Abstract
Women's breast-feeding patterns are complex, and existing definitions of breast-feeding behavior do not capture this complexity adequately. We used results from a prior qualitative study to define trajectories for feeding during the first half of infancy, and then examined household-, maternal-, and infant-level determinants of these trajectories using logistic regression analysis. The 1472 women in the study cohort lived in rural Bangladesh and were participants in the Maternal and Infant Nutrition Intervention in Matlab trial. The 3 infant feeding trajectories included women who fed only breast milk and water [full breast-feeding trajectory (FBT)]; offered mixed feeding continuously when their babies were 0–4 mo old [continuous mixed feeding trajectory (CMFT)]; and practiced any other type of breast-feeding [intermittent feeding trajectory (IFT)], which was the normative feeding behavior in this community. In adjusted regression models, women who lived in rural areas [odds ratio (OR), 2.1; 95% CI, 1.2, 3.4], came from the poorest households (OR, 3.4; 95% CI, 1.5, 7.7), and offered prelacteal (OR, 1.7; 95% CI, 1.0–2.7) were more likely to be in the FBT. Women from the richest households (OR, 1.6; 95% CI, 1.1, 2.6), employed mothers (OR, 1.7; 95% CI, 1.1, 2.6), and older mothers (OR, 1.02; 95% CI, 1.0, 1.1) were more likely to be in the CMFT, and women with higher birth-weight infants (OR, 0.6; 95% CI, 0.4–0.8) were less likely to be in the CMFT. Thus, these trajectories were associated with distinct groups of women and these results provide information useful for developing interventions to improve breast-feeding practices.
Introduction
Exclusive breast-feeding (EBF)6 for 6 mo has been promoted as the preferred breast-feeding practice by the WHO (1). In developing countries, the practice of EBF (giving nothing but breast milk and medicine) offers significant benefits for infant health, and quality and quantity of breast milk substitutes are often inadequate (2). Despite the WHO recommendation, 70% of mothers in Bangladesh feed nonbreast milk foods to infants before they are 6 mo old (3).
Although a high prevalence of non-EBF exists in many communities around the world as in Bangladesh, little attention has been paid to identifying the longitudinal patterns of non-EBF in the first 6 mo of life. The standard definitions describing breast-feeding practices, EBF (breast milk only), predominant breast-feeding (breast milk and nonfood–based liquids), and partial breast-feeding (mixed feeding with breast milk and any other sources of energy and nutrients), are not suitable for longitudinal description of breast-feeding patterns (4). Long-term breast-feeding patterns are often complex as mothers move into and out of different patterns over time; in the Philippines (5), some mothers moved from EBF to non-EBF and back again. To bring feeding behavior more in line with optimal practice, it is important to understand the different long-term feeding patterns that exist in communities.
In this study, we used the WHO recommendation and mothers' perspectives of normative and nonnormative breast-feeding practices that we had previously observed in breast-feeding practices over time. We defined the full breast-feeding trajectory (FBT) to identify women who fed breast milk and water during the first 6 mo of life and, therefore, almost practiced EBF. In a previous study, we found that when mothers perceived that their breast milk was inadequate, they described giving nonhuman milk foods continuously during 0–4 mo (6); we called this pattern the continuous mixed feeding trajectory (CMFT). If breast-feeding was going well, mothers sometimes fed nonbreast milk foods intermittently to their infants during 0–4 mo and continuously during 5–6 mo (6); we called this pattern the intermittent feeding trajectory (IFT). Compared with EBF, intermittent feeding of nonhuman milk foods (as in IFT) has been associated with increased diarrhea (7). Regular introduction of nonhuman milk foods to 0- to 3-mo-old infants, as in the CMFT, has been associated with significant increases of diarrhea (8) and growth faltering (9,10). Given the important consequences of introducing nonhuman milk foods during the first 6 mo of life, it is important to understand the determinants of the 3 feeding trajectories.
The objective of our study was to examine the household-, maternal-, and infant-level characteristics of women following the 3 breast-feeding trajectories. To accomplish this, we compared women in the FBT and CMFT to those in the normative breast-feeding trajectory (IFT). The results of our analysis identify how selected social and behavioral factors affect feeding norms and also identify those women with special needs for breast-feeding counseling.
Methods
Subjects and study design.
We conducted secondary analysis of the data from the Maternal and Infant Nutrition Intervention in Matlab (MINIMat). In MINIMat, women were enrolled early in pregnancy and randomly assigned to nutritional supplements during pregnancy with the objective of increasing birth weight and reducing infant mortality. Women received 1 of 3 micronutrient formulations and food supplementation that was started earlier or later during pregnancy. In addition, MINIMat subjects were individually randomized during pregnancy to receive either general health counseling alone or along with intensive breast-feeding counseling that began during pregnancy and continued during the early postpartum period. We used information from only those women (n = 1607) who were assigned to the health-counseling group (as we were interested in existing feeding patterns) and gave birth from May 2002 to June 2004. To be eligible for this investigation, these women had to give birth to a live infant, live in the study area, and give consent to participate in the infant follow-up (n = 1501). Infants were excluded if they were a woman's second child born into the MINIMat study (n = 8) (as closely spaced pregnancies have a negative effect on breast-feeding duration) or if any feeding information was missing for the first 6 mo (n = 30). Finally, information from 1472 mother-infant dyads was included in the analysis.
Ethical clearance.
Ethical clearance for this secondary analysis was obtained from the ICDDR,B Ethical Review Committee and the Cornell University Committee on Human Subjects.
Construction of the dependent variable.
MINIMat staff members collected monthly data on consumption of 7 types of foods. The food types were: breast milk, water, fruit juice, other liquids (sugar water, tea, and honey), other milk, and semisolid and solid foods. If mothers gave any of these foods, they were asked whether these foods were given during the first or second 2-wk period of the month. No information was available about the amounts of nonhuman milk foods and beverages given to the infants. In the analysis, we used the feeding information for the first 6 mo of the infants' lives.
We summarized the infant feeding patterns into 3 trajectories. Infants who were fed only breast milk and water until 6 mo of age were in the FBT. Infants who were fed nonmilk liquids (water, fruit juice, and sugar water were not considered nonmilk liquids), cow milk, semisolids, or solid foods for 3 consecutive 2-wk periods when their babies were 0–4 mo old were in the CMFT. Infants who were fed nonhuman milk foods < 3 consecutive times starting at 0–4 mo were in the IFT. In the community, the IFT is considered the normative feeding pattern.
Selection of independent variables.
We adopted the conceptual framework of perceived insufficient milk supply (IMS) (11) to select independent variables from the MINIMat dataset. In the IMS conceptual framework, sociocultural factors [area of residence, socioeconomic status (SES), mother's education], maternal time restraint (maternal employment), and infant factors (gender and birth weight) work along with maternal physiological (prepregnancy BMI) and psychological factors (maternal age and distress during pregnancy) and breast-feeding behavior (prelacteal feeding) to affect breast milk production. Some of these factors can also negatively affect breast milk volume, leading to inadequate infant intake. Other researchers have shown that maternal physiological factors (12,13), psychological factors (14), and breast-feeding behaviors (15) affect breast milk volume and affect the duration of EBF.
Variables created for use in this study.
A wealth index was constructed using landholding, type of material used in the walls of the house, and ownership of household items excluding beds and clothing for ceremonial use. Principal component analysis was used to create 5 quintiles. In the lowest quintile were the poorest households, in the highest quintile were the richest households, and in the middle quintiles were the middle-income households. We merged the 3 middle quintiles, because the relationship between the wealth quintiles and the dependent variable did not reflect dose-response across these middle quintiles.
Maternal distress was measured at 30 wk of pregnancy using a self-reporting questionnaire of 20 items (16). We used a cutoff of 8 of the 20 questions answered positively to identify cases of distress as suggested by the previous validation in other developing countries (16). We validated the distress measured by the self-reporting questionnaire of 20 items against measurement of known stressors (e.g. household food insecurity and domestic violence) and found that the associations were significant (P < 0.01).
Statistical methods.
To test the bivariate associations, we conducted the chi-square for categorical variables and ANOVA for continuous variables. In the tables, proportions were presented for categorical variables and means ± SD were presented for continuous variables. P-values < 0.05 were considered significant. To test whether the independent variables were associated with the odds of being in one trajectory compared with another, we used logistic regression. To test for collinearity among variables, we ran collinearity diagnostics. The variance inflation factors for all the variables were <2 and the tolerances were >0.1, indicating there was no multicollinearity within the variables in the model. In the tables, odds ratios (OR) and 95% CI are presented. We used SPSS version 14 (2004) for these analyses.
Our first hypothesis was that mothers who practiced normative breast-feeding (IFT) differed from those who adhered to the WHO recommendation of EBF for 6 mo (proxied with the FBT) (n = 902). Differences identified in this analysis would provide information about why some mothers chose more intensive breast-feeding when it was not a community norm. Our second hypothesis was that mothers who were in the CMFT differed from those in the IFT (n = 1328). Differences identified in this analysis would provide information that could be used to identify women in need of specific breast-feeding support. For each analysis, individuals were selected out during the analysis when they did not have information in the independent variables.
To test each hypothesis, we analyzed 3 models. The first model contained distal factors (sociocultural, maternal time restraint, and infant variables), the second model contained maternal proximal factors (psychological, physiological, and breast-feeding behavior variables), and the 3rd model contained both proximal and distal factors. We did not seek to create a parsimonious model, because we were interested in keeping the variables that represented the concepts of the conceptual model used. A broader presentation of the concept is described by Milman et al. (17). The effect of food and micronutrient supplementation during pregnancy was controlled in all the models.
Results
Sample characteristics.
The 38 women excluded from the study were better educated, had better SES, and lived in the semiurban (as opposed to rural) area compared with those who were included. Mothers who lived in the semiurban areas, came from households with high SES, were employed, were better educated, and had lower infant birth weight were less likely to practice FBT (Table 1).
TABLE 1.
Characteristics of women and their infants classified by infant feeding trajectory1
| Independent variables | FBT | IFT | CMFT |
|---|---|---|---|
| n | 144 | 758 | 570 |
| Semiurban residence,* % | 18.1 | 27.7 | 27.7 |
| Household SES,*** % | |||
| Poorest | 29.2 | 19.9 | 15.3 |
| Middle income | 60.4 | 58.0 | 60.4 |
| Richest | 10.4 | 22.0 | 24.4 |
| Mother's education,** y | 4.2 ± 3.9 | 5.1 ± 4.0 | 5.5 ± 4.1 |
| Mother employed,** % | 4.2 | 6.4 | 12.3 |
| Infant gender, % male | 45.5 (143) | 50.3 (752) | 52.4 (565) |
| Birth weight,* kg | 2.66 ± 0.38 (135) | 2.72 ± 0.39 (705) | 2.66 ± 0.38 (527) |
| Prelacteal given, % | 18.5 (135) | 25.4 (713) | 27.6 (539) |
| Maternal age, y | 26.2 ± 4.3 | 25.5 ± 5.8 (757) | 25.9 ± 5.6 (569) |
| Prepregnancy BMI, kg/m2 | 19.9 ± 2.5 | 20.3 ± 2.6 (757) | 20.1 ± 2.6 |
| Maternal distress, % | 19.1 (136) | 18.8 (730) | 16.6 (549) |
Values are mean ± SD or % (number of mother-infant dyads if not that noted in the column head). Asterisks indicate groups differed: ***P < 0.001, **P < 0.01, *P < 0.05.
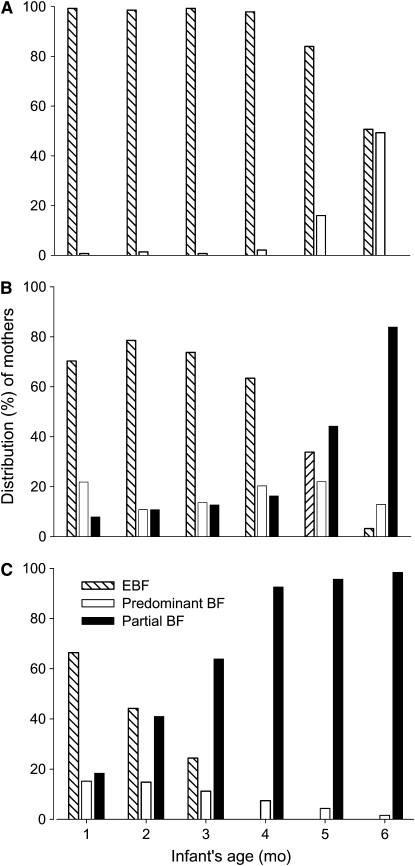
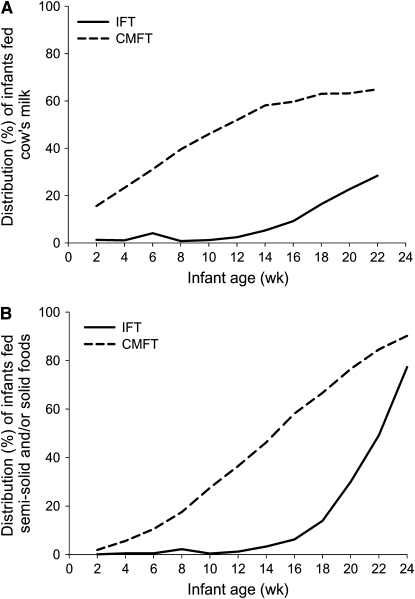
Mothers in the FBT practiced mostly EBF until 5 mo. By 6 mo, almost one-half practiced predominant breastfeeding; they had started feeding water (Fig. 1A). Mothers in the IFT mostly practiced EBF from 1–4 mo and then partial breast-feeding increased dramatically (Fig. 1B). Mothers in the CMFT increasingly practiced partial breast-feeding from 1–3 mo. By mo 4, no one from the CMFT was practicing EBF (Fig. 1C). A similar proportion of mothers in the IFT and CMFT fed fruit juice, but a much higher proportion of mothers in the CMFT fed cow milk (Fig. 2A) and semisolid and solid foods (Fig. 2B) compared with mothers in the IFT.
FIGURE 1 .
The monthly feeding patterns of mothers in the FBT (n = 144) (A), IFT (n = 758) (B), CMFT (n = 570) (C) according to conventional definitions of breast-feeding behavior (EBF, predominant breast-feeding, and partial breast-feeding).
FIGURE 2 .
Comparison of the proportions of infants fed cow milk (A) and semisolids and/solids (B) in the IFT and CMFT.
Those who lived in the rural area, came from poor or middle-income households (Table 2, model 1), and offered prelacteals to their infants (Table 2, model 2) had significantly higher odds of being in the FBT. The full model showed similar results (Table 2, model 3).
TABLE 2.
The odds of being in the FBT compared with IFT (n = 902) by sociocultural and infant factors (model 1), maternal physiological, psychological, and behavioral factors (model 2), and all the factors (model 3)1
| Independent variables | Model 1, n = 840 | Model 2, n = 817 | Model 3, n = 810 |
|---|---|---|---|
| OR (95% CI) | |||
| Rural residence | 1.93 (1.19–3.12)** | 2.06 (1.25–3.39)** | |
| SES | |||
| Poorest | 3.44 (1.59–7.40)** | 3.46 (1.55–7.70)** | |
| Middle income | 2.41 (1.26–4.60)** | 2.39 (1.21–4.70)* | |
| Maternal education, y | 0.98 (0.93–1.04) | 0.98 (0.93–1.05) | |
| Mother employed | 0.49 (0.19–1.26) | 0.49 (0.19–1.32) | |
| Infant gender, male | 0.80 (0.55–1.17) | 0.82 (0.56–1.21) | |
| Birth weight, 400 g | 1.00 (0.83–1.21) | 1.03 (0.84–1.26) | |
| Prelacteal given | 1.66 (1.01–2.73)* | 1.76 (1.06–2.90)* | |
| Maternal age, y | 1.09 (0.99–1.07) | 1.02 (0.98–1.05) | |
| Prepregnancy BMI, kg/m2 | 0.97 (0.89–1.05) | 0.98 (0.90–1.06) | |
| No distress | 0.91 (0.60–1.58) | 0.90 (0.55–1.48) | |
Models adjusted for pregnancy food and micronutrient supplementation. **P < 0.01, * P < 0.05.
Living in the richest households, maternal employment, and lower infant birth weight were associated with higher odds of being in the CMFT (Table 3, model 1). In the final model, in addition to the factors identified previously (Table 3, model 3), maternal age reached significance. Older mothers had higher odds of being in the CMFT.
TABLE 3.
The odds of being in the CMFT compared with IFT (n = 1324) by sociocultural and infant factors (Model 1), maternal physiological, psychological and behavioral factors (Model 2), and all the factors (Model 3)1
| Independent variables | Model 1, n = 1232 | Model 2, n = 1213 | Model 3, n = 1193 |
|---|---|---|---|
| OR (95% CI) | |||
| Rural residence | 0.92 (0.71–1.18) | 0.98 (0.75–1.27) | |
| SES | |||
| Middle income | 1.37 (0.99–1.91) | 1.40 (0.99–1.96) | |
| Richest | 1.54 (1.00–2.37)* | 1.65 (1.06–2.57)* | |
| Maternal education, y | 1.01 (0.98–1.04) | 1.02 (0.99–1.06) | |
| Mother employed | 1.86 (1.23–2.80)** | 1.71 (1.12–2.62)* | |
| Infant gender, male | 0.14 (0.91–1.44) | 1.11 (0.88–1.41) | |
| Birth weight, 400 g | 0.83 (0.74–0.93)** | 0.81 (0.72–0.92)*** | |
| Prelacteal given | 0.89 (0.69–1.16) | 0.92 (0.70–1.20) | |
| Maternal age, y | 1.01 (0.99–1.03) | 1.02 (1.01–1.05)* | |
| Prepregnancy BMI, kg/m2 | 0.96 (0.92–1.00) | 0.96 (0.92–1.01) | |
| No distress | 1.20 (0.89–1.63) | 1.26 (0.92–1.71) | |
Models adjusted for pregnancy food and micronutrient supplementation. ***P < 0.001, **P < 0.01, *P < 0.05.
Discussion
We created breast-feeding trajectories based both on mothers' behaviors and perspectives from our previous research and on the WHO infant feeding recommendations (6,1). This gave us a unique and meaningful way of distinguishing between different prevalent breast-feeding patterns. Defining breast-feeding trajectories will allow us to assess the long- and short-term risks of morbidity and poor growth associated with each trajectory. The trajectories also allow us to think about interventions to change normative feeding practices separately from interventions to address specific breast-feeding support needs. For instance, to change the normative feeding practice (IFT) in this population, we may need appropriate behavior change and communication materials and channels that help the mothers to come to a common understanding of the meaning and usefulness of EBF. But to change the nonnormative feeding practice (CMFT), mothers may need practical training on how to increase breast milk production.
An important strength of our study is the availability of infant feeding data, which we used to construct the trajectories. Compared with recalls of infant feeding since birth, cross-sectional assessments of feeding practices, such as 24-h recalls, often overestimate the prevalence of EBF (18,19), whereas recalls of feeding practices since birth are subject to recall bias because of the length of the recall period (18,20). In the present study, breast-feeding information was collected every month, which yielded more valid data than would a retrospective assessment covering 6 mo of lactation.
This study is valuable because it joins a small number of studies in which breast-feeding practices have been assessed longitudinally (5,21), but it does have some limitations. We did not have information about the amounts of foods or frequency of offering foods. Periodic introduction of small amounts of nonbreast milk foods may not be as harmful as regular use of nonhuman milk foods. Ensuing misclassifications may have weakened the relationship between the independent variables and breast-feeding trajectories.
We created the breast-feeding trajectories based on the breast-feeding practices of a small purposive sample of mothers in a qualitative study (6). It is possible that we did not identify all possible breast-feeding trajectories. Moreover, the mothers in the quantitative study were not asked about their reasons for feeding nonbreast milk foods. In future studies, it would be useful to assess mothers' reasons for offering nonbreast milk foods, because some of these reasons may lead to the harmful practice of sustained introduction of complementary foods early in an infant's life.
A further limitation of this study is that we did not find variables in the MINIMat data to represent all the concepts of the IMS conceptual framework. Among the distal factors, we could not find a suitable proxy indicator for maternal comfort. Among the proximal factors, we could not include breast-feeding frequency to represent the concept of breast-feeding behavior, as feeding frequency was collected only at 3 and 5 mo. To represent maternal physiologic factors, we had information on violence and distress during pregnancy. We chose distress to represent maternal psychological factor, as it was measured with an existing scale. However, because distress was measured at 30 wk of pregnancy, it is unknown whether it is a good representation of distress during lactation.
Comparison of mothers in the FBT with those in the IFT.
That a majority of the mothers in our study did not practice EBF for 6 mo is not surprising. Researchers from Bangladesh and other countries have reported that mothers do not adhere to this recommendation (3,18,20). Comparing these 2 groups, however, allows us to understand why some mothers adhere to the WHO recommendation when this is not the norm in this community. Mothers in the FBT were less likely to live in the semiurban area than the women in the IFT. Other researchers have consistently reported a negative association between urban living and breast-feeding duration (3,22–24). In the urban slums of Dhaka, Bangladesh, Haider et al. (25) reported that mothers believed that breast milk was not sufficient for their infants. Although Matlab's semiurban area was not an urban slum, it is possible that the association between the area of residence and FBT was related to the influence of urban living conditions on breast-feeding in terms of beliefs, constraints, and accessibility of breast milk substitutes.
Mothers in the FBT came from poorer households than mothers in the IFT; similar results relating EBF with poverty were reported elsewhere (3,23,26). A possible explanation is that mothers who fed only breast milk and water would have liked to feed other foods but could not afford acceptable (from their own perspective) breast milk substitutes.
In our study, we divided mothers who introduced complementary foods before 6 mo into the IFT and CMFT. When comparing those in the FBT with those in the IFT, we found that those in the FBT were more likely to have fed prelacteals. In contrast, however, other researchers have reported that those who feed prelacteals are more likely to feed complementary foods early than those who do not feed prelacteals (15). It is possible that the opposite relationship our analysis reveals results from our having used only a subset of the population who introduce complementary foods before 6 mo. Our study also made no distinction between prelacteals fed as a ritual (token amount) and those fed as a response to delayed onset of lactation (significant amount). This lack of distinction may have affected our ability to understand the relationship between prelacteal feeding and early supplementation.
Our analysis shows that the message of “exclusively” breast-feeding an infant has not adequately reached the community. It is possible that reaching the mothers with support related to how to prolong EBF during 3–4 mo will be needed to change the normative feeding practice in Matlab.
Comparison of mothers in the CMFT with those in the IFT.
Mothers from the richest households were more likely to be in the CMFT. Mothers in the CMFT were more likely to be employed outside home. Maternal employment could curtail the opportunities for breast-feeding if the infant was left behind (27). Both high SES and maternal employment could also allow mothers to choose not to EBF. Our finding that the risk of early addition of nonbreast milk foods was higher when birth weight was lower has also been reported in other studies. Some researchers have proposed that lower birth-weight infants had an underdeveloped sucking reflex leading to difficulty establishing an optimal milk supply (12), whereas others found that smaller infants were more likely to be supplemented or weaned, as mothers perceived their breast milk as inadequate (28).
The odds of being in the CMFT increased with increasing maternal age. In a study by Huffman et al. (29) conducted in Matlab, high workload was associated with reduced suckling frequency. Our qualitative study (6) revealed that multiparous (and thus older) mothers received little help with household chores. It is possible that older mothers, constrained by workload, reduced feeding frequency. As a result, breast milk volume decreased to amounts that were inadequate to meet their infants' needs, requiring early complementary feeding. The positive association between multiparity and perceived breast milk inadequacy has been was reported by other researchers (30,31).
To summarize, our analysis allows us to identify mothers who are likely to start sustained introduction of complementary foods before an infant is 4 mo old. Because this practice of providing complementary foods regularly before an infant is 4 mo old has been associated with morbidity and growth impairment, it is important that mothers in the CMFT are reached with suitable support.
In conclusion, in Matlab, what mothers consider normative breast-feeding practices does not conform to the WHO recommendation of EBF for 6 mo; few mothers practiced EBF for this long. Our data suggest that one might affect the normative pattern by disseminating a clear message about the hazards of intermittent mixed feeding and by working with mothers at 3–4 mo to reinforce continued EBF through encouragement and teaching strategies to increase breast milk production.
Despite the prevalent breast-feeding culture, mothers in the CMFT practiced early and sustained introduction of complementary foods. It is encouraging to note that both mothers and nutrition experts view this trajectory of feeding as nonnormative. Mothers in the CMFT had both biological and sociocultural constraints that could be barriers to successful breast-feeding experiences. It is important to target these mothers for breast-feeding support interventions.
The breast-feeding trajectories give us a new way of distinguishing among the different longitudinal patterns of breast-feeding that exist in communities. Identifying longitudinal patterns of non-EBF in the first 6 mo of breast-feeding is essential for developing effective, context-specific infant feeding messages and policies in relation to the WHO recommendations. In future studies, the impact of breast-feeding trajectories on the morbidity and growth of infants should be studied.
Acknowledgments
We thank Drs. Lars Åke Persson and Shams El Arifeen, who were the Principal Investigators of the MINIMat trial, and George Smith for editing the manuscript.
Supported by a Fogarty/NIH training grant (D43 TW001271; S. R. to K. M. R.). The Maternal and Infant Nutrition Intervention in Matlab research study was funded by the United Nations Children's Fund, Swedish International Development Cooperation Agency (SIDA), UK Medical Research Council, Swedish Research Council, Department of International development (DFID), International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B), Global Health Research Fund-Japan, Child Health and Nutrition Research Initiative, Uppsala University, and the United States Agency for International Development. ICDDR,B acknowledges with gratitude the commitment of these donors to the Centre's research efforts. ICDDR,B also gratefully acknowledges these donors who provided unrestricted support to the Centre's research efforts: Australian International Development Agency, Government of Bangladesh, Canadian International Development Agency, Government of Japan, Government of Netherlands, SIDA, Swiss Development Cooperation, and DFID.
Author disclosures: S. Rasheed, E. A. Frongillo, C. M. Devine, D. S. Alam, and K. M. Rasmussen, no conflicts of interest.
Abbreviations used: CMFT, continuous mixed feeding trajectory; EBF, exclusive breast-feeding; FBT, full breast-feeding trajectory; IFT, intermittent feeding trajectory; IMS, insufficient milk supply; MINIMat, Maternal and Infant Nutrition Intervention in Matlab; OR, odds ratio; SES, socioeconomic status.
References
- 1.WHO. Global strategy for infant and young child feeding. Geneva: WHO; 2003. [PubMed]
- 2.Kramer MS, Ristuko K. Optimal duration of exclusive breastfeeding: a systematic review. Geneva: WHO; 2002. [DOI] [PubMed]
- 3.Giashuddin MS, Kabir M. Duration of breastfeeding in Bangladesh. Indian J Med Res. 2004;119:267–72. [PubMed] [Google Scholar]
- 4.Labbok M, Krasovec K. Towards consistency in breastfeeding definitions. Stud Fam Plann. 1990;21:226–30. [PubMed] [Google Scholar]
- 5.Zohoori N, Popkin BM, Fernandez ME. Breast-feeding patterns in the Philippines: a prospective analysis. J Biosoc Sci. 1993;25:127–38. [DOI] [PubMed] [Google Scholar]
- 6.Rasheed S. Understanding breastfeeding practices in Bangladesh: links between mothers' perception and practice. Ithaca: Cornell University; 2007.
- 7.Kramer MS, Ristuko K. Optimal duration of exclusive breastfeeding: a systematic review. Geneva: WHO; 2002. Report No.: WHO/NHD/01.08.
- 8.Brown KH. Infant feeding practices and their relationship with diarrheal and other diseases in Huascar (Lima), Peru. Pediatrics. 1989;83:31–40. [PubMed] [Google Scholar]
- 9.Arifeen SE, Black RE, Caulfield LE, Antelman G, Baqui AH. Determinants of growth in the slums of Dhaka: size and maturity at birth, breastfeeding and morbidity. Eur J Clin Nutr. 2001;55:167–78. [DOI] [PubMed] [Google Scholar]
- 10.Hop LT, Gross R, Giay T, Sastroamidjojo S, Schultink W, Lang NT. Premature complementary feeding is associated with poorer growth outcome of Vietnamese children. J Nutr. 2000;130:2683–90. [DOI] [PubMed] [Google Scholar]
- 11.Hill PD, Humenick SS. Insufficient milk supply. Image J Nurs Sch. 1989;21:145–8. [DOI] [PubMed] [Google Scholar]
- 12.Perez-Escamilla R, Cohen R, Brown KH, Landa-Rivera L, Canahauti J, Dewey KG. Maternal anthropometric status and lactation performance in low-income Honduran population: evidence for the role of infants. Am J Clin Nutr. 1995;61:528–34. [DOI] [PubMed] [Google Scholar]
- 13.Rasmussen KM. The influence of maternal nutrition on lactation. Annu Rev Nutr. 1992;12:103–17. [DOI] [PubMed] [Google Scholar]
- 14.Gussler J, Briesemeister L. Insufficient milk syndrome: a bio-cultural explanation. Med Anthropol. 1980;4:145–74. [Google Scholar]
- 15.Perez-Escamilla R, Segura-Millan S, Canahauti J, Allen H. Pre-lacteal feeds are negatively associated with breastfeeding outcomes in Honduras. J Nutr. 1996;126:2765–73. [DOI] [PubMed] [Google Scholar]
- 16.Harpham T, Huttly S, De Silva MJ, Abramsky T. Maternal mental health and child nutritional status in four developing countries. J Epidemiol Community Health. 2005;59:1060–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Milman A, Frongillo EA, de Onis M, Hwang J. Differential improvement among countries in child stunting is associated with long-term development and specific interventions. J Nutr. 2005;135:1415–22. [DOI] [PubMed] [Google Scholar]
- 18.Engebretsen IMS, Wamani H, Karamagi C, Semiyaga N, Tumwine J, Tylleskar T. Low adherence to exclusive breastfeeding in Eastern Uganda: a community-based cross-sectional study comparing dietary recall since birth with 24-hour recall. BMC Pediatr. 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piwoz EG, Creed de Kanashiro H, Lopez de Romana G, Black RE, Brown KH. Potential for misclassification of infants' usual feeding practices using 24-hour dietary assessment methods. J Nutr. 1995;125:57–65. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez-Cossio T, Rivera-Dommarco J, Moreno-Marcias H, Monterrubio E, Sepulveda J. Poor compliance with appropriate feeding practices in children under 2 y in Mexico. J Nutr. 2006;136:2928–33. [DOI] [PubMed] [Google Scholar]
- 21.Marquis GS, Diaz J, Bartolini R, Creed de Kanashiro H, Rasmussen KM. Recognizing the reversible nature of child-feeding decisions: breastfeeding, weaning and relactation patterns in a shanty town community of Lima, Peru. Soc Sci Med. 1998;47:645–56. [DOI] [PubMed] [Google Scholar]
- 22.Popkin BM, Bisgrove EZ. Urbanization and nutrition in low-income countries. Food Nutr Bull. 1988;10:3–23. [Google Scholar]
- 23.Forman MR. Report of the task force on the assessment of the scientific evidence relating to infant-feeding practices and infant health. Pediatrics. 1984;74 Suppl:667–94. [PubMed] [Google Scholar]
- 24.Engle PL, Menon P, Garrett JL, Slack A. Urbanization and caregiving: a framework for analysis and examples from Southern and eastern Africa. Environ Urban. 1997;9:253–70. [Google Scholar]
- 25.Haider R, Kabir I, Ashworth A. Are breastfeeding promotion messages influencing mothers in Bangladesh? Results from an urban survey in Dhaka, Bangladesh. J Trop Pediatr. 1999;45:315–8. [DOI] [PubMed] [Google Scholar]
- 26.Saha KK, Frongillo EA, Alam DS, Arifeen SE, Persson LA, Rasmussen KM. Household food security is associated with infant feeding practices in rural Bangladesh. J Nutr. 2008;138:1383–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perez-Escamilla R, Lutter C, Segall AM, Rivera A. Exclusive breast-feeding duration is associated with attitudinal, socioeconomic and biocultural determinants in three Latin American countries. J Nutr. 1995;125:2972–84. [DOI] [PubMed] [Google Scholar]
- 28.Adair LS, Popkin BM. Low birth weight reduces the likelihood of breastfeeding among Filipino infants. J Nutr. 1996;126:103–12. [DOI] [PubMed] [Google Scholar]
- 29.Huffman SL, Chowdhury AKM, Chakraborty J, Simpson NK. Breastfeeding patterns in rural Bangladesh. Am J Clin Nutr. 1980;33:144–54. [DOI] [PubMed] [Google Scholar]
- 30.Segura-Millan S, Dewey KG, Perez-Escamilla R. Factors associated with perceived insufficient milk in a low-income urban population in Mexico. J Nutr. 1994;124:202–12. [DOI] [PubMed] [Google Scholar]
- 31.Forman MR, Lewando-Hundt G, Graubard BI, Chang D, Sarov B, Naggan L, Berendes HW. Factors influencing milk insufficiency and its long-term effects: the Bedouin infant feeding study. Int J Epidemiol. 1992;21:53–8. [DOI] [PubMed] [Google Scholar]