Abstract
Objective:
To examine whether social inequalities in all-cause and coronary heart disease (CHD) mortality in Britain have reduced between 1978-2005.
Design:
Prospective study of a socio-economically representative population
Setting:
24 British towns
Participants:
7735 men, aged 40-59 years at recruitment in 1978-80 and followed-up until 2005 through the National Health Service Central Register (164,120 person years).
Main outcome measures:
Relative hazards and absolute risk differences for all-cause and CHD death comparing manual with non-manual social classes, calculated for different calendar periods.
Results:
3009 deaths from all-causes (1003 from CHD) occurred during follow-up. The overall hazard ratio (manual vs. non-manual) was 1.56 (95%CI 1.45-1.69, p<0.001) for all-cause mortality and 1.54 (95%CI 1.35-1.76, p<0.001) for CHD mortality. However, the relative difference between these social groups tended to increase over time. The overall relative increase in hazard ratio comparing manual to non-manual groups over a 20-year calendar period was 1.22 (95%CI 0.83-1.80, p=0.31) for all-cause mortality and 1.75 (95%CI 0.89-3.45, p=0.11) for CHD mortality. However, the absolute difference in probability of survival to age 65 between non-manual and manual groups fell from 29% in 1981 to 19% in 2001 for all-cause mortality and from 17% to 7% for CHD mortality.
Conclusion:
Relative differences in all-cause and CHD mortality between manual and non-manual social class groups persisted and may have increased during this period. However, absolute differences in mortality between these social groups decreased because of falling overall mortality rates. Greater effort is needed to reduce social inequalities in all-cause and CHD mortality in the new millennium.
Marked social inequalities in health and mortality in the UK have been present for many years.[1] The Independent Inquiry into Inequalities in Health[2] summarised evidence that social inequalities were persisting during the 1990s. There has been concern that social inequalities in mortality and life expectancy have been increasing rather than declining during recent years.[3 4 5] Social inequalities in health have been extensively described in middle age, in relation to occupation.[6] However, there is uncertainty about the extent to which inequalities in middle age continues to persist in older age, with a lack of reports on people over 65years.[7]
We have examined the extent of social inequalities in all-cause mortality and CHD mortality (the single most important cause of death) among British men followed up from 1978-80 for a 25-year period. In particular, we have examined whether relative social class differences, based on occupation, have changed over time independent of age, and the influence of age on the relative size of social class differences. Moreover, since mortality rates (both from all causes and from CHD) have been declining during the study period, both in the whole population[8] and in this cohort,[9] we have also examined how the absolute differences in mortality between social classes have changed over time.
Methods
The British Regional Heart Study (BRHS) is a prospective study of cardiovascular disease comprising a socially and geographically representative sample of 7735 men aged 40-59years drawn from one general practice in each of 24 towns representing all major British regions. Details of the BRHS are reported elsewhere.[10] Data on mortality were obtained by the established procedure of ‘flagging’ participants with the NHS Central Register. The period of follow-up used for this report was from 1978-80, when the participants were enrolled in the study, up to 31st October 2005. The longest-held occupation of each man was recorded at the study entry and categorised using the Registrar Generals' Social Class Classification (I, II, III non-manual, III manual, IV and V).[11] Cause of death was coded from deaths certificate using the International classification of diseases, 9th revision (ICD-9). CHD deaths were those with ICD-9 codes 410–414.
Statistical analyses
All analyses were carried out using SAS version 8, with the exception of analyses examining social class*age and social class*period interactions, carried out with STATA version 9. Survival analysis was carried out and Kaplan Meier survival curves were plotted to investigate whether the probability of survival from all-cause and CHD mortality differed according to social class. Kaplan Meier curves were computed for four categories of social class – social classes I and II combined, social class IIInon-manual, social class IIImanual, and social classes IV and V combined. Cox's proportional hazard model was used to assess the relation between social class and all-cause and CHD mortality. Age-adjusted hazard ratios with 95% confidence intervals (CI) were calculated for the above four social class groups using social classes I and II as the reference category. The model was adjusted for age, which was fitted as a continuous variable.
We examined trends in social inequalities in all-cause and CHD mortality over the follow-up time (164,120 person years). The follow-up time was truncated at 25years and was divided into five equal calendar periods starting from the baseline period of 1978-80: 0-5years (1978-80 to 1983-85), 5-10years (1983-85 to 1988-90), 10-15years (1988-90 to 1993-95), 15-20years (1993-95 to 1998-2000), 20-25years (1998-2000 to 2003-05) and baseline age was divided into four groups of 40-44, 45-49, 50-54 and 55-59. Overall hazard ratios with 95%CI for all-cause and CHD mortality comparing manual with non-manual groups were calculated for the four age groups and for the five time periods. Age-adjusted hazard ratios were calculated also for each age group within each time period. Social class I, II and IIInon-manual were grouped as ‘non-manual’ while social classes IIImanual, IV and V were grouped as ‘manual’ to provide a single overall summary of social inequalities and their trends. Cox models included effects of age, period effect, social class, social class*age interaction (to ascertain whether social class effects changed as subjects aged), and social class*period interaction (to ascertain whether the social class effect changed over calendar time). Because of the sampling structure of the study where men were chosen from within towns, we calculated robust standard errors which adjusted for the clustering of responses by men within towns.[12]
Rates of death from all-cause and CHD mortality were estimated to ascertain the absolute difference in survival between manual and non-manual groups. This was done according to the same age groups and calendar periods used for looking at relative differences described above. To estimate the overall trend we calculated the change in hazard ratio over a 20-year calendar period. Crude survival rates were estimated for every year of age from 40 (age of youngest cohort members at the beginning of follow-up) to age 84 (age of oldest member of cohort at the end of follow-up). For each year of age, data used included every subject who passed through that year of age. These crude estimates were then added together to give a cumulative hazard function from age 40. This was then multiplied by exp(β*x), where x represented social class, period and social class*period interaction and β represented effects of these variables, estimated from the appropriate Cox proportional hazards model. Different values for social class (non-manual and manual) and period (1981 and 2001) were chosen to calculate cumulative hazard functions, and thus survival probability, for these particular social class/period combinations.[13] Uncertainty associated with these modelled estimates was addressed by taking 1000 bootstrap samples, using the bias-corrected method for obtaining 95% confidence intervals.[14]
Results
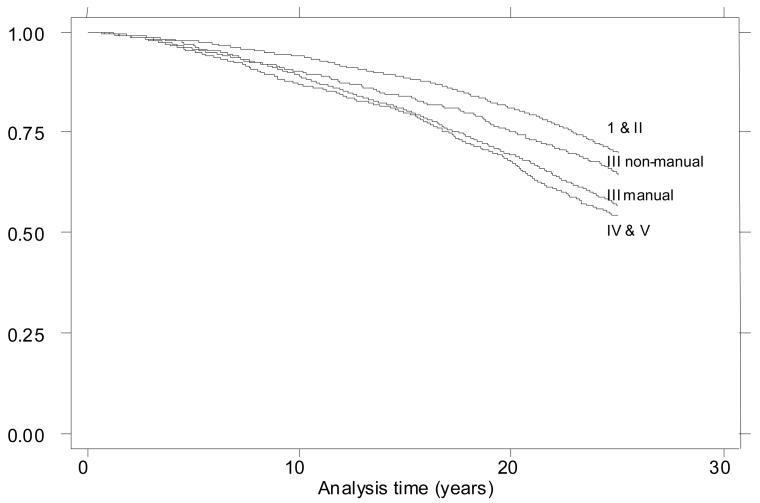
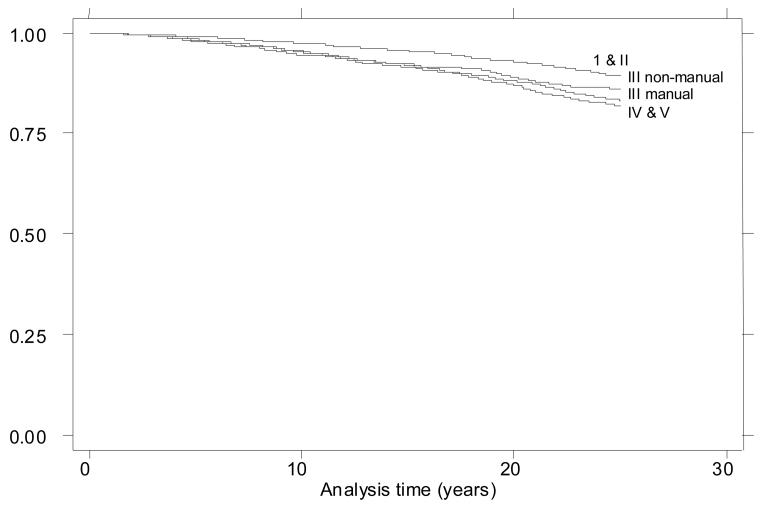
Analyses are based on 7735 men aged 40-59 at entry, followed for 25 years (164,120 person years at risk) to age 65-84, during which 3009 deaths occurred from all causes, of which 1003 were attributed to CHD. The overall hazard ratios comparing men of manual and non-manual social class were 1.56 (95%CI 1.45-1.69, p<0.001) for all-cause mortality and 1.54 (95%CI 1.35-1.76, p<0.001) for CHD mortality. Figures 1 and 2 are Kaplan Meier survival curves showing the difference in probability of survival from all-cause and CHD mortality according to social class. Both sets of curves appear to diverge over the follow-up period. The survival curves also showed that the social class relation with mortality was graded with highest probability of survival in social class I and II and progressively lower probability of survival in IIInon-manual, IIImanual, and IV and V. The age-adjusted hazard ratios demonstrating this relationship of social class and mortality are presented in table 1.
Figure 1.
Kaplan Meier survival curves comparing all-cause mortality according to social class groups in 7735 British Men aged 40-59 years followed-up from 1978-80 till 2005
Figure 2.
Kaplan Meier survival curves comparing coronary heart disease (CHD) mortality according to social class groups in 7735 British Men aged 40-59 years followed-up from 1978-80 till 2005
Table 1.
Age-adjusted hazard ratios for all-cause and coronary heart disease (CHD) mortality according to social class in 7735 British Men aged 40-59 years followed-up from 1978-80 till 2005
| All-cause mortality Hazard ratio (95% confidence interval) |
CHD mortality Hazard ratio (95% confidence interval) |
|
|---|---|---|
| Social class I & II | 1.00 | 1.00 |
| Social class III NM | 1.16 (1.01, 1.34) | 1.27 (1.00, 1.61) |
| Social class III M | 1.49 (1.37, 1.63) | 1.51 (1.29, 1.75) |
| Social class IV & V | 1.64 (1.46, 1.83) | 1.65 (1.36, 2.00) |
Relative social class differences: the influence of age
Table 2 shows age-adjusted hazard ratios comparing manual with non-manual men for all-cause and CHD mortality for different 5-year age groups in the five 5-year calendar periods during the 25-year follow-up. There was evidence that the effect of social class lessened as men grew older (displayed in table 2 by following men with increasing age along the table diagonally downwards to the right). For example, the hazard ratio for all-cause mortality in 55-59year old men at baseline decreased from 1.70 in the first 5-year period to 1.15 in the last 5-year period of follow-up, when aged 75-79. Although this pattern was not seen consistently in all age groups, the overall hazard ratios decreased with increasing baseline age, both for all-cause and CHD mortality (table 2). The ratio of hazard ratios for social class differences in all-cause mortality was 0.77 (95%CI 0.65-0.91, p=0.003), representing a 23% decrease in the relative social class difference in risk for a 20-year increase in age. A similar age-related decline was seen for CHD. The ratio of hazard ratios for a 20-year increase in age for CHD was 0.73 (95%CI 0.55-0.98, p=0.035); the estimated hazard ratio for a manual social class subject would be 1.84 at age 55, but only 1.34 at age 75 years.
Table 2.
Age-adjusted hazard ratios (95% confidence interval) for all-cause and coronary heart disease (CHD) mortality in 5-year time periods comparing manual versus non-manual social classes in 7735 British Men followed-up from 1978-80 till 2005
| Age (years) | 0-5 years 1978-80 to 1983-85 |
5-10 years 1983-85 to 1988-1990 |
10-15 years 1988-90 to 1993-95 |
15-20 years 1993-95 to 1998-2000 |
20-25 years 1998-2000 to 2003-05 |
Overall for each baseline age group |
|---|---|---|---|---|---|---|
|
| ||||||
| 40-44 | ||||||
| N | 1677 | 1.75 (1.35, 2.26) | ||||
| All-cause | 1.64 | 2.05 (1.25, 3.42) | ||||
| CHD | 2.25 | |||||
|
| ||||||
| 45-49 | ||||||
| N | 1838 | 1661 | 1.67 (1.39, 2.01) | |||
| All-cause | 1.82 | 2.55 | 2.11 (1.53, 2.93) | |||
| CHD | 5.26 | 1.68 | ||||
|
| ||||||
| 50-54 | ||||||
| N | 1911 | 1797 | 1630 | 1.60 (1.39, 1.85) | ||
| All-cause | 1.09 | 1.84 | 1.62 | 1.47 (1.15, 1.88) | ||
| CHD | 0.87 | 2.90 | 2.48 | |||
|
| ||||||
| 55-59 | ||||||
| N | 1853 | 1842 | 1735 | 1583 | 1.37 (1.21, 1.54) | |
| All-cause | 1.70 | 1.49 | 1.66 | 2.25 | 1.28 (1.04, 1.58) | |
| CHD | 1.99 | 1.52 | 1.49 | 2.68 | ||
|
| ||||||
| 60-64 | ||||||
| N | 1724 | 1723 | 1641 | 1505 | ||
| All-cause | 1.65 | 1.99 | 1.74 | 1.39 | ||
| CHD | 1.10 | 1.52 | 1.99 | 1.61 | ||
|
| ||||||
| 65-69 | ||||||
| N | 1504 | 1563 | 1522 | |||
| All-cause | 1.25 | 1.69 | 1.57 | |||
| CHD | 1.56 | 1.33 | 2.03 | |||
|
| ||||||
| 70-74 | ||||||
| N | 1286 | 1326 | ||||
| All-cause | 1.42 | 1.55 | ||||
| CHD | 1.27 | 1.91 | ||||
|
| ||||||
| 75-79 | ||||||
| N | 991 | |||||
| All-cause | 1.15 | |||||
| CHD | 1.03 | |||||
|
| ||||||
| Overall for each calendar period |
||||||
| All-cause | 1.58 (1.21, 2.05) | 1.68 (1.36, 2.07) | 1.55 (1.29, 1.86) | 1.63 (1.39, 1.90) | 1.32 (1.15, 1.52) | |
| CHD | 1.71 (1.13, 2.62) | 1.43 (1.05, 1.95) | 1.59 (1.17, 2.17) | 1.49 (1.13 1.97) | 1.49 (1.15, 1.95) | |
Relative SC differences: the influence of period
We examined the extent to which relative differences in risks of death between manual and non-manual men changed over time independent of age (seen in table 2 by following men horizontally along the rows). The relative hazard of all-cause and CHD mortality for men of manual social class appeared to increase over time. For example, in men aged 55-59 at study entry the hazard ratio for all-cause mortality was 1.70 in the first 5 year period of follow-up (early 1980s), while for men aged 55-59 in the 15-20 year period of follow-up (late 1990s), it was 2.25; the corresponding hazard ratios for CHD mortality increased from 1.99 to 2.68. Although this pattern was not consistently seen across all the five time periods, an analysis extending trends across all age groups showed that over a 20-year calendar period the hazard ratio for the change in manual:non-manual social class was 1.22 (95%CI 0.83-1.80, p=0.31) for total mortality and 1.75 (95%CI 0.89-3.45, p=0.11) for CHD, representing estimated relative increases in the social class differences of 22% and 75%. Thus, although there was no conclusive evidence of any change in relative inequalities, the result observed suggested an increase rather than a decrease.
Absolute social class differences: the influence of age and period
Absolute rate differences in all-cause and CHD mortality between manual and non-manual social class groups for different calendar periods and age groups are given in table 3. Overall absolute rate differences in all-cause and CHD mortality increased with baseline age (the absolute difference in all-cause mortality rate was 8.97 per 1000 person years for those aged 55-59 at baseline compared to 3.53 per 1000 person years for 40-44 year olds; see table 3). With each successive calendar period, across all age groups, the absolute differences in mortality rates between manual and non-manual groups had increased as the men grew older (table 3).
Table 3.
Absolute difference in incidence rates per thousand person years for all-cause and coronary heart disease (CHD) mortality in 5-year time periods comparing manual versus non-manual social classes in 7735 British Men followed-up from 1978-80 till 2005
| Age (years) | 0-5 years 1978-80 to 1983-85 |
5-10 years 1983-85 to 1988-1990 |
10-15 years 1988-90 to 1993-95 |
15-20 years 1993-95 to 1998-2000 |
20-25 years 1998-2000 to 2003-05 |
Overall for each baseline age group |
|---|---|---|---|---|---|---|
|
| ||||||
| 40-44 | ||||||
| All-cause | 0.88 | 3.53 | ||||
| CHD | 0.35 | 1.27 | ||||
|
| ||||||
| 45-49 | ||||||
| All-cause | 2.54 | 3.10 | 5.81 | |||
| CHD | 2.19 | 0.78 | 2.94 | |||
|
| ||||||
| 50-54 | ||||||
| All-cause | 0.68 | 4.09 | 2.70 | 8.63 | ||
| CHD | −0.46 | 3.33 | 1.70 | 2.46 | ||
|
| ||||||
| 55-59 | ||||||
| All-cause | 6.99 | 5.06 | 5.45 | 7.49 | 8.97 | |
| CHD | 3.96 | 2.29 | 1.93 | 2.44 | 2.47 | |
|
| ||||||
| 60-64 | ||||||
| All-cause | 12.66 | 12.23 | 7.92 | 4.12 | ||
| CHD | 1.03 | 3.08 | 3.28 | 1.18 | ||
|
| ||||||
| 65-69 | ||||||
| All-cause | 6.80 | 15.96 | 12.26 | |||
| CHD | 4.10 | 2.63 | 5.10 | |||
|
| ||||||
| 70-74 | ||||||
| All-cause | 17.22 | 19.00 | ||||
| CHD | 3.60 | 7.65 | ||||
|
| ||||||
| 75-79 | ||||||
| All-cause | 10.49 | |||||
| CHD | 0.76 | |||||
|
| ||||||
| Overall for each calendar period |
||||||
| All-cause | 3.06 | 6.59 | 7.19 | 12.10 | 11.48 | |
| CHD | 1.65 | 2.01 | 2.76 | 3.08 | 3.92 | |
However, when looking at comparable age groups at different time periods, there appears to be some decrease in absolute risk difference between manual and non-manual groups over time though this is not very consistent (seen in table 3 following men along rows). But, results from modelling showed that the absolute difference in probability of survival from death of any cause from age 40 to age 65 between non-manual and manual subjects was 29% (95% bootstrap CI: 7 to 60%) in 1981 (the mid-point of first 5-year period of our follow-up) and 19% (95% CI: 4 to 47%) in 2001 (mid-point of last 5-year period of follow-up). Similarly the estimated absolute difference in probability of survival to age 65 from CHD decreased from 17% (95% CI: 0 to 64%) in 1981 to 7% (95% CI: 0 to 35%) in 2001.
Discussion
In this study of middle-aged and older British men, social inequalities in all-cause and CHD mortality appeared to persist over the period 1978-2005. Men in manual social classes had a greater hazard of all-cause and CHD mortality compared to men in non-manual social classes. The relative difference in all-cause and CHD mortality between manual and non-manual social class groups appeared to increase rather than to decline in the period 1978-2005. However, the absolute magnitude of the social class differences appeared to decline because of the fall in overall mortality rates.
Strengths and limitations of the study
Our data comes from a socio-economically representative sample of middle-aged British men. More than 98% of the cohort has been followed-up for over 25 years through the NHS Central Register and general practice records. The main strength of this paper is that it quantifies the extent of social inequalities in major health outcomes in a defined population over an extended period, using a stable indicator of social class status, in a way which few earlier studies have been able to do. The social class measure we used was based on longest held occupation, which was recorded at baseline in 1978-80 when subjects were 40-59 years. The longest held occupation (classified as non-manual or manual) is an extremely stable and well-established marker of social class, which was defined for almost all study participants. Only 8% of subjects changed their social class status under this definition over a 20 year period, confirming the stability of the measure.[15] Although social class based on occupation has limitations,[16] it was essential for this analysis to have a single measure of social status which would act as a reference point over the entire study period; we believe that longest held occupation is likely to have fulfilled this criterion better than many other measures. Dichotomising the social classes into manual and non-manual groups in our analyses provides a stable indicator of changes in the two main social class groups than would be possible with six groups. Using these stable and well-defined groups provides a useful summary of the extent of inequalities over time to obtain an overall direction of change of social inequalities. The study was based on older men, excluding subjects from inner cities, and towns with high mobility, thus excluding ethnic minorities and highly mobile people.[10] The results may not therefore be completely generalisable to younger subjects, women and ethnic minority groups and may not be directly generalisable to other Western countries. Within the study population, it is possible that the extent of social inequalities in early life will have differed appreciably between the 1920s and 1930s, when unemployment was particularly high. This is difficult to examine in the current analyses, in which we have taken into account the effect of age and calendar period and are therefore unable to define the influence of the year of birth of our cohort, as it is not possible to take into account all the three effects in the same statistical model. However, in the present study the influence of childhood social status on both all-cause and CHD mortality was modest, both among subjects born in the 1920s and 1930s.[17] Moreover, if social inequalities were stronger in the 1930s, the effect on our results would be to under-estimate either or both of the decline in social inequalities with age or the increase in social inequalities with calendar time.
Time trends in social class differences in all-cause and CHD mortality
In this study we have investigated whether social inequalities in mortality both from all causes and from CHD, the leading cause of death in the UK [18] have changed over a period of time in Britain. Though there are previous studies reporting on trends in health inequalities in Britain,[2 3 4 19 20 21] information on current trends in social class inequalities in mortality in the UK is very limited. Our findings are similar to that of some recent studies, which have shown that relative inequalities have not narrowed, and may have increased over time.[4 19 20] The Acheson report[2] demonstrated a clear widening in relative social inequalities in all-cause and CHD mortality between the early 1970s and 1990s. A recent Department of Health report demonstrated that absolute differences in social inequalities, measured by area deprivation, in circulatory disease mortality were falling till early 2000 with signs of widening relative inequalities.[5] This decline in absolute difference, which is important in public health terms, probably reflects the decline both in overall mortality rates and in CHD mortality rates,[22] since relative mortality differences have not narrowed.
With increasing age, the relative difference in mortality rates between social classes declined, but persisted at older ages, while absolute differences increased, as a result of the higher death rates among older subjects. The decrease in relative social differences with age alongside increasing absolute difference was also observed in a study in 11 European populations,[23] while the persistence of social differences at older ages is consistent with the results of other British and European studies.[23 24] The relative decline in the importance of social class at older ages is in keeping with the widely observed attenuation of risk factor-chronic disease relations at older ages.[25]
In this study we have only described the extent of inequalities over time and have not investigated possible causal pathways or mechanisms. It has been previously reported that an increase in social inequalities can be attributed to a decrease in rate of disease in higher social class with little or no improvement in lower social classes.[2 4] This implies greater beneficial changes in social classes I and II compared to lower social classes. Especially for a leading cause of death like cardiovascular disease faster change in health related behaviours such as smoking, alcohol, diet and physical activity amongst higher social classes compared to lower socio-economic groups could play a role in contributing to widening inequalities.[4] The cumulative effect of these behavioural and other factors over the life course has also been implicated as a pathway of inequalities.[7 26]
Implications of the study
The results suggest that policies in place during the 1978-2005 period have not led to a reduction in relative inequalities in total and CHD mortality, though declining death rates have mitigated the consequences of this inequality. If relative reductions in mortality are to be achieved, greater efforts will be needed to bring this about. The actions required are likely to include both general measures to reduce income inequality and improve living standards of poorer households[2] as well as more specific measures to reduce cigarette smoking prevalence and improve nutritional intakes among lower-income groups, by a combination of national and local action.[27] Ensuring equitable provision of health services, particularly preventive services, will also be important.[2] These actions need to be set in a broader policy framework ensuring that other Government policies are monitored for their impact on inequality.[2 28] Monitoring the impact of such policies on key risk factors as well as establishing targets for reducing relative differences in mortality will be important. Several such issues have been highlighted in the Department of Health publications like the Programme for Action[29] and more recently in Choosing Health.[30] More rigorous and determined steps need to be taken in implementing these reforms and policies if we want to see a narrowing of social inequalities.
Conclusions
Despite a decrease in absolute social class difference, which is of public health significance, there is still considerable scope for reducing existing inequalities in mortality. No reduction in relative social inequalities implies that manual social class groups are continuing to be at a disadvantage compared to non-manual groups. The results of our study reaffirm that greater effort needs to be made if the gap between the health of those at the higher and lower end of the social hierarchy is to be narrowed.
What is already known on this subject?
Inequalities according to social class in mortality and coronary heart disease exist.
What this study adds?
Relative social class differences in all-cause and CHD mortality did not decrease over the 25 years prior to 2005 in Britain.
Absolute social class differences in mortality have decreased over this period.
Policy implications
Although absolute social inequalities have narrowed concerted policy efforts need to be made to further reduce inequalities.
Acknowledgments
Funding: The British Regional Heart Study is funded by the Department of Health, England. The British Regional Heart Study is also a British Heart Foundation Research Group. SR is funded by a UK MRC Special Training Fellowship in Health Services Research and Health of the Public. The views expressed in this study are those of the authors and not necessarily those of the funding bodies.
Footnotes
Publisher's Disclaimer: This is a pre-copy-editing, author-produced PDF of an article accepted for publication in the Journal of Epidemiology & Community Health following peer review. The definitive publisher-authenticated version [J of Epidemiology & Community Health 2008;62:75-80] is available online at: http://jech.bmj.com/cgi/content/abstract/62/1/75
Competing interests: All authors declare that there are no competing interests.
Ethical approval: The British Regional Heart Study has local (from each of the districts in which the study was based) and multicentre ethical committee approvals.
References
- 1.Black D, Morris JN, Smith C, et al. Inequalities in health: report of a Research Working Group. Department of Health and Social Security; London: 1980. [Google Scholar]
- 2.Acheson Donald. Independent Inquiry into Inequalities in Health. The Stationary Office; London: 1998. [Google Scholar]
- 3.Shaw M, Davey Smith G, Dorling D. Health inequalities and New Labour: how the promises compare with real progress. BMJ. 2005;330:1016–21. doi: 10.1136/bmj.330.7498.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mackenbach JP, Bos V, Andersen O, et al. Widening socioeconomic inequalities in mortality in six Western European countries. Int J Epidemiol. 2003;32:830–7. doi: 10.1093/ije/dyg209. [DOI] [PubMed] [Google Scholar]
- 5.Department of Health . Tackling Health Inequalities: Status Report on the Programme for Action. Department of Health Publications; London: 2005. [Google Scholar]
- 6.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–98. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 7.Bowling A. Socioeconomic differentials in mortality among older people. J Epidemiol Community Health. 2004;58:438–40. doi: 10.1136/jech.2003.017582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petersen S, Peto V, Scarborough P, et al. Coronary heart disease statistics 2005. BHF; London: 2005. [Google Scholar]
- 9.Lampe FC, Morris RW, Walker M, et al. Trends in rates of different forms of diagnosed coronary heart disease, 1978 to 2000: prospective, population based study of British men. BMJ. 2005;330:1046–9. doi: 10.1136/bmj.330.7499.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walker M, Whincup PH, Shaper AG. The British Regional Heart Study 1975-2004. Int J Epidemiol. 2004;33:1185–92. doi: 10.1093/ije/dyh295. [DOI] [PubMed] [Google Scholar]
- 11.Classification of Occupations 1970. HM Stationary Office; London: 1970. [Google Scholar]
- 12.Diggle PJ, Heagerty P, Liang K-Y, et al. Analysis of longitudinal data. 2 ed. Oxford University Press; New York: 2002. [Google Scholar]
- 13.Collett D. Modelling Survival Data in Medical Research. 2nd ed. Chapman & Hall; London: 2003. [Google Scholar]
- 14.Efron B, Tibshirani RJ. An Introduction to the Bootstrap. Chapman and Hall; London: 1993. [Google Scholar]
- 15.Emberson JR, Whincup PH, Morris RW, et al. Social class differences in coronary heart disease in middle-aged British men: implications for prevention. Int J Epidemiol. 2004;33:289–96. doi: 10.1093/ije/dyh006. [DOI] [PubMed] [Google Scholar]
- 16.Krieger N, Williams DR, Moss NE. Measuring Social Class in US Public Health Research:Concepts, Methodologies, and Guidelines. Annu Rev Public Health. 1997;18:341–78. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 17.Ramsay SE, Whincup PH, Morris RW, et al. Are childhood socio-economic circumstances related to coronary heart disease risk? Findings from a population-based study of older men. Int J Epidemiol. 2007;36:560–6. doi: 10.1093/ije/dym060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petersen S, Peto V, Rayner M. 2004 Coronary heart disease statistics. London: BHF: 2004. [Google Scholar]
- 19.Avendano M, Kunst AE, van Lenthe F, et al. Trends in Socioeconomic Disparities in Stroke Mortality in Six European Countries between 1981-1985 and 1991-1995. Am J Epidemiol. 2005;161:52–61. doi: 10.1093/aje/kwi011. [DOI] [PubMed] [Google Scholar]
- 20.Davey Smith G, Dorling D, Mitchell R, et al. Health inequalities in Britain: continuing increases up to the end of the 20th century. J Epidemiol Community Health. 2002;56:434–5. doi: 10.1136/jech.56.6.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marang-van de Mheen P, Davey Smith G, Hart CL, et al. Socioeconomic differentials in mortality among men within Great Britain: time trends and contributory causes. J Epidemiol Community Health. 1998;52:214–8. doi: 10.1136/jech.52.4.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Unal B, Critchley JA, Capewell S. Explaining the Decline in Coronary Heart Disease Mortality in England and Wales Between 1981 and 2000. Circulation. 2004;109:1101–7. doi: 10.1161/01.CIR.0000118498.35499.B2. [DOI] [PubMed] [Google Scholar]
- 23.Huisman M, Kunst AE, Andersen O, et al. Socioeconomic inequalities in mortality among elderly people in 11 European populations. J Epidemiol Community Health. 2004;58:468–75. doi: 10.1136/jech.2003.010496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Breeze E, Sloggett A, Fletcher A. Socioeconomic and demographic predictors of mortality and institutional residence among middle aged and older people: results from the Longitudinal Study. J Epidemiol Community Health. 1999;53:765–74. doi: 10.1136/jech.53.12.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prospective Studies C Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. The Lancet. 2002 Dec 14;360(9349):1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 26.Graham H. Building an inter-disciplinary science of health inequalities: the example of lifecourse research. Soc Sci Med. 2002;55:2005–16. doi: 10.1016/s0277-9536(01)00343-4. [DOI] [PubMed] [Google Scholar]
- 27.Lynch J, Davey Smith G, Harper S, et al. Explaining the social gradient in coronary heart disease: comparing relative and absolute risk approaches. J Epidemiol Community Health. 2006;60:436–41. doi: 10.1136/jech.2005.041350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Whitehead M, Petticrew M, Graham H, et al. Evidence for public health policy on inequalities: 2: Assembling the evidence jigsaw. J Epidemiol Community Health. 2004;58:817–21. doi: 10.1136/jech.2003.015297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Department of Health . Tackling Health Inequalities: A Programme for Action. Department of Health Publications; London: 2003. [Google Scholar]
- 30.Department of Health . Choosing health - Making healthy choices easier. The Stationary Office; London: 2004. [Google Scholar]