Abstract
Every year, worldwide, about 42 million women with unintended pregnancies choose abortion, and nearly half of these procedures, 20 million, are unsafe. Some 68,000 women die of unsafe abortion annually, making it one of the leading causes of maternal mortality (13%). Of the women who survive unsafe abortion, 5 million will suffer long-term health complications. Unsafe abortion is thus a pressing issue. Both of the primary methods for preventing unsafe abortion—less restrictive abortion laws and greater contraceptive use—face social, religious, and political obstacles, particularly in developing nations, where most unsafe abortions (97%) occur. Even where these obstacles are overcome, women and health care providers need to be educated about contraception and the availability of legal and safe abortion, and women need better access to safe abortion and postabortion services. Otherwise, desperate women, facing the financial burdens and social stigma of unintended pregnancy and believing they have no other option, will continue to risk their lives by undergoing unsafe abortions.
Key words: Unsafe abortions, Maternal mortality, Postabortion care
According to the World Health Organization (WHO), every 8 minutes a woman in a developing nation will die of complications arising from an unsafe abortion. An unsafe abortion is defined as “a procedure for terminating an unintended pregnancy carried out either by persons lacking the necessary skills or in an environment that does not conform to minimal medical standards, or both.”1 The fifth United Nations Millennium Development Goal recommends a 75% reduction in maternal mortality by 2015. WHO deems unsafe abortion one of the easiest preventable causes of maternal mortality and a staggering public health issue.
Scope of the Problem
Obtaining accurate data for abortions is challenging, and especially so for unsafe abortion. Two-thirds of nations do not have the capacity to collect data, and data collection varies from country to country in both quantity and quality.2 Because unsafe abortion is often done clandestinely by untrained individuals or by the pregnant women themselves, much of it goes undocumented; figures are therefore estimates. Data suggest that even as the overall abortion rate has declined, the proportion of unsafe abortion is on the rise, especially in developing nations. From 1995 to 2003, the overall number of abortions declined, but the unsafe abortion rate was steady (from 15 to 14 abortions per 1000 women, respectively), constituting an increase from 44% to 48%.3
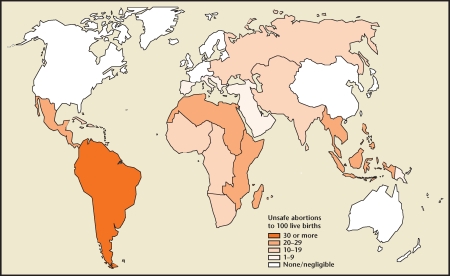
In Western nations, only 3% of abortions are unsafe, whereas in developing nations 55% are unsafe. The highest incidences of abortions that are unsafe occur in Latin America, Africa, and South East Asia (Figure 1).
Figure 1.
Unsafe abortion: global and regional estimates of incidence of unsafe abortion and associated mortality in 2003. Reproduced with the permission from the World Health Organization.1
Methods
Even safe abortion in developing nations carries risks that depend on the health facility, the skill of the provider, and the gestational age of the fetus. With unsafe abortion, the additional risks of maternal morbidity and mortality depend on what method of abortion is used, as well as on women’s readiness to seek postabortion care, the quality of the facility they reach, and the qualifications (and tolerance) of the health provider. Methods of unsafe abortion include drinking toxic fluids such as turpentine, bleach, or drinkable concoctions mixed with livestock manure. Other methods involve inflicting direct injury to the vagina or elsewhere—for example, inserting herbal preparations into the vagina or cervix; placing a foreign body such as a twig, coat hanger, or chicken bone into the uterus; or placing inappropriate medication into the vagina or rectum. Unskilled providers also improperly perform dilation and curettage in unhygienic settings, causing uterine perforations and infections. Methods of external injury are also used, such as jumping from the top of stairs or a roof, or inflicting blunt trauma to the abdomen.1,4
Health Consequences
Worldwide, some 5 million women are hospitalized each year for treatment of abortion-related complications such as hemorrhage and sepsis, and abortion-related deaths leave 220,000 children motherless.4,5 The main causes of death from unsafe abortion are hemorrhage, infection, sepsis, genital trauma, and necrotic bowel.1 Data on nonfatal long-term health complications are poor, but those documented include poor wound healing, infertility, consequences of internal organ injury (urinary and stool incontinence from vesicovaginal or rectovaginal fistulas), and bowel resections. Other unmeasurable consequences of unsafe abortion include loss of productivity and psychologic damage.
The burden of unsafe abortion lies not only with the women and families, but also with the public health system. Every woman admitted for emergency postabortion care may require blood products, antibiotics, oxytocics, anesthesia, operating rooms, and surgical specialists. The financial and logistic impact of emergency care can overwhelm a health system and can prevent attention to be administered to other patients.
Relationship With Abortion Law
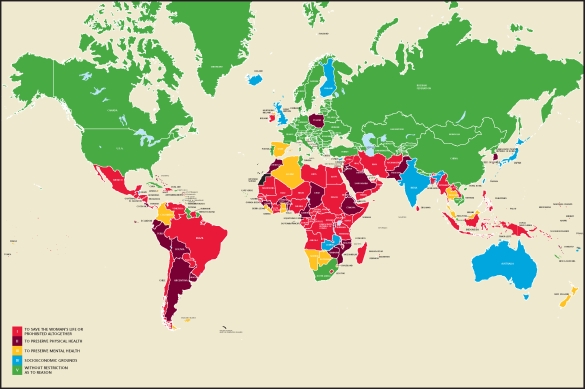
Abortion laws have a spectrum of restrictiveness. Nations may allow abortions based on saving the mother’s life, preserving physical and mental health, and socioeconomic grounds, or may be completely unrestrictive (Figure 2). Data indicate an association between unsafe abortion and restrictive abortion laws. The median rate of unsafe abortions in the 82 countries with the most restrictive abortion laws is up to 23 of 1000 women compared with 2 of 1000 in nations that allow abortions.4 Abortion-related deaths are more frequent in countries with more restrictive abortion laws (34 deaths per 100,000 childbirths) than in countries with less restrictive laws (1 or fewer per 100,000 childbirths).1
Figure 2.
World abortion laws. Reproduced with permission from the Center for Reproductive Rights.
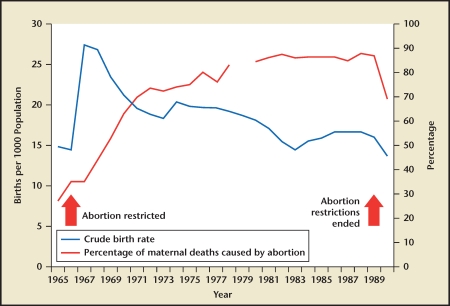
The same correlation appears when a given country tightens or relaxes its abortion law. In Romania, for example, where abortion was available upon request until 1966, the abortion mortality ratio was 20 per 100,000 live births in 1960. New legal restrictions were imposed in 1966, and by 1989 the ratio reached 148 deaths per 100,000 live births. The restrictions were reversed in 1989, and within a year the ratio dropped to 68 of 100,000 live births; by 2002 it was as low as 9 deaths per 100,000 births (Figure 3). Similarly, in South Africa, after abortion became legal and available on request in 1997, abortion-related infection decreased by 52%, and the abortion mortality ratio from 1998 to 2001 dropped by 91% from its 1994 level.6
Figure 3.
Live births and proportion of maternal deaths due to abortion. Reprinted from The Lancet, Vol. 368, Grimes DA et al, “Unsafe abortion: the preventable pandemic,” pp. 1908–1919, Copyright 2006, with permission from Elsevier.4
Less restrictive abortion laws do not appear to entail more abortions overall. The world’s lowest abortion rates are in Europe, where abortion is legal and widely available but contraceptive use is high; in Belgium, Germany, and the Netherlands, the rate is below 10 per 1000 women aged 15 to 44 years. In contrast, in Africa, Latin America, and the Caribbean, where abortion laws are the most restrictive and contraceptive use is lower, the rates range from the mid-20s to 39 per 1000 women.3
Less restrictive abortion laws also do not guarantee safe abortions for those in need; better education and access to health care are also required. In India, unsafe illegal abortions persist despite India’s passage of the Medical Termination of Pregnancy Act in the early 1970s. The act appeared to remove legal hindrances to terminating pregnancies in the underfunded (national) health care system, but women still turn to unqualified local providers for abortion. Clearly, the implications of the law never reached the population that most needed to rely on it.7 This example is also seen in Cambodia, where abortion is legally available on request and women often attempt to abort themselves before turning to hospital.8
Lack of Contraception Access and Use
More than one-third of all pregnancies are unintended, and 1 in 5 ends in abortion. In developing countries, two-thirds of unintended pregnancies occur among women who were not using any method of contraception.9 Greater contraceptive access and use alone can thus drastically reduce safe and unsafe abortion by reducing unintended pregnancies. In the Russian Federation, abortion rates sharply declined with the advent of modern contraceptive technologies.10
Obstacles to increased contraceptive access and use include religious objections, lack of awareness of the availability of contraceptive methods, concerns about possible health risks and side effects, and the mistaken belief that one cannot or will not become pregnant. Contraceptive use must also be regular to be effective: the average woman must use some form of effective contraception for at least 16 years to limit her family to 4 children, and for 20 years to limit it to 2 children.11
What Needs to Be Done?
Although daunting, the predicament is not without solutions. Preventing unintended pregnancy should be a priority for all nations. Educating women regarding their reproductive health should be incorporated in schools. In nations that are not opposed to contraceptive use, increasing contraceptive services is necessary; this includes providing accurate information choices and proper use of contraceptive methods. Governments and nongovernmental organizations need to find effective ways to overcome cultural and social misconceptions that restrict women from receiving necessary health care.
In nations where abortion is legal, providing women better access to health centers that perform abortions is imperative. Practitioners need to become better trained in safer abortion methods and be able to transfer patients to a medical facility that is capable of providing emergency care when a complication arises. WHO strongly advises that all health facilities that treat women with incomplete abortions have the appropriate equipment and trained staff needed to ensure that care is consistently available and provided at a reasonable cost. In addition, postabortion family planning counseling needs to be an integral part of the service.
Evidence demonstrates that liberalizing abortion laws to allow services to be provided openly by skilled practitioners can reduce the rate of abortion-related morbidity and mortality. However, sociopolitical and religious obstacles have and will continue to play a role in passing abortion laws. The roles of research, grassroots organizations, health providers, activists, and media are vital in highlighting the importance of relaxing abortion laws. The emotional, physiologic, and financial cost on women and families, as well as the burden on the economic health system, should no longer be ignored.
Main Points.
The World Health Organization deems unsafe abortion one of the easiest preventable causes of maternal mortality.
Data suggest that even as the overall abortion rate has declined, the proportion of unsafe abortion is on the rise.
Methods of unsafe abortion include drinking toxic fluids; inflicting direct injury to the vagina, cervix, or rectum; or inflicting external injury to the abdomen. Complications also arise from unskilled providers causing uterine perforation and infections.
Worldwide, 5 million women are hospitalized each year for treatment of abortion-related complications, and abortion-related deaths leave 220,000 children motherless.
Data indicate an association between unsafe abortion and restrictive abortion laws.
Preventing unintended pregnancy, providing better access to health care, and liberalizing abortion laws to allow services to be openly provided can reduce the rate of abortion-related morbidity and mortality.
References
- 1.World Health Organization. Unsafe abortion, authors. Global and Regional Estimates of the Incidence of Unsafe Abortion and Associated Mortality in 2003. 5th ed. Geneva: World Health Organization; 2007. http://www.who.int/reproductivehealth/publications/unsafeabortion_2003/ua_estimates03.pdf. [Google Scholar]
- 2.Graham WJ, Ahmed S, Stanton C, et al. Measuring maternal mortality: an overview of opportunities and options for developing countries. BMC Med. 2008;6:12. doi: 10.1186/1741-7015-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sedgh G, Henshaw S, Singh S, et al. Induced abortion: rates and trends worldwide. Lancet. 2007;370:1338–1345. doi: 10.1016/S0140-6736(07)61575-X. [DOI] [PubMed] [Google Scholar]
- 4.Grimes DA, Benson J, Singh S, et al. Unsafe abortion: the preventable pandemic. Lancet. 2006;368:1908–1919. doi: 10.1016/S0140-6736(06)69481-6. [DOI] [PubMed] [Google Scholar]
- 5.Singh S. Hospital admissions resulting from unsafe abortion: estimates from 13 developing countries. Lancet. 2006;368:1887–1892. doi: 10.1016/S0140-6736(06)69778-X. [DOI] [PubMed] [Google Scholar]
- 6.Jewkes R, Rees H, Dickson K, et al. The impact of age on the epidemiology of incomplete abortion in South Africa after legislative change. BJOG. 2005;112:355–359. doi: 10.1111/j.1471-0528.2004.00422.x. [DOI] [PubMed] [Google Scholar]
- 7.Malhotra A, Nyblade L, Parasuraman S, et al., editors. Realizing Reproductive Choice and Rights: Abortion and Contraception in India. Washington, DC: International Center for Research on Women; 2003. http://www.icrw.org/docs/RCA_India_Report_0303.pdf. [Google Scholar]
- 8.Long C, Ren N. Abortion in Cambodia. Country report; Paper presented at: Advancing the Role of Midlevel Providers in Menstrual Regulation and Elective Abortion Care conference; December 2–6, 2001; Pilanesberg National Park, South Africa. [Google Scholar]
- 9.Singh S, Darroch JE, Vlassoff M, Nadeau J. Adding It Up: The Benefits of Investing in Sexual and Reproductive Health Care. New York: The Alan Guttmacher Institute and United Nations Population Fund; 2003. http://www.guttmacher.org/pubs/addingitup.pdf. [Google Scholar]
- 10.Westoff C. Recent Trends in Abortion and Contraception in 12 Countries. Calverton, MD: MEASURE DHS; 2005. (DHS Analytical Studies No. 8). http://www.measuredhs.com/pubs/pdf/AS8/AS8.pdf. [Google Scholar]
- 11.The Alan Guttmacher Institute, authors. Facts on Induced Abortion Worldwide. New York: The Alan Guttmacher Institute; 2008. http://www.guttmacher.org/pubs/fb_IAW.pdf. [Google Scholar]