“A new wave of technological innovation is allowing us to capture, store, process and display an unprecedented amount of information about our planet and a wide variety of environmental and cultural phenomena. Much of this information will be ‘geo-referenced’ - that is, it will refer to some specific place on the Earth's surface. The hard part of taking advantage of this flood of geospatial information will be making sense of it, turning raw data into understandable information. Today, we often find that we have more information than we know what to do with… Now we have an insatiable hunger for knowledge. Yet a great deal of data remains unused. Part of the problem has to do with the way information is displayed.” - Former American Vice President Al Gore1
At the Global Ministerial Forum on Research for Health held in Bamako, Mali, 17–19 November 2008, ministers from 59 countries adopted a call to action on research for health. One of the adopted measures was “To harness the potential of research by drawing on new sciences, emerging technologies and social and technological innovations to address priority health challenges”.2 Indeed, in the attempt to address health problems and prioritization of health services and resource allocation, there is the need for health information systems to support the decision-making process. One such system and technology draws on the importance of geographic location in health and disease, which is strongly emphasized by the classic public health triad of man, agent and environment. Interactions within this triad can change with time, allowing geography to play a major role in understanding the dynamics of health, and the causes and spread of disease.3
In recent years, health planners aim at developing health policies and services that address geographical and social inequalities in health, and therefore should benefit from evidence-based approaches that can be used to investigate spatial aspects of health policy and practice, and evaluate geographical equity (or inequity) in health service provision and management.4 Public health practitioners also have important and related tasks of prioritizing interventions and programs, providing emergency health responses, intersectorial engagement, and community development initiatives. In all these tasks, there is the need to integrate searching for and using best evidence in everyday decision-making processes so as to minimize investment of efforts and funds in areas where there is solid evidence of no effect or of poor cost-effectiveness. Evidence-based approaches can also highlight areas where the evidence may be less than reliable, requiring further assessment before spending large amounts of resources (financial and human). If possible, the tools to accomplish this goal should be available to public health practitioners, transparently embedded into routine workflows, and built into existing work environments.5
In many countries, data generated by the health sector is geography based. This spatial reference is vital in the conversion of data into information, and for combining multiple datasets covering same and adjacent areas.6 The US National Library of Medicine, in 2003, added the term “Geographic Information Systems” (GIS) to its Medical Subject Headings7, reflecting the importance and growing use of GIS in health, towards the provision of an evidence-based approach to decision-making.
GIS is an automated system for the capture, storage, retrieval, analysis, and display of spatial data.8 It provides means of analyzing epidemiological data, revealing trends, dependencies and inter-relationships that would be more difficult to discover in tabular format. At the same time, it provides a mechanism to integrate various data sets, analyze their spatial and statistical components, and model possible scenarios, thereby supporting interdisciplinary research.
Nonetheless, the link between geography and medical data has not been well defined, and health information systems have been weak due to multiple case definitions, irregular reporting, under reporting and poor coordination.
The need to put in place an effective and efficient information system including climatic and health parameters could be an appropriate strategy to better monitor the occurrence, distribution and control of parasitic diseases in different geographical areas and time periods. This could also serve as an instrument for defining events that can be used to predict potential epidemics, and to adapt and implement appropriate control strategies. Applications of GIS in health research could be done by relating epidemiological information to, for example, environmental factors that are likely to influence the distribution of diseases.
The use of remote sensing (RS) techniques in the collection of meteorological data can further enhance GIS applications by providing proxy environmental information derived from satellite sensors9, especially when the collection of meteorological data in developing countries is inadequate due to the lack of infrastructure.
GIS are potentially powerful resources for community health for many reasons including their ability to integrate data from multiple sources to generate new information. Their inherent visualization functions, which allow one to view data in ways not possible in tabular formats, can promote creative problem solving and sound decisions with lasting, positive impacts on people's lives.10, 11 Due to the problems encountered in identifying, acquiring and integrating a wide range of geo-referenced data relevant to health in order to support decision-making and problem-solving in planning health activities, service delivery, and health promotion, GIS have been usually applied to time-limited, aggregated data, singly isolated etiological research or surveillance issues processing mainly retrospective data rather than to ongoing, wide-scale applications processing real-time data. It must be noted that any health-related phenomenon that can be defined spatially (atmospheric, aquatic or terrestrial) can be subjected to GIS analysis.12
GIS applications range from studying disease patterns (e.g., identify geo-spatial hotspots of tuberculosis), identifying spatio-temporal variations in health outcomes, and possible causes of mapped patterns (e.g., the relationship between asthma incidence and air pollution). However, they usually involve identifying the link between health information and environmental and socio-economic data. GIS have also been used in resource allocation for disease prevention by highlighting areas with significantly high rates, and predicting areas which might be at future risk and which may benefit most from future local population screening13. Together, GIS and remote sensing have been used successfully to explain the distribution of various infectious diseases with application to disease control14 and in the implementation of national control programs for onchocerciasis15 and filariasis.16
GIS can also be used to plan healthcare delivery, accessibility and utilization of healthcare facilities, and aid resource allocation in providing better health to all. In order to be truly integrated into the strategic decision-making process, these applications should incorporate task-appropriate statistical and modeling techniques, e.g., spatial interaction models (allowing proposed health services/centers to be added interactively to assess their impact), and location-allocation models in order to forecast and evaluate the implication of modifying the configuration of existing services, and thus play a proactive role in the healthcare planning process. GIS have been used in studies to estimate the best/optimal location for a new clinic or hospital to minimize distances potential patients need to travel taking into account existing facilities, transport provision and population density. A number of these studies using the networking capabilities of GIS have been concerned with the concept of potential accessibility, while the revealed accessibility patterns of health service utilization has been the concern of other studies based on spatially disaggregated data.13
GIS health applications in Ghana are few, with little or perhaps no effects on policy and decision making. In the Ghana National Health Policy document17 there is no mention of the role of spatial information in health improvement programs or performance management. However, the importance of Health Information Systems (HIS) is clearly identified. Including GIS as part of HIS can go a long way in promoting the generation and use of evidence for decision-making, program development, resource allocation and surveillance systems. The potential for GIS to support partnership approaches for providing and exchanging information on such issues at national or local scales and integrating data from the various sources could also be exploited.
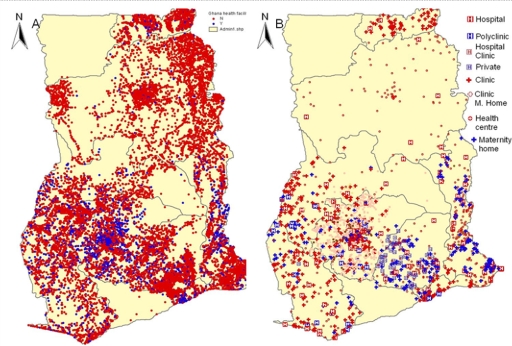
The rest of this article will demonstrate some practical aspects of Health GIS in Ghana. The data from the HealthMapper, a basic mapping and surveillance software developed by WHO's Communicable Disease Surveillance and Response Department18, which contains coordinates of most communities together with the respective health centers and hospitals are plotted to show the disparities in health facilities in the country (Figure 1 A and B). The plots exclude data from the Central and Upper West Region, which were not available.
Figure 1A.
Distribution of health facilities in Ghana; 1B: Health facility types in Ghana.
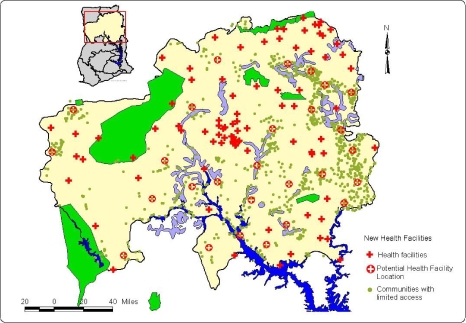
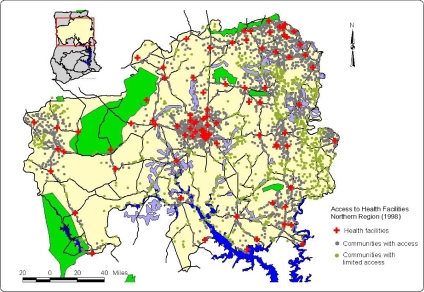
These maps combined with population density maps could actually reveal areas that need to be provided with many more facilities and could be used for decision making when providing health services to the population (Figures 2A and 2B). Based on these maps, the best/optimal location for a new clinic or hospital to reduce travelling distances to access health services taking into account existing facilities, transportation could be determined.
Figure 2A.
Communities with full access and limited access in the Northern Region of Ghana, based on a Euclidean distance of 16 km from the health facility.
Figure 2B.
Placement of new health facilities to provide access to communities with limited access, in the Northern Region of Ghana.
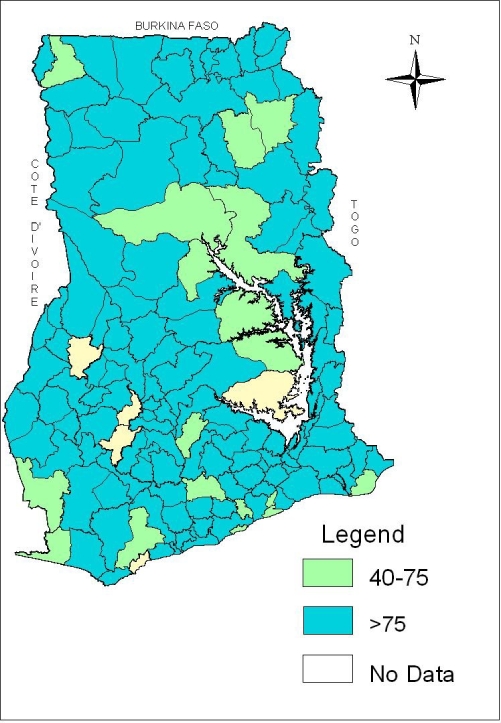
Another example of the practical use of GIS in decision-making is from the 2007 Ghana National Deworming Programme.19 The distribution of the treatment coverage in the country is presented in Figure 3. The map shows the percentage coverage by districts that meet the WHO's recommendation of covering at least 75% of the target population.
Figure 3.
Percentage coverage of national deworming program by district that met the WHO recommended levels of greater than 75%
Even though these maps are very simple in nature, revealing the simplest application of GIS, the beauty is in the ability to spatially observe the information. There is a gap between academic health-related applications of GIS and their everyday use in Ghana and within the Ghana Health Service (GHS). Therefore, there is the need for closer collaboration between GIS academics and GHS professionals to advance health-based GIS work.
Many benefits can be derived from setting up a health GIS infrastructure in Ghana. Among these are:
Mapping disease prevalence and determining factors hindering disease control programs in different areas/districts in Ghana
Improving community health and healthcare practices
Improving health services provision and healthcare access to deprived communities
Identifying and solving the challenges and problems currently facing the implementation of the National Health Insurance Scheme in various districts in Ghana
Identifying the most important requirements and ingredients for addressing health challenges, and realizing GIS potential within the GHS, guided by related initiatives worldwide.
Illuminating the road towards implementing a comprehensive national, multi-agency spatio-temporal health information infrastructure functioning proactively in real time.
Working in accordance with WHO's Public Health Mapping and GIS program aimed at leading a global partnership in the promotion and implementation of GIS to support decision-making for a wide range of infectious diseases and public health programs.
Providing consistent and reliable epidemiological information to the ministry of health and national control programs, enabling them to precisely locate and profile target populations without time-consuming and costly field research.
The objective of the Ghana National Health Policy with regards to Health Information Systems is “to promote the generation and use of evidence for decision-making, programme development, resource allocation and management through research, statistics, information management and deployment of ICT”.17
As the National Health Policy seeks to achieve health for all Ghanaians and achieve a middle income status by 2015, it is important to take advantage of every technological innovation that can assist in the set up of an integrated National Spatial Health Information Infrastructure System. This system can collect, analyze and interpret health-related information for the prevention of a wide range of health problems, or at least the early detection of such problems in order to mitigate their effects. Such surveillance service will require a sound and comprehensive spatial health data and information infrastructure to be built and maintained in a coherent way at all operation levels.
Acknowledgement
I would like to thank Dr. Collins Ahorlu of the Epidemiology Department of the Noguchi Memorial Institute for Medical Research for proof-reading this paper.
References
- 1.Gore A. The Digital Earth: Understanding our Planet in the 21st Century; Speech given at the California Science Centre; 31 January 1998; Los Angeles, California. http://www.digitalearth.gov/VP19980131.html. [Google Scholar]
- 2.The Bamako Call to Action on Research for Health from the Global Ministerial Forum on Research for Health Bamako, Mali, 17–19 November 2008. http://bamako2008.org/dmdocuments/Call%20to%20Action%20_E.pdf.
- 3.Davenhall B. Building a Community Health Surveillance System. ArcUser Online. 2002 [ http://www.esri.com/news/arcuser/0102/comhealth1of2.html]
- 4.Higgs G, Richards W. The use of geographical information systems in examining variations in sociodemographic profiles of dental practice catchments: a case study of a Swansea practice. Prim Dent Care. 2002;9(2):63–69. doi: 10.1308/135576102322527829. [DOI] [PubMed] [Google Scholar]
- 5.Waters E, Doyle J. Evidence-based public health: Cochrane update. J Public Health Med. 2003;25(1):72–75. doi: 10.1093/pubmed/fdg015. [DOI] [PubMed] [Google Scholar]
- 6.The Nairobi Statement on Spatial Information for Sustainable Development. FIG Publication no 30 - Recommendations of the International Conference on Spatial Information for Sustainable Development, Nairobi, Kenya, 2–5 October 2001. Frederiksberg, Denmark: The International Federation of Surveyors (FIG); http://www.fig.net/figtree/pub/figpub/pub30/figpub30.htm. [Google Scholar]
- 7.Medical Subjects Headings. http://www.nlm.nih.gov/cgi/mes200MB_cgi?term=GEOGRAPHIC+INFORMATION+SYSTEMS.
- 8.Clarke KC. Analytical and Computer Cartography. 2nd edition. Upper Saddle River, NJ: Prentice Hall; 1995. [Google Scholar]
- 9.Hay SI. An overview of remote sensing and geodesy for epidemiology and public health applications. Advances in Parasitology. 2000;47:2–27. doi: 10.1016/s0065-308x(00)47005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buckeridge DL, Mason R, Robertson A, Frank J, Glazier R, Purdon L, Amrhein CG, Chaudhuri N, Fuller-Thomson E, Gozdyra P, Hulchanski D, Moldofsky B, Thompson M, Wright R. Making health data maps: a case study of a community/ university research collaboration. Soc Sci Med. 2002;55(7):1189–1206. doi: 10.1016/s0277-9536(01)00246-5. [DOI] [PubMed] [Google Scholar]
- 11.Gavin E other member of EIS-AFRICA, author. Geo-Information Supports Decision-Making in Africa - An EIS-AFRICA Position Paper 2002 Pretoria, South Africa: EISAFRICA. http://www.eis-africa.org/DOCS/A5-Engv7.pdf.
- 12.Croner CM, Sperling J, Broome FR. Geographic information systems (GIS): new perspectives in understanding human health and environmental relationships. Stat Med. 1996;15(17–18):1961–1977. doi: 10.1002/(sici)1097-0258(19960930)15:18<1961::aid-sim408>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 13.Higgs G, Gould M. Is there a role for GIS in the ‘new NHS’? Health Place. 2001;7(3):247–259. doi: 10.1016/s1353-8292(01)00014-4. [DOI] [PubMed] [Google Scholar]
- 14.Hay SI, Randolph S, Rogers DJ. Remote sensing and geographical information systems in epidemiology. London: Academic Press; 2000. [Google Scholar]
- 15.Ngoumou P, Walsh JF, Mace JM. A rapid mapping technique for the prevalence and distribution of onchocerciasis: a Cameroon case study. Annals of Tropical Medicine and Parasitology. 1994;88:463–474. doi: 10.1080/00034983.1994.11812893. [DOI] [PubMed] [Google Scholar]
- 16.Lindsay SW, Thomas CJ. Mapping and estimating the population at risk from lymphatic filariasis in Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2000;94:37–44. doi: 10.1016/s0035-9203(00)90431-0. [DOI] [PubMed] [Google Scholar]
- 17.Ghana National Health Policy, Creating Wealth Through Health. Ministry of Health; 2007. Sep, [Google Scholar]
- 18.World Health organization, author. The Health Mapper. Available at: http://www.who.int/health_mapping/tools/healthmapper/en/index.html/
- 19.Ghana National De-worming Programme, School Health Education Programme, Ghana Education Service. 2007