Abstract
Chronic pain, a debilitating medical condition affecting approximately 15% of the US population, leads to individual suffering and costs to society in terms of health care dollars and lost productivity. To examine the effectiveness of a comprehensive pain management program, data from 108 program participants were evaluated. Preprogram, postprogram, and 6-month follow-up data were collected from 80 participants, and preprogram, postprogram, and 1-year data were collected from 46 participants. Outcomes data from several domains were assessed: pain severity, emotional distress, interference of pain on function, perceived control of pain, treatment helpfulness, and number of hours resting. Within-subject repeated-measure analyses of variance found statistically significant findings on the six outcome measures utilized in this study for both the 6-month and 1-year samples. Examination of 95% confidence intervals revealed no overlap in pretreatment scores with 6-month and 1-year outcomes in five of the six domains studied. Mean scores on emotional distress did not maintain statistical significance in the 6-month or 1-year review. Overall, this study strengthens the case for interdisciplinary care for chronic pain management and provides evidence for the long-term effectiveness of this therapy. Furthermore, this study lends support to the notion that interdisciplinary treatments are effective in targeting multiple domains affected by the pain condition.
Chronic pain is a debilitating condition that causes an individual distress and has a societal impact in terms of days of lost work and dollars spent on health care (1). Yearly estimates of health care costs in the USA for the effects of chronic pain range from $100 to $150 billion (2, 3). This number is likely an underestimate, as these data were produced over a decade ago. These figures underscore the need for improved treatment strategies and innovative approaches to pain management.
The comprehensive outpatient program at the Baylor Center for Pain Management in Dallas, Texas, was developed to address the multifaceted needs of these patients. Baylor's interdisciplinary pain program is accredited by the Commission on Accreditation of Rehabilitation Facilities. Patients engage in treatment 6 hours per day, 5 days per week, for 4 weeks.
The program is based on a biopsychosocial approach. Although chronic pain initially begins as a biological event—in which electrical and chemical processes occur within the body as a response to noxious stimuli—psychological, social, and cultural factors enter into the process. Previous experiences with pain, consequences of pain, mood, and stress, among other factors, quickly influence initial reactions to the pain sensation (4).
As time progresses, psychosocial factors become increasingly important in the maintenance of pain. The interactions of these events may lead to multiple areas that complicate pain management. As pain continues, individuals often react by decreasing activity level and developing beliefs that “hurt” equals “harm.” As social and recreational activities decrease, patients often become isolated from friends and family and no longer engage in activities they previously enjoyed. Interpersonal relationships become strained, as interactions often are focused on the pain, causing friends and family members to become frustrated and angry. The negative impact on multiple life areas frequently leads to a perception of a lack of control or self-efficacy in managing pain (4).
Effective treatment strategies should address all aspects of the pain experience. Thus, interdisciplinary treatment programs attempt to incorporate elements targeting the biological, psychological, and social factors that serve to maintain and even exacerbate pain. Specifically, interdisciplinary care involves the active participation and coordination of medical specialists from different fields with a focus on pain management. Typically, these programs consist of physicians, psychologists, counselors, physical therapists, case managers, occupational therapists, and other health professionals (e.g., psychiatrists, nursing staff, etc.). In most interdisciplinary programs, treatment consists of physical therapy, cognitive behavioral therapy, and instruction in self-regulatory techniques, enhanced with group educational meetings. The goals of interdisciplinary care include providing skills in decreasing muscle tension and sympathetic nervous system activation by addressing and reframing beliefs about pain and coping. The patients are guided in overcoming fear and avoidance of behavior associated with pain and in improving physical strengthening and conditioning.
Interdisciplinary treatment programs have been demonstrated to serve as an effective approach for chronic pain management and the ensuing disability that results from pain (5–7). Additional research into the long-term effectiveness of these programs would add to the growing literature that supports these long-term benefits. Robbins, Gatchel, Noe, and colleagues (8) studied an interdisciplinary pain program and found significant improvements in pain and functioning 1 year later, which supports observations from other studies (9, 10). This study examined a heterogeneous pain population seen at the Baylor Center for Pain Management at Baylor University Medical Center to determine the effectiveness of maintaining changes in a variety of life domains at 6-month and 1-year intervals after discharge from treatment.
METHODS
Data from 108 participants with chronic pain who completed a comprehensive pain program at Baylor University Medical Center were analyzed. The study was approved by Baylor's institutional review board. All participants were initially evaluated by a physician and clinical psychologist and, based on input from the treatment team, were referred to the comprehensive outpatient program. Patients who were referred to less-intensive treatment programs were not included in the analysis. Preprogram, postprogram, and 6-month follow-up data were collected from 80 participants, and preprogram, postprogram, and 1-year data were collected from 46 participants. Since certain patients could not be reached at 6-month and 1-year follow-ups, separate within-subject repeated-measure analyses of variance were run utilizing 6-month and 1-year data. Both 6-month and 1-year data were collected on 18 of the 108 participants.
Each participant completed two questionnaires at the onset of the comprehensive program and upon discharge from the program. The first, the Multidimensional Pain Inventory (MPI), provides information on psychosocial and behavioral functioning (11). Von Korff (12) developed a shortened version of the MPI that consists of eight questions in four domains: pain severity, emotional distress, interference of pain on functioning, and perceived control of pain. Scores range from 0 to 12 on each scale. The second, the Daily Life Questionnaire (DLQ), consists of questions related to pain chronicity, health care utilization, hours resting per day, treatment helpfulness, and other relevant demographic information. Participants were asked to rate helpfulness of treatment for managing their pain on a scale of 1 (not helpful) to 10 (very helpful). Participants were also asked to indicate how many hours a day (i.e., 8:00 am to 8:00 pm) they rested or reclined due to pain.
Only a subset of these questions were used at 6-month and 1-year follow-up interviews, which were conducted by phone when possible.
Six treatment components were administered:
Individual behavioral medicine sessions (8 sessions). The sessions taught self-regulatory skills, such as relaxation training, within a cognitive-behavioral therapy framework. This framework allows for maladaptive thoughts regarding pain to be addressed. Furthermore, the sessions increased patients' self-efficacy through the development of multiple tools that improve pain coping, such as distraction and pacing.
Physical therapy (19 sessions). Tailored physical therapy goals were determined at the onset of treatment, with emphasis on flexibility and core strengthening.
Aquatic physical therapy (15 sessions). Aquatic therapy was also incorporated to safely improve strength and conditioning.
Occupational therapy (19 sessions). These sessions focused on developing adaptive changes in daily living.
Group education (19 sessions). Group education sessions provided for the dissemination of information regarding managing chronic pain. Topics ranged from nutrition to the relationship between stress and pain. Patient group interaction was encouraged as a source of additional information and motivation.
Group relaxation (11 sessions). Instruction in relaxation and other self-regulatory techniques was provided within a group setting and was meant to complement the more tailored efforts within the individual behavioral medicine sessions.
RESULTS
Of the 108 participants, 70% were female and 63% suffered from low back pain (Table 1). The mean duration of pain for the sample was 110.44 months (standard deviation [SD], 136.73 months; range, 3 months to 62 years). These numbers are similar to those found in the entire population of pain patients treated at this site.
Table 1.
Demographic characteristics of the 108 participants
| Variable | Result |
| Mean age: years (SD) | 55 (11.47) |
| Duration of pain: months (SD) | 110.44 (136.73) |
| Gender | |
| Male | 32 (29.6%) |
| Female | 76 (70.4%) |
| Race/ethnicity | |
| African American | 14 (13%) |
| Latino | 4 (3.7%) |
| White/Non-Hispanic | 90 (83.3%) |
| Marital status | |
| Single | 10 (9.3%) |
| Married/cohabitating | 74 (68.5%) |
| Divorced/separated | 17 (15.7%) |
| Widowed/other | 7 (6.5%) |
| Diagnosis | |
| Lumbar | 68 (63%) |
| Thoracic | 3 (2.8%) |
| Cervical | 17 (15.7%) |
| Myofascial | 2 (1.9%) |
| Headache | 3 (2.8%) |
| Neuropathy/neuralgia | 5 (4.6%) |
| Other | 10 (9.3%) |
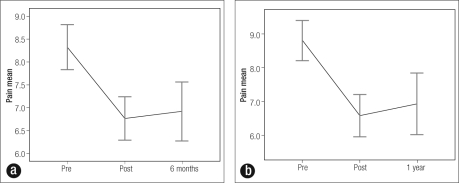
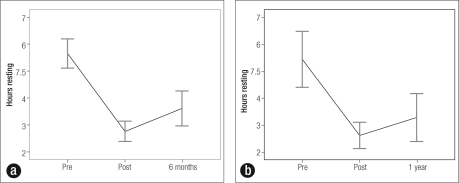
Within-subject repeated-measure analyses of variance found statistically significant findings on the six outcome measures used in this study (Tables 2 and 3). Pain severity decreased significantly in the 6-month sample, with a 19% decrease in pain severity by the end of treatment (P < .001). A 17%decrease was noted when pretreatment scores were compared with 6-month data. Further, 95% CI values revealed no overlap between pretreatment pain severity scores (mean = 8.33; 95% CI 7.84–8.82) and 6-month pain severity scores (mean = 6.93; 95% CI 6.28–7.57) (Figure 1a). Analyses for those followed for 1 year yielded significant results (P < .001) that were similar to the 6-month sample. In the 1-year sample, a 25% decrease of pain severity at posttreatment and a 21% decrease of pain severity at 1-year follow up was found. As with the 6-month sample, 95% CI values revealed no overlap between pretreatment and 1-year pain severity scores (Figure 1b). The number of hours resting also de creased significantly (P < .001): in the 6-month sample, there was a 51% decrease in hours resting by the end of treatment and a 36% decrease when pretreatment scores were compared with 6-month data; in the 1 year sample, the decrease was 52% and 40%, respectively (Figure 2). The CIs revealed no overlap between pretreatment and 6-month values.
Table 2.
Within-subject repeated-measure analysis of variance of outcomes of a comprehensive pain management program for 80 participants with a 6-month follow-up
| Mean ± standard error (95% confidence interval) |
|||||
| Variable | Pretreatment | Posttreatment | 6-month follow-up | F-statistic (df) | P value |
| Pain severity (n = 80) |
8.33 ± .25 (7.84–8.82) | 6.78 ± .24 (6.30–7.25)∗ | 6.93 ± .32 (6.28–7.57)∗ | 17.820 (2) | <.001 |
| Interference (n = 80) |
10.05 ± .27 (9.51–10.59) | 7.9 ± .23 (7.26–8.54)∗ | 7.35 ± .44 (6.47–8.23)∗ | 25.205 (2) | <.001 |
| Distress (n = 80) |
7.19 ± .36 (6.47–7.91) | 4.53 ± .32 (3.88–5.17)∗ | 6.53 ± .34 (5.86–7.19) | 22.391 (2) | <.001 |
| Control (n = 80) |
6.27 ± .29 (5.71–6.85) | 8.56 ± .24 (8.08–9.05)∗ | 8.6 ± .29 (8.07–9.19)∗ | 36.449 (2) | <.001 |
| Helpfulness (n = 74) |
3.15 ± .27 (2.6–3.69) | 7.2 ± .27 (6.66–7.74)∗ | 7.14 ± .3 (6.54–7.73)∗ | 101.461 (2) | <.001 |
| Hours resting (n = 74) |
5.65 ± .27 (5.12–6.19) | 2.77 ± .19 (2.39–3.15)∗ | 3.62 ± .32 (2.97–4.26)∗ | 48.819 (2) | <.001 |
∗No overlap in 95% confidence interval between pretreatment and either posttreatment or 6-month scores.
Table 3.
Within-subject repeated-measure analysis of variance of outcomes of a comprehensive pain management program for 46 participants with a 1-year follow-up
| Mean ± standard error (95% confidence interval) |
|||||
| Variables | Pretreatment | Posttreatment | 1-year follow-up | F-statistic (df) | P value |
| Pain severity (n = 46) |
8.8 ± .29 (8.21–9.40) | 6.59 ± .31 (5.96–7.21)∗ | 6.94 ± .45 (6.03–7.84)∗ | 20.744 (2) | <.001 |
| Interference (n = 46) |
10.43 ± .30 (9.83–11.04) | 8.04 ± .42 (7.19–8.90)∗ | 7.35 ± .56 (6.22–8.48)∗ | 16.887 (2) | <.001 |
| Distress (n = 46) |
7.07 ± .49 (6.08–8.05) | 3.91 ± .38 (3.15–4.67)∗ | 5.57 ± .45 (4.65–6.48) | 15.819 (2) | <.001 |
| Control (n = 46) |
5.91 ± .29 (5.10–6.72) | 8.8 ± .24 (8.16–9.45)∗ | 8.67 ± .29 (8.02–9.33)∗ | 40.386 (2) | <.001 |
| Helpfulness (n = 46) |
2.37 ± .22 (1.93–2.81) | 7.35 ± .29 (6.76–7.93)∗ | 7.13 ± .4 (6.34–7.93)∗ | 95.903 (2) | <.001 |
| Hours resting (n = 40) |
5.45 ± .51 (4.42–6.48) | 2.63 ± .24 (2.14–3.12)∗ | 3.29 ± .44 (2.40–4.18)∗ | 16.976 (2) | <.001 |
∗No overlap in 95% confidence interval between pretreatment and either posttreatment or 1-year scores.
Figure 1.
Pain severity rating: mean and 95% confidence interval bars for preprogram, postprogram, and follow-up data for (a) 80 participants with a 6-month follow-up and (b) 46 participants with a 1 -year follow-up
Figure 2.
Number of hours resting per day: mean and 95% confidence interval bars for preprogram, postprogram, and follow-up data for (a) 80 participants with a 6-month follow-up and (b) 46 participants with a 1-year follow-up
Similarly, results for the interference from pain, perceived control of pain, and perceived helpfulness of treatment measures were significant in both the 6-month and 1 year sample, with no overlap in the 95% CI pretreatment and posttreatment values.
Emotional distress significantly decreased between the pretreatment and completion of treatment measures (a 37% decrease among the 6-month group and a 45% decrease among the 1-year group), but values at 6-month and 1-year follow-up approached the pretreatment levels.
DISCUSSION
The results of this study support the effectiveness of this interdisciplinary program. Consistent with prior studies (5–10), measures of pain, emotional distress, and function all showed significant improvement after 4 weeks of comprehensive interdisciplinary care. Additionally, in both the 6-month and 1-year samples, the benefit was maintained for pain severity, interference of pain on lifestyle, perception of control of pain, perception of helpfulness of pain management techniques, and number of hours resting.
In spite of the observed decreases in emotional distress from pretreatment to posttreatment, emotional distress scores returned to levels that fell within the 95% CIs of pretreatment scores. In the 6-month sample, scores returned to within 9% of pretreatment scores. This finding may reflect an adjustment period, as many individuals who leave the comprehensive program have stressors related to work and family life with which they continue to contend. Although 1-year emotional distress scores still fell within the 95% CIs of pretreatment scores, the difference reached 21%. The results support the hypothesis of an adjustment period resolving and emotional distress levels approaching the levels of improvement commensurate with those of pain severity, hours resting, and other significant outcomes. Furthermore, a 21% decrease in emotional distress 1 year after discharge, while not statistically significant in the research, is arguably clinically significant.
Overall, the study results lend support to the notion that interdisciplinary treatments are effective in targeting multiple domains affected by the pain condition. They also support the justification of interdisciplinary care for third-party payers. Further, results provide guidance for future areas of clinical research and interventions. Clearly, additional well-controlled randomized studies examining outcomes 1 and 2 years after discharge would strengthen the findings, as would examination of moderating and mediating variables of change. Finally, these results suggest the need for continued follow-up care to assist in the maintenance of gains regarding levels of emotional distress.
References
- 1.Chronic Pain Management Programs: A Market Analysis. Valley Stream, NY: Author; 1995. Marketdata Enterprises. [Google Scholar]
- 2.National Institutes of Health . The NIH Guide: New Directions in Pain Research I. Washington, DC: US Government Printing Office; 1998. [Google Scholar]
- 3.US Census Bureau . Statistical Abstract of the United States: 1996. Washington, DC: US Bureau of the Census; 1996. [Google Scholar]
- 4.Gatchel RJ. Clinical Essentiah of Pain Management. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- 5.Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992;49(2):221–230. doi: 10.1016/0304-3959(92)90145-2. [DOI] [PubMed] [Google Scholar]
- 6.Dysvik E, Vinsnes AG, Eikeland OJ. The effectiveness of a multi-disciplinary pain management programme managing chronic pain. Int J Nurs Pract. 2004;10(5):224–234. doi: 10.1111/j.1440-172X.2004.00485.x. [DOI] [PubMed] [Google Scholar]
- 7.Johansson C, Dahl J, Jannert M, Melin L, Andersson G. Effects of a cognitive-behavioral pain-management program. Behav Res Ther. 1998;36(10):915–930. doi: 10.1016/s0005-7967(98)00079-5. [DOI] [PubMed] [Google Scholar]
- 8.Robbins H, Gatchel RJ, Noe C, Gajraj N, Polatin P, Deschner M, Vakharia A, Adams L. A prospective one-year outcome study of interdisciplinary chronic pain management: compromising its efficacy by managed care policies. Anesth Analg. 2003;97(1):156–162. doi: 10.1213/01.ane.0000058886.87431.32. [DOI] [PubMed] [Google Scholar]
- 9.Becker N, Sj⊘gren P, Bech P, Olsen AK, Eriksen J. Treatment outcome of chronic non-malignant pain patients managed in a Danish multidisciplinary pain centre compared to general practice: a randomised controlled trial. Pain. 2000;84(2–3):203–211. doi: 10.1016/s0304-3959(99)00209-2. [DOI] [PubMed] [Google Scholar]
- 10.Patrick LE, Altmaier EM, Found EM. Long-term outcomes in multidisciplinary treatment of chronic low back pain: results of a 13-year follow-up. Spine. 2004;29(8):850–855. doi: 10.1097/00007632-200404150-00006. [DOI] [PubMed] [Google Scholar]
- 11.Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23(4):345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 12.Von Korff M. Epidemiologie and survey methods: chronic pain assessment. In: Turk DC, Melzack R, editors. Handbook of Pain Assessment. New York: Guilford Press; 1992. pp. 391–408. [Google Scholar]