi: 10.1080/0361073049025746. [DOI] [PubMed] [Google Scholar]
- 9.Kristal-Boneh E, Harari G, Melamed S, Froom P. Association of physical activity at work with mortality in Israeli industrial employees: the CORDIS study. J Occup Environ Med. 2000;42:127–35. doi: 10.1097/00043764-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Krause N, Brand RJ, Kaplan GA, Kauhanen J, Malla S, Tuomainen TP, et al. Occupational physical activity, energy expenditure and 11-year progression of carotid atherosclerosis. Scand J Work Environ Health. 2007;33:405–24. doi: 10.5271/sjweh.1171. [DOI] [PubMed] [Google Scholar]
- 11.National Research Council; Institute of Medicine. Musculoskeletal disorders and the workplace: low back and upper extremities. Washington: National Academy Press; 2001. [PubMed] [Google Scholar]
- 12.Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol. 2004;14:13–23. doi: 10.1016/j.jelekin.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Punnett L, Prüss-Ütün A, Nelson DI, Fingerhut MA, Leigh J, Tak S, et al. Estimating the global burden of low back pain attributable to combined occupational exposures. Am J Ind Med. 2005;48:459–69. doi: 10.1002/ajim.20232. [DOI] [PubMed] [Google Scholar]
- 14.Bongers PM, de Winter CR, Kompier MAJ, Hildebrandt VH. Psychosocial factors at work and musculoskeletal disease. Scand J Work Environ Health. 1993;19:297–312. doi: 10.5271/sjweh.1470. [DOI] [PubMed] [Google Scholar]
- 15.Bongers PM, Kremer AM, ter Laak J. Are psychosocial factors, risk factors for symptoms and signs of the shoulder, elbow, or hand/wrist?: a review of the epidemiological literature. Am J Ind Med. 2002;41:315–42. doi: 10.1002/ajim.10050. [DOI] [PubMed] [Google Scholar]
- 16.Hartvigsen J, Lings S, Leboeuf-Yde C, Bakketeig L. Psychosocial factors at work in relation to low back pain and consequences of low back pain; a systematic, critical review of prospective cohort studies. Occup Environ Med. 2004;61:e2. [PMC free article] [PubMed] [Google Scholar]
- 17.Hoogendoorn WE, Bongers PM, de Vet HC, Ariens GA, van Mechelen W, Bouter LM. High physical work load and low job satisfaction increase the risk of sickness absence due to low back pain: results of a prospective cohort study. Occup Environ Med. 2002;59:323–8. doi: 10.1136/oem.59.5.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warren N. Work stress and musculoskeletal disorder etiology: the relative roles of psychosocial and physical risk factors. Work. 2001;17:221–34. [PubMed] [Google Scholar]
- 19.Belkic KL, Landsbergis PA, Schnall PL, Baker D. Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health. 2004;30:85–128. doi: 10.5271/sjweh.769. [DOI] [PubMed] [Google Scholar]
- 20.Guimont C, Brisson C, Dagenais GR, Milot A, Vezina M, Masse B, et al. Effects of job strain on blood pressure: a prospective study of male and female white-collar workers. Am J Public Health. 2006;96:1436–43. doi: 10.2105/AJPH.2004.057679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–55. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 22.Kivimaki M, Virtanen M, Elovainio M, Kouvonen A, Vaananen A, Vahtera J. Work stress in the etiology of coronary heart disease—a meta-analysis. Scand J Work Environ Health. 2006;32:431–42. doi: 10.5271/sjweh.1049. [DOI] [PubMed] [Google Scholar]
- 23.Kristensen TS. Job stress and cardiovascular disease: a theoretical critical review. J Occup Health Psychol. 1996;1:246–60. doi: 10.1037//1076-8998.1.3.246. [DOI] [PubMed] [Google Scholar]
- 24.Schnall P, Belkic K, Landsbergis P, Baker D, editors The workplace and cardiovascular disease. Occup Med State Art Rev. 2000;15:1–68. [PubMed] [Google Scholar]
- 25.Theorell T, Karasek RA. Current issues relating to psychosocial job strain and cardiovascular disease research. J Occup Health Psychol. 1996;1:9–26. doi: 10.1037//1076-8998.1.1.9. [DOI] [PubMed] [Google Scholar]
- 26.Bildt C, Michelsen H. Gender differences in the effects from working conditions on mental health: a 4-year follow-up. Int Arch Occup Environ Health. 2002;75:252–8. doi: 10.1007/s00420-001-0299-8. [DOI] [PubMed] [Google Scholar]
- 27.Griffin JM, Greiner BA, Stansfeld SA, Marmot M. The effect of self-reported and observed job conditions on depression and anxiety symptoms: a comparison of theoretical models. J Occup Health Psychol. 2007;12:334–49. doi: 10.1037/1076-8998.12.4.334. [DOI] [PubMed] [Google Scholar]
- 28.Mausner-Dorsch H, Eaton WW. Psychosocial work environment and depression: epidemiologic assessment of the demand-control model. Am J Public Health. 2000;90:1765–70. doi: 10.2105/ajph.90.11.1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Michie S, Williams S. Reducing work-related psychological ill health and sickness absence: a systematic literature review. Occup Environ Med. 2003;60:3–9. doi: 10.1136/oem.60.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pikhart H, Bobak M, Pajak A, Malyutina S, Kubinova R, Topo R, et al. Psychosocial factors at work and depression in three countries of Central and Eastern Europe. Soc Sci Med. 2004;58:1475–82. doi: 10.1016/S0277-9536(03)00350-2. [DOI] [PubMed] [Google Scholar]
- 31.Rugulies R, Bultmann U, Aust B, Burr H. Psychosocial work environment and incidence of severe depressive symptoms: prospective findings from a 5-year follow-up of the Danish work environment cohort study. Am J Epidemiol. 2006;163:877–87. doi: 10.1093/aje/kwj119. [DOI] [PubMed] [Google Scholar]
- 32.Stanfeld SA, Head J, Fuhrer R, Wardle J, Cattel V. Social inequalities in depressive symptoms and physical functioning in the Whitehall II study: exploring a common cause explanation. J Epidemiol Community Health. 2003;57:361–7. doi: 10.1136/jech.57.5.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang JL, Patten SB. Perceived work stress and major depression in the Canadian employed population, 20–49 years old. J Occup Health Psychol. 2001;6:283–9. doi: 10.1037//1076-8998.6.4.283. [DOI] [PubMed] [Google Scholar]
- 34.Lipscomb JA, Trinkoff AM, Geiger-Brown J, Brady B. Work-schedule characteristics and reported musculoskeletal disorders of registered nurses. Scand J Work Environ Health. 2002;28:394–401. doi: 10.5271/sjweh.691. [DOI] [PubMed] [Google Scholar]
- 35.Niedhammer I, Lert F, Marne MJ. Prevalence of overweight and weight gain in relation to night work in a nurses' cohort. Int J Obes Relat Metab Disord. 1996;20:625–33. [PubMed] [Google Scholar]
- 36.Steenland K. Shift work, long hours, and cardiovascular disease: a review. Occup Med State Art Rev. 2000;15:7–17. [Google Scholar]
- 37.Knutsson A. Shift work and coronary heart disease. Scand J Soc Med. 1989;44(Suppl):1–36. [PubMed] [Google Scholar]
- 38.Lennernas M, Akerstedt T, Hambraeus L. Nocturnal eating and serum cholesterol of three shift workers. Scand J Work Environ Health. 1994;20:401–6. doi: 10.5271/sjweh.1381. [DOI] [PubMed] [Google Scholar]
- 39.Sharifian A, Farahani S, Pasalar P, Gharavi M, Aminian O. Shift work as an oxidative stressor. J Circadian Rhythms. 2005;3:15. doi: 10.1186/1740-3391-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parkes KR. Shift work and age as interactive predictors of body mass index among offshore workers. Scand J Work Environ Health. 2002;28:64–71. doi: 10.5271/sjweh.648. [DOI] [PubMed] [Google Scholar]
- 41.Kivimaki M, Kuisma P, Virtanen M, Elovainio M. Does shift work lead to poorer health habits? A comparison between women who had always done shift work with those who had never done shift work. Work – Stress. 2001;15:3–13. [Google Scholar]
- 42.Tenkanen L, Sjöblom T, Härmä M. Joint effect of shift work and adverse life-style factors on the risk of coronary heart disease. Scand J Work Environ Health. 1998;24:351–7. doi: 10.5271/sjweh.355. [DOI] [PubMed] [Google Scholar]
- 43.Ala-Mursula L, Vahtera J, Kouvonen A, Vaananen A, Linna A, Pentti J, et al. Long hours in paid and domestic work and subsequent sickness absence: does control over daily working hours matter? Occup Environ Med. 2006;63:608–16. doi: 10.1136/oem.2005.023937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Davis KD, Goodman WB, Pirretti AE, Almeida DM. Nonstandard work schedules, perceived family well-being, and daily stressors. J Marriage Fam. 2008;70:991–1003. doi: 10.1111/j.1741-3737.2008.00541.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van der Hulst M, Geurts S. Associations between overtime and psychological health in high and low reward jobs. Work – Stress. 2001;15:227–40. [Google Scholar]
- 46.Estryn-Behar M, Kaminski M, Peigne E, Bonnet N, Vaichere E, Gozlan C, et al. Stress at work and mental health status among female hospital workers. Br J Ind Med. 1990;47:20–8. doi: 10.1136/oem.47.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Büssing A. Social tolerance of working time scheduling in nursing. Work – Stress. 1996;10:238–50. [Google Scholar]
- 48.Hendrick HW, Kleiner BM. Macroergonomics: theory, methods, and applications. Mahwah (NJ): Lawrence Erlbaum Associates; 2002. [Google Scholar]
- 49.Macdonald LA, Harenstam A, Warren ND, Punnett L. Incorporating work organisation into occupational health research: an invitation for dialogue. Occup Environ Med. 2008;65:1–3. doi: 10.1136/oem.2007.033860. [DOI] [PubMed] [Google Scholar]
- 50.Sauter SL, Brightwell WS, Colligan MJ, Hurrell JJ, Jr, Katz TM, LeGrande DE, et al. The changing organization of work and the safety and health of working people: knowledge gaps and research directions. Cincinnati: National Institute for Occupational Safety and Health (US); 2002. [Google Scholar]
- 51.Lamontagne AD, Keegel T, Louie AM, Ostry A, Landsbergis PA. A systematic review of the job-stress intervention evaluation literature, 1990–2005. Int J Occup Environ Health. 2007;13:268–80. doi: 10.1179/oeh.2007.13.3.268. [DOI] [PubMed] [Google Scholar]
- 52.Amick BC, III, Habeck RV, Hunt A, Fossel AH, Chapin A, Keller RB, et al. Measuring the impact of organizational behaviors on work disability prevention and management. J Occup Rehab. 2000;10:21–38. [Google Scholar]
- 53.Anderzen I, Arnetz BB. The impact of a prospective survey-based workplace intervention program on employee health, biologic stress markers, and organizational productivity. J Occup Environ Med. 2005;47:671–82. doi: 10.1097/01.jom.0000167259.03247.1e. [DOI] [PubMed] [Google Scholar]
- 54.Blau FD, Ferber MA, Winkler AE. The economics of women, men, and work. 4th ed. Upper Saddle River (NJ): Prentice Hall; 2002. [Google Scholar]
- 55.Bond MA, Kajala A, Markkanen P, Cazeca D, Daniel S, Tsurikova L, et al. Cincinnati: National Institute for Occupational Safety and Health (US); 2007. Expanding our understanding of the psychosocial work environment: a compendium of measures of discrimination, harassment and work-family issues. DHHS/NIOSH Publication No. 2008-104. [Google Scholar]
- 56.d'Errico A, Punnett L, Cifuentes M, Boyer J, Tessler J, Gore R, et al. Hospital injury rates in relation to socioeconomic status and working conditions. Occup Environ Med. 2007;64:325–33. doi: 10.1136/oem.2006.027839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de Castro AB, Fujishiro K, Sweitzer E, Oliva J. How immigrant workers experience workplace problems: a qualitative study. Arch Environ Occup Health. 2006;61:249–58. doi: 10.3200/AEOH.61.6.249-258. [DOI] [PubMed] [Google Scholar]
- 58.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–30. [PubMed] [Google Scholar]
- 59.Wadsworth E, Dhillon K, Shaw C, Bhui K, Stansfeld S, Smith A. Racial discrimination, ethnicity and work stress. Occup Med (Lond) 2007;57:18–24. doi: 10.1093/occmed/kql088. [DOI] [PubMed] [Google Scholar]
- 60.Sorensen G, Barbeau E. Steps to a healthier US workforce. Integrating occupational health and safety and worksite health promotion: state of the science. Paper presented at the Steps to a Healthier US Workforce Symposium; 2004 Oct 26–28; Washington. [Google Scholar]
- 61.Deitz D, Cook R, Hersch R. Workplace health promotion and utilization of health services: follow-up data findings. J Behav Health Serv Res. 2005;32:306–19. doi: 10.1007/BF02291830. [DOI] [PubMed] [Google Scholar]
- 62.Hildebrandt VH, Bongers PM, Dul J, van Dijk FJ, Kemper HC. The relationship between leisure time, physical activities and musculoskeletal symptoms and disability in worker populations. Int Arch Occup Environ Health. 2000;73:507–18. doi: 10.1007/s004200000167. [DOI] [PubMed] [Google Scholar]
- 63.Goldberg MS, Scott SC, Mayo NE. A review of the association between cigarette smoking and the development of nonspecific back pain and related outcomes. Spine. 2000;25:995–1014. doi: 10.1097/00007632-200004150-00016. [DOI] [PubMed] [Google Scholar]
- 64.John U, Hanke M, Meyer C, Volzke H, Baumeister SE, Alte D. Tobacco smoking in relation to pain in a national general population survey. Prev Med. 2006;43:477–81. doi: 10.1016/j.ypmed.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 65.Leino-Arjas P. Smoking and musculoskeletal disorders in the metal industry: a prospective study. Occup Environ Med. 1998;55:828–33. doi: 10.1136/oem.55.12.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Leboeuf-Yde C, Kyvik KO, Bruun NH. Low back pain and lifestyle. Part I: smoking. Information from a population-based sample of 29,424 twins. Spine. 1998;23:2207–13. doi: 10.1097/00007632-199810150-00012. discussion 14. [DOI] [PubMed] [Google Scholar]
- 67.Leboeuf-Yde C, Kyvik KO, Bruun NH. Low back pain and lifestyle. Part II—obesity. Information from a population-based sample of 29,424 twin subjects. Spine. 1999;24:779–83. doi: 10.1097/00007632-199904150-00009. discussion 83-4. [DOI] [PubMed] [Google Scholar]
- 68.Leboeuf-Yde C. Smoking and low back pain. A systematic literature review of 41 journal articles reporting 47 epidemiologic studies. Spine. 1999;24:1463–70. doi: 10.1097/00007632-199907150-00012. [DOI] [PubMed] [Google Scholar]
- 69.Leboeuf-Yde C. Alcohol and low-back pain: a systematic literature review. J Manipulative Physiol Ther. 2000;23:343–6. doi: 10.1067/mmt.2000.106866. [DOI] [PubMed] [Google Scholar]
- 70.Leboeuf-Yde C. Body weight and low back pain. A systematic literature review of 56 journal articles reporting on 65 epidemiologic studies. Spine. 2000;25:226–37. doi: 10.1097/00007632-200001150-00015. [DOI] [PubMed] [Google Scholar]
- 71.Leino-Arjas P, Kaila-Kangas L, Solovieva S, Riihimaki H, Kirjonen J, Reunanen A. Serum lipids and low back pain: an association? A follow-up study of a working population sample. Spine. 2006;31:1032–7. doi: 10.1097/01.brs.0000214889.31505.08. [DOI] [PubMed] [Google Scholar]
- 72.Leino-Arjas P, Solovieva S, Kirjonen J, Reunanen A, Riihimaki H. Cardiovascular risk factors and low-back pain in a long-term follow-up of industrial employees. Scand J Work Environ Health. 2006;32:12–9. doi: 10.5271/sjweh.971. [DOI] [PubMed] [Google Scholar]
- 73.Ball K, Timperio AF, Crawford DA. Understanding environmental influences on nutrition and physical activity behaviors: where should we look and what should we count? Int J Behav Nutr Phys Act. 2006;3:33. doi: 10.1186/1479-5868-3-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Duncan MJ, Spence JC, Mummery WK. Perceived environment and physical activity: a meta-analysis of selected environmental characteristics. Int J Behav Nutr Phys Act. 2005;2:11. doi: 10.1186/1479-5868-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Koelen MA, Lindstrom B. Making healthy choices easy choices: the role of empowerment. Eur J Clin Nutr. 2005;59(Suppl 1):S10–5. doi: 10.1038/sj.ejcn.1602168. discussion S6, S23. [DOI] [PubMed] [Google Scholar]
- 76.Seedhouse D. Health promotion: philosophy, prejudice and practice. New York: John Wiley & Sons; 1997. [Google Scholar]
- 77.World Health Organization. Ottawa charter for health promotion; First International Conference on Health Promotion; 1986 Nov 21; Ottawa. [Google Scholar]
- 78.Albertsen K, Hannerz H, Borg V, Burr H. Work environment and smoking cessation over a five-year period. Scand J Public Health. 2004;32:164–71. doi: 10.1080/14034940310017779. [DOI] [PubMed] [Google Scholar]
- 79.Albertsen K, Borg V, Oldenburg B. A systematic review of the impact of work environment on smoking cessation, relapse and amount smoked. Prev Med. 2006;43:291–305. doi: 10.1016/j.ypmed.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 80.Brisson C, Larocque B, Moisan J, Vezina M, Dagenais GR. Psychosocial factors at work, smoking, sedentary behavior, and body mass index: a prevalence study among 6,995 white collar workers. J Occup Environ Med. 2000;42:40–6. doi: 10.1097/00043764-200001000-00011. [DOI] [PubMed] [Google Scholar]
- 81.Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II Study. Am J Epidemiol. 2007;165:828–37. doi: 10.1093/aje/kwk058. [DOI] [PubMed] [Google Scholar]
- 82.Chandola T, Brunner E, Marmot M. Chronic stress at work and the metabolic syndrome: prospective study. BMJ. 2006;332:521–5. doi: 10.1136/bmj.38693.435301.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Head J, Stansfeld SA, Siegrist J. The psychosocial work environment and alcohol dependence: a prospective study. Occup Environ Med. 2004;61:219–24. doi: 10.1136/oem.2002.005256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.John U, Riedel J, Rumpf HJ, Hapke U, Meyer C. Associations of perceived work strain with nicotine dependence in a community sample. Occup Environ Med. 2006;63:207–11. doi: 10.1136/oem.2005.020966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kivimaki M, Head J, Ferrie JE, Shipley MJ, Brunner E, Vahtera J, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II Study. Int J Obes (Lond) 2006;30:982–7. doi: 10.1038/sj.ijo.0803229. [DOI] [PubMed] [Google Scholar]
- 86.Kouvonen A, Kivimaki M, Virtanen M, Heponiemi T, Elovainio M, Pentti J, et al. Effort-reward imbalance at work and the co-occurrence of lifestyle risk factors: cross-sectional survey in a sample of 36,127 public sector employees. BMC Public Health. 2006;6:24. doi: 10.1186/1471-2458-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ostry AS, Radi S, Louie AM, LaMontagne AD. Psychosocial and other working conditions in relation to body mass index in a representative sample of Australian workers. BMC Public Health. 2006;6:53. doi: 10.1186/1471-2458-6-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Radi S, Ostry A, LaMontagne AD. Job stress and other working conditions: relationships with smoking behaviors in a representative sample of working Australians. Am J Ind Med. 2007;50:584–96. doi: 10.1002/ajim.20492. [DOI] [PubMed] [Google Scholar]
- 89.Ragland DR, Greiner BA, Yen IH, Fisher JM. Occupational stress factors and alcohol-related behavior in urban transit operators. Alcohol Clin Exp Res. 2000;24:1011–9. [PubMed] [Google Scholar]
- 90.Schulte PA, Wagner GR, Ostry A, Blanciforti LA, Cutlip RG, Krajnak KM, et al. Work, obesity, and occupational safety and health. Am J Public Health. 2007;97:428–36. doi: 10.2105/AJPH.2006.086900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Leboeuf-Yde C, Kjaer P, Bendix T, Manniche C. Self-reported hard physical work combined with heavy smoking or overweight may result in so-called Modic changes. BMC Musculoskelet Disord. 2008;9:5. doi: 10.1186/1471-2474-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Miranda H, Punnett L, Viikari-Juntura E, Heliovaara M, Knekt P. Physical work and chronic shoulder disorder. Results of a prospective population-based study. Ann Rheum Dis. 2008;67:218–23. doi: 10.1136/ard.2007.069419. [DOI] [PubMed] [Google Scholar]
- 93.Golaszewski T, Barr D, Pronk N. Development of assessment tools to measure organizational support for employee health. Am J Health Behav. 2003;27:43–54. doi: 10.5993/ajhb.27.1.5. [DOI] [PubMed] [Google Scholar]
- 94.Whysall ZJ, Haslam C, Haslam R. Developing the stage of change approach for the reduction of work-related musculoskeletal disorders. J Health Psychol. 2007;12:184–97. doi: 10.1177/1359105307071753. [DOI] [PubMed] [Google Scholar]
- 95.Aldana SG, Pronk NP. Health promotion programs, modifiable health risks, and employee absenteeism. J Occup Environ Med. 2001;43:36–46. doi: 10.1097/00043764-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 96.Dishman RK, Oldenburg B, O'Neal H, Shephard RJ. Worksite physical activity interventions: toward a social ecology of health promotion. Am J Prev Med. 1998;15:344–61. doi: 10.1016/s0749-3797(98)00077-4. [DOI] [PubMed] [Google Scholar]
- 97.Glanz K, Seewald-Klein T. Nutrition at the worksite: an overview. J Nutr Educ. 1986;15:395–415. [Google Scholar]
- 98.Glasgow RE, McCaul KD, Fisher KJ. Participation in worksite health promotion: a critique of the literature and recommendations for future practice. Health Educ Q. 1993;20:391–408. doi: 10.1177/109019819302000309. [DOI] [PubMed] [Google Scholar]
- 99.Heaney CA, Goetzel RZ. A review of health-related outcomes of multi-component worksite health promotion programs. Am J Health Promot. 1997;11:290–307. doi: 10.4278/0890-1171-11.4.290. [DOI] [PubMed] [Google Scholar]
- 100.Karjalainen KA, Malmivaara A, van Tulder MW, Roine R, Jauhiainen M, Hurri H, et al. Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults. Cochrane Database Syst Rev. 2003;2:CD002194. doi: 10.1002/14651858.CD002194. [DOI] [PubMed] [Google Scholar]
- 101.Koopman FS, Edelaar M, Slikker R, Reynders K, van der Woude LH, Hoozemans MJ. Effectiveness of a multidisciplinary occupational training program for chronic low back pain: a prospective cohort study. Am J Phys Med Rehabil. 2004;83:94–103. doi: 10.1097/01.PHM.0000107482.35803.11. [DOI] [PubMed] [Google Scholar]
- 102.Maher CG. A systematic review of workplace interventions to prevent low back pain. Aust J Physiother. 2000;46:259–69. doi: 10.1016/s0004-9514(14)60287-7. [DOI] [PubMed] [Google Scholar]
- 103.Silverstein B, Clark R. Interventions to reduce work-related musculoskeletal disorders. J Electromyogr Kinesiol. 2004;14:135–52. doi: 10.1016/j.jelekin.2003.09.023. [DOI] [PubMed] [Google Scholar]
- 104.Booth SL, Sallis JF, Ritenbaugh C, Hill JO, Birch LL, Frank LD, et al. Environmental and societal factors affect food choice and physical activity: rationale, influences, and leverage points. Nutr Rev. 2001;59(3 Pt 2):S21–39. doi: 10.1111/j.1753-4887.2001.tb06983.x. discussion S57-65. [DOI] [PubMed] [Google Scholar]
- 105.Clark DO, Nothwehr F. Exercise self-efficacy and its correlates among socioeconomically disadvantaged older adults. Health Educ Behav. 1999;26:535–46. doi: 10.1177/109019819902600410. [DOI] [PubMed] [Google Scholar]
- 106.De Vries H, Backbier E, Kok G, Dijkstra M. The impact of social influence in the context of attitude, self-efficacy, intention, and previous behavior as predictors of smoking onset. J Appl Soc Psychol. 1995;25:237–57. [Google Scholar]
- 107.Hausenblas HA, Carron AV, Mack DE. Application of the theories of reasoned action and planned behavior to exercise behavior: a meta-analysis. J Sport Exercise Psychol 1998; 1936. 51 pp. [Google Scholar]
- 108.Oei TPS, Fergusson S, Lee NK. The differential role of alcohol expectancies and drinking refusal self-efficacy in problem and nonproblem drinkers. J Stud Alcohol. 1998;59:704–11. doi: 10.15288/jsa.1998.59.704. [DOI] [PubMed] [Google Scholar]
- 109.Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–7. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 110.Powell KE, Blair SN. The public health burdens of sedentary living habits: theoretical but realistic estimates. Med Sci Sports Exerc. 1994;26:851–6. [PubMed] [Google Scholar]
- 111.Denison E, Asenlof P, Lindberg P. Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain. 2004;111:245–52. doi: 10.1016/j.pain.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 112.Gunnarsdottir S, Bjornsdottir K. Health promotion in the workplace: the perspective of unskilled workers in a hospital setting. Scand J Caring Sci. 2003;17:66–73. doi: 10.1046/j.1471-6712.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- 113.Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working-class, multiethnic workers: results of the healthy directions—small business study. Am J Public Health. 2005;95:1389–95. doi: 10.2105/AJPH.2004.038745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Park KO, Schaffer BS, Griffin-Blake CS, Dejoy DM, Wilson MG, Vandenberg RJ. Effectiveness of a healthy work organization intervention: ethnic group differences. J Occup Environ Med. 2004;46:623–34. doi: 10.1097/01.jom.0000131793.44014.91. [DOI] [PubMed] [Google Scholar]
- 115.Watts GF, Donahue RE, Eddy JM, Wallace EV. Use of an ecological approach to worksite health promotion. Am J Health Studies. 2001;17:144–7. [Google Scholar]
- 116.Vezina M, Bourbonnais R, Brisson C, Trudel L. Workplace prevention and promotion strategies. Healthc Pap. 2004;5:32–44. doi: 10.12927/hcpap..16822. [DOI] [PubMed] [Google Scholar]
- 117.Cole DC, Wells RP, Frazer MB, Kerr MS, Neumann WP, Laing AC. Methodological issues in evaluating workplace interventions to reduce work-related musculoskeletal disorders through mechanical exposure reduction. Scand J Work Environ Health. 2003;29:396–405. doi: 10.5271/sjweh.746. [DOI] [PubMed] [Google Scholar]
- 118.Eakin JM, Cava M, Smith TF. From theory to practice: a determinants approach to workplace health promotion in small businesses. Health Promot Pract. 2001;2:172–81. [Google Scholar]
- 119.Grzywacz JG, Fuqua J. The social ecology of health: leverage points and linkages. Behav Med. 2000;26:101–15. doi: 10.1080/08964280009595758. [DOI] [PubMed] [Google Scholar]
- 120.Israel BA, Baker EA, Goldenhar LM, Heaney CA, Schurman SJ. Occupational stress, safety, and health: conceptual framework and principles for effective prevention interventions. J Occup Health Psychol. 1996;1:261–86. doi: 10.1037//1076-8998.1.3.261. [DOI] [PubMed] [Google Scholar]
- 121.Lotters F, Burdof A. Are changes in mechanical exposure and musculoskeletal health good performance indicators for primary interventions? Int Arch Occup Environ Health. 2002;75:549–61. doi: 10.1007/s00420-002-0368-7. [DOI] [PubMed] [Google Scholar]
- 122.Shain M, Kramer DM. Health promotion in the workplace: framing the concept; reviewing the evidence. Occup Environ Med. 2004;61:643–8. doi: 10.1136/oem.2004.013193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Swedish National Committee for Public Health. Health on equal terms—national goals for public health. Scand J Public Health Suppl. 2001;57:1–68. [PubMed] [Google Scholar]
- 124.Omenn GS, Goodman G, Thornquist M, Barnhart S, Balmes J, Cherniack M, et al. Chemoprevention of lung cancer: the beta-carotene and retinol efficacy trial (CARET) in high-risk smokers and asbestos-exposed workers. Lyon (France): IARC; 1996. [PubMed] [Google Scholar]
- 125.Hignett S, Wilson JR, Morris W. Finding ergonomic solutions—participatory approaches. Occup Med (Lond) 2005;55:200–7. doi: 10.1093/occmed/kqi084. [DOI] [PubMed] [Google Scholar]
- 126.Imada AS. Macroergonomics: theory, methods, and applications. Mahwah (NJ): Lawrence Erlbaum Associates; 2002. A macroergonomic approach to reducing work-related injuries. In: Hendrick HW, Kleiner BM, editors; pp. p. 151–72. [Google Scholar]
- 127.Ozminkowski RJ, Dunn RL, Goetzel RZ, Cantor RI, Murnane J, Harrison M. A return on investment evaluation of the Citibank, N.A , health management program. Am J Health Promot. 1999;14:31–43. doi: 10.4278/0890-1171-14.1.31. [DOI] [PubMed] [Google Scholar]
- 128.Chapman LS. Meta-evaluation of worksite health promotion economic return studies: 2005 update. Am J Health Promot. 2005;19:1–11. doi: 10.4278/0890-1171-19.4.TAHP-1. [DOI] [PubMed] [Google Scholar]
- 129.Serxner SA, Gold DB, Grossmeier JJ, Anderson DR. The relationship between health promotion program participation and medical costs: a dose response. J Occup Environ Med. 2003;45:1196–200. doi: 10.1097/01.jom.0000095002.12772.6a. [DOI] [PubMed] [Google Scholar]
- 130.Abrams DB, Emmons KM, Linnan L, Biener L. In: Richmond R, editor. Interventions for smokers: an international perspective. New York: Williams – Wilkins; 1994. Smoking cessation at the workplace: conceptual and practical considerations; pp. p. 137–69. [Google Scholar]
- 131.Emmons KM. Promoting health: intervention strategies from social and behavioral research. Washington: National Academy Press; 2000. Behavioral and social science contributions to the health of adults in the United States. In: Smedley BD, Syme SL, editors; pp. p. 254–321. [Google Scholar]
- 132.Pelletier KR. A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: 1995–1998 update. Am J Health Promot. 1999;13:333–45. doi: 10.4278/0890-1171-13.6.333. [DOI] [PubMed] [Google Scholar]
- 133.Terborg JR, Glasgow RE. Cambridge handbook of psychology, health and medicine. London: Cambridge University Press; 1997. Worksite interventions. In: Baum A, Newman S, Weinman J, West R, McManus C, editors; pp. p. 264–8. [Google Scholar]
- 134.Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: conceptual filters explain underreporting. Am J Public Health. 2002;92:1421–9. doi: 10.2105/ajph.92.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Azaroff LS, Lax MB, Levenstein C, Wegman DH. Wounding the messenger: the new economy makes occupational health indicators too good to be true. Int J Health Serv. 2004;34:271–303. doi: 10.2190/4H2X-XD53-GK0J-91NQ. [DOI] [PubMed] [Google Scholar]
- 136.Biddle J, Roberts K, Rosenman KD, Welch EM. What percentage of workers with work-related illnesses receive workers' compensation benefits? J Occup Environ Med. 1998;40:325–31. doi: 10.1097/00043764-199804000-00006. [DOI] [PubMed] [Google Scholar]
- 137.Morse T, Dillon C, Warren N. Reporting of work-related musculoskeletal disorder (MSD) to workers compensation. New Solut. 2000;10:281–92. doi: 10.2190/GXAR-M4FY-BAR1-UQB5. [DOI] [PubMed] [Google Scholar]
- 138.Punnett L. The costs of work-related musculoskeletal disorders in automotive manufacturing. New Solut. 1999;9:403–26. doi: 10.2190/Y93Q-DEAQ-FEU2-8B26. [DOI] [PubMed] [Google Scholar]
- 139.Bryan A, Fisher JD, Fisher WA. Tests of the mediational role of preparatory safer sexual behavior in the context of the theory of planned behavior. Health Psychol. 2002;21:71–80. [PubMed] [Google Scholar]
- 140.Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002;21:177–86. [PubMed] [Google Scholar]
- 141.Garber AM. Evidence-based coverage policy. Health Aff (Millwood) 2001;20:62–82. doi: 10.1377/hlthaff.20.5.62. [DOI] [PubMed] [Google Scholar]
- 142.Oxenburgh M, Marlow P, Oxenburgh A. Increasing productivity and profit through health and safety: the financial returns from a safe working environment. 2nd ed. Boca Raton (FL): CRC Press; 2004. [Google Scholar]
- 143.Lahiri S, Gold J, Levenstein C. Net-cost model for workplace interventions. J Safety Res. 2005;36:241–55. doi: 10.1016/j.jsr.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 144.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 145.Henning R, Warren N, Robertson M, Faghri P, Cherniack M the CPH-NEW Research Team. Workplace health protection and promotion through participatory ergonomics: an integrated approach. Public Health Rep. 2009;124(Suppl 1):26–35. doi: 10.1177/00333549091244S104. [DOI] [PMC free article] [PubMed] [Google Scholar]